Abstract
Objective:
The aim of this study was to describe the diameter and the position of the greater palatine foramen (GPF) in relation to adjacent anatomical landmarks in the maxilla in a Lebanese population using cone-beam computed tomography (CBCT) technology.
Materials and Methods:
CBCT images of 58 Lebanese adult patients were included in this study and a total of 116 GPF were evaluated bilaterally. The diameter of the GPF and its position relative to the maxillary molars, and distances to the midline maxillary suture and to the anterior nasal spine were analyzed.
Results:
Of all foramina assessed, 41.38% were located opposite to the third molar, 29.31% were distal to it, 27.59% were between the second and the third, and only 1.72% were opposite to the second. The average diameter was 5.633 mm on the right and 5.723 mm on the left, and the average distances to midline maxillary suture and anterior nasal spine were 16.228 mm and 48.294 mm on the right and 14.907 mm and 48.122 mm on the left, respectively.
Conclusion:
Within the limits of this study, we conclude that in Lebanese patients, the GPF location is variable, very rarely opposite to the second molar, and more closely related to the third, but may present mesial or distal to it in one-fourth of patients.
Keywords: Cone-beam computed tomography, greater palatine foramen, Lebanese population
INTRODUCTION
The greater palatine canal (GPC) transmits the greater palatine nerve and the descending palatine artery from the pterygopalatine fossa to the oral cavity through its lower orifice, the greater palatine foramen (GPF).[1] The GPC is the most common approach to administer local anesthesia to the pterygopalatine fossa in order to anesthetize the maxillary division of the trigeminal nerve. This technique, the maxillary nerve block, produces anesthesia of the entire hemi-maxilla, including teeth, palatal and gingival mucosa, skin of the midface, maxillary sinus, and nasal cavity.[2] It also achieves hemostasis of the nose, essential for various procedures including endoscopic sinus surgery and septorhinoplasty, by the vasoconstriction affecting the maxillary artery.[3] The ability to reliably and accurately locate the GPF is, therefore, essential for specialists in the fields of dentistry, periodontology, maxillofacial surgery, and otolaryngology alike, failure of which commonly results in inadequate anesthesia.[4] Poor knowledge of the GPF location and anatomy can also increase the risk of injury to the greater palatine nerve and vessels.[5] Unfortunately, textbook descriptions of its location are often clinically inadequate: In the postero-lateral border of the palate,[6] near the lateral border of the transverse palatal suture,[7] just anterior to the posterior edge of the hard palate,[3] and between the second and third molar teeth.[8] Even more significantly, the results of numerous published studies indicate that there are variations in the geometrical position of the GPF.[4,9]
In clinical practice, the maxillary molars and the maxillary midline suture (MMS) are among the most useful landmarks that can be used as references when localizing the GPF intraorally, owing to ease of identification and orientation. Numerous studies have been carried out on dry skulls of varying ethnicities and they have reported that the GPF most commonly resides opposite to the third molar.[4,5,10,11,12,13] However, the actual reported proportions range from 47.5%[5] to as high as 92%,[14] highlighting the considerable variability. Although less dramatic, the reported distance from the MMS ranges between 12–13 mm and 16–18 mm, but mostly averages between 14 and 15.5 mm.[4,5,10,11]
One of the major limitations of studies carried out on dry skulls is that they are mostly of unknown gender. This lack of differentiation between males and females results in pooled averages that may apply neither to males nor to females because of the presence of sexual dimorphism.[9,15] Technological advancement of imaging techniques has provided alternatives for detailed and accurate assessments using Computed Tomography (CT)[9,16] and Cone-beam Computed Tomography (CBCT).[14,17] In a recent study conducted on 1500 head CT scans, in addition to reporting different GPC paths and GPF opening locations, Tomaszewska et al. illustrated both sexual dimorphism and side-related differences.[9] Ikuta et al. assessed 50 CBCT images of Brazilian adults, corroborating previous work on dry skulls with respect to distance from the MMS.[14] However, they reported that 92% of GPF were located opposite to the maxillary third molar, which widens the envelope of variability even further.
