Abstract
There is controversy among neurosurgeons regarding whether irrigation or drainage is necessary for achieving a lower revision rate for the treatment of chronic subdural hematoma (CSDH) using burr-hole craniostomy (BHC). Therefore, we performed a meta-analysis of all available published reports. Multiple electronic health databases were searched to identify all studies published between 1989 and June 2012 that compared irrigation and drainage. Data were processed by using Review Manager 5.1.6. Effect sizes are expressed as pooled odds ratio (OR) estimates. Due to heterogeneity between studies, we used the random effect of the inverse variance weighted method to perform the meta-analysis. Thirteen published reports were selected for this meta-analysis. The comprehensive results indicated that there were no statistically significant differences in mortality or complication rates between drainage and no drainage (P > 0.05). Additionally, there were no differences in recurrence between irrigation and no irrigation (P > 0.05). However, the difference between drainage and no drainage in recurrence rate reached statistical significance (P < 0.01). The results from this meta-analysis suggest that burr-hole surgery with closed-system drainage can reduce the recurrence of CSDH; however, irrigation is not necessary for every patient.
Keywords: chronic subdural hematoma, burr-hole, irrigation, drainage, meta-analysis
Introduction
The annual estimated incidence of chronic subdural hematoma (CSDH) is 13.5 per 100,000 individuals per year. However, it is more common in the elderly population and may reach up to 58.1 and 74 per 100,000 persons for patients 65 years of age or older.1–3) Although CSDH can commonly be treated by neurosurgeons and is usually cured, recurrence has not been eliminated.
One decision analysis suggests that burr-hole craniostomy (BHC) is the most efficient choice for surgical drainage of uncomplicated CSDH because it balances low recurrence rates with a low incidence of highly-morbid complications.4) This study also used Monte Carlo simulations to compare three surgical approaches to BHC: (1) irrigation and a drain (+I+D), (2) an indwelling drain alone (–I+D), and (3) irrigation alone (+I–D). The results suggested a trend toward better outcomes when an indwelling drain was inserted unaccompanied by intraoperative irrigation; however, the differences were not significant.4)
No previous systematic review has compared the revision rates of intraoperative irrigation and postoperative drainage in BHC. There have been a few observational studies that compared recurrence rates of +I+D vs. –I+D or +I+D vs. +I–D in BHC for CSDH treatment.5–17) However, these studies have conflicting results. Postoperative CSDH recurrence requiring another operation is relatively infrequent, but it is a clinically significant complication after BHC.18) By providing a systematic review of the available published studies examining irrigation and drainage, we aim to provide neurosurgeons with an evidence-based guidance for the treatment of CSDH patients in an effort to eliminate the requirement of a second operation to evacuate recurrent or residual CSDH.
Methods
I. Search strategy
We searched multiple electronic health databases, including Pubmed, MEDLINE (OvidSP), EMBASE (OvidSP), the Cochrane Central Register of Controlled Trials, and the Cochrane Database of Systematic Reviews for all randomized and observational studies as well as any previous systematic reviews published between 1989 and June 2012 that compared the recurrence rate of CSDH after BHC with irrigation and a drain, an indwelling drain alone, or irrigation alone.
We used a keyword search mapped to subject headings (MeSH terms in MEDLINE and EMTREE Thesaurus in EMBASE), and these subject headings were “exploded” using advanced keyword searches to include all subtopics. We then included all subheadings of those terms to allow the widest capture of relevant studies. The terms used were chronic subdural hematoma and craniostomy.
For a more inclusive search, we used a text word search for the same keywords and for other terms not linked to subject headings (MeSH terms or EMTREE thesaurus).
Terms used in the text word search were chronic subdural hematoma, subdural hematoma, subdural hemorrhage, burr-hole, mini craniotomy, and craniotomy. After using each keyword separately in the above-mentioned databases, we combined keywords using the Boolean operator “OR” in two different concepts (chronic subdural hematoma and surgical treatment of CSDH). Next, we combined searches resulting from keywords of these two concepts using the Boolean operator “AND.” We also searched for relevant studies in the references listed in selected studies. The search was limited to studies published in English.
