Abstract
Aim:
The aim of this study is to compare the oral hygiene status among institutionalized visually impaired children of age between 6 and 20 years given with Braille and audio instructions in Raichur city of Karnataka.
Materials and Methods:
A total of 50 children aged between 6 to 20 years were included in this study from a residential school for visually impaired children. These children were randomly divided into two equal groups. One group was given oral hygiene instructions by audio recordings and another written in Braille and were instructed to practice the same. After three months time the oral hygiene status and dental caries experience was recorded and compared using patient performance index. Statistical analysis was done by student paired t test and multiple comparison by Tukey's HSD (honest significant difference) test.
Results:
The mean PHP (Patient Hygiene Performance) score of group A at baseline was 3.88 compared to 3.90 of group B. At 7 days PHP score of group A and group B was 3.42 and 3.45 respectively. At 3 month PHP score of group A and group B was 2.47 and 2.86 respectively. Even though over a period of time the mean score of PHP index reduced the score comparison between the 2 groups were statistically non significant. In group A the mean difference of PHP score between baseline and 7 days was 0.46, between baseline and 3 months it was 1.40. The PHP score between 7 days and 3 months was 0.94. All the above values were statistically significant.
Conclusion:
Effective dental health education method has to be instituted for visually impaired children. The present study shows improvement of oral health status in both the study population by decrease in the mean plaque score. Hence continuous motivation and reinforcement in the form of Braille and audio instruction is beneficial to achieve good oral hygiene levels in visually impaired children.
Keywords: Braille, dental caries, oral hygiene, visually impaired
INTRODUCTION
It is estimated that there are 1.4 million blind children in the world, two-thirds of whom live in the developing countries.[1] The prevalence of childhood blindness was 0.17% in India.[2] Maintaining oral hygiene is one of the difficult tasks along with other tasks for visually impaired children. When compared with children with normal sight, the children with visual impairment will have poorer oral hygiene and high caries index. Studies performed by Anaise in Israel,[3] Shaw et al. in UK,[4] and Purohit et al. in South India[5] found poor oral health attributes among special care children. Unfortunately, conventional methods of teaching maintenance of oral hygiene like using visual aids, disclosing agents does not help the visually impaired children who depend of touch and feel to learn.[6]
Maintenance of oral health, removal of plaque, and proper brushing of teeth are the difficult tasks for these children. Plaque is one of the risk factors for caries development.[7] The difficulty in making the child understand to maintain oral hygiene and children following the instructions properly are the major hurdles. Chemical plaque control, individual care and training for visually impaired children will help in maintaining oral health.[8]
Even though these children are visually impaired, their true ability of understanding things is often unnoticed. Oral hygiene instructions given to their understanding by any other means will improve their practice.
Braille is a tactile writing system used by the blind and the visually impaired people. It is traditionally written with embossed paper.[9] There are a very few studies in which visually impaired children are given Braille instructions for oral hygiene maintenance and their performances are evaluated.
In this study, we compared the oral hygiene of visually impaired children who were given oral hygiene instructions in Braille and audio recordings using the Patient Hygiene Performance (PHP) index of Podshadley and Haley (1968).[10]
MATERIALS AND METHODS
Prior to the study, ethical clearance was obtained from the Institutional Ethical Committee of Navodaya Dental College and Hospital, Raichur, Karnataka. The study design was explained to the district educational officer of Raichur district and permission to conduct the study was obtained. Permission was taken from a private residential institution for visually challenged children in Raichur city after explaining the benefits of the study. Informed consent was taken from the parents. A total of 50 children from the age group of 6–20 years were included in the study.
The children with a recent history of dental treatment, systemic antibiotics or topical fluoride treatments 3 months prior to baseline, habitual use of dairy probiotics, Xylitol chewing gums, severe medical conditions were excluded from the study.
Fifty visually impaired children with no systemic diseases and those who are not using probiotic products and any other oral hygiene supplements, such as mouthwashes, were included in this study. Their oral hygiene was checked using the PHP index.[10] The scores were recorded at baseline data. The children were randomly divided using chit selection into two equal groups (N = 25)—groups A and B. Children in group A were given written instructions in Braille and those in group B were given audio recordings. These children were instructed to use circular motion of brushing twice daily, to gargle with water after every meal, and to do regular flossing. They were also given soft manual toothbrushes and toothpaste (Colgate® with 1000 ppm fluoride). The instructions on to how to brush and floss are given both in Braille and audio instructions to the children as mentioned earlier. The children were given balanced diet meal throughout the study period and snacks in between meals are restricted. The resident school in-charge was keeping the track to make sure that all the children follow the instructions properly.