Variations in the GPF geometry are likely to be, at least in part, the result of ethnic craniofacial differences.[9,18] To address the lack of data on the GPF geometry in the Lebanese population, we assessed the GPF diameter and position relative to adjacent anatomical landmarks using CBCT images in a Lebanese adult population.
MATERIALS AND METHODS
This cross-sectional study was conducted on CBCT scans of 58 Lebanese adult patients attending a private imaging specialized center in Beirut, Lebanon. Patients were referred from different dental clinics for radiological diagnosis, with a range of diverse indications (implants, impacted wisdom teeth, and so on). The study design was approved by the institutional review board, and all the patients were informed that the radiographs might be anonymously used for research purposes at a later stage and their consent were obtained. The field of view (FOV) was selected according to the clinical case, taking into consideration the limitation of the exposure dose.
The inclusion criteria included: (a) Age 18 years or older; (b) presence of all maxillary fully erupted molars on both sides and visualization on CBCT image; and (c) absence of any pathological conditions or deformities of the jaws.
CBCT images of 28 males and 30 females (a total of 116 GPF) with an average age of 42.5 ± 16.26 years met the inclusion criteria and were included in this study. The images were acquired using the PaX-Zenith3D© machine (Vatech, Co., Ltd., Yongin-Si, Republic of Korea) which provides a wide range of FOV between 5 × 5 and 24 × 19 cm and voxel sizes of 0.08–0.3 mm (depending on FOV). Images were obtained at 90 kVp and 7 mA, with an exposure time of 20–35 s and FOV compatible with the indications for referral.
After acquisition, the images were assessed using the proprietary software (EZ 3D©; Vatech Co., Ltd.) on a personal computer (Intel Pentium® D CPU 3.60 GHz, 3.25 GB of RAM running Microsoft Windows 7)
with a 19-inch monitor providing a resolution of 1.280 × 1.024 pixels and contrast of 700:1 (EIZO Nanao Corporation, Hakusan, Japan). The observer was allowed to adjust brightness and contrast, as needed.
One investigator carried out all measurements on the right and left GPF in each CBCT image. For each GPF, four observations were made as follows:
Position relative to maxillary molars [Figure 1a]: In the sagittal view, the GPF location was first identified. Sagittal cut thickness was then set to 20 for visualization of the maxillary molars. Based on the perpendicular line extending from GPF location, GPF position relative was classified into one of four positions: (a) Between the mesial and distal surfaces of the second molar (M2); (b) between the distal surface of the second molar and the mesial surface of the third molar (M2–M3); (c) between the mesial and distal surfaces of the third molar (M3); and d) distal to the distal surface of the third molar, i.e., retromolar (D–M3)
Distance to the anterior nasal spine (ANS): In the axial cut containing the GPF, a middle line (M) was drawn through the ANS and the MMS [Figure 1b]. The measurements were taken from ANS to the right GFP and from ANS to the left GFP
Distance to the maxillary midline suture (MMS): On the same axial cut used to measure distance to ANS [Figure 1b], a perpendicular line was drawn from the medial edge of each GPF toward the line (M)
Opening diameter: The antero-posterior diameter of the GPF was measured in the sagittal view by measuring the distance at the opening of the foramen [Figure 1c].
Figure 1.
