
In the November 2015 issue of Global Advances in Health and Medicine, we published abstracts from the Annual Integrative Medicine for the Underserved (IM4US) conference held in Boston, Massachusetts, August 6-8, 2015.1 The mission of IM4US is “a collaborative, multidisciplinary group of people committed to affordable, accessible integrative health care for all.” The abstracts described a number of innovative projects, including integrating mindfulness into the patient-centered medical home in federally qualified community health centers; group visits for Spanish-speaking patients with chronic pain; complementary therapy educational institutions offering free services at community events; introducing integrative approaches into public schools; and use of web-based and smart phone technology. The mission of IM4US to make more equitable access to integrative healthcare is laudable. It begs the following question: Can integrative medicine and health have an impact on reducing health disparities?
A health disparity is defined as “a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; gender; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion.”2
Throughout the world, many substantial, well-documented health disparities exist. Obesity, diabetes, chronic pain, cardiovascular disease, HIV/AIDS, maternal-child outcomes, mental health, and cancer are a few of the major conditions with prominent sociodemographic disparities.2 Poverty is a risk factor for premature mortality and increased morbidity. Across all races and ethnicities, greater life expectancy is associated with higher income.3 In the United States, non-Hispanic blacks are 50% more likely to die from cardiovascular disease than non-Hispanic whites.4 Health-related quality of life in blacks with chronic medical conditions is associated with greater and longer impairment in activities of daily living than whites.5 Morbidity and mortality from heart disease and diabetes is greatest in individuals with lower education.6 Health literacy—the ability to comprehend information needed to make informed appropriate decisions about one's health7—is a strong predictor of health.8 Persons with low or limited health literacy utilize more treatment services than prevention services. Employed individuals have lower levels of asthma, diabetes, hypertension, obesity, persistent anxiety, sadness, and depression.5 Geographic disparities in health are common. Obesity and diabetes in the United States are least in the Northeast and West compared to the Southeast and Midwest.9 At the level of the neighborhood, Figure 1 illustrates the correlation between areas of lower education attainment in Boston, Massachusetts, with rates of hospitalization for chronic disease and poor birth outcomes.5 Similar associations can be seen for income and race.
Figure 1.
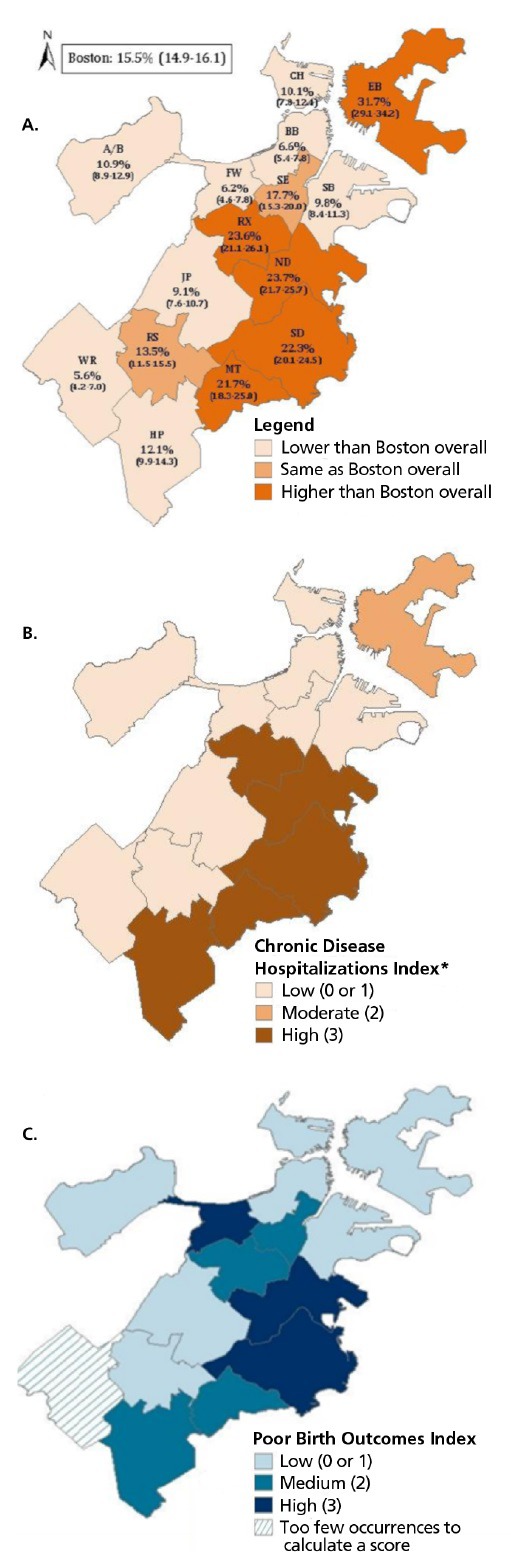
Correlation between educational attainment and health disparities in Boston, Massachusetts. (A) Percentage of population by neighborhood with less than a high-school education in Boston, 2008-2012. (B) Rates of hospitalization from chronic diseases by Boston neighborhoods, 2012. (C) Poor birth outcomes (eg, low birth weight, infant mortality, maternal death).