II. Study types
Any study (randomized, control trial, or observational) that compared the recurrence rates of CSDH after BHC with irrigation and a drain, an indwelling drain alone, or irrigation alone was considered. Studies that examined the CSDH recurrence rate after either irrigation or drainage in BHC without comparison to each other in the same population of patients were excluded.
III. Type of outcome measures
In this systemic review and meta-analysis, the outcome for each patient is categorical (whether the patient required another surgery to evacuate the CSDH). The outcomes for the studies were the number of patients who required revision (i.e., needed another surgery) for CSDH after being treated by BHC with/without irrigation or with/without drainage.
IV. Inclusion criteria
We included studies with ≥ 10 patients, where less than 10% of patients were lost to follow up at the time of their statistical evaluation. The CSDH diagnosis had to be confirmed by computed tomography (CT) scans and/or magnetic resonance imaging (MRI) in all patients prior to surgery. Studies had to identify BHC (irrigation or drain) as the first surgical treatment. Only reports that compared the recurrence rate of CSDH after BHC with/without irrigation or with/without drain were included.
V. Study quality assessment
Because all studies in our systematic review were observational retrospective cohort studies, we used the Newcastle-Ottawa Quality Assessment Scale for cohort studies as our quality assessment tool. This validated scale evaluates cohort studies based on three characteristics: selection of the study groups, comparability between the groups, and outcome of interest. We considered a study with score ≥ 7 (on a scale of 9) to be of good quality. Based on these criteria, all studies used in our systematic review appeared to be good quality studies.
VI. Statistical analyses
Data were processed using Review Manager 5.1.6 as supplied by the Cochrane Collaboration, Oxford, UK. Statistical analyses for dichotomous variables were performed using odds ratios (ORs) as the summary statistic. Statistical significance was set at P < 0.05 or a 95% confidence interval (CI) of odds ratios not including 1. Effect sizes are expressed as (pooled) odds ratio estimates. Pooled data were interpreted to be heterogeneous if the probability value of the χ2 test was < 0.10.
Results
Among all studies, we identified three reports as randomized control studies that compared the recurrence rate of CSDH after BHC with or without irrigation. Three randomized control studies and two observational retrospective cohort studies were identified that described the outcomes of 228 BHC cases with irrigation and drainage and 313 cases with drainage alone (Table 1).
Table 1.
Basic information from the published reports (irrigation vs. no irrigation)
| Author | Publication year | Collection time | Sample (n) | Recurrence/+I+D (n) | Recurrence/–I+D (n) | Randomized controlled | Mean age (years) |
|---|---|---|---|---|---|---|---|
| Suzuki et al.5) | 1998 | 1986–1993 | 186 | 2/67 | 4/119 | Not mentioned | 66.5 |
| Kuroki et al.6) | 2001 | 1994.9–1999.12 | 101 | 5/45 | 1/56 | Not mentioned | 67.3/70.3 |
| Gurelik et al.7) | 2007 | 2001–2004 | 80 | 8/42 | 4/38 | Randomized | 58.4/59.2 |
| Zakaraia et al.8) | 2008 | 2002.2–2004.8 | 82 | 4/40 | 6/42 | Randomized | 59.7/57.6 |
| Ishibashi et al.9) | 2011 | 1998.1–2009.12 | 92 | 1/34 | 6/58 | Randomized | 79.1/77.9 |
+I+D: irrigation and drainage, –I+D: drainage alone, +I–D: irrigation alone.
Additionally, there were five reports identified as randomized control studies that compared the recurrence rate of CSDH after BHC with or without drainage. Eight studies were identified that described the outcomes of 515 BHC cases with irrigation and drainage and 438 BHC cases with irrigation alone (Table 2).
Table 2.