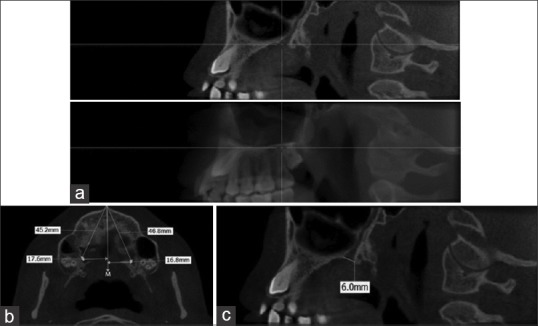
(a) Sagittal cuts illustrating the method of determining position of GPF relative to maxillary molars. Top Figure: small thickness cut shows the opening of GPF. Bottom Figure: full thickness shows the relative position of GPF to the molars. (b) Axial cut illustrating the method of determining position of GPF relative to ANS and MMS. (c) Sagittal cut illustrating the method of measuring antero-posterior diameter of GPF
A total of 11 randomly chosen CBCTs (19%) were selected to assess measurement error and all measurements were repeated by the first examiner 2 weeks after the first readings. Two-way mixed-effects intra-class correlations (ICCs) for absolute agreement on single measures were used to assess intra-examiner reliability for all linear millimeter measurements and for GPF location relative to molars as an ordinal variable.[19] Calculated ICCs were: 0.661 (vertical distance to ANS), 0.782 (horizontal distance to midline), and 0.933 (diameter) on the right; and 0.916 (horizontal distance to midline), 0.517 (vertical distance to ANS), and 0.945 (diameter) on the left. For GPF location relative to molars, ICCs yielded the values 0.754 on the right and 0.6 on the left.
Descriptive statistics of age, gender, GPF diameter and location to craniofacial anatomic structures (ANS and MMS) and position relative to maxillary molars were calculated. Additionally, GPF diameter and position relative to ANS, MMS, and molars were compared between right and left anatomical sides and across genders. Measurements of diameter in millimeters and GPF location were compared between the right and left sides using the paired t test and between males and females using the independent t test. The Chi-square test of association was used to test the difference in percent distribution of GFP location between right and left sides and between genders. Fisher's exact test was applied whenever the expected cell count requirement of 5 was violated. The IBM® SPSS® statistics 20.0 statistical package was used to carry out all statistical analyses. Statistical significance was set at 0.05.
RESULTS
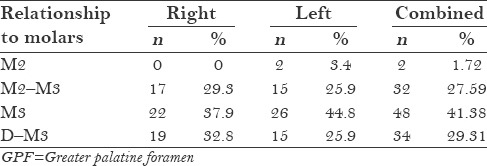
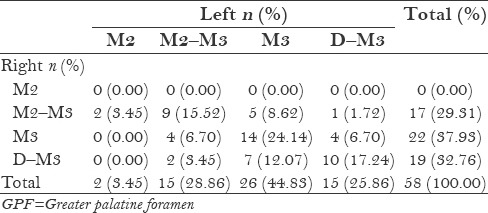
The anatomic location of the GPF varied significantly among the assessed adult population (mean age 42.5 ± 16.261 years). Horizontal distance from the midline ranged from a minimum of 10 mm on the left to a maximum of 24 mm and vertical distance to ANS ranged from 41 to 60 mm [Table 1]. Similarly, the maximum GPF diameter ranged from 3.05 to 8.85 mm on the right and to 10.38 mm on the left. In 98.28% of all cases (both sides combined), the GPF was located distal to the second molar, with an insignificant number of the foramina on the left located opposite to the second molar (1.72% of the whole sample, 3.40% of GPF on the left [Table 2]. The majority of the foramina (41.38%) were located opposite to the maxillary third molar on either side (right or left), with the remaining distributed almost equally mesial and distal to the third molar [Table 2].
Table 1.
Descriptive statistics of subjects’ age and GPF diameter and location relative to anatomical structures (n=58)
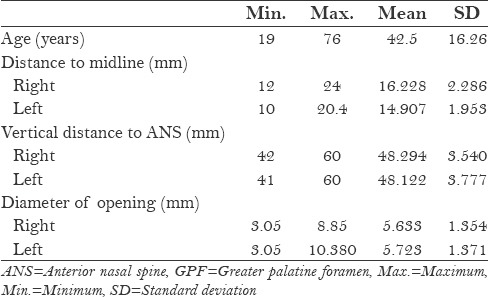
Table 2.