According to the Academic Consortium for Integrative Medicine and Health, integrative medicine and health “reaffirms the importance of the relationship between practitioner and patient, focuses on the whole person, is informed by evidence, and makes use of all appropriate therapeutic and lifestyle approaches, health-care professional and disciplines to achieve optimal health and healing.”10 An integrative medicine and health approach is thus relationship-centered and patient-centered and combines the best of mainstream and complementary/lifestyle approaches. Increasing research is suggesting the safety and effectiveness of a variety of integrative approaches. Nutritional and physical activity interventions for the prevention and treatment of cardiovascular disease,11 mindfulness techniques for mental health conditions such as anxiety,12 and mind-body approaches such as yoga for chronic low back pain are a few examples.13 However, relatively few integrative medicine clinical services and research studies have been done in non-white, lower income, less-educated populations.
Nationally representative data on integrative therapy use in the United States from the 2012 National Health and Interview Survey show overall 33.2% of US adults used at least one of these therapies during the previous year.14 However, disparities in use exist across a number of sociodemographic variables. Use among Hispanics (22%) and non-Hispanic blacks (19.3%) were both less than use among non-Hispanic whites (37.9%). Only 15.6% of adults who did not complete high school used integrative therapies compared to 42.6% with college degrees. Among poor individuals (household income <100% of the US Census Bureau poverty threshold), use was 20.6% compared to 38.4% of non-poor adults (income >200% of the poverty threshold). Compared to 2002 data, there was a statistically significant trend toward less overall use of integrative therapies among minorities, less-educated, and poor individuals. If we look specifically at yoga as an example, overall use has almost doubled from 2002 to 2012 (5.1% to 9.5%). Although yoga use among Hispanics and non-Hispanic blacks has increased, significant disparities still exist. In 2012, 11.2% of non-Hispanic Americans used yoga compared to 5.1% of Hispanics and 5.5% of non-Hispanic blacks.
There are 4 categories of barriers to integrative medicine use among the underserved.
Awareness. A secondary analysis of 2007 National Health Interview Survey data examined the reasons why US adults chose not to use chiropractic, acupuncture, natural products, and yoga. Individuals with less than high school–level education were more likely to cite lack of knowledge as an important factor for not using any of these therapies.15 For example, compared to those without a high school degree, individuals with college education were 46% less likely to cite lack of knowledge as a factor for not using chiropractic. Similarly, those with higher income levels were significantly less likely to select lack of knowledge as a reason for non-use of chiropractic, acupuncture, and yoga. Poor compared to non-poor individuals were 61% more likely to select lack of knowledge as a reason for not using acupuncture. We have also observed this lack of awareness in our yoga studies in Boston with predominantly low income minority adults with non-specific chronic low back pain. Despite the growing popularity of yoga nationally and emerging evidence for its use in pain, the majority of patients approached had little previous knowledge of this.16 Interviews with our participants supported this:
I didn't think that it [yoga] was for me. You see people do it on TV, and it looked complicated to get started…. I always wanted to do it, but it was just so foreign to me…. So I kind of just stayed away from yoga.
