Abstract
Inevitable human exposure to ionizing radiation from man-made sources has been increased with the proceeding of human civilization and consequently public concerns focus on the possible risk to human health. Moreover, Fukushima nuclear power plant accidents after the 2011 East-Japan earthquake and tsunami has brought the great fear and anxiety for the exposure of radiation at low levels, even much lower levels similar to natural background. Health effects of low dose radiation less than 100 mSv have been debated whether they are beneficial or detrimental because sample sizes were not large enough to allow epidemiological detection of excess effects and there was lack of consistency among the available experimental data. We have reviewed an extensive literature on the low dose radiation effects in both radiation biology and epidemiology, and highlighted some of the controversies therein. This article could provide a reasonable view of utilizing radiation for human life and responding to the public questions about radiation risk. In addition, it suggests the necessity of integrated studies of radiobiology and epidemiology at the national level in order to collect more systematic and profound information about health effects of low dose radiation.
Keywords: Low Dose Radiation, Health Effects, Radiobiology, Epidemiology, LNT Model
Graphical Abstract
INTRODUCTION
Since the discoveries of X-ray by Roentgen, W.C. in 1895 and radioactivity by Becquerel, H. in 1896 (1), radiation has been used in diverse fields for the improvement of human life, including medical diagnosis and treatment for diseases, industrial application, scientific and educational uses (2). In the early days after finding radiation, it was prevalent all over the industrial fields without recognizing that exposure to large radiation dose could cause serious harmful effects on human health, for example, “Radiothor” (a popular and expensive radium containing water) and “Fluoroscope” (a shoe-fitting X-ray unit) (3). Owing to the scientific research such as Herman J. Muller’s pioneering works on the mutagenic X-ray and the radiation disaster by two atomic bombs in 1945 in Japan, the view of the public for the radiation had been changed, and finally the protection standards for exposure to radiation was constructed by several expert authorities (4).
RADIATION EXPOSURE AND BIOLOGICAL RESPONSE
Challenge to the target theory in low dose radiation response
Despite the uncertainty of the Muller’s data due to insufficient analysis and lack of overall consistent findings for low dose range, his achievement is one of the critical contributing factors consolidating LNT (linear-no-threshold) model as a standard concept for regulation of the human radiation exposure (5,6). In the LNT model, any low dose of radiation can dose-proportionally cause detrimental effects such as cancer and heritable genetic mutation without a threshold dose. This model is now accepted to adopt policy for radiation protection in the world (7). However, the LNT model neglects the important facts that all living beings on the earth have been evolved and adapted to harsher natural radiation environments for billions of years. Moreover, there is a growing body of experimental and epidemiological evidence that does not support the LNT model for estimating cancer risks at low doses (8). In addition, the traditional concept that radiation hits a defined target in cells and genes has been changed into that there are also non-targeted DNA mechanisms in low dose radiation response. They are very complex to investigate, and the prediction for their occurrence is more difficult due to the presence of several agonistic or antagonistic confounding factors such as pollutants, ages and life styles. Recent reports issued by international authorities of radiation such as NAS (the National Academy of Sciences), UNSCEAR (the United Nations Scientific Committee on the Effects of Atomic Radiation), ICRP (the International Commission on Radiological Protection), FAS (the French Academy of Sciences) analyzed a great number of experimental data related to low dose radiation (9,10,11,12). They commonly announced that biological responses of low dose radiation were different from those of high dose radiation with various dose-response relationships and therefore, low dose effects cannot be concluded to be harmful to human health (9,12). They also recommended holistic approaches combining biological system-based methods with epidemiological data to develop more sophisticated dose-response models at low dose levels, considering a dose and dose-rate effectiveness factor (DDREF) (7).
Complexity of biological effects of radiation exposure
Radiation may damage various cellular components including DNA, directly (molecule ionization) or indirectly (reactive oxygen species production). Irradiated cells protect themselves by many innate defense mechanisms such as removal of oxidative stress and damaged cells, and DNA repair. Remained damages of cells may cause tissue/organ dysfunction and malignant diseases. For radiation protection, the biological effects of radiation are conventionally categorized into two broad classes: stochastic and deterministic effects (or recently termed tissue reactions) (13).
Stochastic effects have probability of occurrence depending on the irradiated doses without threshold. These effects can occur by chance and consist primarily of cancer and genetic effects such as inherited mutations. Stochastic effects often show up years after exposure. In addition, because they can occur in individuals under background radiation levels without exposure, it can never be determined that an occurrence of these effects was due to a specific exposure (2).
Deterministic effects (or non-stochastic effects) are malfunctions of organs by irradiation at more than threshold. These effects do not exist below their threshold doses, for example, skin burns, cataracts, cardiovascular disease, intestinal damage, and hemopoietic system and central nervous system failure (14). Recent ICRP report referred to deterministic effects as tissue reactions because it was recognized that these effects are not decided at the moment of irradiation and can be modified through various biological responses (15). This simplistic classification is not absolute. Deterministic effects can occur as a result from the loss of normally functioning large number of critical cells caused by stochastic killing of irradiated individual cells.
RISK ASSESSMENT OF RADIATION EXPOSURE
Proposed models for risk assessment of radiation exposure and ongoing debate
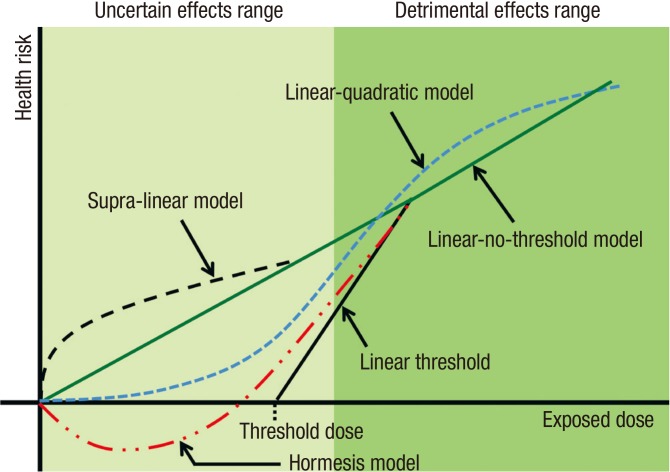
During the early decades of the 20th century, consensus of the public had been achieved that the most fundamental radiation dose-response relationships have a threshold (16). Protection agencies recommended dose limits for workers and the public following linear model with a threshold dose. They believed the presence of tolerance levels against radiation exposure. In this model, there is no radiation risk at less than a threshold dose. However, this concept was rapidly changed after atomic bomb disaster. The atomic bomb survivor data and several evidence from various medical exposure groups had successively reduced the recommended dose limit over the years (13). For the protection against radiation exposure, the dose-response model was finally replaced with a conservative model with the LNT hypothesis that there is no threshold to induce radiation response (17). This model was accepted for human protection of radiation exposure and published as a guideline of radiation policy by ICRP (18). The LNT hypothesis was very useful to estimate the risk of radiation exposure at high doses based on the solid scientific evidence, but not at low doses since the data at low doses are imprecise and often conflicting. A great deal of research has been performed to establish dose-response relationships, especially, in low dose range using data including Japanese atomic bomb survivors, cancer and life-shortening in animals, chromosome aberrations in somatic cells, and then other risk assessment models has been proposed to estimate the radiation toxicity in low levels (19). Nowadays, five risk assessment models has been discussed (Fig. 1). These models focus on primarily cancer risk. Regarding heritable risk, its nominal risk coefficient in the whole population was estimated as 0.2% per Sv in ICRP 103, which was substantially reduced by a factor of 6-8 compared to the estimates from the former ICRP 60, becoming less of a concern about health risks of low dose radiation. The LNT (linear-no-threshold) model is a gold standard model for radiation safety regulation, as mentioned above. This relationship implies proportionality between dose and cancer risk. Because risk estimation at low doses is achieved by extrapolation of linear dose-response relationship for high doses without definite scientific evidence, it should be carefully revaluated in the low level of radiation. LQ (linear quadratic) model is widely view in radiotherapy and it is the best fit to leukemia data from the Life Span Study (LSS) of atomic bomb survivors (20). Some experimental data such as bystander effect and low-dose hypersensitivity were observed at low doses and should yield a supralinear dose-response relationship (21). Low dose hypersensitivity decreases with increasing dose and disappears at doses higher than 0.5 Gy due to the biological defense system (22). Low dose hypersensitivity could eliminate potential mutant cells at low doses, thereby reducing the carcinogenic risk. Hormesis model shows U-shaped dose-response relationships at low doses. In various experiments in vitro and in vivo, low dose radiation induced the activation of protective mechanisms at the cell and tissue levels, against carcinogenic factors other than ionizing radiation and even against spontaneous cancer (23,24,25).
Fig. 1.
Schematic diagram illustrating various dose-response models in risk assessments. Radiation exposed level is represented on the x-axis and overall risk for diseases is represented on the y-axis.
Diverse observation on the biological effects of low dose radiation
Profound insight on carcinogenesis at the molecular level opens widely the ways to understand physiological responses of radiation. Progress of biological technologies also enables us to collect a great number of new experimental data related to low dose radiation. Thousands of reports indicate that LNT model is inappropriate to explain the biological responses of low dose radiation at the levels of genome, cells, tissues, and experimental animals.
Immediate defense mechanisms
Living organisms have innate defense systems, including antioxidant molecules against oxidative stress generated from metabolism, repair system to restore damaged DNA, and removal of damaged cells. These systems could be activated by low dose radiation and less effective when the irradiated dose is high. Reactive oxygen species produced by low dose radiation are rapidly removed by anti-oxidative enzymes, and DNA damages by irradiation are also repaired by two main systems, homologous recombination (HR) and non-homologous end joining (NHEJ) (26). Both are influenced by irradiated dose, dose-rate, nature of radiation, and cell state. The efficacy of repair in the irradiated cells at low dose would be higher than at high dose (27). Therefore, the carcinogenic risk seems to be negligible at low doses and low dose-rates irradiation. The irradiation at doses less than 100 mSv did not induce the intra-chromosomal inversions and deletions in human (28). Programmed cell death (apoptosis) activated by low doses under 200 mSv could remove damaged cells (29,30). The number of eliminated cells at low dose irradiation did not affect the tissue function for organism’s living.