Distribution of GPF location relative to molars (n=58)
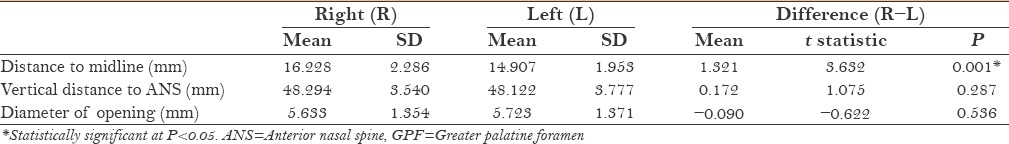
On average, the distance between the GPF and the midline was significantly larger on the right side (16.228 ± 2.286 mm) compared to the left (14.907 ± 1.953 mm), the GPF on the right being on average 1.321 mm further away from the midline than its opposite counterpart. However, neither vertical distance to the anterior spine nor the diameter of opening showed any significant differences between the right and left sides [Table 3].
Table 3.
Distribution of GPF diameter and location relative to anatomical structures by anatomical right or left side (n=58)
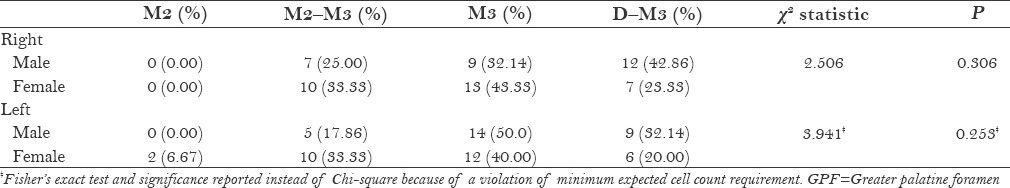
The location of the GPF relative to the molar teeth differed significantly between right and left sides (χ2 = 19.375, P = 0.001). Among the foramina that were located opposite to the third molar or distal to it, a greater proportion on the right side were located distal to the third molar (32.76%) compared to those on the left (25.86%). Similarly, 44.83% of the foramina on the left were located opposite to the third molar, compared to 38.93% on the right side [Table 4].
Table 4.
Percent distribution of GPF position relative to molars by anatomical right or left side (n=58)
The assessed sample was almost equally distributed by gender (48.28% males, n = 28) [Table 5]. On comparing males and females, all distance measurements were statistically significantly larger in males except for the vertical distance to the ANS on the left side (P = 0.079) [Table 5]. The GPF in male subjects was significantly wider in diameter on both sides and was at a larger distance from both the midline horizontally (both sides) and the ANS vertically (on the right side). The difference was greatest for the vertical distance from ANS, at 2.002 mm on the right (P = 0.03), and it was the least for the diameter of opening (1.299 mm on the right, P value 0.000; and 1.120 mm on the left, P = 0.001). However, the percent distribution of the foramina based on their position relative to the molars showed no significant differences by gender [Table 6].
Table 5.
Summary and test statistics for GPF diameter and location relative to anatomical structures by gender
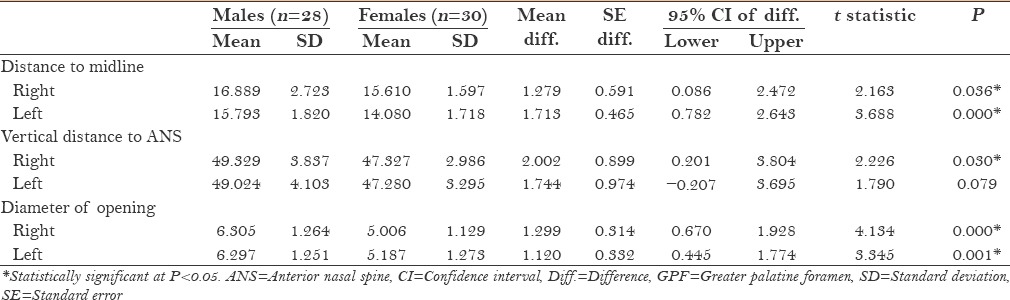
Table 6.