Basic information from the published reports (drainage vs. no drainage)
| Author | Publication year | Collection time | Sample (n) | Recurrence/+I+D (n) | Recurrence/+I–D (n) | Randomized controlled | Mean age (years) |
|---|---|---|---|---|---|---|---|
| Laumer et al.10) | 1989 | 1984.9–1987.9 | 96 | 13/49 | 12/47 | Randomized | Not mentioned |
| Wakai et al.11) | 1990 | 1986.3–1987.9 | 38 | 1/20 | 6/18 | Not mentioned | 70.8/71.7 |
| Tsutsumi et al.12) | 1997 | 1992.7–1996.6 | 118 | 2/65 | 9/53 | Randomized | 68.0/69.7 |
| Erol et al.13)] | 2005 | 1994–2002 | 70 | 5/35 | 6/35 | Randomized | Not mentioned |
| Santarius et al.14) | 2009 | 2004.11–2007.11 | 215 | 10/108 | 26/107 | Randomized | 74.4/77.9 |
| Carlsen et al.15) | 2011 | 2004–2009 | 344 | 29/206 | 36/138 | Not mentioned | Not mentioned |
| Javadi et al.16) | 2011 | 2007.6–2009.7 | 40 | 1/20 | 1/20 | Randomized | 68/65 |
| Seçer et al.17) | 2012 | 2001–2008 | 32 | 0/12 | 5/20 | Not mentioned | 72.33/69.55 |
+I+D: irrigation and drainage, –I+D: drainage alone, +I–D: irrigation alone.
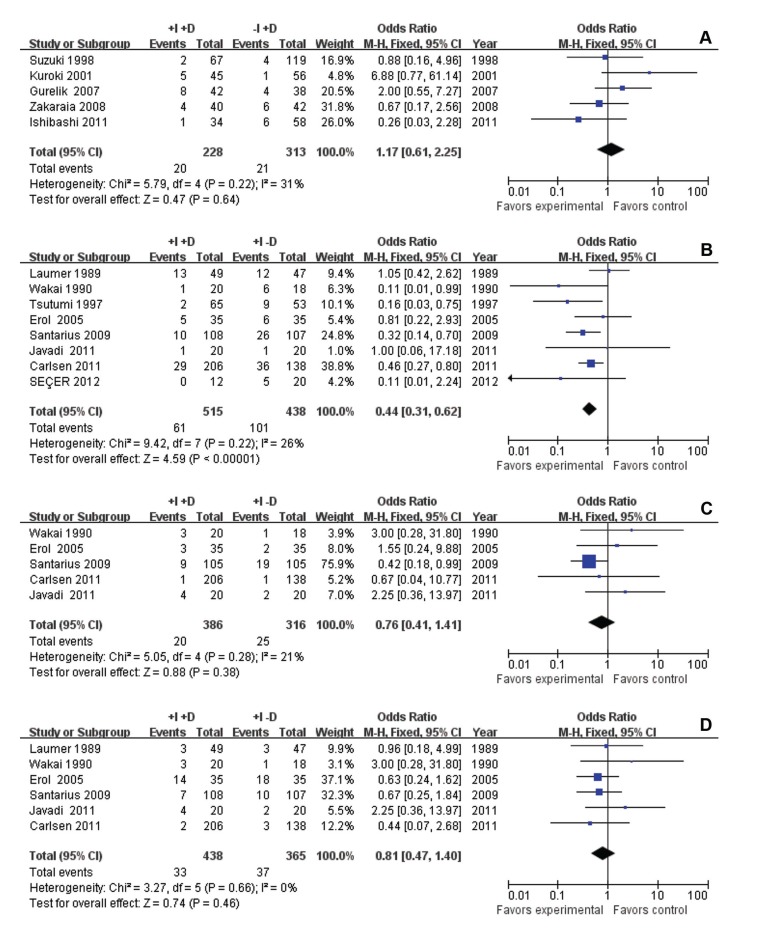
Figs. 1A to D show 95% CIs and odds ratios for each individual study, summarized in forest plots.
Fig. 1.
Meta-analysis of irrigation vs. no irrigation for recurrence (A); drainage vs. no drainage for recurrence (B); drainage vs. no drainage for mortality (C); drainage vs. no drainage for complication (D).
