Abstract
Background:
The oral disease burden in Nigerian rural areas is considered high with limited dental services. Normative need assessment to facilitate oral health promotion and interventional activities is essential. Therefore, the aim of this study was to evaluate the dental service utilization and trends of patents attending a rural outreach dental clinic.
Materials and Methods:
A retrospective study was conducted using data from clinical records of patients seen over a period of 54 months at a rural outreach dental clinic of comprehensive health center, Udo, Edo State, and were analyzed for descriptive variables with Chi-square test and P value set at ≤0.05 significance.
Results:
One hundred and sixty four (164) patients [males = 74 (45.1%), females = 90 (54.9%)] were seen with a mean age of 36.15 ± 18.05 years. The major reason for clinic visit was due to dental caries (sequelae) and condition representing 43.3% and 34.8%, respectively. Extractions (41.5%) and scaling and polishing (S and P) (21.3%) accounted for the most frequently provided treatment. Almost 20% patients did not receive any form of treatment.
Conclusion:
The study revealed a low health seeking behavior, low utilization of dental services among the rural dwellers and need for oral health awareness, periodic screening, and preventive approach in the rural population through more frequent outreach visits of dental personnel resident in the community.
Keywords: Dental services, rural dental outreach, treatment needs
INTRODUCTION
Oral diseases continue to be prevalent in many of the developing countries including Nigeria where people from deprived communities and of ethnic minorities are not sufficiently covered by oral health care.[1,2] Outreach dental services through mobile or fixed rural clinics are necessary to tackle the burden of poor oral health of people with limited resources and lack of tradition regular oral health care.[3] Oral health is part of general health and associations between oral health and general health has been established in several studies. Oral diseases have been shown to adversely affect diet, nutrition, quality of life, and socioeconomic status.[4,5] Individuals’ utilization of dental services may be influenced by access to care, financial restrictions, attitudes toward dental care, and dental fear.[6]
There are few studies that have focused on outreach oral health services in rural areas in southwestern Nigeria.[7,8,9] More information on effective national outreach models is required for advocacy, resource acquisition, interventional program design, and modification. The oral disease burden in Nigerian rural areas is considered to be high with limited dental services. Normative need assessment to facilitate objective oral health promotion and interventional activities is essential.[10,11] The purpose of this study was to evaluate normative treatment needs, service utilization, and trends in Udo community, a rural area, where a community dental clinic was established for outreach programs.
MATERIALS AND METHODS
A retrospective study was conducted using data from clinical records of patients seen by visiting dental team over a period of 54 months at a rural outreach dental clinic of comprehensive health center, Udo, Ovia South West Local Government Area, and Edo State. Udo is a rural community located about 40 km from Benin City, the state capital and 8 km from Iguobazuwa, the Ovia South West Local Government Council headquarters. The local government area has a population of 138,072 persons.[12] Udo inhabitants are predominantly peasant farmers. Inclusion criteria were dental records of all patients visiting or referred to the clinic for the first time. Records of subsequent visits of same patients were excluded. The data on initial diagnosis or diagnoses, the treatment(s) given, and annual attendance were collated for analysis.
The Comprehensive Health Centre is one of satellite health centers of the University of Benin Teaching Hospital to provide full package primary health-care services, preventive care, and some surgical services in rural communities but had no dental component until the present initiative to provide dental residents and students with clinical training opportunity in rural areas.
Statistical analysis
Data obtained were subjected to descriptive analysis using Statistical Package for the Social Sciences (SPSS) version 16 (SPSS-Inc., Chicago, IL). Correlations between variables were analyzed using Pearson or Likelihood ratio Chi-square test where applicable with P value set at ≤0.05 significance.
RESULTS
A total number of 164 patients were seen, of which 74 (45.1%) were males and 90 (54.9%) were female. The age range was 3–78 years with the mean age of 36.15 ± 18.05 years. The annual attendance of the patients in 2011, 2012, 2013, 2014, and 2015 were 20.7%, 26.2%, 14.0%, 17.7%, and 21.3%, respectively. The major reason for clinic visit was due to dental caries (or its sequelae) and condition representing 43.3% and 34.8%, respectively. Extractions (41.5%) and scaling and polishing (S and P) (21.3%) accounted for the most frequently provided treatment. Almost 20% patients did not receive any form of treatment.
Of the number of patients seen at the outreach clinic, 74.5% received treatment while the others were referred to the dental centre at the Teaching Hospital in Benin City.
