Highlights
-
•
De Garengeot hernia is a rare type of femoral hernia that involves an appendix within the hernia sac.
-
•
Diagnosis is clinically difficult. Imaging may assist in pre-operative diagnosis.
-
•
There are various surgical methods in the approach to repair of femoral hernia. A recently published surgical method is described in this report.
Keywords: Hernia, De Garengeot, Femoral, Inguinal, McEvedy, Lothiessen, Lockwood
Abstract
Introduction
De Garengeot hernia is a rare type of femoral hernia, defined as a sac containing a vermiform appendix. Due to its rare occurrence the information available on diagnosis and management is scarce. We report the use of a recently described technique for femoral hernia repair and appendicectomy.
Presentation of case
A 67 year old female presented to the emergency department with features of incarcerated femoral hernia. CT imaging revealed an incarcerated appendix within a femoral hernia. The patient subsequently underwent surgery, where the femoral hernia was repaired and appendicectomy performed concurrently.
Discussion
Clinical diagnosis is difficult, and there have only been a few documented cases of pre-operative CT diagnoses in the literature. The usual risk factors for developing a hernia would apply to this pathology, and other anatomical and embryological considerations are explored. The King’s College technique for femoral hernia repair involves an incision that allows repair of the hernia and also the ability to enter the peritoneal cavity using the same incision. This approach was used in this case, where the abdominal cavity had to be entered to perform the appendicectomy, before the femoral hernia could be repaired.
Conclusion
Pre-operative diagnosis of De Garengeot hernia is difficult, as it may mimic an incarcerated femoral hernia containing other contents. The diagnosis becomes apparent intra-operatively. The clinical significance lies in that intra-abdominal access may be required to safely perform an appendicectomy before the repair of the hernia defect, and this article includes a description of a suitable technique for this particular pathology.
1. Introduction
A femoral hernia is defined as a sac which projects through the femoral canal, and presents clinically as a groin hernia below and lateral to the pubic tubercle, or a finger breadth medial to the femoral artery below the inguinal ligament [1]. Femoral hernias are relatively uncommon, and have a high risk of strangulation [1], [2].
This article presents a rare case of appendicitis within a De Garengeot hernia, which is described as an appendix which has migrated within the femoral hernia sac [3]. There has been fewer than 100 cases reported in the literature [2], [3], [4]. Pre-operative diagnosis of De Garengeot hernia is very difficult due to its rare occurence, non-specific history and clinical findings, and a paucity of data on the utility of diagnostic imaging [5].
Due to its rare occurrence and lack of published guidelines on standard management [3], this report attempts to add further insight into the disease entity, and highlights the use of a recently described surgical technique which has not previously been employed for use in repair of this hernia. Also included in this report is a descriptive computed tomography (CT) finding of femoral hernia appendicitis, which is one of a very few cases to be reported in the literature with a pre-operative CT diagnosis.
2. Case presentation
A 67 year old female presented to the emergency department with a 1 day history of increasing pain in a pre-existing lump in the right groin. This lump became apparent to the patient 4 days before the onset of pain. She describes having an upper respiratory tract infection for 2 weeks prior, and the persistence of a cough led to the development of this groin lump. There was no history of nausea or vomiting. She had regular bowel motions and was passing flatus. No other significant medical history or surgery in the past. On examination there were no documented fevers, and she was haemodynamically stable. Her abdomen was non-tender, soft and without distention. Below the inguinal ligament, identified by palpating the pubic tubercle, was a 4 cm firm, tender, and irreducible lump. This was associated with erythema of the skin over the lump. The biochemical profile and inflammatory markers were normal. The primary care physician had organised a CT scan prior to presentation to hospital. This demonstrated a right sided femoral hernia containing an appendix, with the tip appearing thickened and surrounded by fat stranding, suggestive of inflammation (Fig. 1, Fig. 2).
Fig. 1.

Tip of appendix within the femoral hernia sac (white arrow) with some surrounding fat stranding.
Fig. 2.
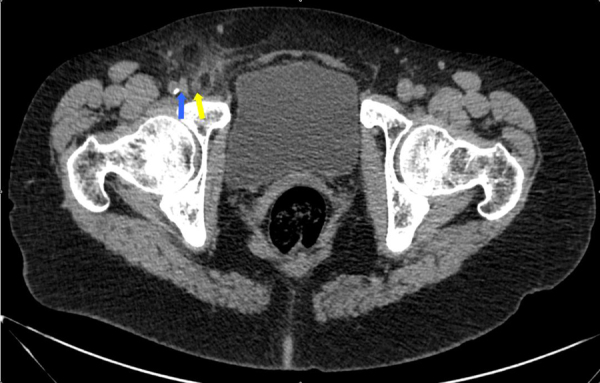
Fluid-filled tubular structure representing the appendix (yellow arrow) lying medially to the femoral vein (blue arrow), just before entering the femoral canal.