I. Meta-analysis
According to the results of χ2 and P value for χ2 with degree of freedom, we used the fixed effect of the inverse variance weighted method in all comparisons.
Irrigation vs. no irrigation for recurrence: The combined odds ratio for all studies was 1.17 (95% CI 0.61–2.25), and the Z score of the combined odds ratio of recurrence of CSDH for these studies was 0.47 (P = 0.64) (Fig. 1A).
Drainage vs. no drainage for complications: The combined odds ratio for six studies was 0.81 (95% CI 0.47–1.40), and the Z score of the combined odds ratio of recurrence of CSDH for these studies was 0.74 (P = 0.46) (Fig 1B).
Drainage vs. no drainage in mortality: The combined odds ratio for six studies was 0.76 (95% CI 0.41–1.41), and the Z score of the combined odds ratio of recurrence of CSDH for these studies was 0.88 (P = 0.38) (Fig. 1C).
Because the 95% CI of the combined odds ratio of the recurrence of CSDH for these studies included one, and the P value of the combined Z score for the combined odds ratio did not reach significance (0.05), we concluded that there are no statistically significant differences in the recurrence rates after BHC with or without irrigation. In addition, there are no statistically significant differences in complication and mortality rates after BHC with or without drainage when performed to evacuate CSDH.
Drainage vs. no drainage in recurrence: The combined odds ratio for all studies was 0.44 (95% CI 0.31–0.62), and the Z score of the combined odds ratio of recurrence of CSDH for these studies was 4.59 (P < 0.00001) (Fig. 1D).
Because the 95% CI of the combined odds ratio of the recurrence of CSDH for these studies excluded one, and the P value of the combined Z score for the combined odds ratio was less than 0.01, we concluded that there are statistically significant differences in the recurrence rates after BHC with or without drainage when performed to evacuate CSDH.
II. Sensitivity analyses
We performed sensitivity analyses to test the results under varied conditions. We used the jackknife method to perform sensitivity analyses. We had five BHC studies with or without irrigation and eight BHC studies with or without drainage in our review. Therefore, we repeated the meta-analysis five and eight times, respectively, each omitting a different study. The same results were obtained in all conditions.
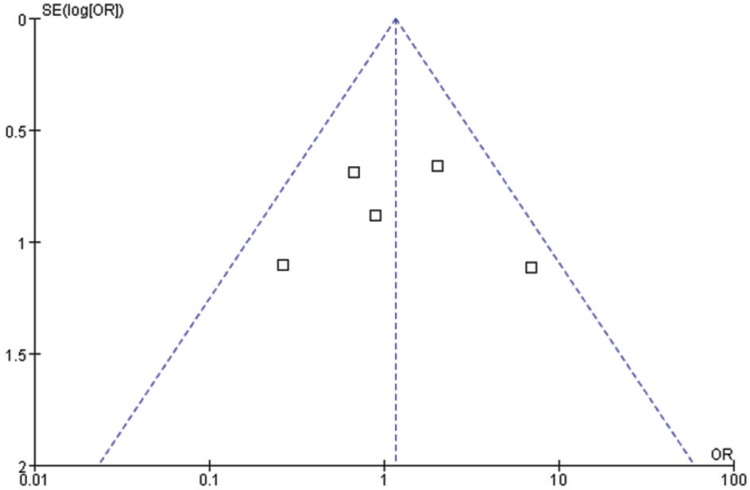
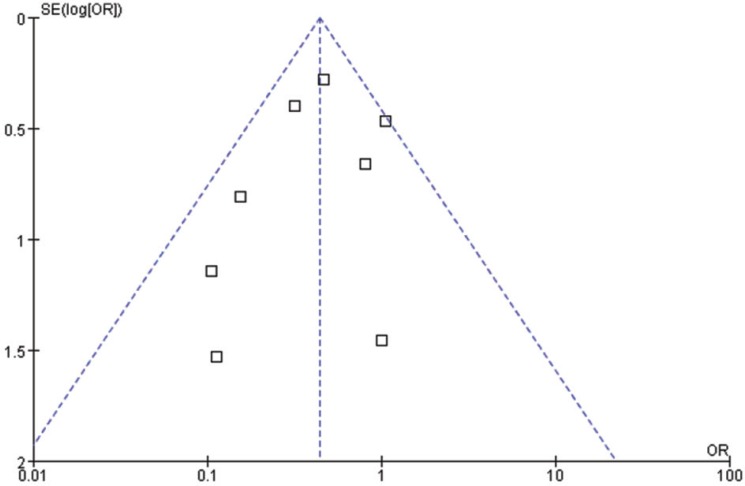
III. Assessment of different types of bias
To test whether publication bias was present among studies included in our meta-analysis, we used funnel plots (Figs. 2, 3). Although the total number of studies in this meta-analysis is low, distribution in the funnel plots is nearly symmetrical. This result suggests that there is no publication bias. Although some were retrospective studies, recall bias was also not a factor in these studies because in all cases the CSDH diagnosis was confirmed by imaging, whereas surgical procedures and outcomes were identified by searching the surgical records for each patient. Attrition bias or bias due to loss to follow-up is also unlikely because CSDH recurrence most often occurs soon after surgery, prior to patient discharge. Furthermore, clinical follow-up data from post-operative visits, which were provided in all studies, indicated no loss to follow-up.
