Highlights
-
•
Retained foreign objects (RFO), is one of the most dreadful complications of surgery.
-
•
Despite a seemingly correct count, laparotomy pads were missed at the end of surgery in three patients.
-
•
Human errors continue to occur and RFO continues to plague the surgical practice.
-
•
To avoid human error, one of several recent technologies designed to check for items left behind, should be employed.
-
•
In our report, we give an important tip on how to extract the retained surgical sponge without causing much damage.
Keywords: Gossypiboma, Retained object, Prevention
Abstract
Introduction
Leaving a surgical item inside the patient at the end of surgery, is one of the most dreadful complications. The item is frequently a surgical sponge and the resultant morbidity is usually severe. Additionally, the event poses considerable psychic strain to the operating team, notably the surgeon.
Presentation of cases
Here we describe the clinical course of three patients in whom a surgical sponge was missed, despite a seemingly correct count at the end of difficult caesarean sections. In two patients, who presented shortly after surgery, the pad was extracted with no bowel resection. In the third patient, who presented several years after surgery, colectomy was performed.
Discussion
Gossypiboma is under reported and the true incidence is largely unknown. Depending on the body reaction and the characters of the retained sponge, the patient may present within months to years after surgery. Risk factors for retained foreign objects include emergency surgery, an unplanned change in the surgical procedure, higher body mass index, multiple surgical teams, greater number of major procedures done at the same time and incorrect count recording. The surgical procedure needed to extract the retained sponge may be a simple one, as in the first case, or it may be more complex, as seen in the other two cases. Although holding the correct count at the end of surgery is the gold standard safeguard against this mishap, human errors continue to occur, as happened in our patients. For that reason, the correct count should be supplemented by employing one of the several new technologies currently available.
Conclusion
Gossypiboma continues to occur, despite precautionary measures. As its consequences might cost the patient his life and the surgeon his professional reputation, extra preventive measures should be sought and implemented. New advances in technology should be incorporated in the theatre protocol as additional safeguard against human error. When encountered, a direct incision over the encapsulated swelling, in contrast to a formal laparotomy incision, might simplify the surgical procedure.
1. Introduction
Retained foreign object (RFO) is a collective term used to describe any object left unintentionally in the body, at the end of a surgical or other interventional procedure. Surgical sponges form the majority of such RFO with a rate of 68% [1]. Although not precise, gossypiboma is the commonest term used to refer to this condition, and other terms also exist.
2. Case report
2.1. First patient
A female patient, aged 39 years, was referred to the general surgeon, 18 days after an elective caesarean hysterectomy for placenta previa increta. As per the gynaecologist report, the procedure was difficult and bloody, necessitating the utilization of multiple abdominal pads.
Her recent history included abdominal pain, constipation, vomiting and upper respiratory tract infection.
On examination, she looked relatively well. Her pulse was 105/min, blood pressure 113/75 mmHg, temperature 37 °C, and O2 saturation was 98%.
Abdominal examination revealed a soft abdomen with a non tender, firm, 10 × 10 cm globular mass in the right upper quadrant.
Her blood count as well as her liver and renal function tests were within normal.
Abdominal X ray showed multiple air/fluid levels, and ultrasound (US)/computerized axial tomography (CT) scans of the abdomen showed a circumscribed, encapsulated mass in the right upper quadrant, with interspersed gas bubbles (Fig. 1).
Fig. 1.

CT scan of the abdomen showing a spongiform circumscribed encapsulated mass (red arrow) in the right upper quadrant with a radio opaque marker.
After initial preparation with intravenous fluids and antibiotics, minilaparotomy was performed utilizing a short incision directly over the swelling. The abdominal muscles were divided and the peritoneum was opened. The encapsulation surrounding the pad was then encountered and opened and the pad was slowly and gently extricated from the surrounding adhesions (Fig. 2). Saline irrigation and suction of the resultant cavity were done several times, and the wound was closed in layers around a tube drain.
Fig. 2.