DISCUSSION
Only one hundred and sixty-four patients were seen over a 5-year period of study in spite efforts at raising oral health awareness through local street campaign and advocacy visits. This trend was consistent by age groups during the study period [Figure 1]. The inhabitants seemed to place more priority on farming than oral health thus displaying poor health-seeking behavior.[13] Logistical, transport, and accommodation challenges hampered holding dental camps or permanent residence of dental personnel at the outreach center. This limitation may have discouraged patients’ attendance and affected the process of enabling them to increase control over their health and to reduce disease burden.[14]
Figure 1.
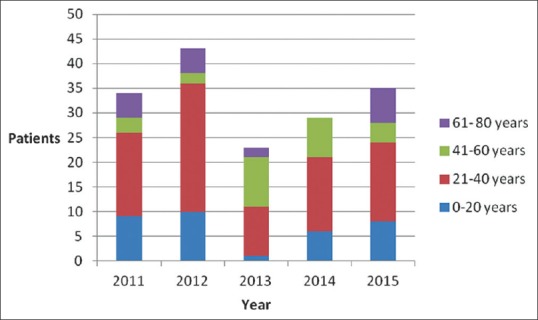
Trends in patients’ attendance at the outreach dental clinic by age group
In this study, majority of the patients (49.1%) who utilized dental services at the comprehensive health center were adults with a greater proportion in the 20–40 years age-group [Table 1]. This is in agreement with studies by Taiwo et al.[15,16,17] where an overwhelming proportion of dental services utilization was by the people belonging to younger age bracket, with a suggestion that younger people have fewer barriers to oral health. It has been opined that more concern for other chronic disease rather than oral health may be responsible for the low utilization of dental services among the elderly.[18,19] In addition, population size demographics have also been proposed to be another cause of poor dental care utilization by the elderly.
Table 1.
Distribution of patients attending clinic by gender and age group
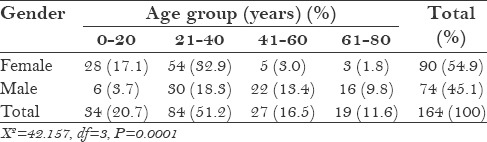
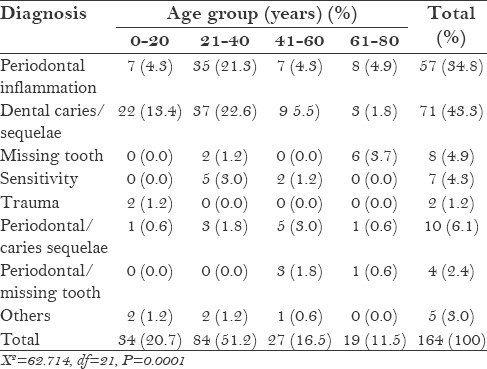
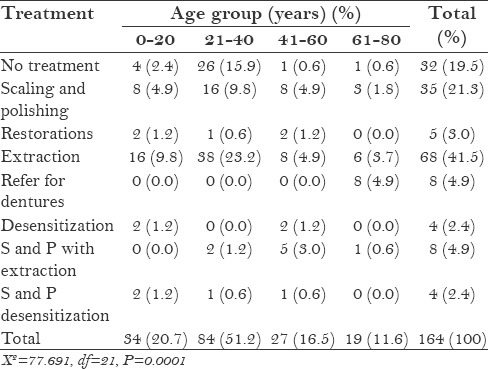
There were more females (58.5%) seeking oral health care than male at the center. This finding was similar to some studies by Denloye et al.,[20] Varenne[21] but contradicts the findings of Taiwo[15] Olaleye,[18] Oginni.[19] This may be attributed to better health-seeking behavior of females or because of frequent contacts with health facility for antenatal care and family planning services. Dental caries and its sequelae (43.3%) (acute apical periodontitis, dentoalveolar abscess) and periodontal inflammation (34.8%) were the major reasons for clinic visit in this study [Table 2]. The reason perhaps may likely be due to the high impact of the burden of caries and periodontal disease on the individual in form of recurrent acute pain, severe discomfort on mastication, and irritating interference with daily living and quality of life.[6,10] Nearly two-thirds of the patients in the 0–20 year's age group [Table 3] presented with caries or its sequelae which may have resulted from the gradual change to Western diet with this group even in rural communities of Nigeria.[22,23,24] Also, the elderly group had a relatively high demand for treatment of edentulous space suggesting a growing awareness on the importance tooth replacement.
Table 2.