After 7 days, the PHP Index[10] was taken to check the efficacy of children maintaining their oral hygiene and data were recorded. The children were instructed to continue the practice for 3 more months and then again the PHP index was checked.
The data thus obtained were subjected to statistical analysis by using Student's paired t-test and Turkey's honest significant difference (HSD) test was applied for multiple comparisons. The results were tabulated and statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 17.0 (SPSS Inc. 233 South Wacker Drive, 11th Floor, Chicago, II, 60606-6412).
RESULTS
Table 1 depicts the comparison of the PHP index between the two groups at baseline, 7 days, and 3 months. The mean PHP score of group A at baseline was 3.88 compared to 3.90 of group B. At 7 days, the PHP scores of group A and group B were 3.42 and 3.45, respectively. At 3 months, the PHP scores of group A and group B were 2.47 and 2.86, respectively. Even though over a period of time the mean score of PHP index reduced the score comparison between the two groups were not statistically significant.
Table 1.
Average oral hygiene at baseline, 7 days, and after 3 months
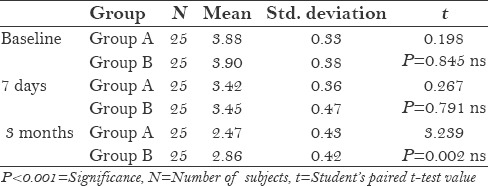
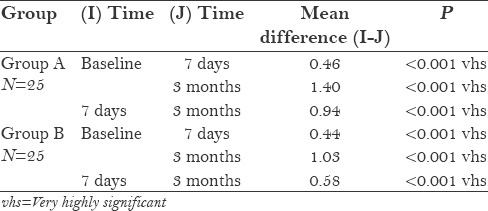
Table 2 depicts the comparison of PHP index within the group at baseline, 7 days, and 3 months. In group A, the mean difference of PHP score between the baseline and 7 days was 0.46, between the baseline and 3 months it was 1.40. The PHP score between 7 days and 3 months was 0.94. All the above values were statistically significant. In group B, the mean difference of PHP score between baseline and 7 days was 0.44, between baseline and 3 months it was 1.03. The PHP score between 7 days and 3 months was 0.58. All the above values were statistically significant.
Table 2.
Multiple comparisons of the groups
DISCUSSION
“The best and the most beautiful things in the world cannot be seen or even touched. They must be felt with the heart” - Helen Keller.[11] Oral health is a vital component of overall health, which contributes to each individual's well-being and quality of life by positively affecting physical and mental healthiness, appearance, and interpersonal relations.[12] The oral health of children who are visually impaired tends to be compromised as they are at a disadvantage and are often unable to adequately apply the techniques necessary to control plaque.[13]
The visually impaired patients present a special challenge to the dentist. Providing comprehensive dental care for the visually impaired children is like a community service and also rewarding to the health-care providers.[14] Visually impaired children are able to learn good techniques of brushing when oriented properly.[15]
Often dental plaque is the main reason for the development of periodontal diseases and dental caries.[7] Early signs of oral diseases may be unnoticed and not possible for people with low vision, and because of this they may not be able to take the necessary action to prevent or treat a particular oral condition.[16] Gingivitis is more common in visually challenged children.[17] In our study, we compared the oral hygiene status using PHP index of Podshadley and Haley among institutionalized visually impaired children aged between 6 years and 20 years given with Braille and audio instructions. The children in our study were designated disabled according to the criteria given by “Persons with Disabilities (Equal Opportunities, Protection of Rights and Full Participation) Act, 1995,”[18] which defines “blindness” as a condition where a person suffers from total absence of sight or visual acuity not exceeding 6/60 or 20/200 in the better eye even with correction lenses or limitation of the field of vision subtending an angle of 20° or worse.