Summary and test statistics for GPF location relative to molars by gender
DISCUSSION
In our sample of Lebanese adults, there was substantial variability in GPF anatomy and location. The variability in GPF diameter and its distance from the MMS and ANS was apparent both in the wide range of values and in the large standard deviations. The maximum observed distance from the MMS was twice as much as the minimum observed distance, whereas the maximum observed antero-posterior GPF diameter was more than 3 times the minimum observed value [Table 1]. Interestingly, the average GPF diameter in our sample is larger than that reported in any other published article. According to a recent systematic review,[9] average values for the antero-posterior diameter of GPF range from 4.5 to 5.3 mm, all of which are lower than our average measures for the entire sample [Table 1] and closer to the average in our female subsample [Table 5]. In a different synthesis of studies assessing GPF distance to the MMS,[13] only 4 out of 22 studies report distances on the right side that fall within 1 mm of our finding (16.22 ± 0.5 mm) in Chinese,[20] Brazilian,[21] Polish,[9] and West Indian populations.[22] In fact, almost 60% of the studies (13 out of 22) report average measures that are at least 1 mm lower than ours, ranging from 14.02 mm[13] to 15.2 mm.[23] On the other hand, in our sample, the distance on the left is strikingly similar to what has been reported in the literature, with 15 out of 22 studies (68.2%) reporting values that fall within 0.5 mm of our finding (14.9 ± 0.5 mm). This contrast highlights the presence of side-related differences in GPF findings. Although this asymmetry in GPF anatomy has not been commonly described in the literature, our results support some reports of side-related differences in the distance to the MMS and in other dimensions including GPF diameter and GPC length.[9,24] Such findings support the more general phenomenon of the predominance of transverse (right/left side) craniofacial asymmetry that has been noted in both children and adults by various authors.[25,26,27]
It is important to note that slightly more than two-thirds of all GPF in our population were located either adjacent to the third molar or distal to it, with a position closer to the second molar being an extremely rare manifestation [Table 2]. Although this finding supports the overwhelming majority of reports associating GPF position to the third rather than the second molar,[13] comparatively few studies have reported a similarly high incidence of retromolar position.[4,28] Unlike our findings, the majority of research suggests a substantial predilection to specifically the third molar region and not mesial or distal to it, with proportions greater than 70% reported in almost 50% of published studies.[13]
Interestingly, GPF position relative to molars displayed significant side-related differences in our sample, suggesting that the location of the GPF bilaterally is not always symmetrical in any one individual [Table 4]. While a similar proportion of foramina was located between the second and third molars on both sides, the remaining tended to be located more mesially on the right side, with a greater proportion located opposite to the second and third molars and a significantly lesser proportion located distal to the third molar compared to the left side. Despite this difference, distance from ANS did not differ between right and left sides, even though both measures assess the antero-posterior position of GPF [Table 3]. One interpretation may be that the difference in GPF location relative to molars is not due to an anatomical difference within the palatine bone, but rather due to asymmetrical antero-posterior positions of molars. Although all CBCT scans were verified for the presence of a complete set of fully erupted maxillary molars, local occlusal disturbances such as impacted or displaced canines and premolars may have accounted for asymmetries in molar position and in arch length. Given the common indication of CBCTs for the diagnosis and treatment planning of impacted canines, this explanation is highly plausible.
Our data also illustrate significant sexual dimorphism in GPF geometry, endorsing previous reports of smaller GPF and GPC dimensions in females.[9,15,22,24] This dimorphism is not surprising in light of consistent reports of male–female differences in various parts of the craniofacial complex.[29,30,31] Although one of our linear measurements did not reach statistical significance in the comparison between sexes (distance to ANS on the left), this may have been the result of coincidence (due to insufficient numbers in the male/female subsamples) or perhaps even due to measurement error. On the other hand, position relative to molars did not show gender dimorphism, supporting the attribution of male–female discrepancy in GPF to differences in skull size rather than to anatomical differences.