I never knew nothing about yoga. So I received a letter … asking me if I wanted to participate in this research study … I really wasn't expecting the relief of the pain. I would've done it 20 years ago if I had known.
Availability. Geographic variation in the availability of healthy foods such as fresh fruits and vegetables is well established.17 Often referred to as food deserts, low-income neighborhoods frequently have a lower density of supermarkets than high-income areas. Although regional variations in integrative medicine use in the United States have been described, little is known regarding the availability of integrative approaches at the neighborhood level. Using geo-mapping software, we superimposed the distribution of yoga studios on a map of Boston showing income levels by zip code (Figure 2A). With few exceptions, yoga studios were predominantly located in neighborhoods where mean resident income was greater than the city average and absent in areas where income was lower than the median. A similar pattern was found for acupuncturists and massage therapists (Figures 2B–C).
Figure 2.
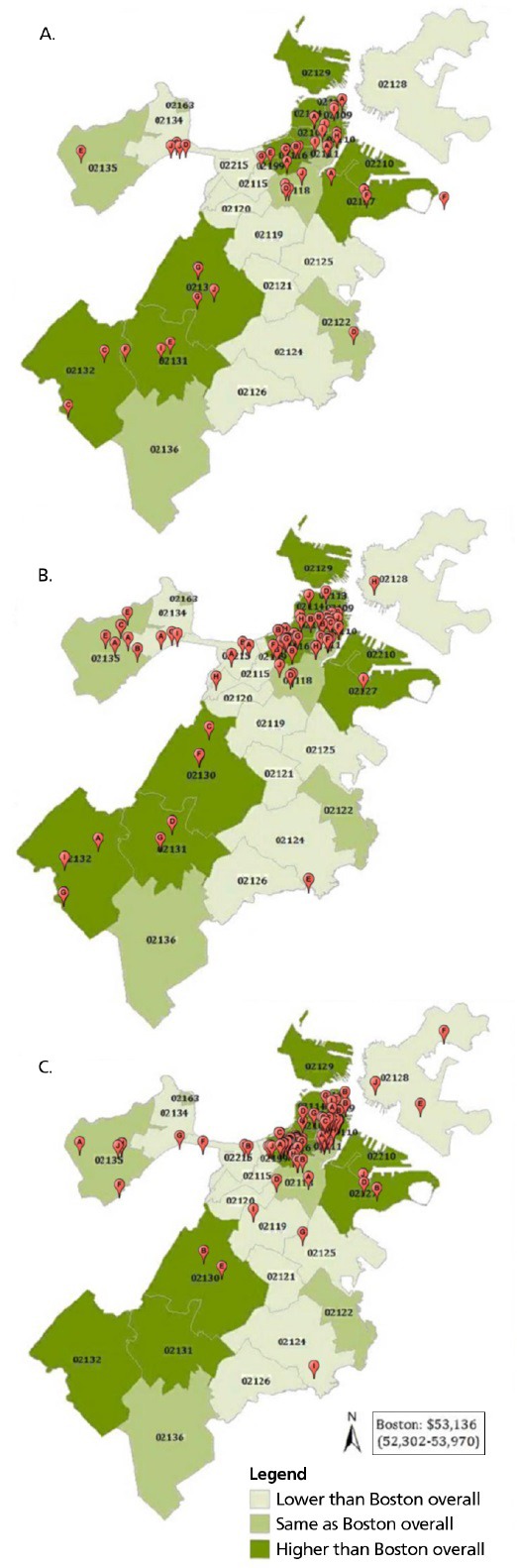
Availability of yoga studios, acupuncturists, and massage therapists in Boston, MA according to neighborhood and income level relative to the median household income of Boston overall. (A) Yoga studios. (B) Acupuncturists. (C) Massage therapists.
