Abstract
Background:
Mindfulness- and acceptance-based interventions are increasingly studied as a potential treatment for a variety of mental conditions.
Objective:
To assess the effects of mindfulness- and acceptance-based interventions on psychotic symptoms and hospitalization in patients with psychosis
Methods:
MEDLINE/PubMed, Embase, the Cochrane Library, and PsycINFO were screened from inception through April 2015. Randomized controlled trials (RCTs) were analyzed when they assessed psychotic symptoms or hospitalization in patients with psychosis; affect, acceptance, mindfulness, and safety were defined as secondary outcomes.
Results:
Eight RCTs with a total of 434 patients comparing mindfulness-based (4 RCTs) or acceptance-based interventions (4 RCTs) to treatment as usual or attention control were included. Six RCTs had low risk of bias. Moderate evidence was found for short-term effects on total psychotic symptoms, positive symptoms, hospitalization rates, duration of hospitalization, and mindfulness and for long-term effects on total psychotic symptoms and duration of hospitalization. No evidence was found for effects on negative symptoms, affect, or acceptance. No serious adverse events were reported.
Conclusion:
Mindfulness- and acceptance-based interventions can be recommended as an additional treatment for patients with psychosis.
Key Words: Psychosis, acceptance, mindfulness, systematic review, meta-analysis
摘要
背景:作为各种精神疾病的潜在治疗,基于正念和无怨接受的干预正得到越来越多的研究。
目的:评估基于正念和无怨接受的干预对精神病患者的精神病症状和住院治疗的影响
方法:从开始到 2015 年 4 月筛选了MEDLINE/PubMed、Embase, Cochrane Library 和 PsycINFO。评估精神病患者的精神病症状或住院治疗时,分析了随机对照试验 (Randomized Controlled Trial, RCT);情绪反应、无怨接受、正念以及安全被定义为次要结果。
结果:包括 8 项 RCT,共计 434名患者,对基于正念(4 项 RCT)或基于无怨接受(4 项 RCT)的干预与常规治疗或注意力控制进行了比较。6 项 RCT 具有低偏倚风险。发现了对总体精神病症状、阳性症状、住院率、住院持续时间和正念具有短期影响,对总体精神病症状和住院持续时间具有长期影响的适度证据。未发现对阴性症状、情绪反应或无怨接受有影响的证据。未曾报告严重不良事件。
结论:基于正念和无怨接受的干预可推荐为精神病患者的附加治疗。
SINOPSIS
Antecedentes:
Las intervenciones basadas en la conciencia plena y la aceptación se estudian cada vez más como posible tratamiento para varios trastornos mentales.
Objetivo:
Evaluar los efectos de las intervenciones basadas en la conciencia plena y la aceptación en los síntomas psicóticos y en la hospitalización de los pacientes con psicosis
Métodos:
Se examinaron MEDLINE/PubMed, Embase, la bibliografía de Cochrane y PsycINFO desde su creación hasta abril de 2015. Se analizaron los ensayos aleatorizados comparativos (EAC) que evaluaban los síntomas psicóticos o la hospitalización de los pacientes con psicosis; como resultados secundarios se definieron el afecto, la aceptación, la conciencia plena y la seguridad.
Resultados:
Se incluyeron ocho EAC con un total de 434 pacientes que comparaban las intervenciones basadas en la conciencia plena (4 EAC) o las intervenciones basadas en la aceptación (4 EAC) con el tratamiento normal o con el control de atención. Seis EAC tuvieron un bajo riesgo de sesgos. Se observaron evidencias moderadas para los efectos a corto plazo de los síntomas psicóticos totales, los síntomas positivos, los índices de hospitalización, la duración de la hospitalización y la conciencia plena y para los efectos a largo plazo de los síntomas psicóticos totales y la duración de la hospitalización. No se observaron evidencias en los efectos sobre los síntomas negativos, el afecto o la aceptación. No se comunicaron acontecimiento adversos graves.
Conclusión:
Las intervenciones basadas en la conciencia plena y la aceptación pueden recomendarse como tratamiento adicional para los pacientes con psicosis.
INTRODUCTION
Psychotic disorders are severe mental conditions that typically manifest themselves mainly by positive symptoms (delusions and hallucinations) and negative symptoms (lack of motivation, reduction in spontaneous speech, and social withdrawal).1,2 These disorders are typically chronic in nature and often restrict quality of life and social function.3–5 Even when patients are compliant to psychopharmaceutical treatment, symptoms, especially negative symptoms, often persist,2,6 and about 30% of patients are therapy refractory.7
Mindfulness- and acceptance-based interventions are increasingly studied as a potential treatment for a variety of physical8–11 and mental conditions.10,12,13 Despite conceptual differences between different acceptance- and mindfulness-based interventions, they share many theoretical underpinnings. These approaches do not try to alter the content of dysfunctional thoughts and symptoms but to alter the patients' relationship towards these thoughts and symptoms. A mindful and accepting observation of every pleasant or unpleasant experience (including thoughts) in the present moment is intended.14,15 However, the specific techniques that are used to achieve this goal differ between different approaches.13 Primarily mindfulness-based interventions like mindfulness-based cognitive therapy (MBCT) or mindfulness-based stress reduction (MBSR) that are more or less direct translations of Buddhist mindfulness traditions into Western medicine use formal mindfulness training like sitting or walking meditation as a main intervention.15,16 While MBSR has been originally designed as an intervention for chronic pain and stress-related symptoms, MBCT combines MBSR with cognitive-behavioral therapy and is normally led by a trained therapist.15,16 MBCT thus focuses more on a therapeutic approach rather than general stress reduction.16 On the other hand, primarily acceptance-based interventions like acceptance and commitment therapy (ACT) or acceptance-based behavior therapy (ABBT) are multimodal approaches that have integrated cognitive interventions into a theoretical framework of mindfulness and acceptance and include shorter and more informal mindfulness exercise.13,14,17 Another major difference between primarily mindfulness-based and primarily acceptance-based intervention is that the former are mostly offered as group sessions16 and the latter mostly as individual sessions.14
As patients with psychotic disorders frequently engage in avoidance strategies like substance abuse or distraction—or on the other extreme, may become engrossed by their symptoms—mindfulness- and acceptance-based interventions have been proposed as approaches to alter the patients' relationship towards their symptoms and hence reduce symptom-related distress.18
The aim of this systematic review and meta-analysis was to investigate whether mindfulness- and acceptance-based interventions are effective and safe interventions for reducing psychotic symptoms and hospitalization in patients with psychosis.
METHODS
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for systematic reviews and meta-analyses19 and the recommendations of the Cochrane Collaboration20 were followed.
Eligibility Criteria
Types of Studies
Randomized controlled trials (RCTs) were eligible. No language restrictions were applied.
Types of Participants
Adults with psychotic disorders (ie, schizophrenia, schizoaffective disorder, schizophreniform disorder, delusional disorder, brief psychotic disorder, and psychotic disorder not otherwise specified) were eligible if they were diagnosed by
the Diagnostic and Statistical Manual, 4th Edition, Revised (DSM-IVR),1 the Research Diagnostic Criteria (RDC),21 or the International Classification of Disease22 (ICD)22;
any other clinician-based diagnosis criterion; or
unclear diagnostic criteria but were currently treated for psychotic disorders.
Studies involving participants with comorbid physical or mental disorders were eligible for inclusion.
Types of Interventions
Experimental
Other, less common interventions were also eligible if they were clearly based on mindfulness or acceptance.