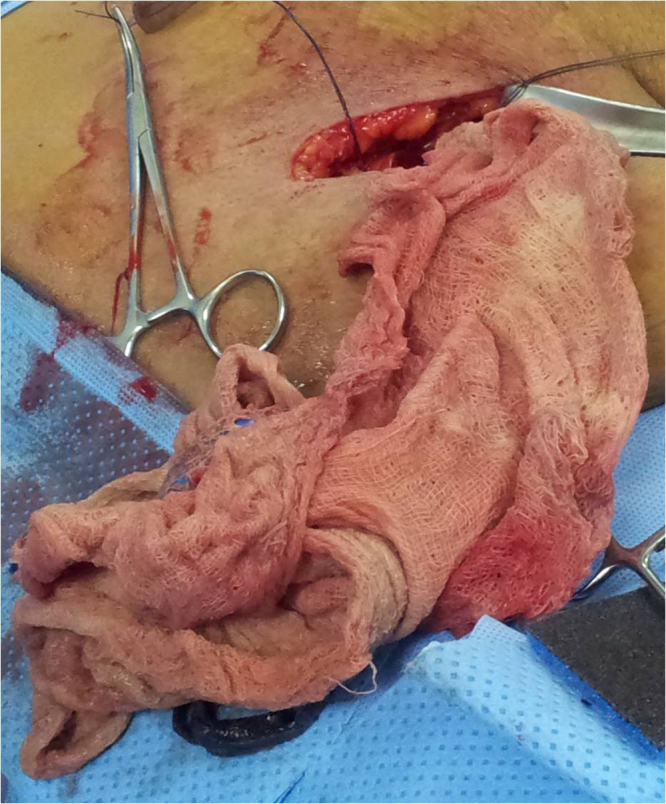
The missed abdominal pad extracted through a direct incision over the swelling.
The patient tolerated surgery well and was discharged on the second post operative day, when she tolerated diet and a checkup X ray showed disappearance of the fluid levels.
One week after surgery, she appeared in the outpatient clinic in good health, and a checkup abdominal US showed minimal residual fluid between bowel loops. In her last followup visit three weeks later, the patient remained well.
When the incidence was investigated, it was discovered that, a commercially available special sponge, which promotes haemostasis when applied to bleeding surfaces, was utilized in the procedure. This sponge when removed, was mistakenly added to the regular sponge count, replacing a regular sponge which was thus left behind. Aiding this mishap to occur, was a change in the nursing staff in the middle of the procedure.
2.2. Second patient
A 46-year-old female, with past history of a previous Caesarean section, underwent a second Caesarean section in November 2003, for obstructed labour. During surgery, extension of the uterine wound into the upper two thirds of right lateral vaginal wall occurred. As the repair was difficult due to vaginal wall oedema and to control the situation, hysterectomy was performed. Blood oozing continued, four units of blood were given and pelvic packing, using five laparotomy pads, was necessary. All the packs were removed 24 h later, and the count was correct at the end of the procedure. The post operative recovery was uneventful, and the patient was discharged in good condition.
On November 2012, nine years after her Caesarean hysterectomy, the patient presented with abdominal pain. Apart from raised white blood count (13.000/μl, reference range 4.000–10.000) and mild elevation of blood glucose and lipid profile levels, her liver and renal functions were within normal. Abdominal US/CT scans showed a large pelvic cyst 13 × 18 cm in diameter, with a smaller cyst to its left, suggestive of ovarian cysts. Another hypodense shadow with a mildly irregular and slightly enhancing wall was also noted in the right upper abdomen, compressing and displacing the surrounding bowel loops, with a very dense structure within it (Fig. 3, Fig. 4). A double pathology of gossypiboma and ovarian neoplasia was then considered. To this end, tumours markers CA 125, alpha feto protein and CEA were requested and came to be normal.
Fig. 3.
