Abstract
Background:
Objectives of the study were to assess the prevalence of tobacco use among the degree students of Oxford institutions in Bangalore city, offer a tobacco cessation intervention for tobacco users among the degree students, and assess the effectiveness of intervention by comparing with the control group.
Materials and Methods:
A randomized control trial was conducted to assess the prevalence of tobacco use and the effectiveness of tobacco cessation behavioral intervention offered to degree students of Oxford institutions in Bangalore city. Then were randomly selected and divided into 55 students in the study group (group A) and 60 students in the control group (group B).
Results:
The effect of intervention of tobacco cessation in group A showed an increase of 29.1% students who stopped using tobacco completely after intervention compared to 15% in group B, and the highest reduction of 21.8% change was noticed in the students using one to five tobacco products per day and the least reduction in percentage (1.8%) change was noticed in the students using one tobacco product per day.
Conclusion:
Findings from the present study suggest that the intervention has suggestive significance on tobacco intervention.
Keywords: Adolescents, nicotine, tobacco cessation
INTRODUCTION
The World Health Organization (WHO), predicts that India will have the fastest rate of rise in deaths attributable to tobacco in the first two decades of the 21st century. Many of these deaths will occur in the productive years of adult life as a consequence of an addiction acquired in youth.[1] Although adolescence is a time of optimum health, adolescents are often inclined to assume behaviors which could damage their health and affect their lifestyle in the future. One such behavior is nicotine dependence, which is the most prevalent, deadliest, costliest, yet the most treatable type of substance dependency.[2] Adolescent tobacco use cessation promises to arrest the physical consequences of use in a rapidly growing and developing body and before the addiction becomes so ingrained that cessation becomes a much more difficult problem.[3]
College students are an important target group for smoking cessation interventions. College students have a higher perception of smoking among their peers and are influenced by this perception. They have more freedom to make personal decisions now than during their schooling. Stress is cited as one of the main reasons for cigarette use among these students. Tobacco companies are more heavily targeting this population through print, media, specialty item distribution, and sponsorship of public entertainment events.[4]
The various treatment approaches include cognitive–behavioral strategies (self-monitoring and coping skills), motivational strategies (techniques to clarify desire for change and reduce ambivalence toward change), and social influence strategies (addressing social influences that serve to promote or maintain smoking). The majority of systematic reviews and meta-analyses of school-based prevention programs have found that curricula using the social influences approach, specifically including normative education and practice of resistance skills, are consistently more effective than curricula adopting other approaches such as information-only or “affective.”[5] Very few intervention studies have been conducted on college prevention programs and there is little information on effectiveness.[4]
Hence, an attempt has been made for the assessment of prevalence of tobacco use and effectiveness of tobacco cessation intervention offered to degree students of Oxford institutions in Bangalore city.
MATERIALS AND METHODS
Randomized controlled trial
Ethical clearance was obtained from the ethical committee of the Oxford Dental College, Hospital and Research Centre, Bangalore, India. Consent forms were prepared in English and consent was obtained from the students of the Oxford institutions as well as from the heads of the concerned institutions. A randomized control trial was conducted to assess the prevalence of tobacco use and the effectiveness of tobacco cessation intervention offered to degree students of Oxford institutions in Bangalore city. There are 32 educational institution offering from UG to PG courses including Dentistry, Nursing, Pharmacy, Physiotherapy, Engineering, Computer Education, Management, Life Science, and Law. The total number of students in these institutions is about 5000. The source of data for this study was the degree students from the Oxford group of institutions, which has 12 degree colleges. Sample size of 155 was obtained while maintaining a statistical power of 90% with 95% confidence level and 5% margin of error (E). Initially, a self-prepared tobacco questionnaire was given to degree college students to assess their smoking behavior by which the prevalence of tobacco use was obtained. There were 248 tobacco users present in the study; out of 248 students, only 115 students gave informed consent for the study. Then, the tobacco users were randomly divided as 55 students in the study group and remaining 60 students in the control group by simple random sampling. Block randomization of the colleges was done to prevent dissemination of the information. The study group students were selected from Dental, Hotel Management, Information Technology and Management, and Commerce. The control group students