Abstract
Objective
The study’s objectives were to calculate the costs and evaluate the cost-effectiveness of implementing a health literacy-focused intervention to promote breast and cervical cancer screenings among Korean American women overdue for these tests
Methods
Researchers estimated the costs of a cluster-randomized controlled trial that evaluated this intervention. Effectiveness was measured as the number of breast or cervical cancer screenings received by women in either the intervention and control arms of the study. Cost-effectiveness was calculated as the incremental cost of each additional screening received by the intervention group.
Results
Comparing the intervention and control group, the incremental cost-effectiveness ratio was estimated to be US$236 per screening, without program development costs.
Conclusion
These findings suggest this program, when compared with others, offered a more cost-effective approach for promoting cancer screening. Local health officials could use this information to guide decisions about reducing cancer disparities among recent immigrant women.
Keywords: Health literacy, Korean American, costs, cost effectiveness, community health workers
In the U.S. the Asian population is one of the fastest growing racial and ethnic groups.1 Asian American women have lower breast and cervical cancer screening rates than other U.S. racial and ethnic groups.2,3 When we disaggregate the Asian American group, studies suggest that Korean Americans are least likely to receive either of the screenings within the recommended time frame.4,5 Mammograms and Pap tests are critical strategies to detect breast and cervical cancer at early stages and they have been shown to be effective in reducing the risk of death.6 There is a broader range of treatment options available when cancer is detected earlier, and more costly and aggressive therapies may be averted as a result of an earlier diagnosis.2,3
The disparity in screening rates among Asian American women, and Korean American women in particular, is reflected in high cancer incidence and mortality rates. Between 2000 and 2009, incidence rates for breast cancer in the U.S. declined among White women, and incidence rates of cervical cancer declined for all women in the U.S.7 During this same time frame, however, breast cancer incidence rates increased for Asian American women.7 Furthermore, in comparison with other Asian American ethnic groups, Korean American women experience the second highest cervical cancer incidence and mortality rates.5
While interventions exist that aim to increase cancer screening rates, evidence suggests that promoting culturally-tailored and theory-based cancer screening interventions for ethnic minority women are more effective than non-tailored interventions.8 This is particularly relevant when considering that health literacy—a person’s ability to make appropriate health decisions by gathering, processing, and understanding basic health information and services9—is emerging as a far-reaching social determinant of health. Poor health literacy has been linked to inadequate utilization of preventive services such as cancer screening.10 In the U.S., where health information is primarily available in English, non-English speaking people are more apt to experience lower health literacy,9 which is relevant here since a majority of Korean Americans are foreign-born and monolingual.11
A health literacy-focused intervention was developed to improve breast and cervical cancer screening among Korean American women. In addition, the intervention was designed to engage community members because research shows that cancer screening participation rates improve when community members are involved with delivering the intervention.12
Whereas the effectiveness of interventions’ ability to increase the use of cancer screening traditionally has been examined, the field is generally lacking in terms of its understanding of the cost-effectiveness of such interventions and few studies have provided evidence on the cost-effectiveness of tailored, culturally-specific interventions for improving cancer-screening.6 To address this gap, we evaluated the cost-effectiveness of the aforementioned health literacy-focused intervention. We used a health care system perspective to account for the resources required to motivate screening uptake and to reflect the information that had been collected and was available from this RCT. Communities that have large numbers of Asian American women, or populations that have limited health literacy and who want to develop and implement a similar intervention, will find this study useful.
Methods
Design
A community-based, cluster-randomized controlled trial (RCT) was conducted among Korean American women who attended one of 23 ethnic churches in the Baltimore-Washington metropolitan area. Churches were randomized to one of two intervention conditions: immediate intervention vs. wait-list control. The churches were chosen to be the study recruitment and intervention site because a large majority of Korean American women regularly attend church. In brief, community health workers (CHWs) from the participating churches were trained to recruit Korean American women to participate in a six-month trial and deliver the study intervention. The intervention consisted of the following components: 1) individually tailored health information, 2) health literacy group education, 3) telephone counseling, and 4) navigation assistance, all delivered by trained CHWs except for the first component. We used the PRECEDE-PROCEED model, which guided the planning and evaluation of our intervention.13 The comprehensive model addresses predisposing, enabling, and reinforcing factors consistently found to affect cancer screening behaviors. The inclusion criteria specified that participants had to be: 1) 21 to 65 years old; 2) self-identified as Korean American women; 3) had not had a mammogram (for women aged 40 years and older only) or Pap test within the last 24 months; 4) able to read and write Korean or English; and 5) willing to provide written consent to allow researchers to audit medical records for mammography and Pap test usage. Women were excluded from the study if they had received a cancer or psychiatric diagnosis, or if they had an acute or terminal health condition. A total of 560 eligible Korean American women were enrolled and completed a study questionnaire at baseline. The majority of women (n=336) were overdue for both screening tests at baseline, whereas 63 women were overdue for a mammogram and 161 for a Pap test at baseline. At six months follow-up, 527 women participated in the final data collection.