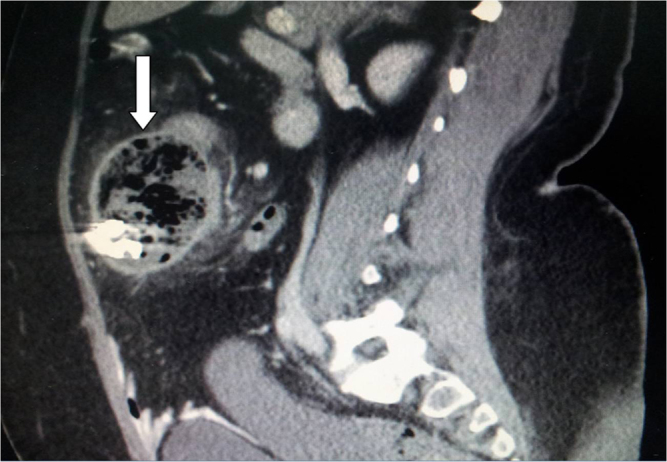
An encapsulated spongiform mass with a radio opaque marker (white arrow), suggestive or a laparotomy pad with its radio opaque ribbon.
Fig. 4.
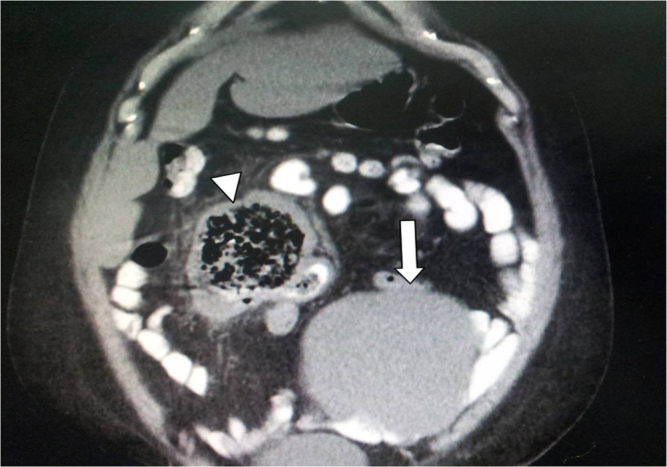
An encapsulated spongiform shadow (white arrow head) suggestive of gossypiboma, with a cystic swelling (white arrow), suggestive of ovarian cyst.
Laparotomy deemed necessary to deal with both lesions but, understandably, the patient refused surgery in our hospital and requested to be transferred to another facility. Later, we came to know that she underwent surgery, in which colonic resection was necessary (exact details are unknown). Shortly thereafter, the husband raised a legal; complaint.
A retrospective review of the patient’s file and operative notes, failed to discover any count discrepancy, contrasting the actual finding of a missed sponge inside the patient.
2.3. Third patient
A 35-year-old female with no past medical history, presented with severe central abdominal pain with nausea, repeated vomiting, fever and dysuria.
Two months prior to presentation, she underwent an elective Caesarean section, which was marked by intense post operative pain and persistent purulent wound discharge, for which she was readmitted to the maternity hospital for a week for wound management.
Her blood counts as well as biochemical investigations were within normal. Plain X ray of the abdomen revealed a foreign body in the left lower quadrant, suggestive of missed laparotomy pad. This was confirmed by CT of the abdomen which showed the characteristic spongiform features of a missed laparotomy pad in the left iliac fossa, associated with a small abscess cavity and evidence of small bowel obstruction (Fig. 5).
Fig. 5.

The characteristic radiologic spongiform feature of a missed laparotomy pad, with the radio opaque ribbon marker and surrounding capsule (red circle).
After a short period of preparation, an exploratory laparotomy was performed through a midline incision. A big laparotomy pad was found in the left iliac fossa, with about 250 ml of thick yellowish pus collection. Marked adhesions were present between the towel and adjacent sigmoid colon and small bowel loops, causing obstruction with distension of the small bowel proximally. By gentle yet tedious dissection, the towel was freed from the adherent bowel loops (Fig. 6). At the end, saline irrigation and suction was performed and the abdomen was closed on suction drainage. Post operatively the patient tolerated surgery well and was discharged in good condition for followup. Again, a legal complaint was raised and the condition is still under investigation.