Our study is not without limitations. Although intra-examiner reliability was high to very high for most measurements, it was moderate for GPF distance from ANS on both sides. This is in line with several reports of low reproducibility in localizing ANS on CBCT images,[32,33] and is perhaps why, to the best of our knowledge, distance from ANS has not been used to assess GPF location in previous studies on CBCTs. Researchers undertaking future studies on GPF in Lebanese adults may explore the possibility of replacing this measurement with another that is commonly utilized in studies on dry skulls: Distance to the incisive fossa.[11,18,24,34,35] Another source of variability in our study may be the possible inclusion of individuals with incomplete growth. We included all patients with fully erupted molars aged over 18 years, which resulted in the inclusion of three individuals younger than 21, of whom two were males (age 19 and 20 years, respectively). Although sutural transverse growth of the maxilla is believed to stop by the age of 17 in males,[36,37] maxillary antero-posterior growth in length has been noted to continue in males, on average, till the age of 20.04 years.[38]
In addition to supporting the presence of ethnic differences in GPF geometry while comparisons are made of estimations on various populations, our findings highlight substantial variability in the diameter and location of the GPF even within the Lebanese population: Among different individuals, between males and females, and even between right and left sides within the same individual. Clinical administration of the maxillary nerve block must, therefore, be preceded by a thorough inspection for GPF location. The administrator must keep in mind that, in at least one in two Lebanese adults, it may be located not opposite to the third molar but mesial or distal to it, with equal probability.
Finally, although our data suggest the possibility of greater dimensions for GPF diameter and distance from MMS in Lebanese adults compared to other populations, definite conclusions must be delayed until future research validates our results. Should larger dimensions be truly confirmed, other important differences may be possible, including the length of the GPC. A longer canal may explain inadequate anesthesia because of insufficient injection proximity to the maxillary nerve in the pterygopalatine fossa. Consequently, available recommendations for the maxillary nerve block technique based on published averages may not be applicable to the Lebanese population and revised population-specific guidelines would be more appropriate. Future research needs to not only corroborate current findings, but also investigate further into variations in the length of the GPC in Lebanese adults and in GPF opening direction, while ensuring adequate sample size, eliminating possible variations resulting from growth and controlling for the appropriate local occlusal disturbances.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the staff at Charts-Research Design and Biostatistics, especially Dr. Suzanna Al Maaly, for their help in the statistical analysis and write up of the study.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
REFERENCES
- 1.Schünke M, Schulte E, Schumacher U. New York: Thieme; 2007. Thieme Atlas of Anatomy: Head and Neuroanatomy; p. 17. [Google Scholar]
- 2.Norton NS. 2nd ed. Philadelphia: Elsevier Health Sciences; 2011. Netter's Head and Neck Anatomy for Dentistry; p. 553. [Google Scholar]
- 3.Wormald PJ. Endoscopic Sinus Surgery: Anatomy, Three-Dimensional Reconstruction, and Surgical Technique: Thieme. 2011:9. [Google Scholar]
- 4.Chrcanovic BR, Custódio AL. Anatomical variation in the position of the greater palatine foramen. J Oral Sci. 2010;52:109–13. doi: 10.2334/josnusd.52.109. [DOI] [PubMed] [Google Scholar]