Non-targeted effects of radiation
Irradiated cells may communicate their information to neighboring cells with small molecules, which is a representative non-targeted effect called “bystander effect”. Similarly, “abscopal effects” is another non-targeted effect defined that a radiation effect in a non-irradiated tissue distant from the irradiated tissue. It could be explained as cases fitting supralinear dose-risk relationships. However, recent results suggest that irradiated cells also protect neighboring cells, thus acting as a beneficial effect (31,32). Health effects at less than 100 mSv are argued whether radiation is good or bad in epidemiological approaches which already include non-targeted effects of radiation in risk estimation.
Radiation-induced genomic instability
Genomic instability is the acquired DNA damage in cell progeny causing chromosomal aberrations, micronuclei, DNA fragmentation, and aneuploidy. It can be induced through targeted and non-targeted bystander effects by irradiation. Instability can be formed by X-ray at doses about 10 mGy, which is regarded to be an early event in radiation carcinogenesis (33). In contrast, some data related to radiation less than 250 mGy of X- or gamma ray showed no genomic instability (34). Moreover, there has been considerable controversy over whether genomic instability is observed in irradiated human populations (35,36,37). Exposed individual showed convincing evidence of genomic instability in acute myeloid leukemia and myelo-dysplastic syndrome patients among Japanese A bomb survivors (38). However, this data is still questioned whether the observed instability is caused by a consequence of the disease or non-targeted effects of irradiation, and whether the instability is correlated to the development of diseases. It remains difficult to determine whether radiation-induced genomic instability at low doses affects health risk.
Adaptive response
In addition to the presence of immediate defense mechanisms against radiation, a stimulation (or activation) of defenses is induced by low dose radiation. These adaptive responses are observed in cultured cells and model animals after irradiation at less than 500 mGy (39,40). Growth of human cells under reduced background radiation increased their sensitivity to acute irradiation at high dose (41). These are thought to be an evidence for the existence of a persistent adaptive response made by normal levels of background radiation. It could be also specifically determined depending on the genetic background in lymphocytes (42). Therefore, adaptive response induced by radiation should be carefully analyzed with various physiological factors.
Radiation hormesis
Hormesis could be defined as the stimulating effect of small doses of substances which in larger doses are inhibitory. Up-regulation of protective mechanisms at the cell and tissue by low doses can function against spontaneous cancer other than radiation-induced carcinogenesis. Indeed, irradiation at 10 mGy reduced the rate of spontaneous transformation in culture cells below background level (43). In addition, irradiated model animals at low dose showed the extension of their lifespan, compared to non-irradiated control (44,45). Innate immunity study using irradiated fruit flies showed low dose radiation enhanced immune system through the activation of the specific signal pathway related to mammalian NF-κB (46). However, radiation protection agencies announced that radiation hormetic effects are now unwarranted and should be further investigated continuously due to the experimental incoherence and uncertainty. In addition, they strongly recommend research into the mechanistic understanding of hormesis that may contribute to improved understanding of low dose radiation-induced response.
New biological research fields to estimate radiation risk at low doses
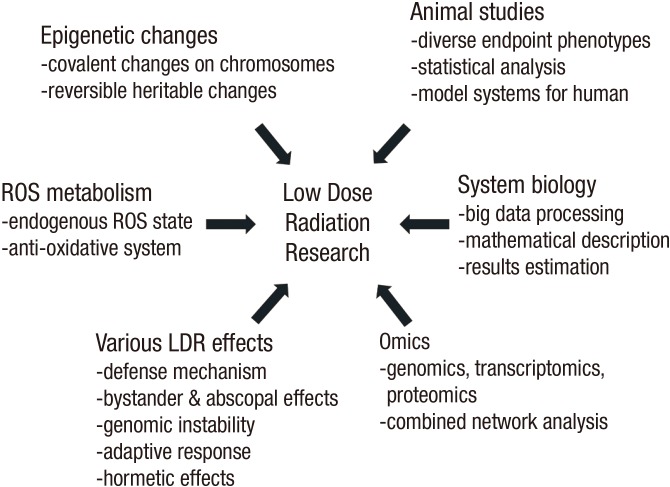
Development of molecular and biochemical approaches to reveal the physiological phenomena like carcinogenesis has been rapidly applied to radiobiology. Especially, reversible heritable changes on genome without a change in the DNA sequences, epigenetic changes, are an outstanding field in understanding carcinogenesis. Additional covalent modifications of chromosomal structure, e.g. phosphorylation, methylation, acetylation and sumoylation, can be particularly affected by radiation. Some epigenetic data using irradiated mice showed that high dose radiation altered gene expression levels through transmitted epigenetic modification and potentially increased the cancer risk (47). ROS (reactive oxygen species) in the irradiated cells is also thought to be an important factor to modulate radiation response. ROS state is significantly regulated by irradiation at low doses, which maintained for a period time accompanying with gene expression changes (48). In the irradiated cells, anti-oxidant molecules such as Mn-SOD (manganese-superoxide dismutase) were regulated by the redox state-sensing transcription factor NF-κB (49). Omics is another excellent arsenal to reveal the overall cellular signal networks rather than one or two specific signaling, e.g. genomics, epigenomics, transcriptomics, proteomics, and metabolomics. Although it can provide high-throughput screening methods to find biomarkers in radiation response, the analytical tools for mass data and much regarding to validation for them remain to be incomplete (50). Finally, system biology is recommended to analyze and estimate the radiation response. It can deal with multi-factors affecting radiation response and elucidate the connectivity among signaling networks with mathematical equations produced by computational biology (51). In addition, mechanistic model is necessary for the explanation of radiation response, especially at low dose, including environmental factors. It can remove the uncertainty and inconsistency from biological specimen. For example, the transcriptional responses for specific genes in system biological approaches displayed considerable inter-individual heterogeneity when intact human skin was exposed to radiation in vivo (52). These cross-talk analytic approaches as mentioned above are required for revealing proper molecular function in the irradiated tissues and radiation-induced cancer risks in the near future (Fig. 2).
Fig. 2.
Recent biological studies on the low dose radiation effects. To increase the consistency and coherence of experimental data on low dose radiation, we should introduce new biological knowledge of emerging area as well as conventional concepts.
Confronting difficulties to separate the effects of low dose radiation from the complicated environmental stressors
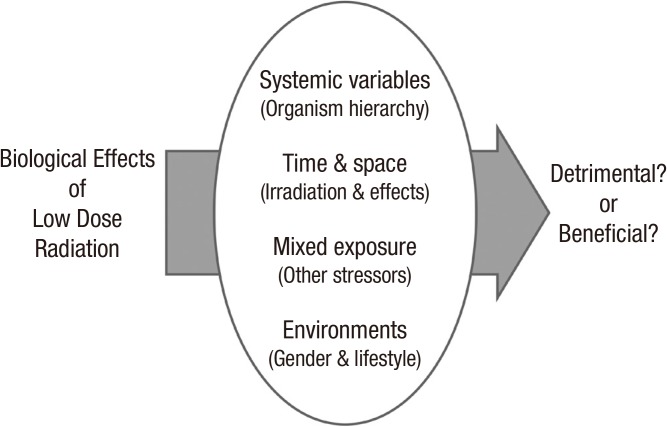
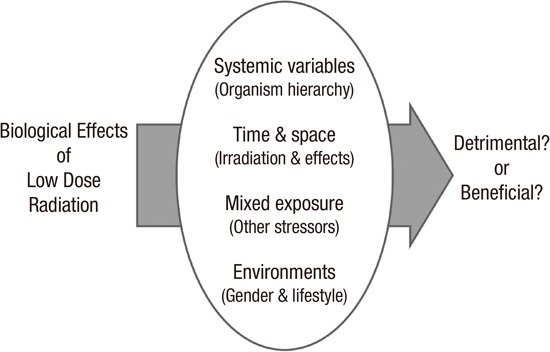
Recently, radiobiologist largely accepted theoretically that low dose radiation could facilitate the distinguished biological response from the targeted detrimental effects caused by high doses, where non-targeted effects are inhibited. However, these concepts are difficult to be proved since there are many confounding factors to be considered in the analysis for end-point phenotypes such as cancers. First, living things are highly organized in hierarchies with multiple dimensions. Some effects by low dose radiation would be beneficial or detrimental depending on the hierarchical level in the organism. Cell death is often regarded as a bad effect, but if it removes the carcinogenic potentials in a tissue, it could be seen as good in the view of organism’s life maintaining. Second, irradiated time to biological organism is thought to be a determining factor to induce various radiation responses. We can observe that young individuals show the severe impacts due to the faster metabolic rate, higher rate of cell proliferation, and immature entity whether they are cells or organisms. However, older individuals did not always show the resistant phenotype in radiation response. We should consider the context variables in the irradiated biological system. Delayed effects and bystander effects are other examples to show the complexity of radiation responses depending on the time and space of exposure to radiation. These concepts are also discussed elsewhere (53). Third, living organisms are usually exposed to many stressors including ionizing radiation. Radiation effects seldom occur in isolation. These stressors can induce the additive, antagonistic, or synergistic effects in combination with radiation, which are not predictable from individual agent dose response data. This complexity has required more attention how to interpret and manage the results from mixed exposures to the low level of stress. In order to resolve this issue, more data related to low dose exposures to multiple stressors involving radiation and chemical should be investigated, and new experimental system to explain this concept is necessary (Fig. 3).
Fig. 3.
Confounding factors in the analysis of low dose radiation effects. Biological effects of low dose radiation could be determined by several confounding factors as detrimental or beneficial. For example, systemic variables such as hierarchy, maturity, and ageing of irradiated organism, time of irradiation and phenotype emergence, and interaction with other environmental factors.