Fig. 6.

The pad while being extracted through the laparotomy wound.
3. Discussions
The term gossypiboma is widely thought to originate from two words: gossypium, or cotton in Latin, and boma meaning concealment place in Swahili. However, this may be incorrect as it is more plausible to consider that the word is derived from gossypium and oma, which is a suffix indicating tumour, as in carcinoma and lymphoma, with the “b” added to separate two vowels [2]. Other terms used to describe the condition are textiloma (from textile or woven fabrics) [3], cottonoid, cottonballoma, muslinoma (from muslin) [4] and gauzeoma [5]. As surgical sponges are made nowadays of different materials in addition to cotton, the word textiloma with its more collective meaning, may be more appropriate.
It is believed that gossypiboma is under reported owing to its medicolegal implications, in addition to its asymptomatic nature at times. The true incidence is largely unknown, and different estimates have been reported. Silva and Sousa estimated its incidence at 1:1000–1:1500 laparotomies [6], whereas Bani-Hani et al. estimate is much lower (1:5027) [7]. Depending on the body reaction as well as the characters of the retained sponge, the patient may present acutely, within months of the original surgery, or may have a delayed presentation years thereafter. In our first and third patients, the duration between surgery and presentation was only several weeks, while it was several years in the second patient. In this regard, the average time of presentation was found to be 6.9 years [8]. However, latency of up to 37 years has been reported [3], [9]. This highlights the fact that, some cases may go around undiscovered for years or may never be discovered. In our second patient with delayed presentation, it is not clear whether her pain originated from the large ovarian cyst or the missed sponge. However, the radiologic investigations performed to clarify the cause of pain led to the discovery of the missed sponge. It is likely that in the absence of the ovarian cyst, the missed sponge might have remained asymptomatic for further more years.
Although no part of the body is exempted, the abdominal cavity, followed by the pelvic and thoracic cavities are the regions most commonly involved [8], [10].
Risk factors for retained foreign objects include emergency surgery, an unplanned change in the surgical procedure, higher body mass index [11], multiple surgical teams, greater number of major procedures done at the same time and incorrect count recording [10].
The clinical features are varied. A palpable mass, pain and fever are the leading features [8], and suspicion of neoplasia may be raised [12] if there is no clue in the history. Adhesions, fistulization and abscess formation are the commonest complications [8] and bowel obstruction due to adhesions or, interestingly, migration of the gauze into the bowel lumen [12], [13], [14] has been reported. The sequels of the condition might be so grave as to cause the patient’s demises [13] or conversely, in about 6% of cases, it may remain asymptomatic [8].
Gossypiboma has certain characteristic radiologic features, facilitating a straightforward diagnosis. On plan X ray, the radio opaque marker attached to the sponge [15], may be easily detected, as in our cases, although it may not be as easily seen, if lies beneath a radiodense area or bone [16]. On US, it may be seen as a well demarcated mass with wavy internal echos, surrounded by a hypoechoic ring and exhibiting strong post acoustic shadows. On CT scan, which is the preferred modality, a spongiform mass containing gas bubbles or having a whorly appearance, is characteristic [16].
The surgical procedure needed to extricate the retained sponge from the surrounding adhesions, may be a simple one, as in the first case presented here, or it may be more complex, as seen in the other two cases. Moreover, it may entail bowel resection [17], as occurred in our second patient. In this regard and in the presence of radiologic evidence of encapsulation around the pad as was encountered in our cases (Figs. 1, 3–5), it might be advisable to put the incision directly over the palpable swelling, rather than performing a formal laparotomy incision. This approach might simplify the procedure by decreasing the magnitude of dissection needed to reach and extract the pad. On occasions, the erroneous diagnosis of malignancy, led to en block resection of the mass, with the related segments of small and large bowel [18]. Interestingly, gastroscopic removal of a large surgical sponge which migrated entirely into the stomach has been recently reported [14], as well as the spontaneous passage of the retained gauze through the rectum [7], [19].