were selected from Pharmacy, Nursing, Physiotherapy, Fashion Designing, Engineering, Science and Law. Inclusion criteria for the study were being degree students of Oxford institutions for assessing the prevalence of tobacco use; among them, the tobacco users who gave informed consent and were willing to participate in the study. The exclusion criterion was students who were in the final year degree as they might not be available for the complete period of the study and were preparing for their exams. A specially prepared proforma, which included demographic data and smoking behavior, associated with physical and psychological complications and other products of tobacco use was obtained from the tobacco users, and also, Fagerstrom test was done using Fagerstrom questionnaire and a carbon monoxide (CO) grade was estimated by using smokerlyzer instrument. ’Fagerstrom questionnaire used by the Arizona Smokers’ helpline’.[6] The tool has been paired to six simple questions. Scoring was been recorded to assist in tailoring nicotine cessation advice to fit the individual needs. The degree of nicotine dependency was assessed by Fagerstrom's test. Depending on the answer that each smoker gives to each question, a certain mark is given, that may vary from 0 to 10 points. A degree of slight dependency is considered when the test result ranges from 0 to 3 points; moderate dependency is from 4 to 6 points; a severe degree of dependency is 7 points or over. The Micro CO is a powerful diagnostic tool for measuring alveolar CO in ppm concentrations and percentage carboxyhemoglobin (COHB). The Smoke Check is designed as a simple screening test for cigarette consumption, giving an instant indication of CO levels in ppm and backed up with color light indicators. The Smoke Check is the most cost-effective CO monitor available today. Conversion of ppm results to % COHB is easily done using the Smoke Check's smoking cessation guide chart. A self-help guide obtained from National Institute of Mental Health and Neuro Sciences (NIMHANS) which contains the reasons to quit tobacco, readiness to quit, how to quit, dealing with withdrawal symptoms, and self-help tips for tobacco quitting was given to the students in the third session. The self-help material was obtained from the institution to be given to the students. The training of the intervener was done in Tobacco Cessation Center (TCC), NIMHANS, Bangalore, for the duration of 1 month. The study was systematically scheduled to spread over a period of 6 months from May 2010 to October 2010. In these sessions, the intervener was trained to give counseling regarding tobacco cessation for the subjects. The Chairman of the Oxford group of institutions was approached, the purpose of the study was explained, and his approval was obtained to proceed with the study. Also, permission from the principals of respective colleges was obtained to conduct the study. A pilot study was undertaken on 10% of the study population (degree students). For the main study, the study sample was divided into two groups: Study group (group A) and control group (group B). Four sessions of intervention were administered to the students of group A. They were administered the intervention after they were grouped into four subgroups which included A1, A2, A3, and A4 with 15 students in each group. In the control group (group B), no intervention was given to the students. The first session consisted of distributing self-help material to the students. The topics for intervention included: Introduction to tobacco, prevalence of tobacco use, effects of tobacco use in general health and dental health, psychosocial factors influencing tobacco use, healthy diet, and behavioral intervention for prevention of tobacco use. The second session intervention was given within 15 days after the first intervention. In this session, group A students were intervened in their individual subgroup (A1, A2, A3, and A4). The content for discussion included the assessment of high-risk situation and enhancement of motivation and the role of high-risk situation with tobacco use/quitting. The third session intervention was given in the 4th month. In this session, group A students were intervened in their individual subgroup (A1, A2, A3, and A4). The content for discussion included reflection of previous session discussion. Management of high-risk situation and educational material on tobacco use were given, and enhancement of self-efficacy by motivation and evaluation were done after 1 week of the third session. The fourth session intervention was given in the 5th month; in this session, group A students were intervened in their individual subgroup (A1, A2, A3, and A4). The content for discussion were enhancing their self-efficacy for quitting tobacco, reinforcement for tobacco cessation, and feedback, and evaluation was done. At the 6th month follow-up, the same proforma was used and, also, Fagerstrom test was done by using Fagerstrom questionnaire and a CO grade was estimated by using smokerlyzer instrument for both the study and control groups. Education and intervention was given for the control group. Descriptive statistical analysis was carried out in the present study. Significance was assessed at 5% level and 95% confidence interval. Chi-square/Fisher exact test was used to find the significance of the study parameters on a categorical scale between two or more groups.