Summary of diagnosis according to gender of patients
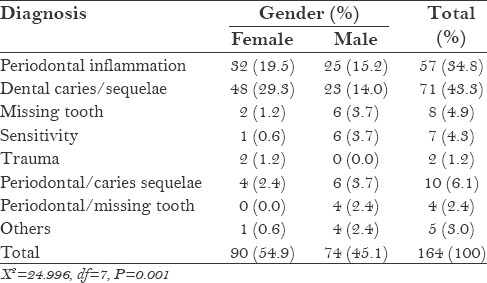
Table 3.
Diagnosis of dental conditions according to age group of patients
There was a significant difference between gender and treatment provided in the results of this study [Table 4]. Tooth extraction accounted for the majority of treatment offered and this in agreement with other studies in Nigeria.[25,26,27] Reasons may be due to the fact that tooth extraction is a relatively cheaper treatment and simpler option, and most of the patients presented at the late symptomatic stage of caries sequelae or periodontal disease opt for it.[28] In addition, a greater number of the extractions were done for young and middle-aged adults [Table 5], which may suggest a need for preventive intervention in younger age groups. A low proportion of the study group had restorations and S and P done with females having more restorations than male. This concurs with the few reports on the subject and may point to the need for oral health education to increase awareness of preventive approach in oral health management in the population.[11,25]
Table 4.
Pattern of treatment rendered according to gender
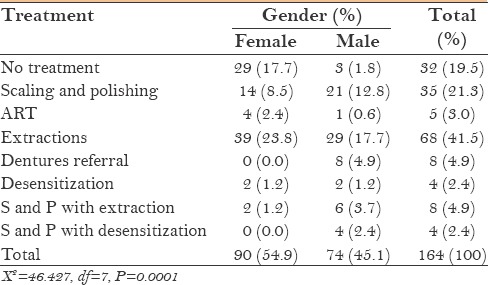
Table 5.
Pattern of treatment according to age group of patients
CONCLUSION
The study showed poor health-seeking behavior among the community dwellers. Dental care service was majorly utilized for periodontal disease in the rural dental clinic, whereas extractions as a principal form of treatment offered for dental caries and its sequelae with. There is a need for oral health promotion and periodic screening in the population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Petersen PE. World Health Organization global policy for improvement of oral health-World Health Assembly 2007. Int Dent J. 2008;58:115–21. doi: 10.1111/j.1875-595x.2008.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 2.WHO; 1997. [Last accessed on 2015 Nov 12]. World Health Organization. The Jakarta Declaration: On leading health promotion into the 21st century. Available from: http://apps.who.int/iris/bitstream/10665/63698/1/WHO_HPR_HEP_4ICHP_BR_97.4_eng.pdf . [Google Scholar]
- 3.Achembong LN, Ashu AM, Hagopian A, Downer A, Barnhart S. Cameroon mid-level providers offer a promising public health dentistry model. Hum Resour Health. 2012;26(10):46. doi: 10.1186/1478-4491-10-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Llewellyn CD, Warnakulasuriya S. The impact of stomatological disease on oral health-related quality of life. Eur J Oral Sci. 2003;111:297–304. doi: 10.1034/j.1600-0722.2003.00057.x. [DOI] [PubMed] [Google Scholar]
- 5.Ingram SS, Seo PH, Sloane R, Francis T, Clipp EC, Doyle ME, et al. The association between oral health and general health and quality of life in older male cancer patients. J Am Geriatr Soc. 2005;53:1504–9. doi: 10.1111/j.1532-5415.2005.53452.x. [DOI] [PubMed] [Google Scholar]
- 6.Heaton LJ, Smith TA, Raybould TP. Factors influencing use of dental services in rural and urban communities: Considerations for practitioners in underserved areas. J Dent Educ. 2004;68:1081–9. [PubMed] [Google Scholar]
- 7.Olabisi AA, Udo UA, Ehimen UG, Bashiru BO, Gbenga OO, Adeniyi AO. Prevalence of dental caries and oral hygiene status of a screened population in Port Harcourt, Rivers State, Nigeria. J Int Soc Prev Community Dent. 2015;5:59–63. doi: 10.4103/2231-0762.151979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawal FB, Taiwo JO, Oke GA. Oral health practices of adult inhabitants of a traditional community in Ibadan, Nigeria. Niger J Med. 2013;22:212–7. [PubMed] [Google Scholar]
- 9.Ibiyemi O, Taiwo JO, Oke GA. Dental education in the rural community: A Nigerian experience. Rural Remote Health. 2013;13:2241. [PubMed] [Google Scholar]
- 10.Adekoya-Sofowora CA. Global theme issue: Poverty and human development the effect of poverty on access to oral health care in Nigeria. Nigerian Dental Journal (NDJ) 2008;16:40–42. [Google Scholar]