Control
Treatment as usual,
attention control, or
other active nonpharmacological interventions were eligible.
Types of Outcome Measures
To be eligible, RCTs had to assess at least 1 primary outcome:
improvement in the severity of symptoms of psychosis, measured by clinician-rated scales, such as the Brief Psychiatric Rating Scale,23 the Positive and Negative Syndrome Scale,24 the Clinical Global Impression Scale,25 or any other validated scale; or
hospitalization, assessed as number of hospitalized patients or days in hospital in a predefined follow-up period.
Secondary outcomes included
- affect, assessed as
acceptance, assessed by validated scales such as the Acceptance and Action Questionnaire II30;
mindfulness, assessed by validated scales such as the Kentucky Inventory of Mindfulness Skills31; and
safety of the intervention assessed as amount of extrapyramidal symptoms or number of adverse events.
Search Methods
Medline/PubMed, Embase, the Cochrane Library, and PsycINFO were searched from their inception through April 13, 2015. The literature search was constructed around search terms for “mindfulness- and acceptance-based interventions” and search terms for “psychosis.” For PubMed, the following search strategy was used: (Psychotic Disorders[MeSH Terms] OR Paranoid Disorders[MeSH Terms]OR Affective Disorders, Psychotic[MeSH Terms] OR Psychosis[Title/Abstract] OR Psychotic[Title/Abstract] OR Schizophrenia[MeSH Terms] OR Schizophrenia[Title/Abstract] OR Schizophrenic[Title/Abstract] OR Schizoaffective[Title/Abstract]) AND (Mindfulness[Title/Abstract] OR MBSR[Title/Abstract] OR MBCT[Title/Abstract] OR Acceptance-based[Title/Abstract] OR (Acceptance[Title/Abstract] AND Commitment[Title/Abstract])). The search strategy was adapted for each database as necessary.
Additionally, reference lists of identified original articles or reviews were searched manually, and the Mindfulness Research Guide (www.mindfulexperience.org) was screened.
Two review authors independently screened abstracts identified during literature search and read potentially eligible articles in full to determine whether they met the eligibility criteria. Disagreements were discussed with a third review author until consensus was reached.
Data Extraction and Management
Two authors independently extracted data on patients (eg, age, gender, diagnosis); interventions (eg, type, frequency, duration); control interventions (eg, type, frequency, duration); cointerventions; outcomes (eg, outcome measures, assessment timepoints); and results using an a priori developed data extraction form. Discrepancies were discussed with a third review author until consensus was reached.
Risk of Bias in Individual Studies
Risk of bias was assessed by 2 review authors independently using the risk of bias tool proposed by the Cochrane Back Review Group.32 This tool assesses risk of bias on the following domains: selection bias, performance bias, attrition bias, reporting bias, and detection bias using 12 criteria as (1) low risk of bias, (2) unclear risk of bias, or (3) high risk of bias. Discrepancies were discussed with a third review author until consensus is reached. Studies that met at least 6 of the 12 criteria and had no serious flaws were rated as having low risk of bias. Studies that met fewer than 6 criteria or had a serious flaw were rated as having high risk of bias.32
Data Analysis
Assessment of Effect Size
Separate meta-analyses were planned for
short-term (outcome measures taken closest to 4 weeks after the intervention) and long-term effects (closest to 12 months after the intervention) and
different control interventions (treatment as usual, attention control, other) using Review Manager 5 software (Version 5.2, The Nordic Cochrane Centre, Copenhagen) by a random effects model.20 Meta-analyses were conducted if at least 2 RCTs for a specific comparison were available.20
For continuous outcomes, standardized mean differences (SMDs) with 95% confidence intervals (CIs) were calculated as the difference in means between groups divided by the pooled standard deviation. A negative SMD was defined as indicating beneficial effects of the intervention compared to the control intervention for symptoms and affect while a positive SMD was defined to indicate beneficial effects for acceptance and mindfulness. If necessary, scores were inverted by subtracting the mean from zero.20
To evaluate the magnitude of the overall effect size, Cohen's categories were used with (1) SMD=0.2 to 0.5, small; (2) SMD=0.5 to 0.8, moderate; and (3) SMD>0.8, large effect sizes.33
For dichotomous outcomes, risk ratios (RRs) with 95% CI were calculated by dividing the risk of event in the experimental group (ie, the number of participants with the respective outcome divided by the total number of participants) by the risk of event in the control group.20
Levels of evidence were determined using the van Tulder recommendations as (1) strong evidence: consistent findings among multiple RCTs with low risk of bias; (2) moderate evidence: consistent findings among multiple high-risk RCTs and/or 1 low-risk RCT; (3) limited evidence: 1 RCT with high risk of bias; (4) conflicting evidence: inconsistent findings among multiple RCTs; and (5) no evidence: no RCTs.34
Assessment of Heterogeneity
To analyze statistical heterogeneity between studies, the I2 statistics, a measure of how much variance between studies can be attributed to differences between studies rather than chance, was calculated. The magnitude of heterogeneity was categorized as (1) I2=0%-25%, low heterogeneity; (2) I2=26%-50%, moderate heterogeneity; (3) I2=51%-75%, substantial heterogeneity; and (4) I2=76%-100%, considerable heterogeneity.35 The chi2 test was used to assess whether differences in results were compatible with chance alone. Given the low power of this test when only few studies or studies with low sample size are included in a meta-analysis, a P value≤0.10 was regarded to indicate significant heterogeneity.20
Subgroup and Sensitivity Analyses
Subgroup analyses were conducted for
type of intervention (primarily acceptance-based such as ACT or ABBT or primarily mindfulness-based such as MBCT or MBSR) and
type of participants (manual-based diagnosis; other or unclear diagnosis).
Subgroup differences were tested using a chi2 test for heterogeneity across subgroup. I2 statistics for subgroup differences were computed as the percentage of the variance between the different subgroups that is due to genuine subgroup differences rather than chance.20
To test the robustness of significant results, sensitivity analyses were conducted for studies with high vs low risk of bias. If statistical heterogeneity was present in the respective meta-analysis, subgroup and sensitivity analyses were also used to explore possible reasons for heterogeneity.
Risk of Bias Across Studies
Assessment of risk of publication bias was originally planned by investigation of funnel plot asymmetry (using Review Manager 5 software) if at least 10 studies were included in a meta-analysis.36 However, as less than 10 studies were included in each meta-analysis, funnel plots were not analyzed.
RESULTS
Literature Search
Three hundred seventy-two records were retrieved in the literature search. Of 247 nonduplicate records, 238 were excluded because they were not randomized, did not include patients with psychosis, and/or did not include mindfulness- or acceptance-based interventions. Nine full-text articles on 8 RCTs with a total of 434 patients were assessed for eligibility.37–45 All 8 RCTs were included in qualitative analysis and meta-analysis (Figure 1).
Figure 1.
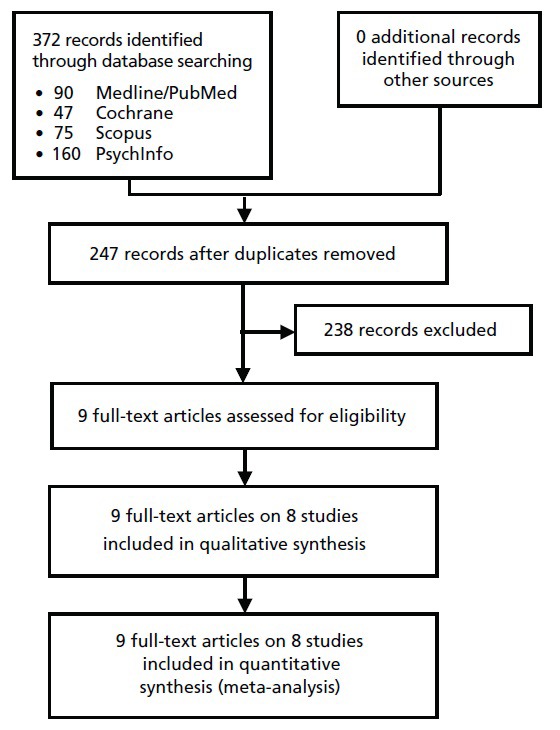
Flowchart of the results of the literature search.