RESULTS
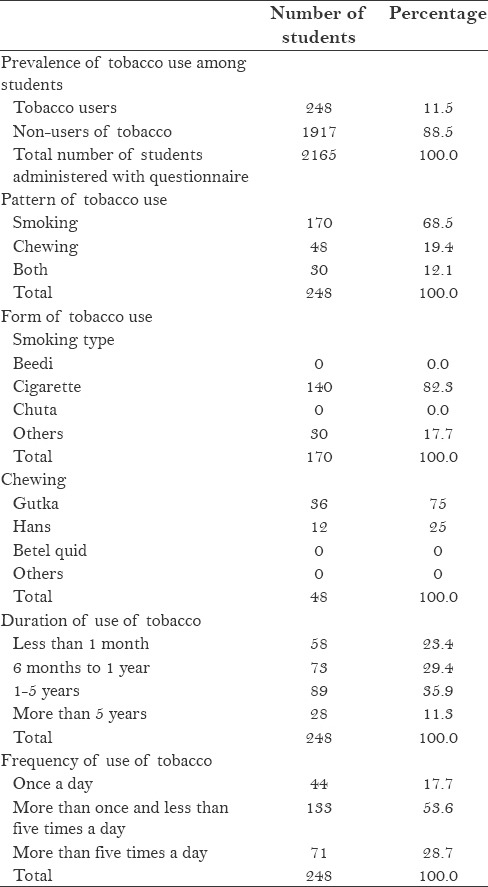
Prevalence and characteristics of tobacco users among the study population are presented in Table 1. A total of 2165 students were administered the questionnaire, of which 248 (11.5%) students were tobacco users and 1917 (88.5%) students were non-users of tobacco. Of the 248 tobacco users, 68.5% of students were smokers, 19.4% of students used smokeless tobacco, and 12.1% of students used both forms of tobacco (smoking and smokeless). Out of 248 students, only 115 (46.4%) students were willing to participate and thus were included in the study. Distribution of study subjects with regard to abstaining from tobacco use showed that around 12.7% students in group A and 21.7% students in group B could abstain from tobacco use for 1 day, 21.8% students in group A and 21.7% students in group B could abstain from tobacco use for 1 week, 23.6% students in group A and 20% students in group B could abstain from tobacco use for 1 month, and 12.7% students in group A and 16.6% students in group B could abstain from tobacco use for more than 6 months. Also, 29.1% students in group A and 20% students in group B were not recorded because they never tried to quit tobacco.
Table 1.
Prevalence and characteristics of tobacco users among study population
Distribution of students according to the CO levels was statistically similar between the two groups (P = 0.280). Distribution of the study subjects according to tobacco usage before and after intervention in group A is shown in Table 2. The effect of intervention of tobacco cessation in group A showed a positive percentage increase of 29.1% showing that they stopped using tobacco completely after intervention. The highest reduction in percentage (21.8%) change was noticed in the students using one to five tobacco products per day and the least reduction in percentage (1.8%) change was noticed in the students using one tobacco product per day. Also, it increased to 3.6% in the students using more than 10 tobacco products per day. The response for the average use of tobacco per day was strongly significant after intervention with P ≤ 0.001. A reduction in percentage change of 7.3% was found among those who said there was no association between smoking and alcohol after intervention. The total 29.1% increase in the students was gained to quit tobacco use after intervention. The response rate for the reason association between smoking and alcohol was not significant after the intervention with P ≤ 0.451. Before intervention, 72.7% students were willing to quit tobacco and 30.9% students were not willing to quit the habit. After intervention, 16 (29%) students quit the habit.
Table 2.