Even though both the groups showed decrease in plaque score, inter-group comparison of PHP index score was not statistically significant. In a study conducted by Mendonça,[19] it was stated that the absence of visual stimuli prevents rapid learning, representing a challenge for surgeons and dentists in motivating these individuals to have appropriate oral hygiene. However, it is arguable that, when well-trained, blind children are able to learn the brushing techniques, thus maintaining good oral condition.
The present study showed a decrease in the mean plaque scores (that is increase in mean difference of PHP score) at all time intervals in individual group as compared to the baseline that was statistically significant. This shows that a proper method of educating the visually impaired children will decrease the plaque score that in turn will improve the oral hygiene [Figure 1].
Figure 1.
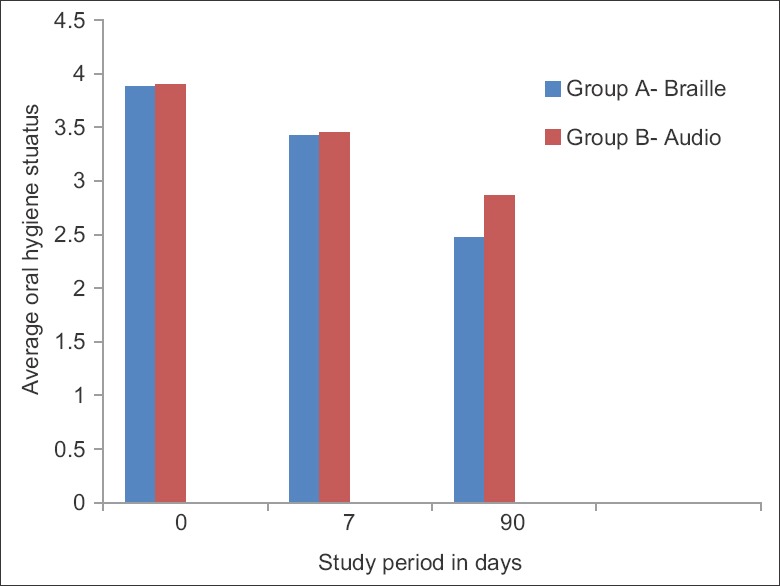
Average oral hygiene in two groups during study period
Studies by Aguiar et al.[20] confirm that there was marked reduction in rates of biofilm and good oral hygiene can be achieved by the usage of appropriate brushing techniques. Proper education and motivation were the key behind this success in these visually impaired children.
Vargas and Goulart[21] in their study showed that, even though they cannot see it, visually impaired patients do express concerns about the functional aspects of oral cavity. These individuals understand the functional importance of the teeth and mouth, citing the pain as the main factor in seeking care. The aesthetic aspect of oral hygiene is rarely mentioned and seems to have less relevance to these individuals.
Visually impaired people have equal right to have a good oral health and social care information needs which are worthy of exploration.[22]
CONCLUSION
Visual impairment may have an impact on the access to dental care and oral health information. An effective dental health education method has to be instituted for visually impaired children. The present study shows improvement of oral health status in both the study population by the decreasing the mean plaque score.
Hence, continuous motivation and reinforcement in the form of Braille and audio instruction are essential to achieve good oral hygiene levels in visually impaired children. Further, long-term study on larger population has to be conducted to obtain a result that will differentiate statistically between the motivational tools for visually impaired children.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Geneva: WHO; 2000. World Health Organization. Preventing blindness in children: Report of WHO/IAPB scientific meeting. Programme for the Prevention of Blindness and Deafness, and International Agency for Prevention of Blindness. [Google Scholar]
- 2.Dandona R, Dandona L. Childhood blindness in India: A population based perspective. Br J Ophthalmol. 2003;87:263–5. doi: 10.1136/bjo.87.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anaise JZ. Periodontal disease and oral hygiene in a group of blind and sighted Israeli teenagers 14-17 years of age. Community Dent Oral Epidemiol. 1979;7:353–6. doi: 10.1111/j.1600-0528.1979.tb01247.x. [DOI] [PubMed] [Google Scholar]
- 4.Shaw L, Maclaurin ET, Foster TD. Dental study of handicapped children attending special schools in Birmingham, UK. Community Dent Oral Epidemiol. 1986;14:24–7. doi: 10.1111/j.1600-0528.1986.tb01488.x. [DOI] [PubMed] [Google Scholar]