Study Characteristics
Characteristics of the sample, interventions, outcome assessment, and results are shown in Table 1.
Table 1.
Characteristics of the Included Studies
| Reference | Patients | Co-interventions | Intervention groups (program length, frequency, duration) | |
|---|---|---|---|---|
| Treatment | Control | |||
| Bach & Hayes (2002) Bach et al (2012) |
80 hospitalized patients experiencing positive psychotic symptoms (auditory hallucinations, delusions) Diagnoses: Schizophrenia, schizoaffective disorder, mood disorder with psychotic feature, delusional disorder, psychosis NOS Mean age: 39.2 y (ACT), 39.5 y (TAU) |
TAU |
ACT 4 × 45-50 minutes every 2 to 3 days + TAU |
TAU Medication, minimum of 3 sessions psychoeducation group, Minimum of 1 session of individual psychotherapy After discharge: case management, 1 monthly visit to the psychiatrist, medication |
| Chadwick et al (2009) | 22 outpatients with psychotic disorders with auditory hallucinations Diagnosis: schizophrenia according to DSM-IV Mean age: 22.6±8.1 y |
Antipsychotic medication | Mindfulness training Meditation, group discussion, training of awareness in breathing and body Weeks 1-5: 2 × weekly + home practice with CD, Weeks 6-10: home practice |
Waiting list control No specific therapy |
| Chien & Lee (2013) | 96 outpatient patients with schizophrenia Diagnosis of schizophrenia according to DSM-IV Mean age: 25.8±8.5 y |
TAU |
MBPP 12 biweekly × 120 min + TAU |
TAU Routine psychiatric outpatient services; advice on medication and community services; brief education sessions |
| Chien & Thompson (2014) | 107 outpatient patients with schizophrenia Diagnosis of schizophrenia according to DSM-IV Mean age: 25.6±7.7 y |
TAU |
MBPP 12 × 120 minutes over 24 wk |
CPEP + TAU: 12 × 120 min over 24 wk TAU: Routine psychiatric outpatient services; advice on medication and community services; brief education sessions |
| Gaudiano & Herbert (2006) | 40 hospitalized patients with current or recent psychotic symptoms Diagnoses: - Psychotic disorder according to DSM-IV - Affective disorder with psychotic symptoms Mean age: 40.0±10.0 y |
TAU |
ACT 4 × 60 minutes + Enhanced TAU |
Enhanced TAU Psychopharmacology, case management, psychotherapy Group therapy and activities 2x daily Individual therapy as needed After discharge: community service referral Enhancement: daily support by the ACT therapist |
| Langer et al (2012) | 23 psychotic outpatients Diagnoses: schizophrenia, schizoaffective disorder, delusional disorder All according to DSM-IV Mean age: 34.7±8.2 y, 33.9±10.7 y WLC |
Antipsychotic medication |
MBCT Bodyscan, Breathing meditation, sitting meditation Weeks 1-8: once weekly 60 min + home practise |
Waiting list control No specific therapy |
| Shawyer et al (2012) | 44 psychotic patients with command hallucinations Diagnosis of schizophrenia or related condition according to DSM-IV Mean age: 39.0±10.0 y |
Antipsychotic medication |
TORCH Acceptance-Based Cognitive Therapy 3 engagement and assessment sessions Weeks 1-12: once weekly + home exercise |
Befriending A series of conversations with a friendly social acquaintance Avoidance of symptom and problem discussions Weeks 1-12: once weekly Waiting list control No specific therapy |
| White et al (2011) | 27 psychotic outpatients Psychotic disorder according to ICD-10 Age: −33.6±8.6 y ACT −34.6±11.0 y TAU |
TAU |
ACT 10 individual sessions × 60 minutes + TAU |
TAU Psychopharmacology, case management, psychotherapy |
| Longest follow-up | Outcome measures | Results | |
|---|---|---|---|
| 1) Psychotic symptoms 2) Hospitalization rate 3) Affect 4) Acceptance 5) Mindfulness 6) Safety |
Short-term | Long-term | |
| 4 mo 12 mo | 1) Number of patients experiencing symptoms; frequency of symptoms (Likert scale) 2) Hospitalization rate |
1) Significantly more patients in the ACT reported symptoms; no significant group differences in frequency 2) Significantly lower hospitalization rate in the ACT group |
2) Significant increase in hazard rate in TAU compared to ACT |
| 10 wk | 1) Severity and intensity of auditory hallucinations and delusions (PSYRATS) 5) Mindfulness (SMQ), mindful responses to voices (SMQ, SMVQ) |
1) No significant group difference 5) No significant group differences |
|
| 18 mo | 1) Psychotic symptom severity (BPRS) 2) Rehospitalization (number and duration) |
1) Significantly higher symptom severity in the TAU group 2) Significantly higher number and longer duration of rehospitalization in the TAU group |
1) Significantly higher symptom severity in the TAU group 2) Significantly higher number and longer duration of rehospitalization in the TAU group |
| 24 mo | 1) Psychotic symptom severity (BPRS) 2) Rehospitalization (number and duration) |
1) Significantly higher symptom severity in the TAU group 2) Significantly longer duration of rehospitalization in the TAU group |
1) Significantly higher symptom severity in the TAU group 2) Significantly longer duration of rehospitalization in the TAU group |
| 4 mo | 1) Psychotic symptoms (BPRS, CGI), frequency of symptoms (Likert scale) 2) Hospitalization rate (Odds Ratio) 3) Affect (BPRS); Distress (Likert scale) 6) Adverse events |
1) No significant group differences 2) No significant group differences 3) Affect: Significant group difference favoring ACT Distress: Significant group difference favoring ACT 6) No adverse events |
|
| 8 wk | 1) Psychotic symptoms (CGI) 4) Acceptance (AAQ II) 5) Mindfulness (SMQ) |
1) No significant group difference 4) No significant group difference 5) Significant group difference favoring MBCT |
|
| 3 mo 6 mo | 1) Psychotic symptoms (PANSS) 4) Acceptance of auditory and command hallucinations (VAAS) |
1) Positive symptoms: significant reduction within TORCH; Negative symptoms: significant increase within waiting list 4) Acceptance: no significant group difference |
1) Positive symptoms: no significant group difference; Negative symptoms: significant reduction within TORCH PANSS total: significant reduction within TORCH 4) Acceptance of auditory hallucinations: significant increase within TORCH; Acceptance of command hallucinations: significant increase within BEF |
| 3 mo | 1) Psychotic symptoms (PANSS) 3) Anxiety and Depression (HADS) 4) Acceptance (AAQ-II) 5) Mindfulness (KIMS) 6) Adverse events |
1) Positive symptoms: no significant group difference; Negative symptoms: significant larger decrease in ACT than TAU 3) No significant group difference 4) No significant group difference 5) Significantly larger increase in ACT than TAU 6) No serious adverse events |
|
Abbreviations: AAQ-II, Acceptance & Action Questionnaire; ACT, Acceptance and Commitment Therapy; BPRS, The Brief Psychiatric Rating Scale; 0CGI, The Clinical Global Impression, CPEP, Conventional Psychoeducation Program; DSM-IV, Diagnostic Statistical Manual; HADS, Hospital Anxiety and Depression Scale; ICD-10, International Classification of Diseases; KIMS, Kentucky Inventory of Mindfulness Skills; MBCT, Mindfulness Based Cognitive Therapy; MBPP, Mindfulness-Based Psychoeducation Program; NOS, not otherwise specified; PANSS, Positive and Negative Syndrome Scale; PSYRATS, The Psychotic Symptom Rating Scales; SMQ, Southampton Mindfulness Questionnaire; SMVQ, Southampton Mindfulness Voices Questionnaire; TAU, treatment as usual; TORCH, Treatment of Resistant Command Hallucinations; VAAS, The Voices Acceptance and Action Scale..