EPIDEMIOLOGY OF LOW DOSE RADIATION
Epidemiological studies on the effects of low dose ionizing radiation
Scientific evidence of health risks from radiation exposure is based on biological and epidemiological studies. The major role of epidemiological studies in radiation research is to provide the essential data for quantifying human health risks from radiation exposure and for setting radiation protection standards (54). A proportional relationship between cancer risk and effective dose above 200 mSv has been well documented mainly based on Japanese atomic bomb survivor, while radiation-associated health effects at low dose still remain unclear. Effects of low dose radiation are generally considered stochastic effects of which the main risks are cancer and heritable disease. Studies on accidental, occupational, environmental and medical exposures provide useful information of the effects of low doses and low dose rates of ionizing radiation. The commission of the ICRP proposed nominal probability coefficients of 5.5% per Sv for detriment-adjusted cancer and 0.2% per Sv for heritable risks for the whole population, using the LNT model with a DDREF of 2 (55). However, given that health effects of low dose are still poorly known, the application of these coefficients should be used for the purpose of radiological protection and be considered carefully in estimating risk of cancer or heritable disease of low dose radiation. Although there is emerging evidence from recent epidemiological studies indicating elevated risks of non-cancer diseases such as circulatory disease and cataract below doses of 1 to 2 Gy, it is still not clear whether this would extend to low dose and low dose rate exposure (56).
Atomic bomb survivors and accidental exposure
The Life Span Study (LSS) cohort of the atomic bomb survivors is the major source of epidemiological data for radiation risk assessment. The latest LSS study found that the additive radiation risk for solid cancers continues to increase with a linear dose-response relationship (57). The sex-averaged excess relative risk (ERR) for all solid cancer was 0.42 per Gy (95% CI, 0.32-0.53) at age 70 years after exposure at age 30 (57). The study also reported that the estimated lowest dose range with a statistically significant ERR (0.56/Gy, 95% CI, 0.15-1.04) was 0-0.2 Gy; however due to possibilities of sociodemographic selection bias and other factors such as additional radiation sources and a large geographical distribution, further investigation considering these factors is required to interpret the health effects of low dose radiation appropriately (57).
There are numerous studies to investigate health effects from the Chernobyl accident. Except for the increase of thyroid cancer in children with relatively high thyroid absorbed doses (58,59,60), there was no clearly demonstrated increase in the incidence of other cancers or non-cancer diseases in the residents of the Chernobyl region (61). Several case-control or ecological studies suggested the increase of radiosensitive disease such as childhood leukemia and breast cancer (62,63,64); however, due to the nature of the study design and lack of consistency among other studies, these data have not been sufficient to provide convincing evidence for low dose effects. For the Chernobyl liquidators more heavily exposed to prolonged low to medium radiation (0-500 mSv), there exist some data indicating the increase in the risk of leukemia, cataracts and cardiovascular diseases (65,66,67,68), but further epidemiological studies is necessary to provide more precise risk estimates and protect individuals exposed to low dose radiation (69).
Health effects following the Fukushima Daiichi nuclear accident have been being extensively monitored by the Japanese government and international organizations such as WHO, UNSCEAR and ICRP. For the comparison of ultrasound screening of thyroid in children between Fukushima and other three Japanese prefectures, no significance differences were observed (70). Until recently, any radiation-induced effects have not been reported, and lifetime health risk would be expected to be minimal based on the risk assessment model with the exposure level of no more than 50 mSv during the first year after the accident (71,72) and the expected lifetime dose after 2012 (73). However, further careful follow-up should be continued in consideration of long latency of radiation effects.
A number of epidemiological studies for the health effects from the Three Mile Island (TMI) nuclear power plant accident have been conducted by different investigators. Despite the low level exposure of 0.09-0.25 mSv within 5-mile area around TMI, elevated risks for non-Hodgkin’s lymphoma, lung cancer and leukemia were noted in a few studies with the first 5 year follow-up after the accident (74,75). These findings were not consistent in the later study with a longer and more comprehensive follow-up of 1979-1998, although dose-response relationships for all lymphatic and hematopoietic tissue (LHT) in males and breast cancer in females cannot be definitely ruled out (76).
In summary, epidemiological data for acute radiation exposure have not provided consistent evidence of health effects in the low dose range.
Occupational exposure (mainly focus on nuclear industrial workers and aircrew)
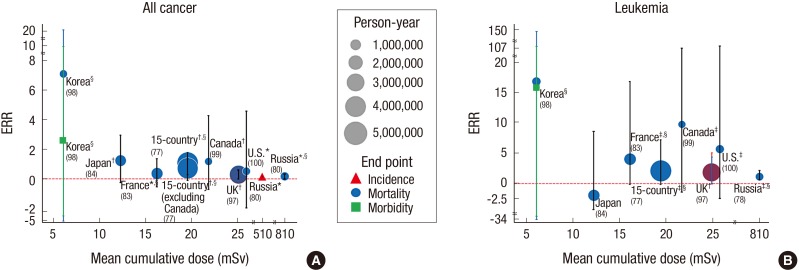
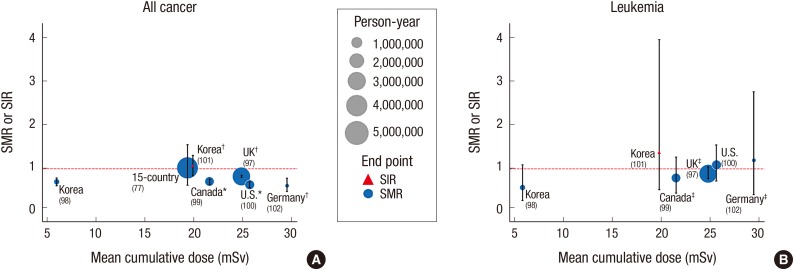
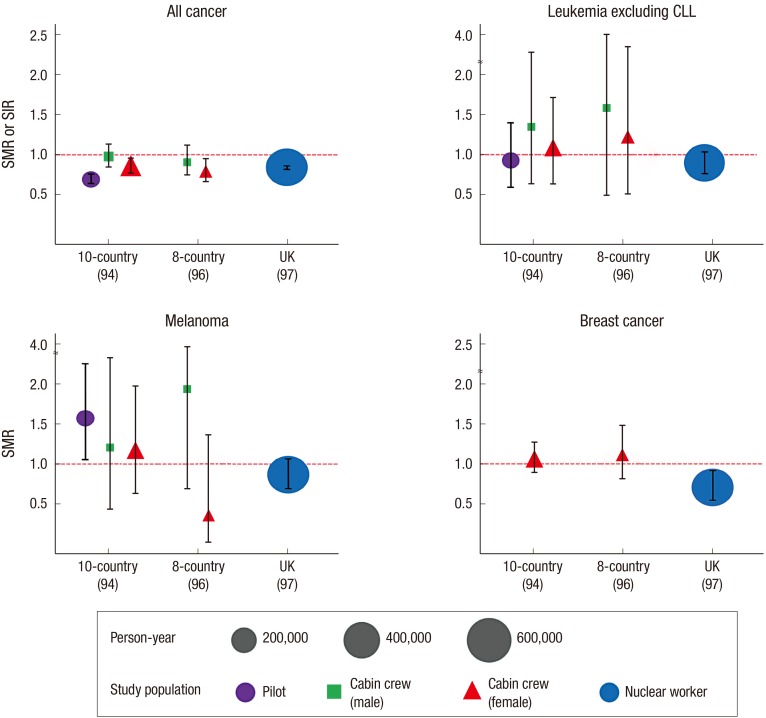
Radiation workers and air crew are well known occupationally exposed cohorts to assess the effects of protracted exposures to low dose radiation. The 15-country collaborative cohort study including 407,391 nuclear industry workers with 5.2 million person-years of follow-up is one of the largest occupational studies (77). From the study a significant ERR of 0.97 (95% CI, 0.27-1.8) for all cancer mortality was reported; however, the significance was not observed after excluding Canada data having uncertainties of dose measurement records (77). Another study reporting an elevated cancer risk is the Mayak nuclear complex cohort studies with the mean cumulative external dose of 810 mGy (78,79,80). The range of the cumulative dose of the study cohort was broader than other nuclear industry cohorts since a substantial number of workers were exposed to relatively high dose in the first decade of the facility operation, which allows some degree of precision in a dose-response relationship with protracted exposure (80). Besides the Mayak cohort studies, elevated risks of certain types of cancer such as leukemia excluding chronic lymphocytic leukemia (CLL) (81,82,83), lung cancer (82) and esophageal cancer (84) were observed in nuclear industry workers in some countries. However, these site-specific risks were not consistent with other study populations and statistical significance was not found in most cohort studies. Since this null finding does not necessarily mean “no risk”, continued studies with long-term follow-up and sophisticated designs and analytical methods are required to draw firmer conclusions. ERR and standardized mortality or incidence ratios (SMR, SIR) for all cancers and leukemia were summarized according to the mean cumulative dose and study populations (Fig. 4 and 5). While cancer risk per unit dose varies across the study populations and exposure doses, possibly due to confounding factors, population heterogeneity or statistical uncertainties (Fig. 4), the tendency to lower SMRs indicates healthy worker effects (Fig. 5).
Fig. 4.
Excess relative risk (ERR) for cancer in major cohort studies of radiation workers. (A) all cancer; (B) leukemia. The mean cumulative doses are represented on the x-axis and ERRs for cancer are represented on the y-axis. *Solid cancer only; †All cancer excluding leukemia; ‡Leukemia excluding CLL; §90% confidence interval.
Fig. 5.
Standardized mortality ratio (SMR) (or Standardized incidence ratio [SIR]) for cancer in major cohort studies of radiation workers. (A) all cancer; (B) leukemia. The mean cumulative doses are represented on the x-axis and SMRs (or SIR) for cancer are represented on the y-axis. *Solid cancer only; †All cancer excluding leukemia; ‡Leukemia excluding CLL.
Aircrew including pilots is the major occupation exposed to cosmic radiation. An average effective dose of aircrew has been estimated to be 2-5 mSv/year and 75 mSv for cumulative effective dose at career end (85). In consideration of that the average effective dose of radiation workers is generally less than 2 mSv/year, epidemiological studies of the aircrew can provide fundamental knowledge and evidence of health effects from the cosmic radiation exposure at low dose levels. Several studies of Nordic, the US and Canada aircrews presented the increase of cancer risk for breast cancer (86,87,88,89), skin cancer (90), brain cancer (91), non-Hodgkin’s lymphoma (92), prostate cancer and acute myeloid leukemia (93), compared to the general population. However, these findings have lacked consistency among studies with no dose-response relationship, and overall cancer risks (e.g., all cancers, all solid cancer or leukemia) were not elevated in most studies. Recent results of the pooled cohort of 93,771 air crews from 10 countries indicated a lower mortality from all cancers, radiation-related cancers and cardiovascular diseases, but a higher mortality from malignant melanoma especially in cockpit crew (94). Similar results were observed in the recent study of the US airline cockpit crew except for an increased risk of the central nervous system (CNS) (95). Due to remarkable differences from the general population in terms of occupational characteristics, lifestyles and disruption of circadian rhythm may be possibly associated with health risks in air crew such as melanoma and breast cancer. Overall cancer mortality in air crew seems similar to one in radiation workers with the suggestion of increased melanoma and breast cancer risks, but not necessarily caused by radiation exposure (Fig. 6).