The patient was consented for emergency surgery the same day. The surgical method used was the King’s College approach described by Sorelli et al., a recently published method described as a single skin incision which is made one centimeter above the medial half of the inguinal ligament [6]. A femoral hernia sac was identified. Within the sac contained a strangulated dusky appearing tip of appendix, surrounded by blood-stained fluid (Fig. 3). Given the tightness of the hernia neck, the full length of the appendix could not be delivered. The nature of the surgical approach allowed entry into the peritoneum through the same skin incision, the caecum was identified and the appendix was safely delivered for routine open appendicectomy. The hernia was repaired by approximating the pectineal ligament to the inguinal ligament with 2–0 prolene sutures. The patient was discharged on post-operative day 2 without complication. The surgical specimen was confirmed histologically to be appendicitis.
Fig. 3.
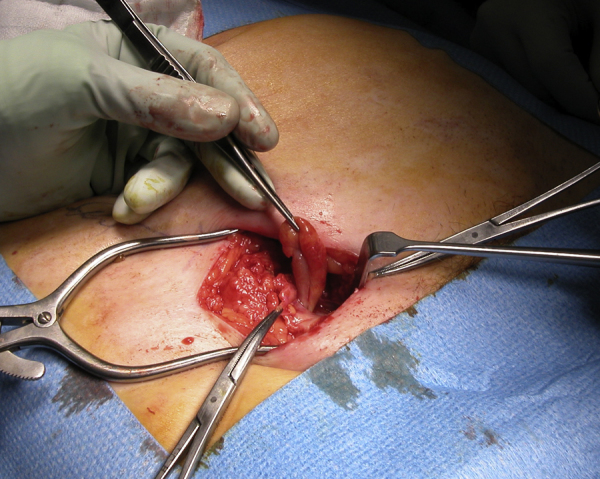
Strangulated portion of appendix incarcerated in the femoral hernia. This represented approximately 30% of the total length of the appendix.
3. Discussion
3.1. Incidence
De Garengeot hernia is defined as a femoral hernia which contains a vermiform appendix. It was first described in 1731 by a Parisian surgeon Rene Jacques Croissant De Garengeot [7]. This entity is extremely rare—reported incidence ranges from 0.8 to 1.0%, with the finding of appendicitis even rarer still, at 0.08–0.5% of all femoral herniae [3]. There has been fewer than 100 cases reported [2], [3], [4]. It must be distinguished from Amyand hernia, which is the presence of an appendix within an inguinal hernia, and is reportedly more common than a De Garengeot hernia [3], [5].
The importance of femoral hernias lies in the high strangulation risk, which is estimated to be 20% at 3 months and 45% at 21 months. This is in contrast to inguinal hernias, which have a risk of strangulation of 3% at 3 months, with a modest increase to 4.5% at 21 months [1]. This increased risk is thought to be due to the narrow and rigid ring attributed by the nature of the anatomy of the femoral canal [2]. A study examining a national hernia register in Sweden found that an emergency femoral hernia operation was associated with a 10 times increase in risk of mortality, with 63% of cases occurring in women [8].
3.2. Pathophysiology
There is a predisposition for postmenopausal females, being four times more common than males [3], [5], reflecting the higher incidence of femoral hernias in females [1]. Contributing factors are thought to be secondary to pregnancy related changes, as well as general factors that increase risk of hernia formation such as increased intra-abdominal pressure, smoking, connective tissue disorders, and older age [3], [5]. There have been several theories proposed to the pathogenesis of the migration of appendix into a femoral hernia. One hypothesis is the presence of a large or over-riding caecum within the pelvis may push the appendix onto the femoral ring [5], [9]. Another thought is that variable anatomic rotation of bowel during development may also play a role [5], [10], [11], as well as a variably mobile caecum which may also predispose to migration of appendix into the femoral canal [5], [9].
Appendicitis may have arisen from intraluminal obstruction caused by the tight neck of the hernia that caused external compression of the appendix, with eventual strangulation and inflammation [12]. This is supported by the fact that the patient had an asymptomatic lump for 4 days before the onset of pain. However, not all De Garengeot hernia will have appendicitis [5], and it is unclear whether the true mechanism always occurs from external compression, or can also arise from intraluminal obstruction, as in cases of wider hernia necks [3], [13].