Setting and Participant Characteristics
Of the 8 RCTs that were included, 2 originated from North America,37,40 3 from Europe,39,41,43 2 from Asia,44,45 and 1 from Australia.42 Patients were recruited from psychiatric hospitals,37,40 outpatient clinics,44,45 mental health services,42,43 or patient associations.41 One RCT did not state the setting from which patients were recruited.39
Patients in 5 RCTs were diagnosed with psychosis or affective disorder with psychotic symptoms according to DSM-IV39–42,44,45 or ICD-10,43 while patients in 1 RCT had a hospital-supplied diagnosis where the diagnostic method was not specified.37 Between 48.1% and 100% of included patients were diagnosed with schizophrenia. Mean time since diagnosis ranged from 2.6 years to 17.7 years. Patients' mean age ranged from 25.6 years to 41.6 years; between 22.2% and 45.0% (median: 36.3%) of patients in each study were female.
Intervention Characteristics
Four RCTs used mainly acceptance-based interventions.37,40,42,43 Three of those used modifications of the ACT treatment manual14 that was modified for patients with psychosis. ACT was offered as 4 individual treatment sessions of 45 to 50 minutes each,37 10 individual sessions of 60 minutes each,43 or as a varying number of individual sessions depending on the individual length of hospital stay.40 All ACT interventions included standard acceptance and mindfulness exercises as outlined in the Hayes et al (1999) protocol14; 1 RCT also included a mindfulness breathing exercise.43 The fourth RCT used “treatment of resistant command hallucinations” (TORCH), an acceptance-based cognitive behavioral therapy intervention for command hallucinations.42 Fifteen individual weekly sessions of 50 minutes each and 2 follow-up sessions consisting of belief modification and acceptance-based interventions that were based on ACT were offered. Additional ACT exercises and mindfulness-based exercises were used. Audiotaped mindfulness-based exercises aimed to cultivate a nonjudgmental response towards positive psychotic symptoms while ACT exercises and metaphors aimed to implement a detached acceptance of psychotic symptoms. Given that TORCH is a relatively novel intervention, it cannot be regarded as widely accepted.
Four RCTs used mainly mindfulness-based interventions,39,41 1 of those being explicitly based on MBCT.41 Two interventions used mindfulness meditation and awareness exercises such as body scan and mindful breathing during 1039 or 841 weekly group sessions of 60 minutes each. Cognitive and metacognitive elements were incorporated, and mindfulness exercises were adapted for patients with psychosis. The remaining 2 RCTs used 12 biweekly sessions (120 minutes each) of a not widely accepted mindfulness-based psychoeducation program that combined MBSR with psychoeducation.44,45
In 7 RCTs, the intervention was combined with treatment as usual and compared with treatment as usual alone as the control intervention. Treatment as usual consisted of individual psychopharmacology, case management, and psychotherapy in 5 RCTs37,40,43–45; patients in 2 RCTs were wait-listed and treatment was not specified.39,41 One RCT used befriending as a control intervention, a fully manualized attention control intervention without therapeutic component that was matched with the experimental intervention for contact time and attention.42
Only 2 RCTs reported on the use of antipsychotic medication during the trial period and reported that compliance to medication was comparable between groups.37,45
Outcome Measures
Severity of symptoms of psychosis was assessed by 7 RCTs using the Brief Psychiatric Rating Scale,40,44,45 the Positive and Negative Syndrome Scale,42,43 the Clinical Global Impression Scale,40,41 or the Psychiatric Symptom Rating Scale.39 Hospitalization was assessed by 4 RCTs as number of hospitalized patients in a predefined follow-up period37,40 or as mean duration of rehospitalization per patient.44,45 Affect was measured by 2 RCTs using the Hospital Anxiety and Depression Scale43 or the Brief Psychiatric Rating Scale.40 Acceptance was assessed by the Acceptance and Action Questionnaire II in 3 RCTs41–43 and by the Voices Acceptance and Action Scale in 1 RCT.42 Mindfulness was measured by the Kentucky Inventory of Mindfulness Skills43 or the Southampton Mindfulness Questionnaire39,41 in 3 RCTs. Safety was assessed as number of adverse events in 2 RCTs.40,43
While all RCTs reported short-term effects, only 4 RCTs reported long-term effects.38,42,44,45
Risk of Bias in Individual Studies
Six RCTs had low risk of bias,37,40,42–45 and 2 RCTs had high risk of bias39,41 (Table 2). Risk of selection bias was mixed; only 3 RCTs each reported adequate randomization or adequate allocation concealment. While no RCT reported blinding of participants or providers, all but 2 RCTs39,40 reported adequate blinding of outcome assessors. All but 1 RCT41 adequately described cointerventions, and 5 RCTs reported acceptable intervention compliance. Attrition bias was mixed as all studies had an acceptable and described dropout rate but only 3 RCTs used an intention-to-treat analysis. Risk of reporting bias and detection bias was low in all RCTs.
Table 2.
Risk of Bias of the Included Studies
| Bias | Selection bias |
Performance bias |
Attrition bias |
Reporting bias |
Detection bias |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author, year | Adequate random sequence generation | Adequate allocation concealment | Similar baseline characteristics | Adequate participant blinding | Adequate provider blinding | Similar or no co-interventions | Acceptable compliance | Acceptable and described dropout rate | Inclusion of an intention-to-treat analysis | No selective outcome reporting | Adequate outcome assessor blinding | Similar timing of outcome assessment | Total: (max. 12)a |
| Bach & Hayes (2002) | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Unclear | Yes | No | Yes | Yes | Yes | 6 |
| Chadwick et al (2009) | No | Unclear | Unclear | Unclear | Unclear | Yes | Unclear | Yes | No | Yes | No | Yes | 4 |
| Chien & Lee (2013) | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8 |
| Chien & Thompson (2014) | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8 |
| Gaudiano & Herbert (2006) | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | No | Yes | 8 |
| Langer et al (2012) | Unclear | Unclear | Yes | Unclear | Unclear | Unclear | Unclear | No | No | Yes | Yes | Yes | 4 |
| Shawyer et al (2012) | No | Yes | No | Unclear | Unclear | Yes | Yes | Yes | No | Yes | Yes | Yes | 7 |
| White et al (2011) | Yes | Yes | Yes | No | No | Yes | Yes | No | No | Yes | Yes | Yes | 8 |
Higher scores indicate lower risk of bias.