Surgical count and its related procedures is a basic skill taught to every debutant operation theatre nurse. The standard counting protocol implies that two operation theatre nurses count all objects to be used in the procedure, at the start and once again at the end of the procedure. The initial count and the end count should be matched, confirming that all items have been retrieved and nothing is left behind. Whenever the count is reported as incorrect, it is the duty of the surgeon to perform a thorough methodological wound exploration, utilizing his visual as well as tactile senses, to find the missed item. If no such item is found, a high resolution X ray should be requested and ideally reported by a radiologist before ending the procedure. However, the intraoperative detection rate on plain radiograph has been estimated to be only 67% [1].
Holding the correct count at the end of surgery is the gold standard safeguard against this mishap. Unfortunately, human errors continue to occur and it has been reported that, a correct count has been declared at the end of the procedure in the majority of gossypiboma cases [7], [8] as in seen in our patients. It is also noteworthy that the three cases followed Caesarean section, a clear message to the gynaecologist to exert extra attention during this type of surgery.
Fortunately, advances in technology which help rectify human errors in counting, have been introduced and several methods are currently available. A radiofrequency device is being utilized in some theatres. By adding a radiofrequency tag to the surgical items, and scanning the surgical field with the device at the end of surgery, any retained item will be discovered and consequently removed. The utility of this system with its high sensitivity and specificity rates, has been approved [20], [21]. Another seemingly valuable method is the barcode sponge system, where a barcode is attached to each surgical sponge. A hand held barcode reader scans each item before it enters the operative field and once again when removed. This system is currently being utilized in several hospitals in the United States and has proved its efficiency, at the expense of a slightly increase cost of about seven dollars per case [22]. A third developing technology is the utilization of a tag made of a specialized magnetic metal, which emits, when demagnetizes, a radio wave that can be detected by a hand held detector [23]. Although these methods are promising, one should consider the likelihood of machine failure. For that reason, a combination of methods should be used to keep the failure rate at its minimum.
The sequels and repercussions of the incident affect the patient and surgeon alike, as the former will suffer the complications of the RFO as well as the required interventions to retrieve it, and the later will suffer the professional disgrace and ill fame. It is obvious that as the surgeon indulges in his surgical endeavour, especially during difficult and prolonged surgeries, events distracting his attention, other than holding the count, are many. At the end of surgery, the words “count is correct” pronounced by the scrub nurse sets the stage for closing the abdomen. In such cases, the surgeon should bear no blame if a missed item was discovered later. On the other side, the surgeon should take all the blame, if he was told about the incorrect count and despite that closes the wound, without taking all possible measures to verify the situation. In this regard, having a high resolution X ray film of the operation site, in the immediate post operative period and before the patient leaves the operation suite, detected RFO in some procedures despite a correct count [1].
After reviewing the literature, the following recommendations may seem appropriate to decrease the incidence of RFO to a minimum, if not to abolish it:
-
1.
Scrupulous surgical counting should be held as dictated by the governing hospital protocol.
-
2.
A new count should be performed whenever there is change in the surgical team or the intended procedure.
-
3.
Using small sized pads and sponges, as 4 × 4 gauze, should be avoided if the operative field is sizable, as they can easily lodge between the tissues and bowel loops and stain with blood, making their identification difficult.
-
4.
A high resolution X ray of the operative field should be obtained, before the patient leaves the operation suite in all except the simplest cases.
-
5.
Incorporating the new technology in the theatre protocol to help rectify human errors should be prompted.
4. Conclusion
Gossypiboma, or better textiloma, continues to occur, despite precautionary measures. As its consequences might cost the patient his life and the surgeon his professional reputation, extra preventive measures should be sought and implemented. New advances in technology should be incorporated in the theatre protocol as additional safeguard against human error. When encountered, a direct incision over the encapsulated swelling, in contrast to a formal laparotomy incision, might simplify the surgical procedure.