- 11.Olusile A. Improving low awareness and inadequate access to oral health care in Nigeria: The Role of Dentists, the Government and Non-Governmental Agencies. Niger Med J. 2010;51:134–6. [Google Scholar]
- 12.National Population Commission. 2006. Population and housing census of the Federal Republic of Nigeria. 2006:60. [Google Scholar]
- 13.Omotoso O. Health seeking behaviour among the rural dwellers in Ekiti State, Nigeria. African Research Review (Afr Rev) 2010;4:125–38. [Google Scholar]
- 14.Adeniyi AA, Sofola OO, Kalliecharan RV. An appraisal of the oral health care system in Nigeria. Int Dent J. 2012;62:292–300. doi: 10.1111/j.1875-595X.2012.00122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taiwo OA, Soyele OO, Ndubuizu GU. Pattern of utilization of dental services at Federal Medical Centre, Katsina, Northwest Nigeria. Sahel Med J. 2014;17:108–11. [Google Scholar]
- 16.Ajayi DM, Arigbede AO. Barriers to oral health care utilization in Ibadan, South West Nigeria. Afr Health Sci. 2012;12:507–13. doi: 10.4314/ahs.v12i4.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olanrewaju I, Arowojolu OM, Gbadebo SO, Ibiyemi TS. An audit of pattern of patients’ presentation at the Periodontics Clinic of the University College Hospital, Ibadan. Ann Ib Postgrad Med. 2009;7:16–20. doi: 10.4314/aipm.v7i1.64057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olaleye AO, Suleiman IK, Solomon S. Pattern of dental treatment in patients attending the Dental Centre University of Maiduguri Teaching Hospital, Maiduguri, Nigeria. BOMJ. 2013;10:12–9. [Google Scholar]
- 19.Oginni AO. Dental care needs and demands in patients attending the dental hospital of the Obafemi Awolowo University Teaching Hospital's Complex Ile-Ife, Nigeria. Niger J Med. 2004;13:339–44. [PubMed] [Google Scholar]
- 20.Denloye OO, Bankole OO, Onyeaso CO. Dental health service utilization by children seen at the University College Hospital-an update. Odontostomatol Trop. 2004;27:29–32. [PubMed] [Google Scholar]
- 21.Varenne B, Msellati P, Zoungrana C, Fournet F, Salem G. Reasons for attending dental-care services in Ouagadougou, Burkina Faso. Bull World Health Organ. 2005;83:650–5. [PMC free article] [PubMed] [Google Scholar]
- 22.Okeigbemen SA, Nnawuihe UC, Osemwegie C. Dental caries experience and oral health behavior among 7-15 years old children attending military and paramilitary schools in Benin City. Savannah Journal of Medical Research and Practice (SJMRP) 2015;4:15–20. [Google Scholar]
- 23.Folaranmi N, Akaji E, Onyejaka N. Pattern of presentation of oral health conditions by children at University of Nigeria Teaching Hospital, Enugu: A retrospective study. Niger J Clin Pract. 2013;17:47–50. doi: 10.4103/1119-3077.122836. [DOI] [PubMed] [Google Scholar]
- 24.Edelstein BL. The dental caries pandemic and disparities problem. BMC Oral Health. 2006;6(Suppl 1):S2. doi: 10.1186/1472-6831-6-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Akpata E. Oral health in Nigeria. Int Dent J. 2004;54(Suppl 1):361–6. doi: 10.1111/j.1875-595x.2004.tb00012.x. [DOI] [PubMed] [Google Scholar]
- 26.Anyanechi C, Chukwuneke F. Survey of the reasons for dental extraction in Eastern Nigeria. Ann Med Health Sci Res. 2012;2:129–33. doi: 10.4103/2141-9248.105659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adeyemo WL, Oderinu HO, Oluseye SB, Taiwo OA, Akinwande JA. Indications for extraction of permanent teeth in a Nigerian teaching hospital: A 16-year follow-up study. Nig Q J Hosp Med. 2008;18:128–32. doi: 10.4314/nqjhm.v18i3.45013. [DOI] [PubMed] [Google Scholar]
- 28.Gbenga Omitola O, Olabisi Arigbede A. Prevalence and pattern of pain presentation among patients attending a tertiary dental center in a southern region of Nigeria. J Dent Res Dent Clin Dent Prospects. 2010;4:42–6. doi: 10.5681/joddd.2010.012. [DOI] [PMC free article] [PubMed] [Google Scholar]