Outcomes
Mindfulness- and Acceptance-based Interventions vs Treatment as Usual
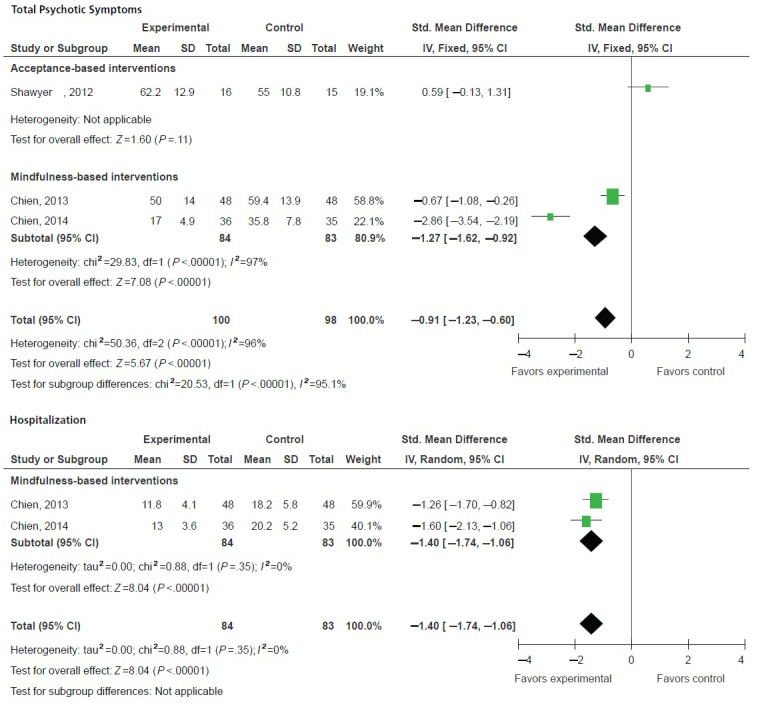
Meta-analyses revealed moderate evidence for short-term effects on total psychotic symptoms and positive symptoms. Heterogeneity was low to moderate and—based on Cohen's categories—effects were of small to moderate size (Figure 2). No evidence was found for short-term effects on negative symptoms (Figure 2). Moderate evidence was found for lower hospitalization rates and for shorter duration of hospitalization in the intervention groups compared to treatment as usual (Figure 2). Regarding secondary outcomes, no evidence was found for short-term effects on affect and acceptance (Figure 3). There was moderate evidence for short-term effects on mindfulness. Heterogeneity was low and effect size was large (Figure 3).
Figure 2.
Short-term effects of mindfulness- and acceptance-based interventions compared to treatment as usual on primary outcomes: total symptoms, positive symptoms, negative symptoms, and hospitalization.
Abbreviations: CI, confidence interval; df, degrees of freedom; IV, inverse variance; SD, standard deviation.
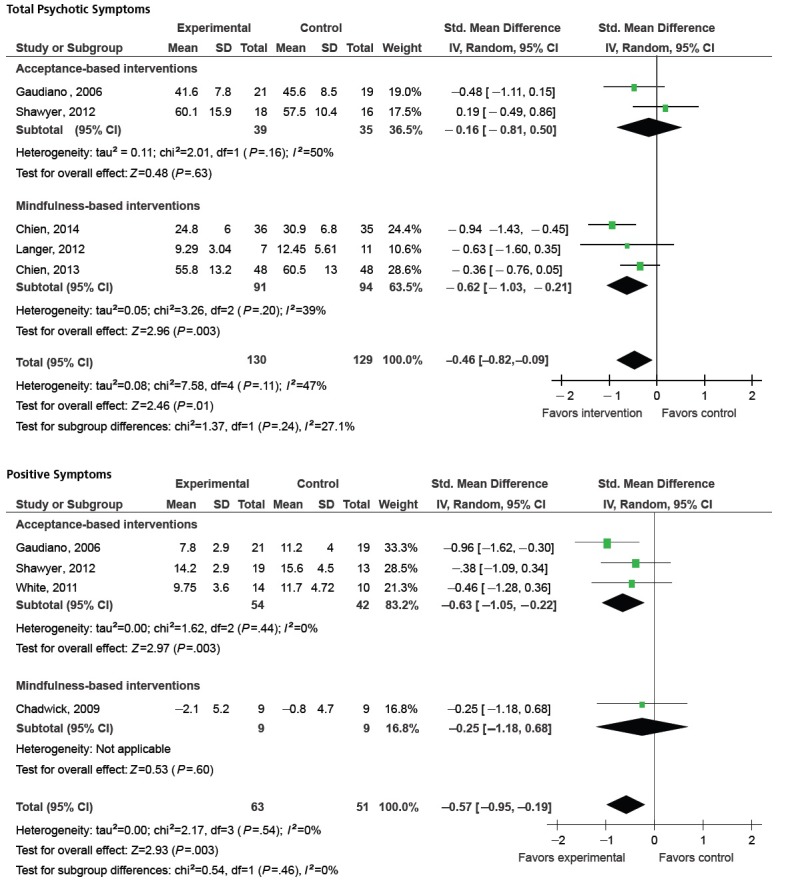
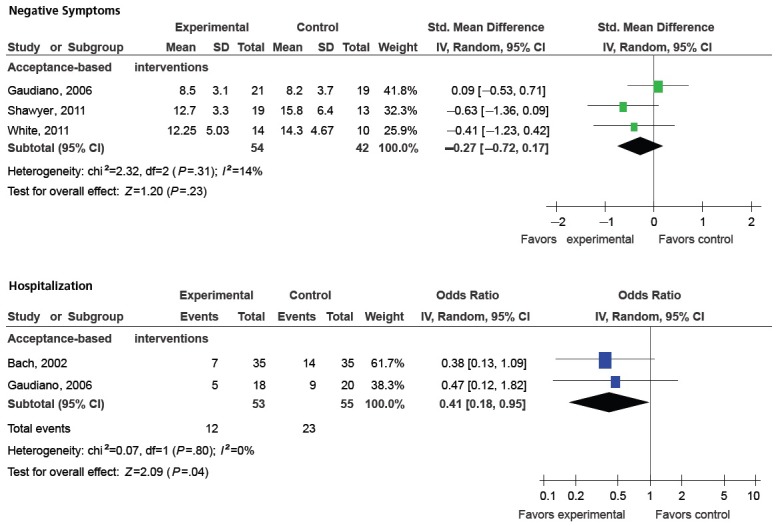
Figure 3.
Effects of mindfulness- and acceptance-based interventions compared to treatment as usual on secondary outcomes: affect, acceptance, and mindfulness.
Abbreviations: CI, confidence interval; df, degrees of freedom; IV, inverse variance; SD, standard deviation.