Fig. 6.
SMR for cancer (all cancer, leukemia excluding chronic lymphocytic leukemia [CLL], melanoma and breast cancer) in major cohort studies of air crews and radiation workers. The names of the studies are represented on the x-axis and SMRs are represented on the y-axis.
In conclusion, radiation-associated health effects at low dose levels have not yet been clearly established in occupationally exposed studies.
High background radiation exposure
The worldwide average natural dose to human is about 2.4 mSv/year (103) with a large variation depending on location and geology. The Yangjiang in China, Karunagappally in India, Guarapari in Brazil, and Ramsar in Iran are well known for their high background radiation areas (HBRAs) of which dose level is up to 260 mSv/year (104). A number of biological and epidemiological studies have been conducted to evaluate health effects in HBRAs. Increased chromosomal aberrations were observed in some studies (105,106), but there was no study reporting an increase in cancer or life-shorting in the residents of HBRAs (107,108,109,110). Increased risk of non-cancer mortality and diseases of digestive system were observed in the study of the Yangjiang area, but not likely to be attributable to radiation exposure (109). Techa River cohort and Taiwan building residents exposed to Co60, are often referred to as the cohort of HBRAs, but strictly speaking they are not HBRAs due to artificial (man-made) radiation sources. Significantly elevated risks of solid cancer and leukemia, which is comparable to risks shown in LSS data, were observed in the Techa River cohort (111,112,113,114) with average effective doses ranging from 35-1,700 mSv for evacuees (115). There were dose-response relationships for leukemia excluding CLL (HR, 1.19/100 mGy; 90% CI, 1.01-1.31) and breast cancer (HR, 1.12/100 mGy; 90% CI, 0.99-1.21) in the Taiwanese residents, but due to the small number of cases, the current data provides limited evidence for the effects of prolonged low dose radiation exposure (116). Most studies of HBRAs were of ecological design due to difficulties in collecting individual data for exposure levels, health outcomes and confounding factors, which may lead to ecological fallacy. Therefore, results from studies of HBRAs should be interpreted with caution. In short, no demonstrated health effects were observed in residents of HBRAs except for the Techa River cohort exposed to artificial radiation above the low dose range.
Medical exposure (diagnostic and therapeutic radiation)
With the remarkable increase in public exposure to diagnostic or therapeutic radiation, numerous studies have examined the link between medical radiation exposure and health risks. Medical exposure cohorts often contain useful information on patients’ characteristics such as demographic data, medical history, smoking and alcohol consumption. Thus, epidemiological studies of these cohorts could provide more accurate assessment of the risks associated with radiation exposure after adjusting for other risk factors. Dose from the diagnostic radiation exposure is generally 0.1-10 mSv, which belongs to the range of low dose radiation, and repeated exposure in childhood is a major concern. Recent retrospective cohort studies for radiation exposure from computed tomography (CT) scan in childhood suggested an increased risk of childhood cancer, especially brain cancer and leukemia (117,118). However, due to some methodological issues including the lack of a control group and potential risks in the patient population, it is difficult to draw a causal relationship between the radiation exposure and cancer risk from these studies. In addition to diagnostic radiation exposure in childhood, a number of studies have conducted to examine the risks from radiotherapy, a risk-benefit analysis of cancer screening programs and genetic susceptibility to the tumorigenic effects of radiation. Overall, it is reasonable to maintain that clinical benefits from the medical exposure outweigh the potential risks from radiation exposure (119,120,121,122). There are some findings about genetic susceptibility for BRAC1/2 mutations related to the risks of radiation (123,124,125,126), but they are not consistent with other studies (127,128,129). Although the exact risk from the medical exposure has not been definitely known, given the increasing use of diagnostic and therapeutic radiation, radiation dose should be kept as low as possible and unnecessary exposure should be avoided, especially for child patients.
UNCERTAINTIES IN ESTIMATING HEALTH RISKS OF LOW DOSE RADIATION
Epidemiological data are essential to investigate low dose effects on human health. Although some evidence for effects of moderate and low doses have been observed to date (null results for very low dose exposure in most studies), they are suggestive rather than conclusive and the interpretation is challenging due to the uncertainties caused by following limitations:
1) Under present knowledge about a dose-response relationship, extremely large sample size is necessary to ensure statistical significance at low dose levels. Based on the US baseline cancer risk and the radiation risk model, sample sizes of 500,000 and 2,000,000 are required with lifetime follow-up for exposure levels of 20 mSv and 10 mSv, respectively (130), which would render a decent epidemiological study unfeasible.
2) Issues of confounding factors such as smoking, genetic variation and socioeconomic status are particularly important in low dose radiation studies. Given the nature of low dose radiation effects with low event (e.g., disease incidence) rates, even a small degree of confounding can distort the study results. It is often not possible to collect all confounding factors and this may lead to inconsistent findings in epidemiological studies. Confounding factors may also mask other radiation-induced endpoints that may be actually present at low dose levels.
3) Uncertainties in radiation dosimetry cannot be avoidable in most epidemiological studies and they influence every aspect of studies. In general, measurement errors related to dosimetry are more likely to mask a true effect rather than to generate a spurious one (131). Continuous improvement of biokinetic and dosimetric models is crucial for the precision of dosimetry measurements.
4) There exist inherent statistical uncertainties in selection of dose-response models, particularly great uncertainties at low dose levels.
In addition to these uncertainties, there also exist other types of uncertainties in estimating health risk through risk assessment models (132). Major components of the uncertainties are as follows: 1) extrapolation of a dose-response relationship through risk transfer between populations with different levels of baseline risk, 2) difference in dose-response relationships according to different types or levels of exposure (e.g., high-energy gamma rays, low-energy photons, alpha particles, neutrons, low doses, acute exposure, chronic exposure, etc), and 3) difference in risk according to parts of the body exposed to radiation (e.g., individual tissue, organ sites and all tumor combined due to whole-body exposure).
Due to these uncertainties, epidemiological studies at low doses become increasingly impractical. Recent research direction is being focused on the integration of biological and epidemiological studies. For example, if we find genetic fingerprints of radiation-induced disease, uncertainties of stochastic models would be largely eliminated (133). In addition, finding the specific gene(s) modulated by low dose radiation will provide more profound information for health effects of low dose radiation. Thus, based on these radiobiological studies, identification of genetically sensitive subpopulation will enable an effective low dose radiation research with increased statistical power. Besides continued investigation of health effects of low dose radiation, social science research including risk communication and education, psychometric paradigm of risk perception and public engagement is essential for risk management, since scientific uncertainties of low dose radiation often bring public concern with lack of social trust for every nuclear or radiation accident.
CONCLUSIONS
As epidemiological and biological data are accumulated indicating cancer and non-cancer diseases associated with protracted low-dose radiation exposure, dose limits have been continuously reduced to 20 mSv/year for radiation workers and 1 mSv/year for the public since the first dose limit of about 10 rad/day (100 mSv/day) in 1902. The recent international large scale cohort study indicated strong evidence of positive associations between leukemia mortality and protracted low dose radiation exposure (134); although the association (i.e., point estimate of relative risk) did not diminish in dose levels less than 300 or 100 mGy, their wide confidence intervals preclude definitive conclusions in the low dose range. In sum, despite a variety of studies, understanding of health effects of low dose radiation, especially less than 100 mSv, is still incomplete and difficult. There are emerging data such as adaptive responses and hormesis against the LNT hypothesis at low dose levels, which could provide useful information to optimize decision making for public health based on the hormetic model where there exist protective effects at low doses and harmful effects at higher doses (135,136). Nevertheless, given the lack of scientific knowledge about health risk of low dose radiation, the LNT approach is the most reasonable risk model at low dose levels and is likely to remain fundamental tenet in terms of radiation protection and safety. On the other hand, caution is required in the interpretation of the estimated risks from the LNT model since the estimate at low doses, which is calculated theoretically based on the LNT hypothesis, does not necessarily correspond to a real risk. Different biological pathways between low and high dose effects are considered proven through sophisticated cellular and molecular studies. Moreover, there is much interest in the interactions between genetic susceptibility and low dose exposure. Although radiation biology cannot currently provide direct evidence of low dose effects in human health, a comprehensive understanding of radiobiological mechanism would facilitate epidemiological studies and improve the precision of a dose-response relationship at low dose levels. The integration of biological and epidemiological studies along with social science research will allow firmer conclusions about low dose effects on human health on the basis of social trust.
Footnotes
Funding: This work was supported by the Nuclear Safety Research Program through the Korea Radiation Safety Foundation, granted financial resource from the Nuclear Safety and Security Commission (NSSC) (No. 1303028), and the Ministry of Science, ICT and Future Planning (MSIP) (No. 50586-2015), Republic of Korea.
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conception and design: Jin YW, Seong KM, Seo S. Acquisition of data: Lee D, Seong KM, Seo S. Writing and review manuscript: Seong KM, Seo S, Kim MJ, Jin YW, Lee SS, Park S, Lee D. Revision of manuscript: Seo S, Seong KM, Jin YW. Study supervision: Jin YW. Manuscript approval: all authors.