- 5.Renu C. The position of greater palatine foramen in the adult human skulls of North Indian origin. J Surg Acad. 2013;3:54–7. [Google Scholar]
- 6.Gardner E, Gray D, O’Rahilly R. 4th ed. Philadelphia: WB Saunders; 1975. Anatomy; p. 997. [Google Scholar]
- 7.Standring S. 40th ed. Philadelphia: Elsevier/Churchill Livingstone; 2008. Gray's Anatomy: The Anatomical Basis of Clinical Practice; p. 414. [Google Scholar]
- 8.Moore KL, Dalley AF, Agur AM. 7th ed. Baltimore, MD: Lippincott Williams and Wilkins; 2013. Clinically oriented anatomy; p. 949. [Google Scholar]
- 9.Tomaszewska IM, Kmiotek EK, Pena IZ, Średniawa M, Czyżowska K, Chrzan R, et al. Computed tomography morphometric analysis of the greater palatine canal: A study of 1,500 head CT scans and a systematic review of literature. Anat Sci Int. 2015;90:287–97. doi: 10.1007/s12565-014-0263-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nimigean V, Nimigean VR, Buţincu L, Sălăvăstru DI, Podoleanu L. Anatomical and clinical considerations regarding the greater palatine foramen. Rom J Morphol Embryol. 2013;54(Suppl):779–83. [PubMed] [Google Scholar]
- 11.Kumar A, Sharma A, Singh P. Assessment of the relative location of greater palatine foramen in adult Indian skulls: Consideration for maxillary nerve block. Eur J Anat. 2011;15:150–4. [Google Scholar]
- 12.Saralaya V, Nayak SR. The relative position of the greater palatine foramen in dry Indian skulls. Singapore Med J. 2007;48:1143–6. [PubMed] [Google Scholar]
- 13.Sarilita E, Soames R. Morphology of the hard palate: A study of dry skulls and review of the literature. Rev Arg de Anat Clin. 2015;7:34–43. [Google Scholar]
- 14.Ikuta CR, Cardoso CL, Ferreira-Júnior O, Lauris JR, Souza PH, Rubira-Bullen IR. Position of the greater palatine foramen: An anatomical study through cone beam computed tomography images. Surg Radiol Anat. 2013;35:837–42. doi: 10.1007/s00276-013-1151-z. [DOI] [PubMed] [Google Scholar]
- 15.Sheikhi M, Zamaninaser A, Jalalian F. Length and anatomic routes of the greater palatine canal as observed by cone beam computed tomography. Dent Res J (Isfahan) 2013;10:155–61. doi: 10.4103/1735-3327.113324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Das S, Kim D, Cannon TY, Ebert CS, Jr, Senior BA. High-resolution computed tomography analysis of the greater palatine canal. Am J Rhinol. 2006;20:603–8. doi: 10.2500/ajr.2006.20.2949. [DOI] [PubMed] [Google Scholar]
- 17.Howard-Swirzinski K, Edwards PC, Saini TS, Norton NS. Length and geometric patterns of the greater palatine canal observed in cone beam computed tomography. Int J Dent 2010. 2010 doi: 10.1155/2010/292753. pii: 292753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siddiqui AU, Gandhi KR, Daimi SR, Saxena S, Trivedi S, Sinha MB, et al. Morphometric assessment of the greater palatine foramen with the adjacent anatomical landmarks. Indian J Anat. 2013;2:61–5. [Google Scholar]
- 19.Hallgren KA. Computing inter-rater reliability for observational data: An overview and tutorial. Tutor Quant Methods Psychol. 2012;8:23–34. doi: 10.20982/tqmp.08.1.p023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang TM, Kuo KJ, Shih C, Ho LL, Liu JC. Assessment of the relative locations of the greater palatine foramen in adult Chinese skulls. Acta Anat (Basel) 1988;132:182–6. doi: 10.1159/000146572. [DOI] [PubMed] [Google Scholar]
- 21.Urbano E, Melo K, Costa S. Morphologic study of the greater palatine canal. J Morphol Sci. 2010;27:102–4. [Google Scholar]
- 22.Dave MR, Yagain VK, Anadkat S. A study of the anatomical variations in the position of the greater palatine foramen in adult human skulls and its clinical significance. Int J Morphol. 2013;31:578–83. [Google Scholar]