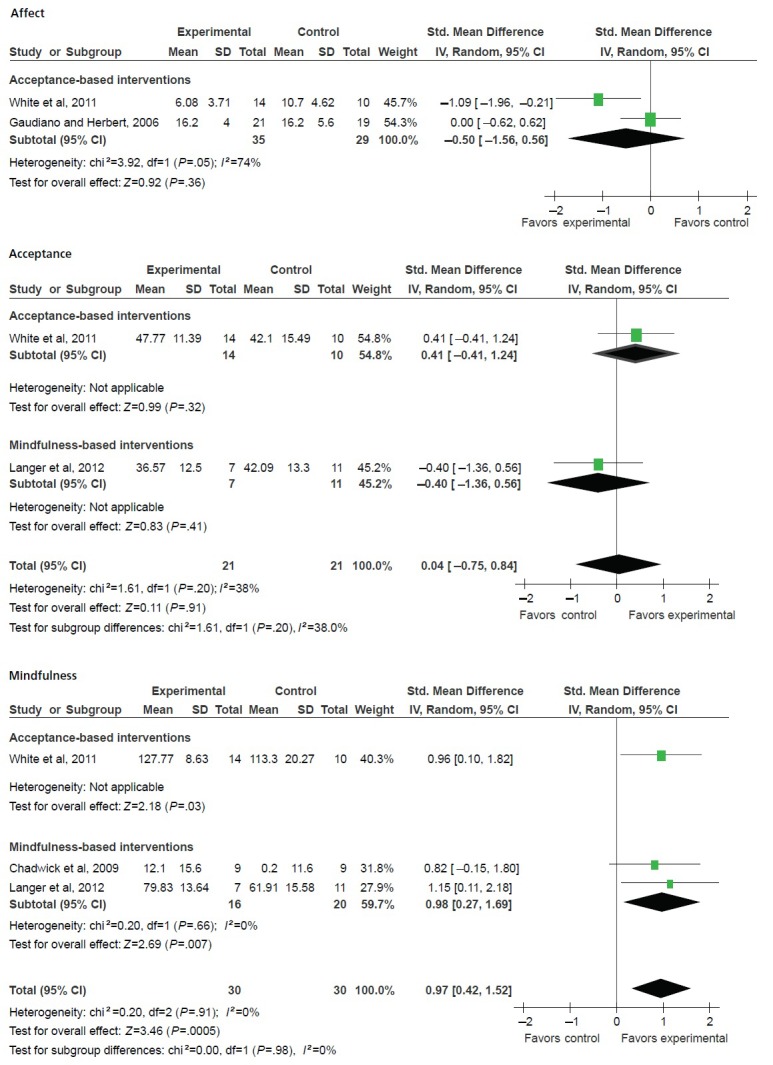
Moderate evidence for long-term effects (12 to 24 months after the intervention) on total psychotic symptoms and for shorter duration of hospitalization in the long term was found in 2 RCTs (Figure 4). Further, hospitalization rate at 12 months was assessed in 1 RCT.38 This RCT reported reduced hospitalization rates in the intervention group compared to the treatment as usual-group (Table 1).
Figure 4.
Long-term effects of mindfulness- and acceptance-based interventions compared to treatment as usual on primary outcomes: total symptoms and hospitalization.
Abbreviations: CI, confidence interval; df, degrees of freedom; IV, inverse variance; SD, standard deviation.
Mindfulness- and Acceptance-based Interventions vs Attention Control
One RCT compared an acceptance-based intervention to attention control and found no evidence for short-term or long-term (6 months after the intervention) group differences for total symptoms, positive symptoms, negative symptoms, or acceptance42 (Table 1).
Safety
Safety data were reported in 2 RCTs. One RCT reported that no adverse events were observed40 and the other RCT reported that no “suspected unexpected serious adverse events” were observed.43 Two further RCTs reported patients that dropped out of the study due to health reasons: 1 patient in the treatment arm of 1 RCT died in a car accident,37,38 and 1 patient in another RCT had a heroin addiction relapse.39
Subgroup Analyses
In studies on primarily mindfulness-based interventions, moderate evidence was found for short-term effects on total psychotic symptoms. No such effects were found in studies on primarily acceptance-based interventions (Figure 2). Patterns were reversed for positive symptoms. Subgroups were however homogeneous, and no significant subgroup differences were found. Moderate evidence for short-term effects on mindfulness was revealed in studies on acceptance-based interventions and limited evidence in studies on mindfulness-based interventions; subgroups were homogeneous and not significantly different (Figure 3). Long-term effects on total symptoms were revealed for mindfulness-based but not for acceptance-based interventions; subgroups were significantly different (Figure 4).
In subgroup analyses regarding diagnostic method, no evidence was found for short-term effects on hospitalization rate for studies with either manual-based diagnosis40 (SMD=0.47; 95% CI=0.12-1.82; P=.28) or unclear diagnostic method3737 (SMD=0.38; 95% CI=0.13-1.09; P=.07).
Sensitivity Analyses
Sensitivity analyses demonstrated a significant effect on total psychotic symptoms and positive symptoms in studies with low risk of bias comparing mindfulness- and acceptance-based interventions to treatment as usual, whereas no such effect was found in studies with high risk of bias. No effects were found for acceptance in studies with either low or high risk of bias while effects on mindfulness were found in both low-risk and high-risk studies. All other comparisons included only studies with low risk of bias.
DISCUSSION
Summary of Evidence
This systematic review found moderate evidence for short- and long-term improvements of psychotic symptoms and hospitalization in patients with psychotic disorders after mindfulness- and acceptance-based interventions compared to treatment as usual. There were no significant subgroup differences between the studies on primarily acceptance-based interventions such as ACT or studies on primarily mindfulness-based interventions.
Agreement With Previous Systematic Reviews
The findings of this meta-analysis are partly in line with those of a previous one that found between-group effects on negative symptoms and rehospitalization but not on positive symptoms for mindfulness- and acceptance-based interventions in patients with psychosis.46 While this previous meta-analysis included all available uncontrolled and controlled studies, further RCTs that were not included are now available. Differences between the 2 meta-analyses likely stem from differences in inclusion criteria and methods of analysis. A further systematic review on mindfulness-based interventions for severe mental disorders concluded that these interventions might reduce symptom-associated distress and hospitalization for individuals with psychotic disorders.47 The main difference between the previous reviews and the present one is the inclusion of additional RCTs, presenting the most up-to-date review on the effectiveness of mindfulness- and acceptance-based interventions for psychosis in RCTs. Moreover, the previous reviews did not included a meta-analysis47 or did not separately meta-analyze effects of mindfulness- and acceptance-based interventions on different outcomes compared to different control interventions.46
Moreover, the results of the present review are partly comparable to those of cognitive behavior therapy (CBT), which shares many intervention components with both ACT and MBCT, for schizophrenia. These reviews reported effects on mental state but not on hospitalization when comparing CBT to treatment as usual48 and effects on psychotic symptoms when comparing CBT to other psychological interventions.49 However, a recent Cochrane review failed to show differences between CBT and other psychological interventions on symptoms or hospitalization in patients with schizophrenia.50 Another systematic review that included only high-quality RCTs on CBT for early psychosis concluded that CBT can improve psychotic symptoms but did not influence relapse or rehospitalization.51
A recent meta-analysis on yoga—which shares many similarities with mindfulness meditation and has been shown to improve cognitive function52,53—for schizophrenia found no evidence for effects on psychotic symptoms or hospitalization.54
External and Internal Validity
Patients in the included studies were recruited from psychiatric hospitals, outpatient clinics, mental health services, and patient associations in North America, Europe, and Australia. All but 1 study37 used clear and well-accepted diagnostic criteria, and patients with different psychotic disorders were included. The majority of patients were males and in the reproductive-age range. The results of this review are therefore applicable to the vast majority of patients with psychotic disorders in clinical practice.
Two out of 8 studies had high risk of bias.39,41 No evidence of effectiveness on primary outcomes was found in studies with high risk of bias while evidence for effects on total symptoms, positive symptoms, and hospitalization was found in studies with low risk of bias. Therefore, this evidence can be regarded as robust against potential methodological bias.
Strengths and Weaknesses
A major strength of this review is that, besides psychopathology, patient-centered outcomes were used.55 Most of the included studies had low risk of bias and the evidence of effectiveness was robust against potential bias. While patients were recruited from different facilities and it could be argued that this would influence severity of symptoms, all significant meta-analyses were free of statistical heterogeneity, suggesting comparability between studies.