References
- 1.Lederman M. The early history of radiotherapy: 1895-1939. Int J Radiat Oncol Biol Phys. 1981;7:639–648. doi: 10.1016/0360-3016(81)90379-5. [DOI] [PubMed] [Google Scholar]
- 2.Mettler FA. Medical effects and risks of exposure to ionising radiation. J Radiol Prot. 2012;32:N9–N13. doi: 10.1088/0952-4746/32/1/N9. [DOI] [PubMed] [Google Scholar]
- 3.Duffin J, Hayter CR. Baring the sole. The rise and fall of the shoe-fitting fluoroscope. Isis. 2000;91:260–282. doi: 10.1086/384721. [DOI] [PubMed] [Google Scholar]
- 4.Preston RJ. Radiation biology: concepts for radiation protection. Health Phys. 2005;88:545–556. doi: 10.1097/00004032-200506000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Calabrese EJ. Muller’s Nobel Prize Lecture: when ideology prevailed over science. Toxicol Sci. 2012;126:1–4. doi: 10.1093/toxsci/kfr338. [DOI] [PubMed] [Google Scholar]
- 6.Calabrese EJ. Key studies used to support cancer risk assessment questioned. Environ Mol Mutagen. 2011;52:595–606. doi: 10.1002/em.20662. [DOI] [PubMed] [Google Scholar]
- 7.Dauer LT, Brooks AL, Hoel DG, Morgan WF, Stram D, Tran P. Review and evaluation of updated research on the health effects associated with low-dose ionising radiation. Radiat Prot Dosimetry. 2010;140:103–136. doi: 10.1093/rpd/ncq141. [DOI] [PubMed] [Google Scholar]
- 8.Calabrese EJ, O’Connor MK. Estimating risk of low radiation doses - a critical review of the BEIR VII report and its use of the linear no-threshold (LNT) hypothesis. Radiat Res. 2014;182:463–474. doi: 10.1667/RR13829.1. [DOI] [PubMed] [Google Scholar]
- 9.National Research Council (US) Committee to Assess Health Risks from Exposure to Low Level of Ionizing Radiation. Health risks from exposure to low levels of ionizing radiation: BEIR VII Phase 2. Washington, D.C.: The National Academies Press; 2006. [PubMed] [Google Scholar]
- 10.ICRP. Low-dose extrapolation of radiation-related cancer risk. ICRP Publication 99. Ann ICRP. 2005;35:1–141. doi: 10.1016/j.icrp.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Tubiana M, Aurengo A, Averbeck D, Bonin A, Le Guen B, Masse R, Monier R, Valleron AJ, de Vathaire F. Dose-effect relationships and estimation of the carcinogenic effect of low doses of ionizing radiation. Paris: Académie des Sciences - Académie National de Médicine; 2005. [Google Scholar]
- 12.United Nations Scientific Committee on the Effects of Atomic Radiation. Biological mechanisms of radiation actions at low doses: a white paper to guide the Scientific Committee's future programme of work. New York, NY: United Nations; 2012. [Google Scholar]
- 13.Goodhead DT. Understanding and characterisation of the risks to human health from exposure to low levels of radiation. Radiat Prot Dosimetry. 2009;137:109–117. doi: 10.1093/rpd/ncp191. [DOI] [PubMed] [Google Scholar]
- 14.Kadhim M, Salomaa S, Wright E, Hildebrandt G, Belyakov OV, Prise KM, Little MP. Non-targeted effects of ionising radiation--implications for low dose risk. Mutat Res. 2013;752:84–98. doi: 10.1016/j.mrrev.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ICRP Statement on Tissue Reactions and Early and Late Effects of Radiation in Normal Tissues and Organs - Threshold Doses for Tissue Reactions in a Radiation Protection Context. ICRP Publication 118. Ann ICRP. 2012;41:1–322. doi: 10.1016/j.icrp.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 16.Vaiserman AM. Radiation hormesis: historical perspective and implications for low-dose cancer risk assessment. Dose Response. 2010;8:172–191. doi: 10.2203/dose-response.09-037.Vaiserman. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.ICRP The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37:1–332. doi: 10.1016/j.icrp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 18.International Commission on Radiological Protection. Radiation protection; recommendations. Adopted September 9, 1958. London: Pergamon; 1959. [Google Scholar]
- 19.Prekeges JL. Radiation hormesis, or, could all that radiation be good for us? J Nucl Med Technol. 2003;31:11–17. [PubMed] [Google Scholar]
- 20.Finch SC. Leukemia: lessons from the Japanese experience. Stem Cells. 1997;15(Suppl 2):135–139. doi: 10.1002/stem.5530150720. [DOI] [PubMed] [Google Scholar]
- 21.Smith LG, Miller RC, Richards M, Brenner DJ, Hall EJ. Investigation of hypersensitivity to fractionated low-dose radiation exposure. Int J Radiat Oncol Biol Phys. 1999;45:187–191. doi: 10.1016/s0360-3016(99)00143-1. [DOI] [PubMed] [Google Scholar]
- 22.Krueger SA, Collis SJ, Joiner MC, Wilson GD, Marples B. Transition in survival from low-dose hyper-radiosensitivity to increased radioresistance is independent of activation of ATM Ser1981 activity. Int J Radiat Oncol Biol Phys. 2007;69:1262–1271. doi: 10.1016/j.ijrobp.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 23.Feinendegen LE. Evidence for beneficial low level radiation effects and radiation hormesis. Br J Radiol. 2005;78:3–7. doi: 10.1259/bjr/63353075. [DOI] [PubMed] [Google Scholar]
- 24.Redpath JL. Radiation-induced neoplastic transformation in vitro: evidence for a protective effect at low doses of low LET radiation. Cancer Metastasis Rev. 2004;23:333–339. doi: 10.1023/B:CANC.0000031771.56142.9b. [DOI] [PubMed] [Google Scholar]
- 25.Azzam EI, de Toledo SM, Raaphorst GP, Mitchel RE. Low-dose ionizing radiation decreases the frequency of neoplastic transformation to a level below the spontaneous rate in C3H 10T1/2 cells. Radiat Res. 1996;146:369–373. [PubMed] [Google Scholar]
- 26.Sancar A, Lindsey-Boltz LA, Unsal-Kaçmaz K, Linn S. Molecular mechanisms of mammalian DNA repair and the DNA damage checkpoints. Annu Rev Biochem. 2004;73:39–85. doi: 10.1146/annurev.biochem.73.011303.073723. [DOI] [PubMed] [Google Scholar]
- 27.Dikomey E, Brammer I. Relationship between cellular radiosensitivity and non-repaired double-strand breaks studied for different growth states, dose rates and plating conditions in a normal human fibroblast line. Int J Radiat Biol. 2000;76:773–781. doi: 10.1080/09553000050028922. [DOI] [PubMed] [Google Scholar]
- 28.Zeng G, Day TK, Hooker AM, Blyth BJ, Bhat M, Tilley WD, Sykes PJ. Non-linear chromosomal inversion response in prostate after low dose X-radiation exposure. Mutat Res. 2006;602:65–73. doi: 10.1016/j.mrfmmm.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 29.Columbano A, Endoh T, Denda A, Noguchi O, Nakae D, Hasegawa K, Ledda-Columbano GM, Zedda AI, Konishi Y. Effects of cell proliferation and cell death (apoptosis and necrosis) on the early stages of rat hepatocarcinogenesis. Carcinogenesis. 1996;17:395–400. doi: 10.1093/carcin/17.3.395. [DOI] [PubMed] [Google Scholar]
- 30.Löbrich M, Rief N, Kühne M, Heckmann M, Fleckenstein J, Rübe C, Uder M. In vivo formation and repair of DNA double-strand breaks after computed tomography examinations. Proc Natl Acad Sci U S A. 2005;102:8984–8989. doi: 10.1073/pnas.0501895102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mothersill C, Seymour CB. Radiation-induced bystander effects and the DNA paradigm: an “out of field” perspective. Mutat Res. 2006;597:5–10. doi: 10.1016/j.mrfmmm.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 32.Schettino G, Folkard M, Michael BD, Prise KM. Low-dose binary behavior of bystander cell killing after microbeam irradiation of a single cell with focused c(k) x rays. Radiat Res. 2005;163:332–336. doi: 10.1667/rr3319. [DOI] [PubMed] [Google Scholar]
- 33.Huang L, Kim PM, Nickoloff JA, Morgan WF. Targeted and nontargeted effects of low-dose ionizing radiation on delayed genomic instability in human cells. Cancer Res. 2007;67:1099–1104. doi: 10.1158/0008-5472.CAN-06-3697. [DOI] [PubMed] [Google Scholar]
- 34.Okada M, Okabe A, Uchihori Y, Kitamura H, Sekine E, Ebisawa S, Suzuki M, Okayasu R. Single extreme low dose/low dose rate irradiation causes alteration in lifespan and genome instability in primary human cells. Br J Cancer. 2007;96:1707–1710. doi: 10.1038/sj.bjc.6603775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lefèvre SH, Vogt N, Dutrillaux AM, Chauveinc L, Stoppa-Lyonnet D, Doz F, Desjardins L, Dutrillaux B, Chevillard S, Malfoy B. Genome instability in secondary solid tumors developing after radiotherapy of bilateral retinoblastoma. Oncogene. 2001;20:8092–8099. doi: 10.1038/sj.onc.1205009. [DOI] [PubMed] [Google Scholar]
- 36.Salomaa S, Holmberg K, Lindholm C, Mustonen R, Tekkel M, Veidebaum T, Lambert B. Chromosomal instability in in vivo radiation exposed subjects. Int J Radiat Biol. 1998;74:771–779. doi: 10.1080/095530098141050. [DOI] [PubMed] [Google Scholar]
- 37.Tawn EJ, Whitehouse CA, Winther JF, Curwen GB, Rees GS, Stovall M, Olsen JH, Guldberg P, Rechnitzer C, Schrøder H, et al. Chromosome analysis in childhood cancer survivors and their offspring--no evidence for radiotherapy-induced persistent genomic instability. Mutat Res. 2005;583:198–206. doi: 10.1016/j.mrgentox.2005.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakanishi M, Tanaka K, Takahashi T, Kyo T, Dohy H, Fujiwara M, Kamada N. Microsatellite instability in acute myelocytic leukaemia developed from A-bomb survivors. Int J Radiat Biol. 2001;77:687–694. doi: 10.1080/095530000110047537. [DOI] [PubMed] [Google Scholar]