Distribution of study subjects according to tobacco usage before and after intervention in group A students
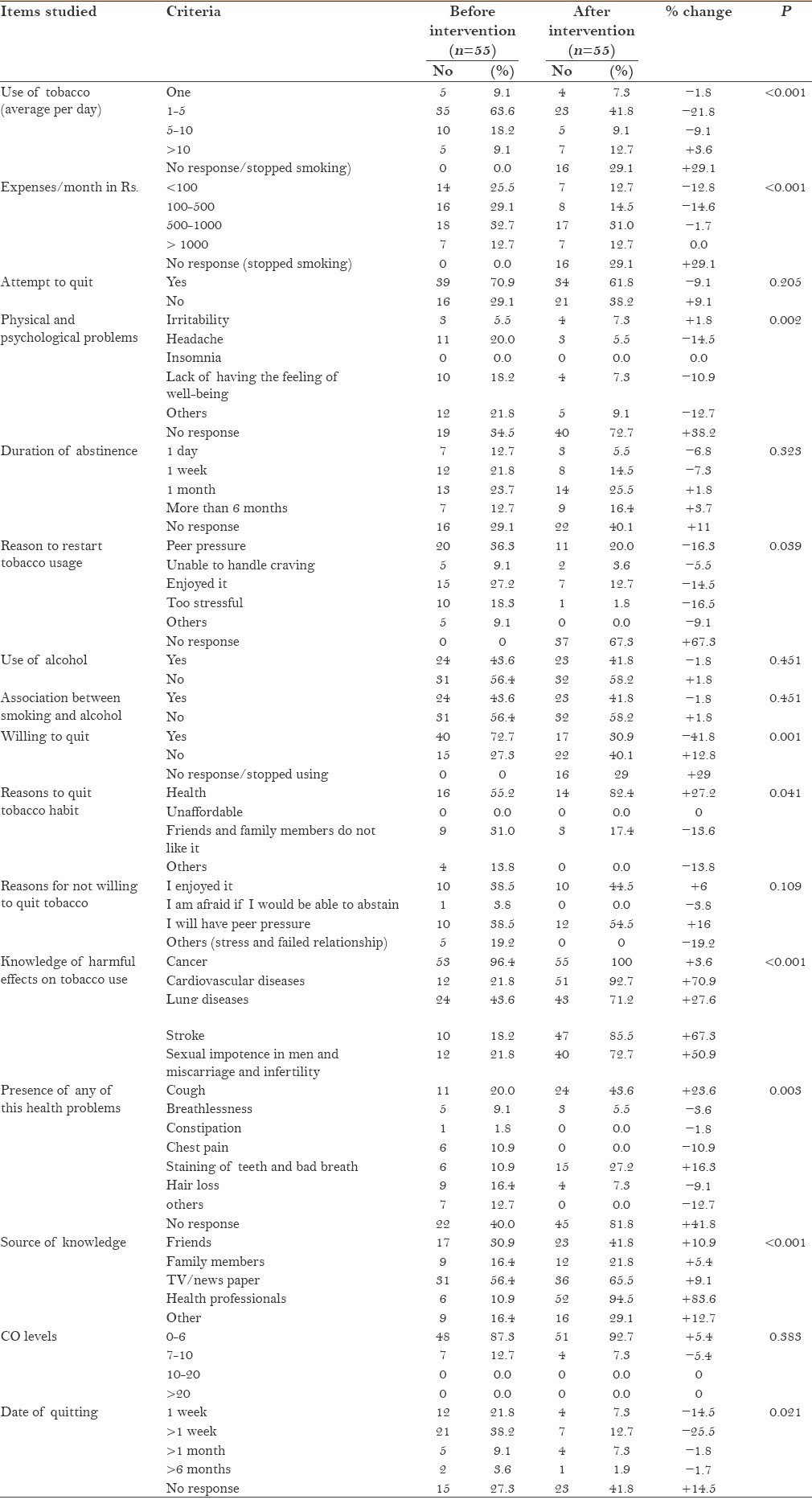
The response for willing to quit tobacco use was strongly significant after intervention with P ≤ 0.001. Before intervention, about 55.2% students in this category wanted to quit due to health problems, followed by 31% students due to the pressure of friends and family members who do not like tobacco usage and 13.8% students for other reasons. The same factors were the reasons after intervention too. The response for the reason for not willing to quit tobacco use was not significant after intervention with P ≤ 0.109. Their knowledge regarding the harmful effects of tobacco increased after intervention. Though majority (96.4% students) regarded cancer as the most harmful effect of tobacco before intervention, the intervention increased knowledge regarding the other harmful effects of tobacco substantially. The response for the knowledge of harmful effects on tobacco use was strongly significant after intervention with P ≤ 0.001. Before intervention, 22 (40%) students did not have any of the health problems and the others faced cough (20% students) and hair loss (16.4% students) as the major health problems.