Accessibility. Even if individuals are aware of integrative therapies and they are available, there can be barriers that make it difficult to take advantage of them. Individuals working multiple part-time lower-skill jobs often have low job autonomy, little control over setting their work schedule in advance, and variable work hours. This can make it challenging to attend a regular mind-body class or keep an acupuncture appointment, particularly Monday through Friday during daytime hours. Transportation can be an obstacle. Not owning a car can make attendance difficult if the location is not accessible by public transportation. Parking can be expensive. Often public transportation is not as well developed in certain poor neighborhoods, necessitating changing buses or subways multiple times. For individuals not working outside the home, some have responsibilities caring for children or grandchildren. Without having someone else to watch the children or being able to bring them along, attendance becomes difficult. It may be difficult for a non-native English speaker to find a practitioner or class that he or she can understand. Our yoga for low back pain study participants16 spoke to several of these barriers:
But things make it easy for me not to go, because of my job, sometimes they just reschedule the night before. So I might say, “Oh, I'm not gonna go, because I don't want to lose my job.”
Sometimes I got a ride from a friend. If I didn't get a ride, I had to take four buses.
Affordability. In 2007, $33.9 billion “out of pocket” costs were spent by US adults on complementary integrative medicine visits, classes, and products.18,19 Of this amount, an estimated $14.9 billion was for the treatment of pain, with back pain being the leading condition for which out-of-pocket spending occurs ($8.7 billion). The annual amount spent per person out of pocket varied from $568 to $895, depending upon the pain condition. The reason for such high out-of-pocket costs is that common integrative therapies such as acupuncture, massage, and yoga are infrequently reimbursed by insurance. Chiropractic reimbursement is more common but still variable depending upon one's insurance plan. Although per-visit charges for these services vary, individual chiropractic, acupuncture, or massage visits may cost from $60 to $120. Yoga and other mind-body classes can vary from $12 to $20 per class. For low-income patients with little or no discretionary income, these fees are prohibitive. If someone is struggling to make ends meet on a limited or fixed income, more basic needs such as food, rent, heat, and clothing will take priority.
Investigating whether integrative medicine and health can truly reduce health disparities will take a substantial interprofessional research effort. Effectiveness studies should be prioritized over efficacy trials. An integrative approach should be targeted to underserved populations with conditions where disparities exist and there is either preliminary evidence or plausibility of effectiveness. Mind-body approaches for pain and lifestyle modification for cardiovascular disease and diabetes are 2 examples of promising areas. Given that social determinants of health are responsible for approximately 80% of health outcomes with clinical care making up the remainder,20 a systems-based approach is critical. Incorporating not only clinical services but also public health and policy reform is critical.
Addressing barriers to implementation and dissemination such as lack of awareness, availability, accessibility, and affordability will be essential. Through television, social media, school-based health education, and community-based events, public awareness about effective integrative approaches can be raised across all sociodemographic groups. Greater awareness among the public and health sectors will lead to greater demand for making integrative services more available in historically low-income, minority communities. Incorporating services into federally qualified community health centers is a particularly promising mechanism for increasing accessibility. Other community-based organizations such as churches, mosques, libraries, community centers, gyms, and veteran centers can similarly make programs and classes available. Innovative online tools, such as smartphone apps for stress reduction and monitoring physical activity, can help address lack of accessibility. Making integrative services affordable will require continuing lobbying efforts for insurance to reimburse for safe, effective integrative therapies, group visit models, and lifestyle modification programs. The current shift from fee-for-service to panel-based compensation provides an important opportunity for integrative medicine and health. It will create an alignment of incentives to make the promotion of health and wellbeing primary with the treatment of disease and its complications secondary. It will be necessary to use research and quality improvement initiatives to demonstrate whether an integrative approach can add value by improving population health through reducing disparities, contributing to high patient satisfaction, and lowering costs. If this is the case, there will be a strong moral and social justice imperative to make integrative medicine and health accessible to all.