- 39.Barquinero JF, Barrios L, Caballín MR, Miró R, Ribas M, Subias A, Egozcue J. Occupational exposure to radiation induces an adaptive response in human lymphocytes. Int J Radiat Biol. 1995;67:187–191. doi: 10.1080/09553009514550231. [DOI] [PubMed] [Google Scholar]
- 40.Stoilov LM, Mullenders LH, Darroudi F, Natarajan AT. Adaptive response to DNA and chromosomal damage induced by X-rays in human blood lymphocytes. Mutagenesis. 2007;22:117–122. doi: 10.1093/mutage/gel061. [DOI] [PubMed] [Google Scholar]
- 41.Carbone MC, Pinto M, Antonelli F, Amicarelli F, Balata M, Belli M, Conti Devirgiliis L, Ioannucci L, Nisi S, Sapora O, et al. The Cosmic Silence experiment: on the putative adaptive role of environmental ionizing radiation. Radiat Environ Biophys. 2009;48:189–196. doi: 10.1007/s00411-008-0208-6. [DOI] [PubMed] [Google Scholar]
- 42.Wolff S. Aspects of the adaptive response to very low doses of radiation and other agents. Mutat Res. 1996;358:135–142. doi: 10.1016/s0027-5107(96)00114-5. [DOI] [PubMed] [Google Scholar]
- 43.Calabrese EJ. Hormesis: from marginalization to mainstream: a case for hormesis as the default dose-response model in risk assessment. Toxicol Appl Pharmacol. 2004;197:125–136. doi: 10.1016/j.taap.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 44.Seong KM, Kim CS, Seo SW, Jeon HY, Lee BS, Nam SY, Yang KH, Kim JY, Kim CS, Min KJ, et al. Genome-wide analysis of low-dose irradiated male Drosophila melanogaster with extended longevity. Biogerontology. 2011;12:93–107. doi: 10.1007/s10522-010-9295-2. [DOI] [PubMed] [Google Scholar]
- 45.Calabrese EJ, Iavicoli I, Calabrese V. Hormesis: why it is important to biogerontologists. Biogerontology. 2012;13:215–235. doi: 10.1007/s10522-012-9374-7. [DOI] [PubMed] [Google Scholar]
- 46.Seong KM, Kim CS, Lee BS, Nam SY, Yang KH, Kim JY, Park JJ, Min KJ, Jin YW. Low-dose radiation induces Drosophila innate immunity through Toll pathway activation. J Radiat Res (Tokyo) 2012;53:242–249. doi: 10.1269/jrr.11170. [DOI] [PubMed] [Google Scholar]
- 47.Hatchwell E, Greally JM. The potential role of epigenomic dysregulation in complex human disease. Trends Genet. 2007;23:588–595. doi: 10.1016/j.tig.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 48.Rugo RE, Schiestl RH. Increases in oxidative stress in the progeny of X-irradiated cells. Radiat Res. 2004;162:416–425. doi: 10.1667/rr3238. [DOI] [PubMed] [Google Scholar]
- 49.de Toledo SM, Asaad N, Venkatachalam P, Li L, Howell RW, Spitz DR, Azzam EI. Adaptive responses to low-dose/low-dose-rate gamma rays in normal human fibroblasts: the role of growth architecture and oxidative metabolism. Radiat Res. 2006;166:849–857. doi: 10.1667/RR0640.1. [DOI] [PubMed] [Google Scholar]
- 50.Marchetti F, Coleman MA, Jones IM, Wyrobek AJ. Candidate protein biodosimeters of human exposure to ionizing radiation. Int J Radiat Biol. 2006;82:605–639. doi: 10.1080/09553000600930103. [DOI] [PubMed] [Google Scholar]
- 51.Amundson SA. Functional genomics in radiation biology: a gateway to cellular systems-level studies. Radiat Environ Biophys. 2008;47:25–31. doi: 10.1007/s00411-007-0140-1. [DOI] [PubMed] [Google Scholar]
- 52.Goldberg Z, Rocke DM, Schwietert C, Berglund SR, Santana A, Jones A, Lehmann J, Stern R, Lu R, Hartmann Siantar C. Human in vivo dose-response to controlled, low-dose low linear energy transfer ionizing radiation exposure. Clin Cancer Res. 2006;12:3723–3729. doi: 10.1158/1078-0432.CCR-05-2625. [DOI] [PubMed] [Google Scholar]
- 53.Baverstock K, Rönkkö M. Epigenetic regulation of the mammalian cell. PLoS One. 2008;3:e2290. doi: 10.1371/journal.pone.0002290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gilbert ES. Ionising radiation and cancer risks: what have we learned from epidemiology? Int J Radiat Biol. 2009;85:467–482. doi: 10.1080/09553000902883836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.ICRP The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37:1–332. doi: 10.1016/j.icrp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 56.United Nations Scientific Committee on the Effects of Atomic Radiation. Report of the United Nations Scientific Committee on the effects of atomic radiation: fifty-seventh session, includes scientific report, summary of low-dose radiation effects on health. New York, NY: United Nations; 2011. [Google Scholar]
- 57.Ozasa K, Shimizu Y, Suyama A, Kasagi F, Soda M, Grant EJ, Sakata R, Sugiyama H, Kodama K. Studies of the mortality of atomic bomb survivors, Report 14, 1950-2003: an overview of cancer and noncancer diseases. Radiat Res. 2012;177:229–243. doi: 10.1667/rr2629.1. [DOI] [PubMed] [Google Scholar]
- 58.Likhtarov I, Kovgan L, Vavilov S, Chepurny M, Ron E, Lubin J, Bouville A, Tronko N, Bogdanova T, Gulak L, et al. Post-Chernobyl thyroid cancers in Ukraine. Report 2: risk analysis. Radiat Res. 2006;166:375–386. doi: 10.1667/RR3593.1. [DOI] [PubMed] [Google Scholar]
- 59.Jacob P, Bogdanova TI, Buglova E, Chepurniy M, Demidchik Y, Gavrilin Y, Kenigsberg J, Meckbach R, Schotola C, Shinkarev S, et al. Thyroid cancer risk in areas of Ukraine and Belarus affected by the Chernobyl accident. Radiat Res. 2006;165:1–8. doi: 10.1667/rr3479.1. [DOI] [PubMed] [Google Scholar]
- 60.Cardis E, Howe G, Ron E, Bebeshko V, Bogdanova T, Bouville A, Carr Z, Chumak V, Davis S, Demidchik Y, et al. Cancer consequences of the Chernobyl accident: 20 years on. J Radiol Prot. 2006;26:127–140. doi: 10.1088/0952-4746/26/2/001. [DOI] [PubMed] [Google Scholar]
- 61.UNSCEAR. Sources and effects of ionizing radiation vol. II: effects scientific annex D. Health effects due to radiation from the Chernobyl accident. UNSCEAR 2008 Report. New York, NY: United Nations; 2011. [Google Scholar]
- 62.Pukkala E, Kesminiene A, Poliakov S, Ryzhov A, Drozdovitch V, Kovgan L, Kyyrönen P, Malakhova IV, Gulak L, Cardis E. Breast cancer in Belarus and Ukraine after the Chernobyl accident. Int J Cancer. 2006;119:651–658. doi: 10.1002/ijc.21885. [DOI] [PubMed] [Google Scholar]
- 63.International Consortium for Research on the Health Effects of Radiation Writing Committee and Study Team Childhood leukaemia in Belarus, Russia, and Ukraine following the Chernobyl power station accident: results from an international collaborative population-based case-control study. Int J Epidemiol. 2006;35:386–396. doi: 10.1093/ije/dyi220. [DOI] [PubMed] [Google Scholar]
- 64.Ivanov EP, Tolochko GV, Shuvaeva LP, Ivanov VE, Iaroshevich RF, Becker S, Nekolla E, Kellerer AM. Infant leukemia in Belarus after the Chernobyl accident. Radiat Environ Biophys. 1998;37:53–55. doi: 10.1007/s004110050092. [DOI] [PubMed] [Google Scholar]
- 65.Kesminiene A, Cardis E, Tenet V, Ivanov VK, Kurtinaitis J, Malakhova I, Stengrevics A, Tekkel M. Studies of cancer risk among Chernobyl liquidators: materials and methods. J Radiol Prot. 2002;22:A137–41. doi: 10.1088/0952-4746/22/3a/324. [DOI] [PubMed] [Google Scholar]
- 66.Kesminiene A, Evrard AS, Ivanov VK, Malakhova IV, Kurtinaitis J, Stengrevics A, Tekkel M, Anspaugh LR, Bouville A, Chekin S, et al. Risk of hematological malignancies among Chernobyl liquidators. Radiat Res. 2008;170:721–735. doi: 10.1667/RR1231.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Romanenko AY, Finch SC, Hatch M, Lubin JH, Bebeshko VG, Bazyka DA, Gudzenko N, Dyagil IS, Reiss RF, Bouville A, et al. The Ukrainian-American study of leukemia and related disorders among Chornobyl cleanup workers from Ukraine: III. Radiation risks. Radiat Res. 2008;170:711–720. doi: 10.1667/RR1404.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ivanov VK. Late cancer and noncancer risks among Chernobyl emergency workers of Russia. Health Phys. 2007;93:470–479. doi: 10.1097/01.HP.0000282195.34508.b0. [DOI] [PubMed] [Google Scholar]
- 69.Cardis E, Hatch M. The Chernobyl accident--an epidemiological perspective. Clin Oncol (R Coll Radiol) 2011;23:251–260. doi: 10.1016/j.clon.2011.01.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hayashida N, Imaizumi M, Shimura H, Okubo N, Asari Y, Nigawara T, Midorikawa S, Kotani K, Nakaji S, Otsuru A, et al. Thyroid ultrasound findings in children from three Japanese prefectures: Aomori, Yamanashi and Nagasaki. PLoS One. 2013;8:e83220. doi: 10.1371/journal.pone.0083220. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 71.World Health Organization. Preliminary dose estimation from the nuclear accident after the 2011 Great East Japan Earthquake and Tsunami. Geneva: World Health Organization Press; 2012. [Google Scholar]
- 72.World Health Organization. Health risk assessment from the nuclear accident after the 2011 Great East Japan Earthquake and Tsunami, based on a preliminary dose estimation. Geneva: World Health Organization Press; 2013. [Google Scholar]