Procedures
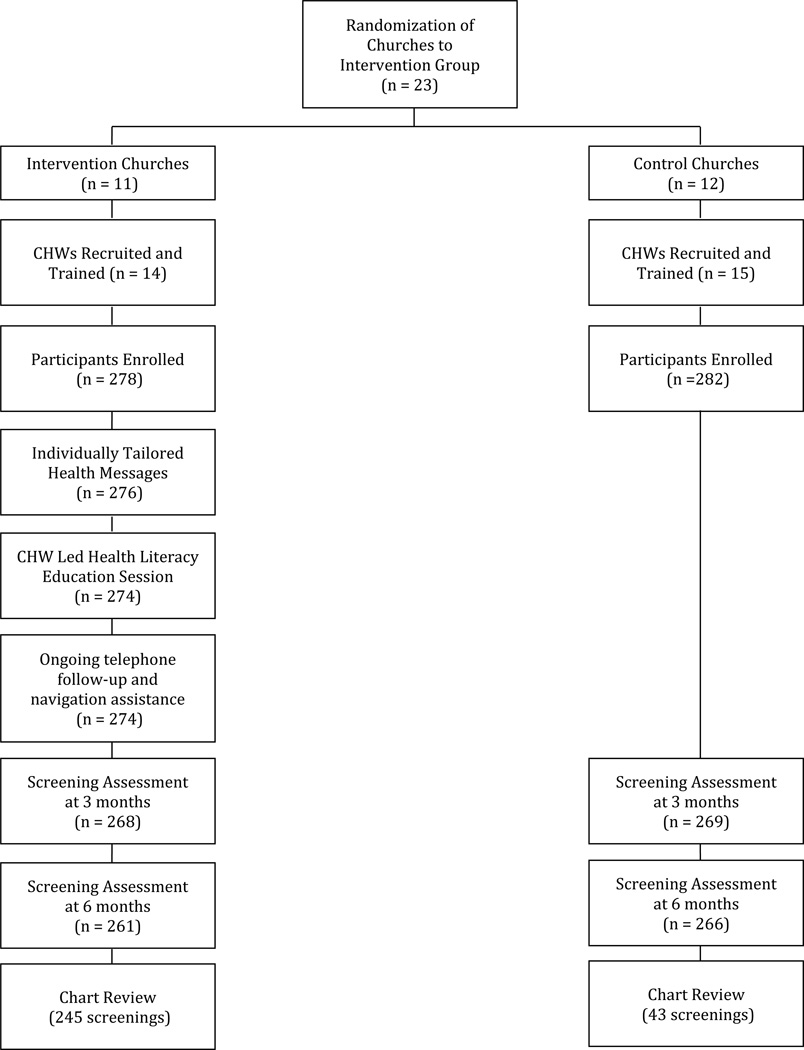
The Johns Hopkins Medicine Institutional Review Board approved all study procedures. Figure 1 shows detailed study procedures. CHWs from the participating churches were recruited based on interest, availability, and commitment to this project. CHWs received training according to their church intervention group assignment (i.e., immediate intervention vs. wait-list control). Those in the intervention group received a three-day training, while those in the control group received a one-day training.
Figure 1.
CHW Health Literacy Intervention Flowchart
Within one to two weeks of completing a baseline assessment from which individual risk factors for breast and cervical cancers were identified, participants in the immediate intervention group received a brochure containing specific health messages and information tailored to individual risk factors and education levels that were generated by a computerized system. Trained CHWs then delivered a two-hour health literacy education session in which participants learned and practiced using medical terminology and saying medical dialogues in English that are used in the context of breast and cervical cancer screening. At the end of the education session, participants received a DVD and a picture guidebook that detailed the health literacy content covered in the class.
For the six months that followed these educational sessions, CHWs made follow-up telephone calls to encourage screening participation, and to offer navigational assistance to participants. Navigational assistance included making a screening appointment, providing transportation and translation services, and/or completing paperwork. CHWs in the control group did not provide the participants with education or follow-up support until the final data collection point at which time they were allowed to offer the intervention. CHWs met monthly with a CHW coordinator (separately for the intervention and control groups), and could, if they chose, contact the CHW coordinator for informational support.