3.3. Clinical features and diagnosis
The pre-operative diagnosis of De Garengeot hernia is very difficult, due to non-specific clinical findings and lack of comprehensive published data on diagnostic imaging. A recent article reviewing the literature found that most patients had a non-specific painful lump that was tender to palpation with or without sepsis. The clinical picture is generally indistinguishable from that of an incarcerated femoral or inguinal hernia, and features of bowel obstruction have also been reported [3], [5], [10]. The nature of the anatomy of the femoral canal limits the spread of intraperitoneal infection, and patients are more likely to present with local signs of tenderness and erythema rather than general intra-abdominal signs of peritonitis [13], [14]. Documentation of acute appendicitis within a femoral hernia by CT is also extremely rare. There has only been 4 other reported cases of CT detected appendicitis within a femoral hernia [2], [5]. In this case, the patient’s primary care physician had organised a CT to further investigate the lump, which revealed the presence of a tubular structure within the femoral hernia sac in continuity with a low-lying caecum, associated with fat-stranding surrounding the portion of appendix within the hernia. Ultrasound scans have also been utilised in several cases, however there has only been one documented case of a positive ultrasound diagnosis, found as a tubular blind-ending structure adjacent to the femoral vein [5], [15].
Complications of untreated symptomatic De Garengeot hernia may lead to necrosis of hernia contents with perforation and sepsis or abscess formation [13], development of bowel obstruction [10], and even necrotising fasciitis [5], [16]. In the case of a misdiagnosed De Garengeot hernia as an abscess and subsequent surgical drainage, an appendico-cutaneous fistula formation has been reported in the literature, which after persisting for a further 2 years eventually required a definitive excision of fistula tract, appendicectomy and femoral hernia repair [13]. These complications highlight the perils of misdiagnosis leading to inappropriate or delayed management. Surgical repair of the femoral hernia and appendicectomy has been the mainstay of management in the reported literature. There is no standardised method of surgical management of this rare condition, with various approaches being described [5]. It has been recommended by some authors that surgical approach should be based on clinical judgement and the condition of the patient [17].
3.4. Surgical management
Surgery is the mainstay of treatment of an acutely presenting femoral hernia. Lockwood’s infra-inguinal, Lotheissen’s trans-inguinal, and McEvedy’s high incisions are the classically taught surgical approaches [6]. Sorelli et al. proposed a technique which utilises a single skin incision to allow all the previously described approaches to the hernia sac, as well as gain entry into peritoneum [6]. As they have described, in this case the author made the incision 1 cm above the medial half of the ligament. Dissection was carried down to the external oblique aponeurosis and creation of superior and inferior flaps made possible adequate views to differentiate between inguinal and femoral hernia. A femoral hernia sac was identified, and within it contained a strangulated and inflamed appendix. The base of the appendix could not be accessed safely through the hernia orifice, so peritoneal entry was gained by creating a plane just superficial to the external oblique. The linea semilunaris is then divided lateral to the rectus, 4 cm above the inguinal ligament in order to allow preservation of the inguinal canal. This allowed exposure of the rectus muscle, which is retracted medially, and the transversalis fascia and peritoneum incised to gain entry into the peritoneum. Appendicectomy was performed in routine fashion, and the hernia orifice closed with 2–0 prolene sutures.
The advantage of the King’s College approach is that both femoral and inguinal hernias can be repaired, and the abdominal cavity also accessed all via the same single incision. Access to peritoneal cavity is of particular importance in cases of strangulated small bowel, and in this case, an incarcerated appendix which appendicectomy had not been possible without entering the abdominal cavity. Previously described case reports had similar problems with inaccessible base of appendix, and some authors have opted to make a second Lanz incision to perform the appendicectomy [3] or laparotomy [14]. In a previous review, most surgeons opted for the inguinal approach, some converted from laparoscopic to standard oblique inguinal, and another case describes repair by the McEvedy approach [5].
The proponents of the King’s College method report that their technique will minimise the pre-operative debate on choosing the best approach to femoral hernias in general and hope to achieve a standard [6]. Indeed this case is the first report to the Author’s knowledge to describe a successful repair of an incarcerated femoral hernia containing an appendix, gaining access into the peritoneum and performing an appendicectomy at the same time using this particular surgical approach.
4. Conclusion
De Garengeot hernia is a rare type of femoral hernia. Misdiagnosis leading to inappropriate or delayed treatment has resulted in some serious complications. This type of hernia typically presents in post-menopausal females. There have been various methods of repair described, however there is no standard recommended surgical repair for this condition. Pre-operative diagnosis is extremely difficult, and the cause usually becomes apparent intra-operatively. Given the rarity of this condition, De Garengeot hernia may not be readily suspected as a pre-operative diagnosis in a patient presenting with a tender groin lump. The clinical significance lies in that intra-abdominal access may be required to safely perform an appendicectomy before the repair of the hernia defect. This article aims to highlight the presentation of a patient with a femoral hernia appendicitis, to improve awareness of this entity, and to describe one method of repair should one encounter this pathology.