- 73.Harada KH, Niisoe T, Imanaka M, Takahashi T, Amako K, Fujii Y, Kanameishi M, Ohse K, Nakai Y, Nishikawa T, et al. Radiation dose rates now and in the future for residents neighboring restricted areas of the Fukushima Daiichi Nuclear Power Plant. Proc Natl Acad Sci U S A. 2014;111:E914–23. doi: 10.1073/pnas.1315684111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hatch MC, Wallenstein S, Beyea J, Nieves JW, Susser M. Cancer rates after the Three Mile Island nuclear accident and proximity of residence to the plant. Am J Public Health. 1991;81:719–724. doi: 10.2105/ajph.81.6.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wing S, Richardson D, Armstrong D, Crawford-Brown D. A reevaluation of cancer incidence near the Three Mile Island nuclear plant: the collision of evidence and assumptions. Environ Health Perspect. 1997;105:52–57. doi: 10.1289/ehp.9710552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Talbott EO, Youk AO, McHugh-Pemu KP, Zborowski JV. Long-term follow-up of the residents of the Three Mile Island accident area: 1979-1998. Environ Health Perspect. 2003;111:341–348. doi: 10.1289/ehp.5662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cardis E, Vrijheid M, Blettner M, Gilbert E, Hakama M, Hill C, Howe G, Kaldor J, Muirhead CR, Schubauer-Berigan M, et al. The 15-country collaborative study of cancer risk among radiation workers in the nuclear industry: estimates of radiation-related cancer risks. Radiat Res. 2007;167:396–416. doi: 10.1667/RR0553.1. [DOI] [PubMed] [Google Scholar]
- 78.Shilnikova NS, Preston DL, Ron E, Gilbert ES, Vassilenko EK, Romanov SA, Kuznetsova IS, Sokolnikov ME, Okatenko PV, Kreslov VV, et al. Cancer mortality risk among workers at the Mayak nuclear complex. Radiat Res. 2003;159:787–798. doi: 10.1667/0033-7587(2003)159[0787:cmrawa]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 79.Gilbert ES, Koshurnikova NA, Sokolnikov ME, Shilnikova NS, Preston DL, Ron E, Okatenko PV, Khokhryakov VF, Vasilenko EK, Miller S, et al. Lung cancer in Mayak workers. Radiat Res. 2004;162:505–516. doi: 10.1667/rr3259. [DOI] [PubMed] [Google Scholar]
- 80.Hunter N, Kuznetsova IS, Labutina EV, Harrison JD. Solid cancer incidence other than lung, liver and bone in Mayak workers: 1948-2004. Br J Cancer. 2013;109:1989–1996. doi: 10.1038/bjc.2013.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Richardson DB, Wing S. Leukemia mortality among workers at the Savannah River Site. Am J Epidemiol. 2007;166:1015–1022. doi: 10.1093/aje/kwm176. [DOI] [PubMed] [Google Scholar]
- 82.Matanoski GM, Tonascia JA, Correa-Villaseñor A, Yates KC, Fink N, Elliott E, Sanders B, Lantry D. Cancer risks and low-level radiation in U.S. shipyard workers. J Radiat Res (Tokyo) 2008;49:83–91. doi: 10.1269/jrr.06082. [DOI] [PubMed] [Google Scholar]
- 83.Metz-Flamant C, Laurent O, Samson E, Caër-Lorho S, Acker A, Hubert D, Richardson DB, Laurier D. Mortality associated with chronic external radiation exposure in the French combined cohort of nuclear workers. Occup Environ Med. 2013;70:630–638. doi: 10.1136/oemed-2012-101149. [DOI] [PubMed] [Google Scholar]
- 84.Akiba S, Mizuno S. The third analysis of cancer mortality among Japanese nuclear workers, 1991-2002: estimation of excess relative risk per radiation dose. J Radiol Prot. 2012;32:73–83. doi: 10.1088/0952-4746/32/1/73. [DOI] [PubMed] [Google Scholar]
- 85.Zeeb H, Hammer GP, Blettner M. Epidemiological investigations of aircrew: an occupational group with low-level cosmic radiation exposure. J Radiol Prot. 2012;32:N15–N19. doi: 10.1088/0952-4746/32/1/N15. [DOI] [PubMed] [Google Scholar]
- 86.Pukkala E, Auvinen A, Wahlberg G. Incidence of cancer among Finnish airline cabin attendants, 1967-92. BMJ. 1995;311:649–652. doi: 10.1136/bmj.311.7006.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rafnsson V, Sulem P, Tulinius H, Hrafnkelsson J. Breast cancer risk in airline cabin attendants: a nested case-control study in Iceland. Occup Environ Med. 2003;60:807–809. doi: 10.1136/oem.60.11.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Reynolds P, Cone J, Layefsky M, Goldberg DE, Hurley S. Cancer incidence in California flight attendants (United States) Cancer Causes Control. 2002;13:317–324. doi: 10.1023/a:1015284014563. [DOI] [PubMed] [Google Scholar]
- 89.Wartenberg D, Stapleton CP. Risk of breast cancer is also increased among retired US female airline cabin attendants. BMJ. 1998;316:1902. doi: 10.1136/bmj.316.7148.1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pukkala E, Aspholm R, Auvinen A, Eliasch H, Gundestrup M, Haldorsen T, Hammar N, Hrafnkelsson J, Kyyrönen P, Linnersjö A, et al. Incidence of cancer among Nordic airline pilots over five decades: occupational cohort study. BMJ. 2002;325:567. doi: 10.1136/bmj.325.7364.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Band PR, Spinelli JJ, Ng VT, Moody J, Gallagher RP. Mortality and cancer incidence in a cohort of commercial airline pilots. Aviat Space Environ Med. 1990;61:299–302. [PubMed] [Google Scholar]
- 92.Pinkerton LE, Waters MA, Hein MJ, Zivkovich Z, Schubauer-Berigan MK, Grajewski B. Cause-specific mortality among a cohort of U.S. flight attendants. Am J Ind Med. 2012;55:25–36. doi: 10.1002/ajim.21011. [DOI] [PubMed] [Google Scholar]
- 93.Band PR, Le ND, Fang R, Deschamps M, Coldman AJ, Gallagher RP, Moody J. Cohort study of Air Canada pilots: mortality, cancer incidence, and leukemia risk. Am J Epidemiol. 1996;143:137–143. doi: 10.1093/oxfordjournals.aje.a008722. [DOI] [PubMed] [Google Scholar]
- 94.Hammer GP, Auvinen A, De Stavola BL, Grajewski B, Gundestrup M, Haldorsen T, Hammar N, Lagorio S, Linnersjö A, Pinkerton L, et al. Mortality from cancer and other causes in commercial airline crews: a joint analysis of cohorts from 10 countries. Occup Environ Med. 2014;71:313–322. doi: 10.1136/oemed-2013-101395. [DOI] [PubMed] [Google Scholar]
- 95.Yong LC, Pinkerton LE, Yiin JH, Anderson JL, Deddens JA. Mortality among a cohort of U.S. commercial airline cockpit crew. Am J Ind Med. 2014;57:906–914. doi: 10.1002/ajim.22318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zeeb H, Blettner M, Langner I, Hammer GP, Ballard TJ, Santaquilani M, Gundestrup M, Storm H, Haldorsen T, Tveten U, et al. Mortality from cancer and other causes among airline cabin attendants in Europe: a collaborative cohort study in eight countries. Am J Epidemiol. 2003;158:35–46. doi: 10.1093/aje/kwg107. [DOI] [PubMed] [Google Scholar]
- 97.Muirhead CR, O’Hagan JA, Haylock RG, Phillipson MA, Willcock T, Berridge GL, Zhang W. Mortality and cancer incidence following occupational radiation exposure: third analysis of the National Registry for Radiation Workers. Br J Cancer. 2009;100:206–212. doi: 10.1038/sj.bjc.6604825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ahn YS, Park RM, Koh DH. Cancer admission and mortality in workers exposed to ionizing radiation in Korea. J Occup Environ Med. 2008;50:791–803. doi: 10.1097/JOM.0b013e318167751d. [DOI] [PubMed] [Google Scholar]
- 99.Zablotska LB, Lane RS, Thompson PA. A reanalysis of cancer mortality in Canadian nuclear workers (1956-1994) based on revised exposure and cohort data. Br J Cancer. 2014;110:214–223. doi: 10.1038/bjc.2013.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Howe GR, Zablotska LB, Fix JJ, Egel J, Buchanan J. Analysis of the mortality experience amongst U.S. nuclear power industry workers after chronic low-dose exposure to ionizing radiation. Radiat Res. 2004;162:517–526. doi: 10.1667/rr3258. [DOI] [PubMed] [Google Scholar]
- 101.Jeong M, Jin YW, Yang KH, Ahn YO, Cha CY. Radiation exposure and cancer incidence in a cohort of nuclear power industry workers in the Republic of Korea, 1992-2005. Radiat Environ Biophys. 2010;49:47–55. doi: 10.1007/s00411-009-0247-7. [DOI] [PubMed] [Google Scholar]
- 102.Merzenich H, Hammer GP, Tröltzsch K, Ruecker K, Buncke J, Fehringer F, Blettner M. Mortality risk in a historical cohort of nuclear power plant workers in Germany: results from a second follow-up. Radiat Environ Biophys. 2014;53:405–416. doi: 10.1007/s00411-014-0523-z. [DOI] [PubMed] [Google Scholar]
- 103.United Nations Scientific Committee on the Effects of Atomic Radiation. UNSCEAR 2000 Report. Sources and effects of ionizing radiation: United Nations Scientific Committee on the Effects of Atomic Radiation UNSCEAR 2000 Report to the General Assembly, with scientific annexes. Vol. I: Sources. New York, NY: United Nations; 2001. Annex B. Exposures from natural radiation sources. [Google Scholar]
- 104.Ghiassi-Nejad M, Mortazavi SM, Cameron JR, Niroomand-rad A, Karam PA. Very high background radiation areas of Ramsar, Iran: preliminary biological studies. Health Phys. 2002;82:87–93. doi: 10.1097/00004032-200201000-00011. [DOI] [PubMed] [Google Scholar]