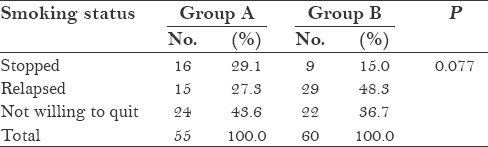
The major sources of knowledge regarding tobacco before intervention were TV/news papers (56.4% students) and friends (30.9% students). Only 10.9% of the students got the information from health professionals. After intervention, the major source of information was from health professionals (94.5% students), TV (65.5% students), and friends (41.8% students). The response for the source of knowledge on tobacco use was strongly significant after intervention with P ≤ 0.001. Distribution of the study subjects according to the effect of intervention on smoking status is given in Table 3. An increase in percentage (14%) of students who stopped tobacco use was noticed among the students of group A after intervention. Incidence of relapse was significantly more in group B compared to group A (48.3% vs 27.3% students) with P = 0.077. Students not willing to quit the habit were more in group A (43.6%) when compared to group B (36.7%) students. Distribution of study subjects according to Fagerstrom/smoking analysis in group A showed an increase in percentage change of 1.9% and 3.8% in the very low dependence and in high dependence categories, respectively. Also, reduction of 5.7% was seen in the low dependence category. In group B, an increase in percentage change of 5.8% was seen in the very low dependence category. Also, reduction of 3.9% and 1.9% was seen in the low dependence and very high dependence categories, respectively. These results cannot be generalized because only students have been included in the study.
Table 3.
Distribution of study subjects according to the effect of intervention on smoking status
DISCUSSION
Young people explore new roles, develop new skills, and begin to consider their future as adults during the teenage years. Therefore, the role of competence skills is highly relevant to understanding the course of adolescent development.[7] Tobacco use and health are intimately related; thus, tobacco use among students is an important issue.[8] Preventive approaches that focus on psychosocial factors associated with drug use initiation and those that emphasize the teaching of social resistance skills either alone or in combination with generic personal and social tactics are effective.[6]
In India, it is generally thought that smoking by girls is socially unacceptable and, therefore, they do not smoke, but in the Northeastern states, a high smoking prevalence has been reported among girls, ranging from 28% in Mizoram to 8.3% in Arunachal Pradesh.[7]
In the present study preferred smoking (68.5%) followed by chewing (19.4%) tobacco. Also, 12.1% of the students used both forms of tobacco. Prevalence of tobacco use in this study was 68.5%, which is higher when compared to 14.4% reported in a study done in Iran.[9] Among smokers, 82.3% preferred cigarette, and 75.5% of the students preferred gutkha form among the smokeless tobacco users. Majority (35.9%) of them used tobacco for 1–5 years, and 53.6% of students used tobacco more than once and less than five times a day.
The majority of the school children started to smoke between 15 and 18 years of age. Whereas in the studies of Aslan et al. and Singh et al.,[10,11] the habit was found to have started much early at 10 years. Early smoking can be regarded as a specific health and psychosociological problem. It has been shown that young people are more reluctant to give up smoking, possibly due to greater addiction to nicotine.[12]
The period of abstinence was positive for 1 month and more than 6 months in group A with intervention. The important variables favoring abstinence for more than a year were increase in age, higher socioeconomic status, male sex, and presence of respiratory symptoms. The odds ratio was higher for Bangalore and Chandigarh versus Delhi or Kanpur.[13] In the present study, 34.4% students in both groups attempted to quit at least 1 day, which is less when compared to 54% reported in the study of Susan.[14]
One of the primary reasons for the failure of smoking prevention and cessation programs among young adult smokers is that they are less likely to be concerned about the health risks of smoking than older smokers. They believe that the health consequences occur much later in life and the health risks of smoking are not clear to them. The CO levels decreased to lower levels in both groups A and B. The reduction was more in the control group (group B) after 6 months. Regarding nicotine dependence (Fagerstrom Test for Nicotine Dependence scores) and daily cigarette consumption, there was a significant reduction from baseline to each of the follow-up sessions. The treatment group also displayed an increase in Fagerstrom Test for Nicotine Dependence scores from 3 months to the subsequent follow-up sessions, relative to smokers in the comparison group, whose nicotine dependence tended to decline.