Conflict of interest
None.
Funding
None.
Ethical approval
None.
Author’s contribution
Ryo Mizumoto—first and corresponding author.
Rasika Hendahewa—secondary author, editor, supervisor.
Gamini Premaratne—contributor and supervisor.
Guarantor
Gamini Premaratne.
References
- 1.Hair A., O’Dwyer P., Paterson C. Diagnosis of a femoral hernia in the elective setting. J. R. Coll. Surg. Edinb. 2001;46(2):117. [PubMed] [Google Scholar]
- 2.Talini C.O., Ocaña L., César Faria Araújo A., Antonio Campelo Spencer Netto F., Pereira Westphalen A. De Garengeot hernia: case report and review. Int. J. Surg. Case Rep. 2015;8:35–37. doi: 10.1016/j.ijscr.2014.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akbari K., Claire W., Hammad A., Middleton S. De Garengeot’s hernia: our experience of three cases and literature review. BMJ Case Rep. 2014. 2014 doi: 10.1136/bcr-2014-205031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allen B.C., Kirsch J., Szomstein S. Case 187: De Garengeot hernia1. Radiology. 2012;265:640–644. doi: 10.1148/radiol.12102051. [DOI] [PubMed] [Google Scholar]
- 5.Kalles V., Mekres A., Mekras D., Papapanagiotou I., Al-Harethee W., Sotiropoulos G., Liakou P., Kastania A., Piperos T., Mariolis-Sapsakos T. De Garengeot’s hernia: a comprehensive review. Hernia. 2013;17(2):177–182. doi: 10.1007/s10029-012-0993-3. [DOI] [PubMed] [Google Scholar]
- 6.Sorelli P.G., El-Masry N.S., Garrett W.V. Open femoral hernia repair: one skin incision for all World. J. Emerg. Surg. 2009;4(1) doi: 10.1186/1749-7922-4-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.P. Huart, Traite des operations de chirurgie, De Garengeot RJC, 2nd edn., Paris, France, 369–371, 1731.
- 8.Dahlstrand U., Wollert S., Nordin P., Sandblom G., Gunnarsson U. Emergency femoral hernia repair: a study based on a national register. Ann. Surg. 2009;249(4):672. doi: 10.1097/SLA.0b013e31819ed943. [DOI] [PubMed] [Google Scholar]
- 9.Zissin R., Brautbar O., Shapiro-Feinberg M. CT diagnosis of acute appendicitis in a femoral hernia. Br. J. Radiol. 2000;73(873) doi: 10.1259/bjr.73.873.11064659. [DOI] [PubMed] [Google Scholar]
- 10.Wyatt J.P., Varma J.S. Femoral hernia appendix causing small intestinal obstruction. J. Postgrad. Med. 1992;68(797):223–224. doi: 10.1136/pgmj.68.797.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salkade P.R., Chung A.Y.F., Law Y.M. De Garengeot’s hernia: an unusual right groin mass due to acute appendicitis in an incarcerated femoral hernia. Hong Kong Med. J. 2012;18(5):442. [PubMed] [Google Scholar]
- 12.Nguyen E.T.K., Ian K. Strangulated femoral hernia containing a perforated appendix. Can. J. Surg. 2004;47(1):68–69. [PMC free article] [PubMed] [Google Scholar]
- 13.Voitk A.J., MacFarlane J.K., Estrada R.L. Ruptured appendicitis in femoral hernias: report of two cases and review of the literature. Ann. Surg. 1974;179(1):24–26. doi: 10.1097/00000658-197401000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shah A., Janardhan H.S. De Garengeot hernia: a case report and review of literature. Indian J. Surg. 2013;75(S1):439–441. doi: 10.1007/s12262-012-0778-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Filatov J., Ilibitzki A., Davidovitch S., Soudack M. Appendicitis within a femoral hernia: sonographic appearance. J. Ultrasound Med. 2006;25(9):1233. doi: 10.7863/jum.2006.25.9.1233. [DOI] [PubMed] [Google Scholar]
- 16.Guirguis E.M., Taylor G.A., Chadwick C.D. Femoral appendicitis: an unusual case. Can. J. Surg. 1989;32(5) [PubMed] [Google Scholar]
- 17.Moris D., Vernadakis S. De Garengeot’s hernia. Am. Surg. 2013;79(11):318–319. [PubMed] [Google Scholar]