- 105.Hayata I, Wang C, Zhang W, Chen D, Minamihisamatsu M, Morishima H, Wei L, Sugahara T. Effect of high-level natural radiation on chromosomes of residents in southern China. Cytogenet Genome Res. 2004;104:237–239. doi: 10.1159/000077496. [DOI] [PubMed] [Google Scholar]
- 106.Ghiassi-Nejad M, Zakeri F, Assaei RG, Kariminia A. Long-term immune and cytogenetic effects of high level natural radiation on Ramsar inhabitants in Iran. J Environ Radioact. 2004;74:107–116. doi: 10.1016/j.jenvrad.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 107.Nair RR, Rajan B, Akiba S, Jayalekshmi P, Nair MK, Gangadharan P, Koga T, Morishima H, Nakamura S, Sugahara T. Background radiation and cancer incidence in Kerala, India-Karanagappally cohort study. Health Phys. 2009;96:55–66. doi: 10.1097/01.HP.0000327646.54923.11. [DOI] [PubMed] [Google Scholar]
- 108.Tao Z, Akiba S, Zha Y, Sun Q, Zou J, Li J, Liu Y, Yuan Y, Tokonami S, Morishoma H, et al. Cancer and non-cancer mortality among Inhabitants in the high background radiation area of Yangjiang, China (1979-1998) Health Phys. 2012;102:173–181. doi: 10.1097/HP.0b013e31822c7f1e. [DOI] [PubMed] [Google Scholar]
- 109.Zou J, Tao Z, Sun Q, Akiba S, Zha Y, Sugahara T, Wei L. Cancer and non-cancer epidemiological study in the high background radiation area of Yangjiang, China. Int Congr Ser. 2005;1276:97–101. [Google Scholar]
- 110.Wei LX, Zha YR, Tao ZF, He WH, Chen DQ, Yuan YL. Epidemiological investigation of radiological effects in high background radiation areas of Yangjiang, China. J Radiat Res (Tokyo) 1990;31:119–136. [PubMed] [Google Scholar]
- 111.Krestinina LY, Davis F, Ostroumova E, Epifanova S, Degteva M, Preston D, Akleyev A. Solid cancer incidence and low-dose-rate radiation exposures in the Techa River cohort: 1956 2002. Int J Epidemiol. 2007;36:1038–1046. doi: 10.1093/ije/dym121. [DOI] [PubMed] [Google Scholar]
- 112.Krestinina L, Preston DL, Davis FG, Epifanova S, Ostroumova E, Ron E, Akleyev A. Leukemia incidence among people exposed to chronic radiation from the contaminated Techa River, 1953-2005. Radiat Environ Biophys. 2010;49:195–201. doi: 10.1007/s00411-009-0257-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ostroumova E, Preston DL, Ron E, Krestinina L, Davis FG, Kossenko M, Akleyev A. Breast cancer incidence following low-dose rate environmental exposure: Techa River Cohort, 1956-2004. Br J Cancer. 2008;99:1940–1945. doi: 10.1038/sj.bjc.6604775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Schonfeld SJ, Krestinina LY, Epifanova S, Degteva MO, Akleyev AV, Preston DL. Solid cancer mortality in the Techa river cohort (1950-2007) Radiat Res. 2013;179:183–189. doi: 10.1667/RR2932.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Standring WJ, Dowdall M, Strand P. Overview of dose assessment developments and the health of riverside residents close to the “Mayak” PA facilities, Russia. Int J Environ Res Public Health. 2009;6:174–199. doi: 10.3390/ijerph6010174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hwang SL, Hwang JS, Yang YT, Hsieh WA, Chang TC, Guo HR, Tsai MH, Tang JL, Lin IF, Chang WP. Estimates of relative risks for cancers in a population after prolonged low-dose-rate radiation exposure: a follow-up assessment from 1983 to 2005. Radiat Res. 2008;170:143–148. doi: 10.1667/RR0732.1. [DOI] [PubMed] [Google Scholar]
- 117.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, Howe NL, Ronckers CM, Rajaraman P, Sir Craft AW, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, Giles GG, Wallace AB, Anderson PR, Guiver TA, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:f2360. doi: 10.1136/bmj.f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.de Gelder R, Draisma G, Heijnsdijk EA, de Koning HJ. Population-based mammography screening below age 50: balancing radiation-induced vs prevented breast cancer deaths. Br J Cancer. 2011;104:1214–1220. doi: 10.1038/bjc.2011.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yaffe MJ, Mainprize JG. Risk of radiation-induced breast cancer from mammographic screening. Radiology. 2011;258:98–105. doi: 10.1148/radiol.10100655. [DOI] [PubMed] [Google Scholar]
- 121.Berrington de González A, Kim KP, Knudsen AB, Lansdorp-Vogelaar I, Rutter CM, Smith-Bindman R, Yee J, Kuntz KM, van Ballegooijen M, Zauber AG, et al. Radiation-related cancer risks from CT colonography screening: a risk-benefit analysis. AJR Am J Roentgenol. 2011;196:816–823. doi: 10.2214/AJR.10.4907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Albert JM. Radiation risk from CT: implications for cancer screening. AJR Am J Roentgenol. 2013;201:W81-7. doi: 10.2214/AJR.12.9226. [DOI] [PubMed] [Google Scholar]
- 123.Andrieu N, Easton DF, Chang-Claude J, Rookus MA, Brohet R, Cardis E, Antoniou AC, Wagner T, Simard J, Evans G, et al. Effect of chest X-rays on the risk of breast cancer among BRCA1/2 mutation carriers in the international BRCA1/2 carrier cohort study: a report from the EMBRACE, GENEPSO, GEO-HEBON, and IBCCS Collaborators’ Group. J Clin Oncol. 2006;24:3361–3366. doi: 10.1200/JCO.2005.03.3126. [DOI] [PubMed] [Google Scholar]
- 124.Gronwald J, Pijpe A, Byrski T, Huzarski T, Stawicka M, Cybulski C, van Leeuwen F, Lubiński J, Narod SA. Early radiation exposures and BRCA1-associated breast cancer in young women from Poland. Breast Cancer Res Treat. 2008;112:581–584. doi: 10.1007/s10549-008-9892-9. [DOI] [PubMed] [Google Scholar]
- 125.Lecarpentier J, Noguès C, Mouret-Fourme E, Stoppa-Lyonnet D, Lasset C, Caron O, Fricker JP, Gladieff L, Faivre L, Sobol H, et al. Variation in breast cancer risk with mutation position, smoking, alcohol, and chest X-ray history, in the French National BRCA1/2 carrier cohort (GENEPSO) Breast Cancer Res Treat. 2011;130:927–938. doi: 10.1007/s10549-011-1655-3. [DOI] [PubMed] [Google Scholar]
- 126.Pijpe A, Andrieu N, Easton DF, Kesminiene A, Cardis E, Noguès C, Gauthier-Villars M, Lasset C, Fricker JP, Peock S, et al. Exposure to diagnostic radiation and risk of breast cancer among carriers of BRCA1/2 mutations: retrospective cohort study (GENE-RAD-RISK) BMJ. 2012;345:e5660. doi: 10.1136/bmj.e5660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.John EM, McGuire V, Thomas D, Haile R, Ozcelik H, Milne RL, Felberg A, West DW, Miron A, Knight JA, et al. Diagnostic chest X-rays and breast cancer risk before age 50 years for BRCA1 and BRCA2 mutation carriers. Cancer Epidemiol Biomarkers Prev. 2013;22:1547–1556. doi: 10.1158/1055-9965.EPI-13-0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Goldfrank D, Chuai S, Bernstein JL, Ramon Y, Cajal T, Lee JB, Alonso MC, Diez O, Baiget M, Kauff ND, et al. Effect of mammography on breast cancer risk in women with mutations in BRCA1 or BRCA2. Cancer Epidemiol Biomarkers Prev. 2006;15:2311–2313. doi: 10.1158/1055-9965.EPI-06-0176. [DOI] [PubMed] [Google Scholar]
- 129.Narod SA, Lubinski J, Ghadirian P, Lynch HT, Moller P, Foulkes WD, Rosen B, Kim-Sing C, Isaacs C, Domchek S, et al. Screening mammography and risk of breast cancer in BRCA1 and BRCA2 mutation carriers: a case-control study. Lancet Oncol. 2006;7:402–406. doi: 10.1016/S1470-2045(06)70624-6. [DOI] [PubMed] [Google Scholar]
- 130.National Research Council (US) Committee on an Assessment of CDC Radiation Studies. Radiation dose reconstruction for epidemiologic uses. Washington, D.C.: National Academy Press; 1995. [Google Scholar]
- 131.Gilbert ES. The impact of dosimetry uncertainties on dose-response analyses. Health Phys. 2009;97:487–492. doi: 10.1097/HP.0b013e3181adc3b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.National Council on Radiation Protection and Measurements. Uncertainties in the estimation of radiation risks and probability of disease causation, NCRP Report No. 171. Bethesda, MD: National Council on Radiation Protection and Measurements; 2012. [Google Scholar]
- 133.Committee on Research Directions in Human Biological Effects of Low-Level Ionizing Radiation; Institute of Medicine (US), Board on the Health of Select Populations; National Research Council (US), Nuclear and Radiation Studies Board. Research on health effects of low-level ionizing radiation exposure: opportunities for the Armed Forces Radiobiology Research Institute. Washington, D.C.: National Academies Press; 2014. [Google Scholar]
- 134.Leuraud K, Richardson DB, Cardis E, Daniels RD, Gillies M, O’Hagan JA, Hamra GB, Haylock R, Laurier D, Moissonnier M, et al. Ionising radiation and risk of death from leukaemia and lymphoma in radiation-monitored workers (INWORKS): an international cohort study. Lancet Haematol. 2015;2:e276–81. doi: 10.1016/S2352-3026(15)00094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cook R, Calabrese EJ. The importance of hormesis to public health. Cien Saude Colet. 2007;12:955–963. doi: 10.1590/s1413-81232007000400017. [DOI] [PubMed] [Google Scholar]
- 136.Calabrese EJ, Shamoun DY, Hanekamp JC. Cancer risk assessment: Optimizing human health through linear dose-response models. Food Chem Toxicol. 2015;81:137–140. doi: 10.1016/j.fct.2015.04.023. [DOI] [PubMed] [Google Scholar]