Measurements
Valuation of resources used
Costs for the development of the CHW intervention were tracked retrospectively using budget reports and itemized receipts. Expenses incurred to develop the intervention included material development costs as well as staff wages and fringe benefits. These materials included an individualized computer health message program that provided specific recommendations to address participants’ unique cancer risk factors, a two-hour health literacy education DVD and a picture guidebook. Research team members gathered relevant information and developed the educational content. Using this, the team worked with a software programmer to build the computerized health message program and they worked with actors, a photographer/videographer, plus a graphic designer to produce the DVD and picture guidebook. There was attention given to making materials that addressed the beliefs, attitudes, and experiences that were specific to the study population. The development and production costs of the DVD and picture guidebook were taken into account, as well as compensation for all of the workers listed above.
Budget reports and itemized receipts were gathered retrospectively to cost out church and CHW recruitment as well as CHW training. Estimates of staff wages per intervention group were approximated based on study team records. Costs associated with implementation of the intervention included stipends to the CHWs, as well as coverage of the CHW coordinator’s wages. The control groups’ implementation costs covered a stipend for CHWs to recruit participants and to meet monthly with the CHW coordinator and they also included the wages paid to the CHW coordinator. Costs were related only to the expenses associated with motivating women to receive a cancer screening; the medical costs of obtaining a mammogram or Pap test were not included.
Measurements
Screening adherence
Participants’ adherence to screening was assessed at three and six months using standardized instruments. Mammogram and Pap test results were verified by using a medical chart review at six months. The measure of effectiveness was defined as the combined total number of screenings completed within six months of receiving the CHW intervention. Screening adherence numbers were compared between the intervention and control groups.
Analysis
To assess the cost-effectiveness of the intervention, the costs and screening outcomes associated with each arm of the trial were compared with generate an incremental cost-effectiveness ratio (ICER). An ICER was calculated as follows: the difference in costs between the intervention and control groups was divided by the difference in the number of screenings completed between the two groups. The ICER represents the additional cost per screening required for a woman in the intervention group to receive a screening test in comparison with those in the no intervention group. The costs and screening outcomes were evaluated over two different time horizons to present one ICER that includes research and development costs and another separate ICER that does not include these costs. Including research and development costs could be meaningful to organizations that may seek to develop a similar program but for a different population. In that case, such an organization would not need to calculate the research and development costs a second time, as this study provides that information.
The two different ICER calculations necessitate using two different time horizons. For the first that included research and development costs, a two-year time horizon was used to reflect that one year was spent on research and development with a second year spent on implementation involving CHW recruitment, training, and delivery of the intervention. A 3% discount rate was applied to the first ICER, because costs were incurred beyond one year. For the second ICER that did not include research and development costs, a one-year time horizon was used and it reflects the time it only took to recruit and train CHWs, and deliver the intervention. Costs were collected in U.S. currency and inflated to US$2013.
Results
Table 1 presents a breakdown of the cost per person and cost per screening associated with administering the health literacy intervention delivered by CHWs. In the intervention group the average cost per person was $444, when research and development costs were considered sunk costs. In comparison, the average cost per participant in the control group was $269. The difference in the costs per participant between the two groups was primarily due to the stipends awarded to the CHWs in each group. The average cost per screening was $504 in the intervention group and $1,766 in the control group when research and development costs were set aside as sunk costs. When the research and development costs were included, however, the intervention group’s average cost per screening approximately doubled to be an estimated $1,002. Thus, whether the development costs were included or excluded, the intervention group’s average cost per screening was less than the control group’s average cost per screening ($1,766).
Table 1.