Fig. 2.
Bias analysis of funnel plot (irrigation vs. no irrigation).
Fig. 3.
Bias analysis of funnel plot (drainage vs. no drainage).
Discussion
Burr-hole irrigation with closed-system drainage for the treatment of CSDH was first reported by McKissock and Richardson in 1960s.19) Currently, it is the most widely used surgical method for the treatment of CSDH. The evidence-based review by Weigel et al.20) and the decision analysis by Lega et al.4) indicate that BHC is the most efficient choice for surgical drainage of uncomplicated CSDH. It balances low recurrence rates with a low incidence of highly-morbid complications. Commonly, BHC surgery includes “intraoperative irrigation” and “postoperative drainage.” However, whether both of these methods are necessary remains unclear.
First, in the past 20 years, many studies have shown that drainage reduces the risk of recurrence in BHC, and a frontal drain position reduces the risk of recurrence20) (type B recommendation). Postoperative continuous drainage may promote the discharge of residual substances from the hematoma cavity. However, because it is a foreign matter, the drainage tube may increase the risk of postoperative infection. Furthermore, because the drainage device is placed on the head, the patient must remain in bed for several days, which may cause complications such as pneumonia or urinary infections, particularly in the elderly. For these reasons, some neurosurgeons remain skeptical about the procedure.21)
Many studies have compared the recurrence, complication, and mortality rates between irrigation and no irrigation. However, there was no consensus in the results of these studies. Directly inserting the drainage tube can avoid air entering the subdural space, prevent contralateral acute subdural hematoma due to the tearing of bridging veins, and prevent ipsilateral epidural hematoma (EDH) caused by a rapid drop in intracranial pressure (ICP) at the primary CSDH side. In contrast, most BHCs are performed under local anesthesia, and reduced irrigation may shorten the operation time to alleviate the suffering of patients. The purpose of using warm saline to irrigate the CSDH cavity is dilution of the hematoma, which facilitates the outflow of fibrin degradation products. However, repeated irrigation may bring air into the brain, which can cause pneumocephalus, headache, and an increased risk of recurrence.6) Multiple-direction irrigation may injure the brain surface, perhaps leading to acute intracranial hematoma.
The results of this meta-analysis suggest no significant statistical differences in recurrence between irrigation and no irrigation; however, there was an opposite outcome with regard to drainage. Okada et al.22) compared burr-hole drainage and burr-hole irrigation in treating CSDH and concluded that postoperative hospitalization times were shorter, and recurrences were less frequent, with drainage compared to irrigation. Thus, these data further prove that drainage plays a more important role in treating CSDH than irrigation.
