Highlights
-
•
Pericardio-diaphragmatic should be suspected in high-velocity blunt thoraco-abdominal trauma.
-
•
Pericardial rupture can be managed in an open or laparoscopic approach.
Keywords: Pericardium, Diaphram, Rupture, Trauma
Abstract
Introduction
Traumatic diaphragmatic rupture (TDR) occurs in 0–5% of patients with major blunt thoraco-abdominal trauma, in most of them on the left side, and an early correct diagnosis is made in less than half of the cases (Meyers and McCabe, 1993; Ball et al., 1982).
Presentation of the case
We report a case of a forty-eight years old man who had a pericardio-diaphragmatic rupture after a high-velocity blunt abdominal trauma that was diagnosed and treated successfully.
Discussion
Pericardio-diaphragmatic rupture (PDR) is an uncommon problem that poses a diagnostic challenge to surgeons. The incidence of PDR is between 0.2% and 3.3% of cases with TDR (Sharma, 1999 [3]).
Conclusion
PDR should be suspected in any patient with high velocity thoraco-abdominal trauma. Early diagnosis is essential and needs a high index of suspicion. Early Management is important in decreasing morbidity and mortality.
1. Introduction
Traumatic diaphragmatic rupture (TDR) occurs in 0–5% of patients with major blunt thoraco-abdominal trauma, in most of them on the left side, and an early correct diagnosis is made in less than half of the cases [1], [2]. Pericardio-diaphragmatic rupture (PDR) is an uncommon problem that poses a diagnostic challenge to surgeons. The incidence of PDR is between 0.2% and 3.3% of cases with TDR [3]. We report a case of a forty-eight years old man who had a pericardio-diaphragmatic rupture after a high-velocity blunt abdominal trauma that was diagnosed and treated successfully. Early diagnosis and treatment are essential in decreasing the morbidity and mortality.
2. Case report
A 48-year-old male of Asian origin was brought by ambulance to the accident and emergency department after a history of fall from seven meters height (witnessed fall). On presentation, the patient was conscious and oriented with a GCS 14/15. He was complaining of severe abdominal pain and respiratory distress. There was an evidence of multiple body abrasions mainly on the abdomen. Hemodynamically, he was unstable with systolic blood pressure 90/43 mmHg, pulse rate (P = 100 bpm) & a respiratory rate (RR = 22/min). The Patient was resuscitated according to ATLS and hospital protocols. Chest examination revealed absent breath sounds on the right side, and pneumothorax was confirmed by extended FAST. Right sided intercostal drain was inserted and the vital signs of the patient improved. Then the patient was shifted to the radiology department where a CT scan was done and showed pneumomediastinum with a remnant right sided pneumothorax (Fig. 1, Fig. 2), so another chest tube was inserted on the right side, and a provisional diagnosis of post-traumatic diaphragmatic hernia was made and the patient was shifted to the operating theatre.
Fig. 1.
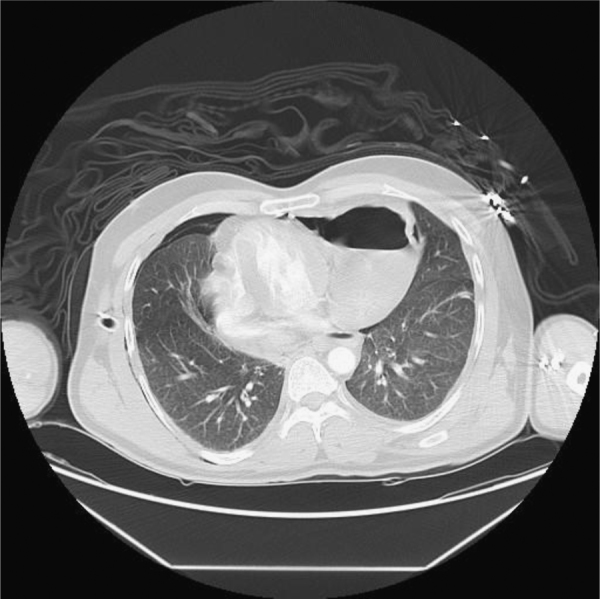
CT scan of the chest- cross-sectional view showing pneumothorax and air-fluid level in the chest suspecting diaphragmatic hernia or diaphragmatic rupture.
Fig. 2.

CT scan of the chest- coronal view showing pneumothorax, pneumo-mediastinum and air-fluid level in the chest suspecting diaphragmatic hernia or diaphragmatic rupture.
Diagnostic laparoscopy was done and showed a big left diaphragmatic injury around 15 cm with a big pericardial sac defect exposing the pumping heart and containing part of the stomach and the omentum. A retroperitoneal hematoma was noticed as well extending from the pelvis to the root of mesentery.
The procedure was converted to laparotomy; the stomach was pulled down and looked completely normal and healthy. A cardio-thoracic surgeon was consulted and placed a drain in the pericardial sac. Then the diaphragmatic defect was repaired using non-absorbable sutures in an interrupted pattern, the abdomen was explored again and was closed. The patient had a concomitant pelvic fracture that was managed by the trauma team.
Postoperatively, the patient remained for few days in the surgical ICU, and then was shifted successfully to a general ward. He had an eventful hospital recovery and was discharged home in a stable condition with an outpatient follow up.