Activity Costs of Intervention for the CHW Health Literacy Group and the Control Group (US$ 2013)
| Program activity |
Intervention group |
Control group |
|---|---|---|
| Research and development | ||
| Staff salary and benefits | 102,112 | - |
| Intervention material development | 19,705 | - |
| Total | 121,817 | - |
| Recruitment and training | ||
| Staff salary and benefits | 48,765 | 48,765 |
| Training of CHWs | ||
| Printing | 92 | 131 |
| Supplies | 550 | 786 |
| DVD players | 1,556 | 0 |
| Staff wages | 1,741 | 1,161 |
| Refreshments | 425 | 185 |
| Total | 53,130 | 51,028 |
| Implementation of intervention | ||
| CHW stipend | 61,459 | 21,920 |
| CHW site supervisor | 8,977 | 2,993 |
| Total | 70,437 | 24,913 |
| Study total | 245,383 | 75,941 |
| Average cost per participant (including research and development cost) | 883 | 269 |
| Average cost per participant (excluding research and development cost) | 444 | 269 |
| Average cost per screening (including research and development cost) | 1,002 | 1,766 |
| Average cost per screening (excluding research and development cost) | 504 | 1,766 |
Estimates for the ICER are presented in Tables 2 and 3. Both tables illustrate the intervention group completed an additional 202 screenings in comparison with the control group. Table 2 presents the ICER results when research and development costs were included in the analysis, and indicates that it cost $839 per additional screening for the intervention group versus the control group. In comparison, the ICER results shown in Table 3, when research and development costs were not included, estimate the cost per incremental screening for the intervention group versus the control group was $236.
Table 2.
Incremental cost-effectiveness ratio (ICER) that includes development costs comparing CHW health literacy intervention group to control group
| Group | Costs (US$) |
Incremental cost |
Screenings completed |
Additional screening |
ICER US$) |
|---|---|---|---|---|---|
| Control group | 75,941 | 43 | |||
| Intervention group | 245,383 | 169,441 | 245 | 202 | 839 |
Table 3.
Incremental cost-effectiveness ratio (ICER) that excludes development costs comparing CHW health literacy intervention group to control group
| Group | Costs (US$) |
Incremental cost |
Screenings completed |
Additional screening |
ICER (US$) |
|---|---|---|---|---|---|
| Control group | 75,941 | 43 | |||
| Intervention group | 123,566 | 47,625 | 245 | 202 | 236 |
Discussion
We can extrapolate from this CHW intervention that another one like it, which provides the same materials and structure but on a larger scale, will require an estimated additional cost per screening of $236. There are few studies that establish a threshold by which to compare these ICER results. One cost-effectiveness analysis conducted in 2002 reports an ICER of $726 for each additional Pap smear obtained when comparing an outreach worker intervention to a control group.14 Another cost-effectiveness study reports an ICER of $2,451 per additional mammography user for an intervention in rural areas using three different approaches (individual counseling, community activities, and a combined intervention including both).15
It is important to note that direct comparisons of our findings to these studies are not possible. For instance, the analysis conducted by Andersen and colleagues14 assumed a societal perspective, whereas we did not. Moreover both studies calculated an ICER for a specific type of cancer screening, which contrasts with the combined screening measure of effectiveness used in the current analysis. Taking those differences into consideration, these ICERs nonetheless provide a benchmark by which to compare the results. They indicate that at a cost of $236 per additional screening, excluding research and development costs, the estimates of this intervention are favorable. Even when research and development costs are included, the ICER of $839 per additional screening also appears to be reasonable when matched against other ICER values in the field.14,15
In a systematic review of interventions to increase breast and cervical cancer screenings among Asian American women, Lu and colleagues6 identify a need for more studies that assess the cost-effectiveness and affordability of effective intervention programs. This study responds by analyzing one of the aforementioned. It is an initial step to what could be a larger analysis. An important follow-up study would be able to calculate the specific costs per additional breast or cervical cancer screening. In addition, researchers could assess if late stage cancer treatment costs within a community could be mitigated by an intervention’s promotion of regular screenings, and if so, to what degree.
Though this analysis provides valuable insight into the costs associated with developing and providing a CHW health literacy intervention to the Korean American population, it does have some limitations. First, the findings may be limited in their generalizability when applied to other parts of the U.S. since the original study only included costs for states on the East Coast. Another limitation is that costs and time valuation were not collected continuously throughout the development and implementation of the study and this makes it difficult to provide precise estimates for staff time and CHW time. Similarly, costs were aggregated and cannot be separated by cancer screening type. For this reason we had to use combined screenings as the outcome, whereas it would have been more informative to specify an ICER for each additional mammogram or Pap test. Finally, this analysis adopted a health care perspective instead of a societal perspective; originally, the study did not intend to conduct a cost analysis and therefore the cost measures needed for a societal perspective were not collected.
Policymakers need to be aware of the growing Asian American population in the U.S. and the need to address their high cancer incidence and mortality rates. This study demonstrated the economic promise of providing a culturally specific, tailored health literacy program to improve breast and cervical cancer screening participation among Korean American women. As programmatic costs are important when making decisions about the allocation of funding, this study provides strategic information for health care stakeholders who will decide how to allocate resources to primary, secondary, or tertiary prevention. Future research should continue to evaluate health intervention costs for this population and other vulnerable populations.