We suggest that neurosurgeons should carefully evaluate whether it will be easy to perform drainage according to the liquid flowing out of the hematoma capsule after its incision. If the effluent is watery (i.e., the main component of CSDH is subdural effusion), closed-system drainage can be directly connected. Otherwise, if the effluent is thick and accompanied by blood clots (i.e., the main component of CSDH is blood), which is difficult to drain, warm saline can be used to irrigate the cavity. However, the degree and frequency of irrigation should be controlled and it is not necessary to wait until the fluid becomes completely clear. A drainage catheter can be inserted and connected to a collection apparatus. Because the type of each manufacturer’s drainage tube is different, the length in each is not identical. However, compared with the length of the drainage tube, the tube’s position of exit appears more important. If the tube is placed too high, the speed of the drainage is not effective. Conversely, if the location of the tube is too low, the drainage speed will be too fast and may cause sharp change in intracranial pressure.
There are some limitations of this meta-analysis. First, some studies were observational retrospective cohort studies and not randomized, matched, or paired between the two patient groups. Thus, confounding variables such as CSDH thickness, patient use of anticoagulants, alcohol use, comorbidities, and the age of the patients between study groups were not controlled. However, some studies in this review did examine different confounds and found no difference between the groups. Another limitation is that the surgical methods cannot occur blinded. In addition, the degree of irrigation and the closed-system drainage device used in each study are different. Despite these limitations, we believe the results of our meta-analysis are the best available evidence regarding recurrence rate, complications, and mortality rate between irrigation and drainage when performed to treat adult patients with CSDH.
Conclusion
The results of this meta-analysis suggest that a burr-hole with closed-system drainage can reduce the recurrence of CSDH. However, irrigation is not necessary for every patient. More randomized controlled trials would be required to control all confounds and confirm this conclusion. There may be only weak support for such a trial in the neurosurgical world, considering the good outcomes and relatively low recurrence risk achieved with any of the surgical treatments used for CSDH. However, neurosurgeons should also improve their surgical skills to reduce the impact of human factors in surgical procedures.
References
- 1). Kudo H, Kuwamura K, Izawa I, Sawa H, Tamaki N: Chronic subdural hematoma in elderly people: present status on Awaji Island and epidemiological prospect. Neurol Med Chir (Tokyo) 32: 207– 209, 1992. [DOI] [PubMed] [Google Scholar]
- 2). Taussky P, Fandino J, Landolt H: Number of burr holes as independent predictor of postoperative recurrence in chronic subdural haematoma. Br J Neurosurg 22: 279– 282, 2008. [DOI] [PubMed] [Google Scholar]
- 3). Cenic A, Bhandari M, Reddy K: Management of chronic subdural hematoma: a national survey and literature review. Can J Neurol Sci 32: 501– 506, 2005. [DOI] [PubMed] [Google Scholar]
- 4). Lega BC, Danish SF, Malhotra NR, Sonnad SS, Stein SC: Choosing the best operation for chronic subdural hematoma: a decision analysis. J Neurosurg 113: 615– 621, 2010. [DOI] [PubMed] [Google Scholar]
- 5). Suzuki K, Sugita K, Akai T, Takahata T, Sonobe M, Takahashi S: Treatment of chronic subdural hematoma by closed-system drainage without irrigation. Surg Neurol 50: 231– 234, 1998. [DOI] [PubMed] [Google Scholar]