Conflict of interest
The authors declare no conflict of interest.
Funding
No funds were needed for this report.
Ethical approval
This research paper has been approved by the medical ethics committee, AFHSR.
Consent
Patients gave their consent for this research.
Author contribution
All authors agreed on the basic concepts in the paper.All authors provided clinical care for their respective patients.M. Ezzedien Rabie, Mohammad Hassan Hosni and Fadel Hussain Ghaleb collected the data.M. Ezzedien Rabie, Mohammad Hassan Hosni, Alaa Al Safty analysed the data.M. Ezzedien Rabie wrote the manuscript.All authors reviewed the manuscript and approved its final form.
Guarantor
The authors of the paper are the guarantors.
References
- 1.Cima R.R., Kollengode A., Garnatz J., Storsveen A., Weisbrod C., Deschamps C. Incidence and characteristics of potential and actual retained foreign object events in surgical patients. J. Am. Coll. Surg. 2008;207(1):80–87. doi: 10.1016/j.jamcollsurg.2007.12.047. [DOI] [PubMed] [Google Scholar]
- 2.http://www.worldwidewords.org/weirdwords/ww-gos1.htm.
- 3.Soares F.V., Vicentini L., Dell’Aringa A.R., e Silva L.C. Textiloma in abdominal cavity: 35 years later. Arq. Bras. Cir. Dig. 2013;26(January–March (1)):74–75. doi: 10.1590/s0102-67202013000100018. [DOI] [PubMed] [Google Scholar]
- 4.Yoon M.A., Kim E., Kwon B.J., Kim J.E., Kang H.S., Park J.H., Sohn C.H., Kim J.H., Lee D.H. Muslinoma and muslin-induced foreign body inflammatory reactions after surgical clipping and wrapping for intracranial aneurysms: imaging findings and clinical features. J. Neurosurg. 2010;112(March (3)):640–647. doi: 10.3171/2009.7.JNS081625. [DOI] [PubMed] [Google Scholar]
- 5.Kawahara S., Honda M., Kosuda S., Tamura K., Miwa K., Hashimoto T., Nobusawa H., Satoh S., Ootsuki N., Gokan T. CT and US findings of gauzeoma. Nihon Igaku Hoshasen Gakkai Zasshi. 1990;50(April (4)):375–381. [PubMed] [Google Scholar]
- 6.Silva S.M., Sousa J.B. Gossypiboma after abdominal surgery is a challenging clinical problem and a serious medicolegal issue. Arq. Bras. Cir. Dig. 2013;26(June (2)):140–143. doi: 10.1590/s0102-67202013000200015. PMID: 24000029. [DOI] [PubMed] [Google Scholar]
- 7.Bani-Hani K.E., Gharaibeh K.A., Yaghan R.J. Retained surgical sponges (gossypiboma) Asian J. Surg. 2005;28(April (2)):109–115. doi: 10.1016/s1015-9584(09)60273-6. [DOI] [PubMed] [Google Scholar]
- 8.Wan W., Le T., Riskin L., Macario A. Improving safety in the operating room: a systematic literature review of retained surgical sponges. Curr. Opin. Anaesthesiol. 2009;22(April (2)):207–214. doi: 10.1097/ACO.0b013e328324f82d. [DOI] [PubMed] [Google Scholar]
- 9.Cattaneo F., Graffeo M., Brunetti E. Extrahepatic textiloma long misdiagnosed as calcified echinococcal cyst. Case Rep. Gastrointest. Med. 2013;2013:261685. doi: 10.1155/2013/261685. Epub 2013 Feb 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lincourt A.E., Harrell A., Cristiano J., Sechrist C., Kercher K., Heniford B.T. Retained foreign bodies after surgery. J. Surg. Res. 2007;138(April (2)):170–174. doi: 10.1016/j.jss.2006.08.001. Epub 2007 Feb 1. [DOI] [PubMed] [Google Scholar]