Acknowledgments
This study was supported by a grant from the National Cancer Institute (R01 CA129060, Clinical Trials Registry NCT00857636). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors are grateful to all Korean American women and community health workers who participated in this study, and to the research staff, Jung-Ah Ahn, Hyekyung Chin, and Myunghee Kim. The authors also thank Ms. Kyunghae Kim for her assistance with cost-related data collection.
Contributor Information
Anne L.R. Schuster, Department of Health Systems, Management and Policy, Colorado School of Public Health.
Kevin D. Frick, Johns Hopkins University (JHU) Carey Business School.
Bo-Yun Huh, Department of Community-Public Health, JHU School of Nursing (SON) at the time of the study.
Kim B. Kim, Korean Resource Center in Ellicott City, Maryland.
Miyong Kim, University of Texas at Austin, School of Nursing.
Hae-Ra Han, Department of Community-Public Health, JHU School of Nursing.
References
- 1.U.S. Department of Commerce. Hoeffel E, Rastogi S, Kim MO, et al., editors. The Asian population: 2010. U.S. Census Bureau, 2010 Census Briefs (C2010BR-11) Available at www.census.gov/prod/cen2010/briefs/c2010br-11.pdf.
- 2.Breast Cancer Facts & Figures 2011–2012. Atlanta, GA: American Cancer Society; 2011. Available at: http://www.cancer.org/research/cancerfactsfigures/breastcancerfactsfigures/breast-cancer-facts-and-figures-2011-2012. [Google Scholar]
- 3.Cancer Prevention & Early Detection Facts & Figures 2013. Atlanta, GA: American Cancer Society; 2013. Available at: http://www.cancer.org/research/cancerfactsfigures/cancerpreventionearlydetectionfactsfigures/cancer-prevention-early-detection-facts-figures-2013. [Google Scholar]
- 4.Lee HY, Eunsu J, Der Vang P, et al. Breast and cervical cancer screening among Asian American women and Latinas: does race/ethnicity matter? J Womens Health. 2010 Oct;19(10):1877–1884. doi: 10.1089/jwh.2009.1783. [DOI] [PubMed] [Google Scholar]
- 5.McCracken M, Olsen M, Chen MS, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese Ethnicities. CA Cancer J Clin. 2007 Jul-Aug;57(4):190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- 6.Lu M, Moritz S, Lorenzetti D, et al. A systematic review of interventions to increase breast and cervical cancer screening uptake among Asian women. BMC Public Health. 2012 Jun 7;12:413–428. doi: 10.1186/1471-2458-12-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jemal A, Simar EP, Dorell C, et al. Annual Report to the Nation on the status of cancer 1975–2009, featuring the burden and trends in Human Papillomavirus (HPV) associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013 Feb 6;105(3):175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Han HR, Kim J, Lee JE, et al. Interventions that increase use of Pap tests among ethnic minority women: a meta-analysis. Psycho-Oncology. 2011 Apr;20(4):341–351. doi: 10.1002/pon.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute of Medicine. Health literacy: a prescription to end confusion. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 10.Lindau ST, Tomori C, Lyons T, et al. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am J Obstet Gynecol. 2002 May;186(5):938–943. doi: 10.1067/mob.2002.122091. [DOI] [PubMed] [Google Scholar]
- 11.Han HR, Kim J, Kim MT, et al. Measuring health literacy among immigrants with a phonetic primary language: a case of Korean American women. J Immigr Minor Health. 2011 Apr;13(2):253–259. doi: 10.1007/s10903-010-9366-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han HR, Lee JE, Kim J, et al. A meta-analysis of interventions to promote mammography among ethnic minority women. Nurs Res. 2009 Jul-Aug;58(4):246–254. doi: 10.1097/NNR.0b013e3181ac0f7f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Green LW, Kreuter MW. Health promotion planning: an educational and environmental approach. Mountain View, CA: Mayfield Publishing Co; 1991. [Google Scholar]
- 14.Thompson B, Thompson LA, Chan NL, et al. Cost effectiveness of cervical cancer screening among Chinese women in North America. Asian Pac J Cancer Prev. 2007 Apr-Jun;8(2):287–293. [PubMed] [Google Scholar]
- 15.Andersen MR, Hager M, Su C, et al. Analysis of the Cost-effectiveness of mammography promotion by volunteers in rural communities. Health Educ Behav. 2002 Dec;29(6):755–770. doi: 10.1177/109019802237942. [DOI] [PubMed] [Google Scholar]