- 23.Aterkar S, Rawal PM, Kumar P. Position of greater palatine foramen in adults. J Anat Soc India. 1995;44:126–33. [Google Scholar]
- 24.Teixeira C, Souza V, Marques C, Silva Junior W, Pereira K. Topography of the greater palatine foramen in macerated skulls. J Morphol Sci. 2010;27:88–92. [Google Scholar]
- 25.Rossi M, Ribeiro E, Smith R. Craniofacial asymmetry in development: An anatomical study. Angle Orthod. 2003;73:381–5. doi: 10.1043/0003-3219(2003)073<0381:CAIDAA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Shah SM, Joshi M. An assessment of asymmetry in the normal craniofacial complex. Angle Orthod. 1978;48:141–8. doi: 10.1043/0003-3219(1978)048<0141:AAOAIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Farkas LG, Cheung G. Facial asymmetry in healthy north American caucasians. An anthropometrical study. Angle Orthod. 1981;51:70–7. doi: 10.1043/0003-3219(1981)051<0070:FAIHNA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Langenegger JJ, Lownie JF, Cleaton-Jones PE. The relationship of the greater palatine foramen to the molar teeth and pterygoid hamulus in human skulls. J Dent. 1983;11:249–56. doi: 10.1016/0300-5712(83)90197-5. [DOI] [PubMed] [Google Scholar]
- 29.Bigoni L, Velemínská J, Brůzek J. Three-dimensional geometric morphometric analysis of cranio-facial sexual dimorphism in a Central European sample of known sex. Homo. 2010;61:16–32. doi: 10.1016/j.jchb.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 30.Takegoshi H, Kikuchi S. An anatomic study of the horizontal petrous internal carotid artery: Sex and age differences. Auris Nasus Larynx. 2007;34:297–301. doi: 10.1016/j.anl.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 31.Didia BC, Orish C, Ibeachu PC. Macrometric and micrometric study of sexual dimorphism in moramina of middle crania fossa of adult Nigerians. Int J Morphol. 2010;28:519–24. [Google Scholar]
- 32.Lagravère MO, Low C, Flores-Mir C, Chung R, Carey JP, Heo G, et al. Intraexaminer and interexaminer reliabilities of landmark identification on digitized lateral cephalograms and formatted 3-dimensional cone-beam computerized tomography images. Am J Orthod Dentofacial Orthop. 2010;137:598–604. doi: 10.1016/j.ajodo.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 33.Ludlow JB, Gubler M, Cevidanes L, Mol A. Precision of cephalometric landmark identification: Cone-beam computed tomography vs conventional cephalometric views. Am J Orthod Dentofacial Orthop. 2009;136:312-3.e1–e.10. doi: 10.1016/j.ajodo.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sharma NA, Garud RS. Greater palatine foramen - Key to successful hemimaxillary anaesthesia: A morphometric study and report of a rare aberration. Singapore Med J. 2013;54:152–9. doi: 10.11622/smedj.2013052. [DOI] [PubMed] [Google Scholar]
- 35.Anjankar VP, Gupta S, Nair S, Thaduri N, Trivedi G, Budhiraja V. Analysis of position of greater palatine foramen in central Indian adult skulls: A consideration for maxillary nerve block. Indian J Pharm Biol Res. 2014;2:51–4. [Google Scholar]
- 36.Björk A. Sutural growth of the upper face studied by the implant method. Acta Odontol Scand. 1966;24:109–27. doi: 10.3109/00016356609026122. [DOI] [PubMed] [Google Scholar]
- 37.Björk A, Skieller V. Growth in width of the maxilla studied by the implant method. Scand J Plast Reconstr Surg. 1974;8:26–33. doi: 10.3109/02844317409084367. [DOI] [PubMed] [Google Scholar]
- 38.Nahhas RW, Valiathan M, Sherwood RJ. Variation in timing, duration, intensity, and direction of adolescent growth in the mandible, maxilla, and cranial base: The Fels longitudinal study. Anat Rec (Hoboken) 2014;297:1195–207. doi: 10.1002/ar.22918. [DOI] [PMC free article] [PubMed] [Google Scholar]