[15] Finally, the students who stopped smoking were more in group A after intervention than in group B without intervention after 6 months. The relapse was more in group B than group A after intervention. The students who were not willing to quit were more in group A after intervention than group B. In this study, there was decrease in smoking cases and relapse cases in group A after intervention than group B, but it was only a minor change. Another possible reason for the small cessation effect is the less than anticipated sample size and consequent reduction in statistical power to detect group differences.[10]
Young adults who initiate late smoking and college students may experience greater success at quitting than early initiators. Any prevention and cessation program for adolescents or young adults needs to multiple ways by which tobacco is used.[16]
CONCLUSION
It is concluded from the study that majority of the students were found to be smokers and started using tobacco product for style and fun and by the influence of friends in both groups. Findings from the present study suggest that the intervention has suggestive significance on tobacco usage. Their knowledge regarding the harmful effects of tobacco increased after intervention. This may be explained mainly by factors such as peer influence and psychosocial aspects related to tobacco usage.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Reddy KS, Gupta PC. New Delhi, India: Ministry of Health and Family Welfare; 2004. Report on Tobacco Control in India. [Google Scholar]
- 2.Ziaaddini H, Meymandi MS, Zarezadeh A. The Prevalence and Motivation of Cigarette Smoking among Kerman high school students. Iran J Psychiatry. 2007;2:41–5. [Google Scholar]
- 3.Sussman S. Effects of sixty six adolescent tobacco use cessation trials and seventeen prospective studies of self-initiated quitting. Tob Induc Dis. 2002;1:35–81. doi: 10.1186/1617-9625-1-1-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolburg JM. Misguided optimism among college student smokers: Leveraging their quit-smoking strategies for smoking cessation campaigns. The Journal of Consumer Affairs. 2009;43:305–331. [Google Scholar]
- 5.Stead M, McDermott L, Gordon R, Angus K, Hastings G. London: National Social Marketing Centre for excellence; 2006. A review of the effectiveness of social marketing alcohol, tobacco and substance misuse interventions. [Google Scholar]
- 6.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The fagerström test for nicotine dependence: A rvision of the fagerström tolerance questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 7.Botvin GJ, Griffin KW. Life skills training as a primary prevention approach for adolescent drug abuse and other problem behaviors. Int J Emerg Ment Health. 2002;4:41–7. [PubMed] [Google Scholar]
- 8.Singh VV, Singh CZ, Banerjee CA, Basannar DR. Determinants of smoking habit among medical students. MJAFI. 2003;59:209–11. doi: 10.1016/S0377-1237(03)80008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nazary AA, Ahmadi F, Vaismoradi M, Kaviani K, Arezomandi M, Faghihzadeh S. Smoking among male medical sciences students in Semnan, Islamic Republic of Iran. East Mediterr Health J. 2010;16:156–61. [PubMed] [Google Scholar]
- 10.Aslan D, Bilir N, Ozcebe H, Stock C, Kucuk N. Prevalence and determinants of adolescent smoking in Ankara, Turkey. Turkjcancer. 2006;36:49–56. [Google Scholar]
- 11.Singh R, Kour H, Jindal SK, Aggarwal AN, Gupta D, Khan GQ. Global Youth Tobacco Survey: A Report from Jammu and Kashmir. JK Science. 2008;10:65–9. [Google Scholar]
- 12.Sieminska A, Jassem E, Konopa K, Damps I, Slominski JM. The prevalence of cigarette smoking among school pupils staying at summer camps. Int J Tuberc Lung Dis. 2000;4:1009–15. [PubMed] [Google Scholar]
- 13.Jindal SK, Aggarwal AN, Chaudhry K, Chhabra SK, D’Souza GA, Gupta D, et al. Asthma Epidemiology Study Group. Tobacco smoking in India: Prevalence, Quit-rates and Respiratory Morbidity. Indian J Chest Dis Allied Sci. 2006;48:37–42. [PubMed] [Google Scholar]
- 14.Moran S, Wechsler H, Rigotti NA. Social smoking among US college students. Pediatrics. 2004;114:1028–34. doi: 10.1542/peds.2003-0558-L. [DOI] [PubMed] [Google Scholar]
- 15.Williams C, Garland A. A cognitive–behavioural therapy assessment model for use in everyday clinical practice. Advances in Psychiatric Treatment. 2002;8:172–9. [Google Scholar]
- 16.Backinger CL, Fagan P, Matthews E, Grana R. Adolescent and young adult tobacco prevention and cessation: Current status and future directions. Tob Control. 2003;12(Suppl 4):IV46–53. doi: 10.1136/tc.12.suppl_4.iv46. [DOI] [PMC free article] [PubMed] [Google Scholar]