The primary limitation of this review is the small total number of eligible RCTs. As no unpublished studies were included in this review and publication bias could not be assessed, it cannot be ruled out that further unpublished RCTs exist that could add further and possibly conflicting evidence. While the included studies suggest superiority of mindfulness- and acceptance-based interventions to treatment as usual, no studies were available that included a head-to-head comparison to other active interventions. While subgroup analyses were conducted to separately analyze the effectiveness of primarily acceptance-based and primarily mindfulness-based interventions, the small number of RCTs in each subgroup limits their expressiveness. Only 2 RCTs reported data on compliance to antipsychotic medication, the possible influence of differences in compliance on trial outcomes thus could not be assessed. One might further question the comparability of primarily mindfulness-based and primarily acceptance-based interventions. As outlined above, while these approaches share many similarities, the practical techniques used in each intervention might strongly differ. Moreover, the different approaches have different therapeutic foci: eg, MBCT has been designed as an intervention for relapse prevention in major depression16 and has been shown to effectively ameliorate recurrent depression.56 On the other hand, ACT has a more broad focus and has been evaluated in a number of psychiatric conditions.57 However, there is no condition yet for which effectiveness of ACT is conclusively established.58 Therefore, the interpretations of overall effects might be less valid than those of the subgroup analyses.
The included studies used varying interventions with and without concomitant medication and varying control group conditions. These factors might weaken the conclusions of this meta-analysis.
Implications for Further Research
While psychopharmacological treatment is the most important intervention for psychosis, its effectiveness on negative symptoms is limited6 and a considerable number of patients are therapy refractory.7 Thus, patients may require adjunctive psychotherapeutic interventions to help them cope with symptoms that are not effectively treated with anti-psychotic medication. Given the low number of available studies, definite conclusions about the effectiveness of mindfulness- and acceptance-based interventions for that end are impossible. However, in light of the preliminary evidence found in this review, further research seems warranted. Future studies should ensure rigorous methodology and reporting, mainly adequate randomization, allocation concealment, and intention-to treat analysis.59 While blinding of participants or providers might not be possible in interventions that involve complex interactions between patients and providers and should thus not be regarded as a lack of quality of the study (while it is still a possible source of bias), adequate blinding of outcome assessors should be intended all the more in future studies. Besides comparisons with treatment as usual or attention control, head-to-head studies are needed to compare the effects of mindfulness- and acceptance-based interventions with those of more traditional approaches—eg, cognitive-behavioral interventions.
Implications for Clinical Practice
While the expressiveness of the findings of this meta-analysis is somewhat limited by the small number of included RCTs, the clearly positive findings are encouraging. No intervention-related serious adverse events were reported. While single cases of psychotic relapse after unsupervised meditation practice and even meditation-induced psychosis have been reported,60 there seems to be little risk of relapse and aggravation of psychotic symptoms in supervised mindfulness- and acceptance-based interventions. Thus both mindfulness- and acceptance-based interventions can be recommended as additional treatments for patients with psychosis but should be closely supervised by adequately trained therapists.
Conclusions
This systematic review and meta-analysis found moderate evidence for short- and long-term effects of mindfulness- and acceptance-based interventions on psychotic symptoms, hospitalization, and mindfulness in patients with psychotic disorders. Both types of interventions can be recommended as an additional treatment for patients with psychosis.
Acknowledgments
This review was supported by a grant from the Rut- and Klaus-Bahlsen-Foundation. The funding source had no influence on the design or conduct of the review; the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
Disclosures The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and had no conflicts to disclose.
Contributor Information
Holger Cramer, Department of Internal and Integrative Medicine, Kliniken Essen-Mitte, Faculty of Medicine, University of Duisburg-Essen, Essen, Germany; Australian Research Centre in Complementary and Integrative Medicine, Faculty of Health, University of Technology Sydney (Dr Cramer), Australia.
Romy Lauche, Department of Internal and Integrative Medicine, Kliniken Essen-Mitte, Faculty of Medicine, University of Duisburg-Essen, Essen, Germany; Australian Research Centre in Complementary and Integrative Medicine, Faculty of Health, University of Technology Sydney (Dr Lauche), Australia.
Heidemarie Haller, Department of Internal and Integrative Medicine, Kliniken Essen-Mitte, Faculty of Medicine, University of Duisburg-Essen, Essen (Haller), Germany.
Jost Langhorst, Department of Internal and Integrative Medicine, Kliniken Essen-Mitte, Faculty of Medicine, University of Duisburg-Essen, Essen (Langhorst), Germany.
Gustav Dobos, Department of Internal and Integrative Medicine, Kliniken Essen-Mitte, Faculty of Medicine, University of Duisburg-Essen, Essen (Dobos), Germany.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th edition Revised Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.van Os J, Kapur S. Schizophrenia. Lancet. 2009;374(9690):635–45. [DOI] [PubMed] [Google Scholar]
- 3.Boyer L, Caqueo-Urizar A, Richieri R, Lancon C, Gutiérrez-Maldonado J, Auquier P. Quality of life among caregivers of patients with schizophrenia: a cross-cultural comparison of Chilean and French families. BMC Fam Pract. 2012. July 6;13:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCabe R, Saidi M, Priebe S. Patient-reported outcomes in schizophrenia. Br J Psychiatry Suppl. 2007. 50:s21–8. [DOI] [PubMed] [Google Scholar]
- 5.Pitkänen A, Hätönen H, Kuosmanen L, Välimäki M. Individual quality of life of people with severe mental disorders. J PsychiatrMent Health Nurs. 2009;16(1):3–9. [DOI] [PubMed] [Google Scholar]
- 6.Stahl SM, Buckley PF. Negative symptoms of schizophrenia: a problem that will not go away. Acta Psychiatr Scand. 2007;115(1):4–11. [DOI] [PubMed] [Google Scholar]
- 7.Sheitman BB, Lieberman JA. The natural history and pathophysiology of treatment resistant schizophrenia. J Psychiatr Res. 1998;32(3-4):143–50. [DOI] [PubMed] [Google Scholar]
- 8.Cramer H, Haller H, Lauche R, Dobos G. Mindfulness-based stress reduction for low back pain. A systematic review. BMC Complement Altern Med. 2012. September 25;12:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cramer H, Lauche R, Paul A, Dobos G. Mindfulness-based stress reduction for breast cancer-a systematic review and meta-analysis. Curr Oncol. 2012;19(5):e343–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fjorback LO, Arendt M, Ornbøl E, Fink P, Walach H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: a systematic review of randomized controlled trials. Acta Psychiatr Scand. 2011;124(2):102–19. [DOI] [PubMed] [Google Scholar]
- 11.Veehof MM, Oskam MJ, Schreurs KM, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: a systematic review and meta-analysis. Pain. 2011;152(3):533–42. [DOI] [PubMed] [Google Scholar]