- 5.Purohit BM, Acharya S, Bhat M. Oral health status and treatment needs of children attending special schools in South India: A comparative study. Spec Care Dentist. 2010;30:235–41. doi: 10.1111/j.1754-4505.2010.00160.x. [DOI] [PubMed] [Google Scholar]
- 6.AlSarheed M, Bedi R, Alkhatib MN, Hunt NP. Dentist's attitude and practices towards provision of orthodontic treatment for children with visual and hearing impairments. Spec Care Dentist. 2006;26:30–6. doi: 10.1111/j.1754-4505.2006.tb01507.x. [DOI] [PubMed] [Google Scholar]
- 7.Yalcinkaya SE, Atalay T. Improvement of oral hygiene knowledge in a group of visually impaired students. Oral Health Prev Dent. 2006;4:243–53. [PubMed] [Google Scholar]
- 8.Ahmed MS, Jindal MK, Khan S, Hashmi SH. Oral health knowledge, practice, oral hygiene status and dental caries prevalence among visually impaired students in residential institute of Aligarh. J Dent Oral Hygiene. 2009;1:22–6. [Google Scholar]
- 9.Braille: [Last accessed on 2015 Oct 22]. Available from: http://en.wikipedia.org/wiki/Braille . [Google Scholar]
- 10.Podshadley AG, Haley JV. A method for evaluating oral hygiene performance. Public Health Rep. 1968;83:259–64. [PMC free article] [PubMed] [Google Scholar]
- 11.Keller H. The Story of My Life. American Foundation for the Blind. 2015. [Last accessed on 2015 Oct 25]. Available from: http://www.afb.org/mylife/book.asp?ch=P2Let45 .
- 12.Rao D, Amitha H, Munshi AK. Oral hygiene status of disabled children and adolescents attending special schools of South Canara, India. Hong Kong Dent J. 2005;2:107–12. [Google Scholar]
- 13.Shetty V, Hegde AM, Bhandary S, Rai K. Oral health status of the visually impaired children-A south Indian study. J Clin Pediatr Dent. 2010;34:281–5. doi: 10.17796/jcpd.34.3.j4781g2w8891848u. [DOI] [PubMed] [Google Scholar]
- 14.Wei SH. Dentistry for special patients. In: Wei SH, editor. Pediatric Dentistry: Total Patient Care. Philadelphia: Lea and Febiger; 1988. pp. 573–4. [Google Scholar]
- 15.Maciel SM, Cordeiro PM, d’Ávila S, Pina Godoy G, Alves RD, Uchôa Lins RD. Assessing the oral condition of visually impaired individuals attending the Paraíba Institute of the Blind. Rev Odonto Ciêc. 2009;24:354–60. [Google Scholar]
- 16.Mohd-Dom TN, Omar R, Malik NA, Saiman K, Rahmat N. Self-Reported oral hygiene practices and periodontal status of visually impaired adults. Glob J Health Sci. 2010;2:184–91. [Google Scholar]
- 17.Nandini NS. New insights into improving the oral health of visually impaired children. J Indian Soc Pedod Prev Dent. 2003;21:142–3. [PubMed] [Google Scholar]
- 18.World Health Organization. Visual impairment and blindness. [Last accessed on 2015 Oct 25]. Available from: http://www.who.int/mediacentre/factsheets/fs282/en/index.html .
- 19.Faustino-Silva DD, Ritter F, Nascimento IM, Fontanive PV, Persici S, Rossoni E. Oral health care in preschool children: Perceptions and knowledge of parents or legally responsible persons in a health care center of Porto Alegre, RS. Rev Odonto Cienc. 2008;23:375–9. [Google Scholar]
- 20.Petry PC, Pretto SM. Education and motivation in oral health. In: Kriger L, editor. Brazilian Association of Preventive Dentistry. Oral health promotion. Sao Paulo: Medical Arts; 2003. pp. 371–86. [Google Scholar]
- 21.Goulart AC, Vargas AM. The perception of the visually impaired on the oral health/Blind patients perception about oral health. Arq Odontol. 1998;34:107–19. [Google Scholar]
- 22.Beverley CA, Bath PA, Booth A. Health information needs of visually impaired people: A systematic review of the literature. Health Soc Care Community. 2004;12:1–24. [PubMed] [Google Scholar]