3. Discussion
Pericardial rupture following blunt chest trauma is rare and is associated with high mortality rate ranging from 30% to 64% [4]. The first case report on a patient diagnosed with PDR preoperatively was published in 1951 and on average, only one case of PDR is published annually [5]. The rent in the pericardium might be situated in 3 regions, the diaphragmatic, superior mediastinal, and left or right pleuropericardial regions [6], [7]. In our case, the pericardial rent was in the diaphragmatic surface, exposing the heart but with no obvious injury. The stomach was herniated and stuck through this defect.
Many investigations have been described for diagnosis of TDR, including chest X-ray, CT scan, MRI, upper GI contrast study, USG, thoracoscopy and laparoscopy [8]. According to literature, initial radiographs allow diagnosis of 27–60% of left-sided and only 17% of right-sided injuries. The finding of bowel or stomach above the diaphragm with focal constriction at the site of injury is diagnostic of TDR [9]. The CT findings of diaphragmatic rupture include discontinuity of the diaphragm (gap sign), an abnormally thickened diaphragmatic crus, herniation of stomach, bowel or solid organs into the chest and the collar sign [9]. In patients with PDR, an abnormal air shadow in the cardiac area on chest X-ray or presence of an air fluid level anterior to the heart on lower chest CT scan is diagnostic [9]. In our case, PDR was suspected according to the above CT findings (Fig. 2) and was confirmed by diagnostic laparoscopy.
The recommended surgical approach in patients with acute left-sided TDR is laparatomy [10]. Thoracotomy is commonly used in delayed cases to safely separate adhesions between abdominal organs and the thoracic wall [10]. Isolated traumatic pericardial rupture can be treated by suturing of the pericardium. However, in the presence of associated diaphragmatic rupture, most authors prefer to treat pericardial injury with drain placement only [10].
4. Conclusion
PDR should be suspected in any patient with high velocity thoraco-abdominal trauma. Early diagnosis is essential and needs a high index of suspicion. Early Management is important in decreasing morbidity and mortality.
Conflict of interest
No conflict of interest is present.
Funding
No involvement of any funding to be mentioned.
Ethical approval
Approval obtained from local research committee. Approval was given by consenting the patient.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
Bassem Abou Hussein: Author.
Ali Khammas: Co-author.
Hadiel Kaiyasah: Co-author.
Abeer Swaleh: Discussion of the case.
Nazim Al Rifai: Discussion of the case.
Alya Al-Mazrouei: Contributor.
Faisal Badri: Contributor.
Guarantor
The corresponding author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive license (or non-exclusive for government employees) on a worldwide basis to permit this article (if accepted) to be published in the International Journal of Surgery Case Reports.
References
- 1.Meyers B.F., McCabe C.J. Traumatic diaphragmatic hernia: occult marker of serious injury. Ann. Surg. 1993;218:783–790. doi: 10.1097/00000658-199312000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ball T., McCrory R., Smith J.D., Clements J.L. Traumatic diaphragmatic hernia: errors in diagnosis. AJR. 1982;138:633–637. doi: 10.2214/ajr.138.4.633. [DOI] [PubMed] [Google Scholar]
- 3.Sharma O.P. Pericardio-diaphragmatic rupture: five new cases and literature review. J. Emerg. Med. 1999;17:963–968. doi: 10.1016/s0736-4679(99)00124-9. [DOI] [PubMed] [Google Scholar]
- 4.Fulda G., Rodriguea A., Turney S.Z., Cowley R.A. Blunt traumatic pericardial rupture. A ten-year ex-perience 1979 to 1989. J. Cardiovasc. Surg. 1990;31(4):525–530. [PubMed] [Google Scholar]
- 5.McCune R.P., Roda C.P., Eckert C. Rupture of diaphragm caused by blunt injury. J. Trauma. 1976;16:531–537. doi: 10.1097/00005373-197607000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Witkowski Z., Lasek J., Wujtewicz M. PDR and cardiac herniation after multiple blunt trauma: diagnostic and therapeutic difficulities. J. Thorac. Cardiovasc. Surg. 2005;130(6):9–10. doi: 10.1016/j.jtcvs.2005.07.054. [DOI] [PubMed] [Google Scholar]
- 7.Van Tornout F., Van Luven M., Parry W. Pericardio-diaphragmatic avulsion and concomitant rupture of central tendon of diaphragm. Eur. J. Cardiothorac. Surg. 2004;26:655–657. doi: 10.1016/j.ejcts.2004.05.038. [DOI] [PubMed] [Google Scholar]
- 8.Haeiibrahimglu G., Sotak O., Olemen A. Management of traumatic diaphragmatic rupture. Surg. Today. 2004;34:111–114. doi: 10.1007/s00595-003-2662-8. [DOI] [PubMed] [Google Scholar]
- 9.Mushtaque M., Younis M., Thoker M. Traumatic isolated pericardio-diaphragmatic rupture. Internet J. Surg. 2009;26(1) [Google Scholar]
- 10.Kutsal T., Ozer M., Alpaslan C. Traumatic diaphragmatic rupture: look to see. Eur. J. Cardiothorac. Surg. 2008;33:1082–1085. doi: 10.1016/j.ejcts.2008.01.029. [DOI] [PubMed] [Google Scholar]