- 6). Kuroki T, Katsume M, Harada N, Yamazaki T, Aoki K, Takasu N: Strict closed-system drainage for treating chronic subdural haematoma. Acta Neurochir (Wien) 143: 1041– 1044, 2001. [DOI] [PubMed] [Google Scholar]
- 7). Gurelik M, Aslan A, Gurelik B, Ozum U, Karadag O, Kars HZ: A safe and effective method for treatment of chronic subdural haematoma. Can J Neurol Sci 34: 84– 87, 2007. [DOI] [PubMed] [Google Scholar]
- 8). Zakaraia AM, Adnan JS, Haspani MS, Naing NN, Abdullah JM: Outcome of 2 different types of operative techniques practiced for chronic subdural hematoma in Malaysia: an analysis. Surg Neurol 69: 608– 615; discussion 616, 2008. [DOI] [PubMed] [Google Scholar]
- 9). Ishibashi A, Yokokura Y, Adachi H: A comparative study of treatments for chronic subdural hematoma: burr hole drainage versus burr hole drainage with irrigation. Kurume Med J 58: 35– 39, 2011. [DOI] [PubMed] [Google Scholar]
- 10). Laumer R, Schramm J, Leykauf K: Implantation of a reservoir for recurrent subdural hematoma drainage. Neurosurgery 25: 991– 996, 1989. [DOI] [PubMed] [Google Scholar]
- 11). Wakai S, Hashimoto K, Watanabe N, Inoh S, Ochiai C, Nagai M: Efficacy of closed-system drainage in treating chronic subdural hematoma: a prospective comparative study. Neurosurgery 26: 771– 773, 1990. [DOI] [PubMed] [Google Scholar]
- 12). Tsutsumi K, Maeda K, Iijima A, Usui M, Okada Y, Kirino T: The relationship of preoperative magnetic resonance imaging findings and closed system drainage in the recurrence of chronic subdural hematoma. J Neurosurg 87: 870– 875, 1997. [DOI] [PubMed] [Google Scholar]
- 13). Erol FS, Topsakal C, Faik Ozveren M, Kaplan M, Tiftikci MT: Irrigation vs. closed drainage in the treatment of chronic subdural hematoma. J Clin Neurosci 12: 261– 263, 2005. [DOI] [PubMed] [Google Scholar]
- 14). Santarius T, Kirkpatrick PJ, Ganesan D, Chia HL, Jalloh I, Smielewski P, Richards HK, Marcus H, Parker RA, Price SJ, Kirollos RW, Pickard JD, Hutchinson PJ: Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet 374: 1067– 1073, 2009. [DOI] [PubMed] [Google Scholar]
- 15). Carlsen JG, Cortnum S, Sørensen JC: Recurrence of chronic subdural haematomata with and without post-operative drainage. Br J Neurosurg 25: 388– 390, 2011. [DOI] [PubMed] [Google Scholar]
- 16). Javadi A, Amirjamshidi A, Aran S, Hosseini SH: A randomized controlled trial comparing the outcome of burr-hole irrigation with and without drainage in the treatment of chronic subdural hematoma: a preliminary report. World Neurosurg 75: 731– 736; discussion 620–623, 2011. [DOI] [PubMed] [Google Scholar]
- 17). Seçer M, Kalyoncu N, Günal M, Kuruoğlu E: Comparison of burr hole irrigation and closed system drainage methods after burr hole irrigation in the treatment of chronic subdural hematoma. Journal of Neurological Sciences (Turkish) 29: 280– 284, 2012. [Google Scholar]
- 18). Kansal R, Nadkarni T, Goel A: Single versus double burr hole drainage of chronic subdural hematomas. A study of 267 cases. J Clin Neurosci 17: 428– 429, 2010. [DOI] [PubMed] [Google Scholar]
- 19). McKissock W, Richardson A, Bloom WH: Subdural hematoma: a review of 389 cases. Lancet 1: 1365– 1369, 1960. [Google Scholar]
- 20). Weigel R, Schmiedek P, Krauss JK: Outcome of contemporary surgery for chronic subdural haematoma: evidence based review. J Neurol Neurosurg Psychiatr 74: 937– 943, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21). Santarius T, Lawton R, Kirkpatrick PJ, Hutchinson PJ: The management of primary chronic subdural haematoma: a questionnaire survey of practice in the United Kingdom and the Republic of Ireland. Br J Neurosurg 22: 529– 534, 2008. [DOI] [PubMed] [Google Scholar]
- 22). Okada Y, Akai T, Okamoto K, Iida T, Takata H, Iizuka H: A comparative study of the treatment of chronic subdural hematoma—burr hole drainage versus burr hole irrigation. Surg Neurol 57: 405– 409; discussion 410, 2002. [DOI] [PubMed] [Google Scholar]