- 12.Ost LG. Efficacy of the third wave of behavioral therapies: a systematic review and meta-analysis. Behav Res Ther. 2008;46(3):296–321. [DOI] [PubMed] [Google Scholar]
- 13.Vollestad J, Nielsen MB, Nielsen GH. Mindfulness- and acceptance-based interventions for anxiety disorders: a systematic review and meta-analysis. Br J Clin Psychol. 2012;51(3):239–60. [DOI] [PubMed] [Google Scholar]
- 14.Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- 15.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. 2003;10(2):144–56. [Google Scholar]
- 16.Segal ZV, Williams JM, Teasdale JD. Mindfulness based cognitive therapy for depression. New York: Guilford Press; 2002. [Google Scholar]
- 17.Roemer L, Orsillo SM, Salters-Pedneault K. Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: evaluation in a randomized controlled trial. J Consult Clin Psychol. 2008;76(6):1083–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jacobsen P, Morris E, Johns L, Hodkinson K. Mindfulness groups for psychosis; key issues for implementation on an inpatient unit. Behav Cogn Psychother. 2011;39(3):349–53. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89(9):873–80. [PubMed] [Google Scholar]
- 20.Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions. West Sussex, UK: Cochrane Collaboration, John Wiley & Sons; 2008. [Google Scholar]
- 21.Spitzer RL, Endicott J, Robins L. Research diagnostic criteria for a selected group of functional disorders. 3rd ed. New York: New York State Psychiatric Institue; 1977. [Google Scholar]
- 22.World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993. [Google Scholar]
- 23.Overall JE, Gorham DL. The Brief Psychiatric Rating Scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
- 24.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76. [DOI] [PubMed] [Google Scholar]
- 25.Guy W. Clinical global impressions scale (CGI). In: Rush AJ, ed. Handbook of psychiatric measures. Washington, DC: American Psychiatric Association; 2000:100–2. [Google Scholar]
- 26.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961. June;4:561–71. [DOI] [PubMed] [Google Scholar]
- 27.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960. February;23:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–5. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–7. [DOI] [PubMed] [Google Scholar]
- 30.Bond FW, Hayes SC, Baer RA, et al. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther. 2011;42(4):676–88. [DOI] [PubMed] [Google Scholar]
- 31.Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: the Kentucky inventory of mindfulness skills. Assessment. 2004;11(3):191–206. [DOI] [PubMed] [Google Scholar]
- 32.Furlan AD, Pennick V, Bombardier C, van Tulder M; Editorial Board Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34(18):1929–41. [DOI] [PubMed] [Google Scholar]
- 33.Cohen JD. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 34.van Tulder M, Furlan A, Bombardier C, Bouter L; Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976). 2003;28(12):1290–9. [DOI] [PubMed] [Google Scholar]
- 35.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bach P, Hayes SC. The use of acceptance and commitment therapy to prevent the rehospitalization of psychotic patients: a randomized controlled trial. J Consult Clin Psychol. 2002;70(5):1129–39. [DOI] [PubMed] [Google Scholar]
- 38.Bach P, Hayes SC, Gallop R. Long-term effects of brief acceptance and commitment therapy for psychosis. Behav Modif. 2012;36(2):165–81. [DOI] [PubMed] [Google Scholar]
- 39.Chadwick P, Hughes S, Russell D, Russell I, Dagnan D. Mindfulness groups for distressing voices and paranoia: a replication and randomized feasibility trial. Behav Cogn Psychother. 2009;37(4):403–12. [DOI] [PubMed] [Google Scholar]
- 40.Gaudiano BA, Herbert JD. Acute treatment of inpatients with psychotic symptoms using Acceptance and Commitment Therapy: pilot results. Behav Res Ther. 2006;44(3):415–37. [DOI] [PubMed] [Google Scholar]
- 41.Langer AI, Cangas AJ, Salcedo E, Fuentes B. Applying mindfulness therapy in a group of psychotic individuals: a controlled study. Behav Cogn Psychother. 2012;40(1):105–9. [DOI] [PubMed] [Google Scholar]
- 42.Shawyer F, Farhall J, Mackinnon A, et al. A randomised controlled trial of acceptance-based cognitive behavioural therapy for command hallucinations in psychotic disorders. Behav Res Ther. 2012;50(2):110–21. [DOI] [PubMed] [Google Scholar]
- 43.White R, Gumley A, McTaggart J, et al. A feasibility study of Acceptance and Commitment Therapy for emotional dysfunction following psychosis. Behav Res Ther. 2011;49(12):901–7. [DOI] [PubMed] [Google Scholar]
- 44.Chien WT, Lee IY. The mindfulness-based psychoeducation program for Chinese patients with schizophrenia. Psychiatr Serv. 2013;64(4):376–9. [DOI] [PubMed] [Google Scholar]
- 45.Chien WT, Thompson DR. Effects of a mindfulness-based psychoeducation programme for Chinese patients with schizophrenia: 2-year follow-up. Br J Psychiatry. 2014;205(1):52–9. [DOI] [PubMed] [Google Scholar]
- 46.Khoury B, Lecomte T, Gaudiano BA, Paquin K. Mindfulness interventions for psychosis: a meta-analysis. Schizophr Res. 2013;150(1):176–84. [DOI] [PubMed] [Google Scholar]
- 47.Davis L, Kurzban S. Mindfulness-based treatment for people with severe mental illness: a literature review. Am J Psychiatr Rehabil. 2012;15(2):202–32. [Google Scholar]
- 48.Jones C, Cormac I, Silveira da Mota Neto JI, Campbell C. Cognitive behaviour therapy for schizophrenia. Cochrane Database Syst Rev. 2004. October 18;(4):CD000524. [DOI] [PubMed] [Google Scholar]
- 49.Sarin F, Wallin L, Widerlöv B. Cognitive behavior therapy for schizophrenia: a meta-analytical review of randomized controlled trials. Nord J Psychiatry. 2011;65(3):162–74. [DOI] [PubMed] [Google Scholar]
- 50.Jones C, Hacker D, Cormac I, Meaden A, Irving CB. Cognitive behaviour therapy versus other psychosocial treatments for schizophrenia. Cochrane Database Syst Rev. 2012. April 18;4:CD008712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bird V, Premkumar P, Kendall T, Whittington C, Mitchell J, Kuipers E. Early intervention services, cognitive-behavioural therapy and family intervention in early psychosis: systematic review. Br J Psychiatry. 2010;197(5):350–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Behere RV, Arasappa R, Jagannathan A, et al. Effect of yoga therapy on facial emotion recognition deficits, symptoms and functioning in patients with schizophrenia. Acta Psychiatr Scand. 2011;123(2):147–53. [DOI] [PubMed] [Google Scholar]
- 53.Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia—a randomized controlled trial. Acta Psychiatr Scand. 2007;116(3):226–32. [DOI] [PubMed] [Google Scholar]
- 54.Cramer H, Lauche R, Klose P, Langhorst J, Dobos G. Yoga for schizophrenia: a systematic review and meta-analysis. BMC Psychiatry. 2013. January 18;13:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Burns T. Evolution of outcome measures in schizophrenia. Br J Psychiatry Suppl. 2007. August;50:s1–6. [DOI] [PubMed] [Google Scholar]
- 56.Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin Psychol Rev. 2011;31(6):1032–40. [DOI] [PubMed] [Google Scholar]
- 57.A-Tjak JG, Davis ML, Morina N, Powers MB, Smits JA, Emmelkamp PM. A meta-analysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychother Psychosom. 2015;84(1):30–6. [DOI] [PubMed] [Google Scholar]
- 58.Ost LG. Efficacy of the third wave of behavioral therapies: a systematic review and meta-analysis. Behav Res Ther. 2008;46(3):296–321. [DOI] [PubMed] [Google Scholar]
- 59.Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152(11):726–32. [DOI] [PubMed] [Google Scholar]
- 60.Kuijpers HJ, van der Heijden FM, Tuinier S, Verhoeven WM. Meditation-induced psychosis. Psychopathology. 2007;40(6):461–4. [DOI] [PubMed] [Google Scholar]