- 11.Gawande A.A., Studdert D.M., Orav E.J., Brennan T.A., Zinner M.J. Risk factors for retained instruments and sponges after surgery. N. Engl. J. Med. 2003;348(January (3)):229–235. doi: 10.1056/NEJMsa021721. [DOI] [PubMed] [Google Scholar]
- 12.Akbulut S., Arikanoglu Z., Yagmur Y., Basbug M. Gossypibomas mimicking a splenic hydatid cyst and ileal tumor: a case report and literature review. J. Gastrointest. Surg. 2011;15(November (11)):2101–2107. doi: 10.1007/s11605-011-1592-9. Epub 2011 Jul 14. [DOI] [PubMed] [Google Scholar]
- 13.Biswas R.S., Ganguly S., Saha M.L., Saha S., Mukherjee S., Ayaz A. Gossypiboma and surgeon–current medicolegal aspect–a review. Indian J. Surg. 2012;74(4):318–322. doi: 10.1007/s12262-012-0446-3. Epub 2012 Mar 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sozutek A., Yormaz S., Kupeli H., Saban B. Transgastric migration of gossypiboma remedied with endoscopic removal: a case report. BMC Res. Notes. 2013;6(October (1)):413. doi: 10.1186/1756-0500-6-413. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whang G., Mogel G.T., Tsai J., Palme S.L. Left behind unintentionally retained surgically placed foreign bodies and how to reduce their incidence—pictorial review. AJR. 2009;193:S79–S89. doi: 10.2214/AJR.09.7153. 0361–803X/09/1936–S7. [DOI] [PubMed] [Google Scholar]
- 16.Manzella A., Filho P.B., Albuquerque E., Farias F., Kaercher J. Imaging of gossypibomas: pictorial review. AJR Am. J. Roentgenol. 2009;193(December (Suppl. 6)):S94–101. doi: 10.2214/AJR.07.7132. [DOI] [PubMed] [Google Scholar]
- 17.Gencosmanoglu R., Inceoglu R. An unusual cause of small bowel obstruction: gossypiboma-case report. BMC Surg. 2003;8(3):6. doi: 10.1186/1471-2482-3-6. http://www.biomedcentral.com/1471-2482/3/6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zbar A.P., Agrawal A., Saeed I.T., Utidjian M.R. Gossypiboma revisited: a case report and review of the literature. J. R. Coll. Surg. Edinb. 1998;43(December (6)):417–418. [PubMed] [Google Scholar]
- 19.Alis H., Soylu A., Dolay K., Kalayci M., Ciltas A. Surgical intervention may not always be required in gossypiboma with intraluminal migration. World J. Gastroenterol. 2007;13(December (48)):6605–6607. doi: 10.3748/wjg.v13.i48.6605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Steelman V.M., Alasagheirin M.H. Assessment of radiofrequency device sensitivity for the detection of retained surgical sponges in patients with morbid obesity. Arch. Surg. 2012;147(October (10)):955–960. doi: 10.1001/archsurg.2012.1556. [DOI] [PubMed] [Google Scholar]
- 21.Macario A., Morris D., Morris S. Initial clinical evaluation of a handheld device for detecting retained surgical gauze sponges using radiofrequency identification technology. Arch. Surg. 2006;141(July (7)):659–662. doi: 10.1001/archsurg.141.7.659. [DOI] [PubMed] [Google Scholar]
- 22.Greenberg C.C., Diaz-Flores R., Lipsitz S.R., Regenbogen S.E., Mulholland L., Mearn F., Rao S., Toidze T., Gawande A.A. Bar-coding surgical sponges to improve safety: a randomized controlled trial. Ann. Surg. 2008;247(April (4)):612–616. doi: 10.1097/SLA.0b013e3181656cd5. [DOI] [PubMed] [Google Scholar]
- 23.http://www.magtecinc.com/.