REFERENCES
- 1.IM4US conference 2015 abstracts: poster and oral presentations. Global Adv Health Med. 2015;4(6):65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smedley BD, Stith AY, Nelson AR, ed. Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 3.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010;100(suppl 1):S186–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services. Coronary heart disease and stroke deaths—United States, 2009. Atlanta, GA: Centers for Disease Control and Prevention; 2013; MMWR Surveill Summ. 2013. November 22;62 Suppl 3:157–60. [PubMed] [Google Scholar]
- 5.Shah SN, Dodds HD, Dooley D, et al. Health of Boston 2014-2015. Boston Public Health Commission website. http://www.bphc.org/healthdata/health-of-boston-report/Documents/HOB-2014-2015/FullReport_HOB_2014-2015.pdf. Accessed December 17, 2015.
- 6.Cutler DM, Lleras-Muney A. Policy Brief #9: Education and health. University of Michigan, National Poverty Center website. http://www.npc.umich.edu/publications/policy_briefs/brief9/. Accessed December 17, 2015.
- 7.Selden CR, Zorn M, Ratzan SC, Parker RM, editors. In: National Library of Medicine current bibliographies in medicine: health literacy. NLM Pub. No. CBM 2000-1. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services; 2000. [Google Scholar]
- 8.van der Heide I, Wang J, Droomers M, Spreeuwenberg P, Rademakers J, Uiters E. The relationship between health, education, and health literacy: results from the Dutch adult literacy and life skills survey. J Health Commun. 2013;18(Suppl 1):172–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services. Maps of trends in diagnosed diabetes and obesity. Atlanta, GA: Centers for Disease Control and Prevention, Division of Diabetes Translation; 2015; http://www.cdc.gov/diabetes/statistics/slides/maps_diabetesobesity_trends.pdf. Accessed December 17, 2015. [Google Scholar]
- 10.Introduction. Academic Consortium for Integrative Medicine & Health Website. http://imconsortium.org/about/about-us.cfm. Accessed December 17, 2015.
- 11.Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014. July 1;63(25 Pt B):2960–84. [DOI] [PubMed] [Google Scholar]
- 12.Marchand WR. Mindfulness meditation practices as adjunctive treatments for psychiatric disorders. Psychiatr Clin North Am. 2013. March;36(1):141–52. [DOI] [PubMed] [Google Scholar]
- 13.Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013;29(5):450–60. [DOI] [PubMed] [Google Scholar]
- 14.Clarke TC, Black LI, Stussman BJ, et al. Trends in the use of complementary health approaches among adults: United States, 2002-2012. National health statistics reports; no. 79. Hyattsville, MD: National Center for Health Statistics; 2015. [PMC free article] [PubMed] [Google Scholar]
- 15.Burke A, Nahin RL, Stussman BJ. Reddy H, ed. Limited health knowledge as a reason for non-use of four common complementary health practices. PLoS One. 2015;10(6): e0129336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keosaian JE, Lemaster CM, Dresner D, et al. ‘We’re all in this together': a qualitative study of predominantly low income minority participants in a yoga trial for chronic low back pain. Complement Ther Med. 2016;24:34–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beaulac J, Kristjansson E, Cummins S. A systematic review of food deserts, 1966-2007. Prev Chronic Dis. 2009. July;6(3):A105. [PMC free article] [PubMed] [Google Scholar]
- 18.Nahin RL, Barnes PM, Stussman BJ, Bloom B. Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. National health statistics reports; no 18. Hyattsville, MD: National Center for Health Statistics; 2009. [PubMed] [Google Scholar]
- 19.Nahin RL, Stussman BJ, Herman PM. Out-of-pocket expenditures on complementary health approaches associated with painful health conditions in a nationally representative adult sample. J Pain. 2015;16(11):1147–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weeks J. The end of tinkering: international academic group explores transformational needs in health professional education. Global Adv Health Med. 2015;4(4):5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


