Abstract
Background:
Osteoarthritis often affects the joint bilaterally, and the single-stage (SS) unicompartmental knee arthroplasty (UKA) is advantageous in terms of a single anesthesia administration, a short hospital stay, lower medical costs, and enhanced patient convenience. However, the complication risk of SS UKA continues to be debated. The aim of this article was to evaluate the clinical effectiveness, complications, and functional recovery of SS and two-stage (TS) UKA.
Methods:
From January 2008 to December 2013, we compared a series of 36 SS UKA with 45 TS UKA for osteoarthritis. The mean age was 65.4 years (range: 55–75 years). The mean body mass index was 25.2 kg/m2 (range: 22–29 kg/m2). The pre- and post-operative Oxford Knee Scores (OKSs), complications, operative times, tourniquet times, the amount of drainage, and hemoglobin (Hb) were evaluated. The Chi-square test, Fisher's exact test, and paired and grouped t-tests were used in this study.
Results:
The mean follow-up was 50 months. No complications of death, fat embolism, deep vein thrombosis, and prosthetic infection were reported. Patients who underwent SS UKA had a shorter cumulative anesthesia time (113.5 vs. 133.0 min, P < 0.01). There were no significant variations between the values of the mean tourniquet time, the amount of drainage, pre- and post-operative Hb in the different groups. No patient required a blood transfusion. No statistical differences were found in the complications between two groups (P > 0.05). At the final follow-up, the mean OKS improved from 39.48 ± 5.69 to 18.83 ± 3.82 (P < 0.01), with no statistical differences between the two groups (P > 0.05). Patients who underwent SS UKA had a faster recovery.
Conclusions:
The single-staged UKA offers the benefits of a single anesthesia administration, reduced total anesthetic time, decreased overall rehabilitation time, and absence of an increase in perioperative mortality or complications compared with the TS bilateral UKA.
Keywords: Arthroplasty, Bilateral, Osteoarthritis, Single-stage, Unicompartmental
INTRODUCTION
In the past decade, unicompartmental knee arthroplasty (UKA) procedure achieved a great success in the treatment of medial compartment osteoarthritis: It reached 97% survival rate in 10 years.[1,2] Compared with the findings reported in earlier literature sources, the better survival of patients at present might be related to improvements in modern prosthetic designs, the application of less-invasive surgical techniques, or the more appropriate patient selection. UKA, with its bone-preserving nature, microdamage, and retention of natural kinematics, is a better solution for the treatment of osteoarthritis than total knee arthroplasty (TKA).
According to the results of some studies, the single-stage (SS) procedure in bilateral total knee replacement is associated with an increased number of complications and mortality.[3,4] There are fundamental differences between TKA and UKA. In contrast to TKA, UKA has a less-invasive procedure in which bone cement is utilized; the recovery is faster, and there are fewer and less severe complications and better function. The data from TKA studies cannot be directly extrapolated to UKA results. The aim of this article was to evaluate the clinical effectiveness, complications, and functional recovery of SS and two-stage (TS) UKA.
METHODS
From January 2008 to December 2013, 81 patients, 33 male, and 48 female patients (162 knees), received medial UKAs in our department. The mean age was 65.4 years (range: 55–75 years). The mean body mass index (BMI) was 25.2 kg/m2 (range: 22–29 kg/m2) [Table 1]. A part of the patients, 36, underwent single-stage (SS group) UKA, while 45 patients were subjected to two-stage (TS group) UKA, with time intervals between 3 and 6 months apart. All operations were performed by the same senior doctor in a district central hospital by updated instruments (Oxford Knee Phase III, Biomet Ltd., Bridgend, UK). All patients underwent anteroposterior, lateral, and valgus/varus stress radiographs [Figure 1].
Table 1.
Demographic data of patients undergoing medial UKAs in the two groups
| Items | SS group | TS group | t/χ2 | P |
|---|---|---|---|---|
| Gender (n) | 0.02 | 0.88† | ||
| Male | 15 | 18 | ||
| Female | 21 | 27 | ||
| ASA grade (n) | 0.32 | 0.85† | ||
| I | 18 | 25 | ||
| II | 9 | 12 | ||
| III | 8 | 8 | ||
| Age* (years) | 65.6 ± 6.1 | 65.3 ± 5.6 | 0.25 | 0.80‡ |
| BMI (kg/m2) | 25.0 ± 1.9 | 25.5 ± 2.0 | 1.15 | 0.25‡ |
Data were expressed as mean ± standard deviation or n. *Average age between two operations; †Chi-square test; ‡Grouped t-test. BMI: Body mass index; ASA: American Society of Anesthesiologists; UKAs: Unicompartmental knee arthroplasties; SS: Single-stage; TS: Two-stage.
Figure 1.
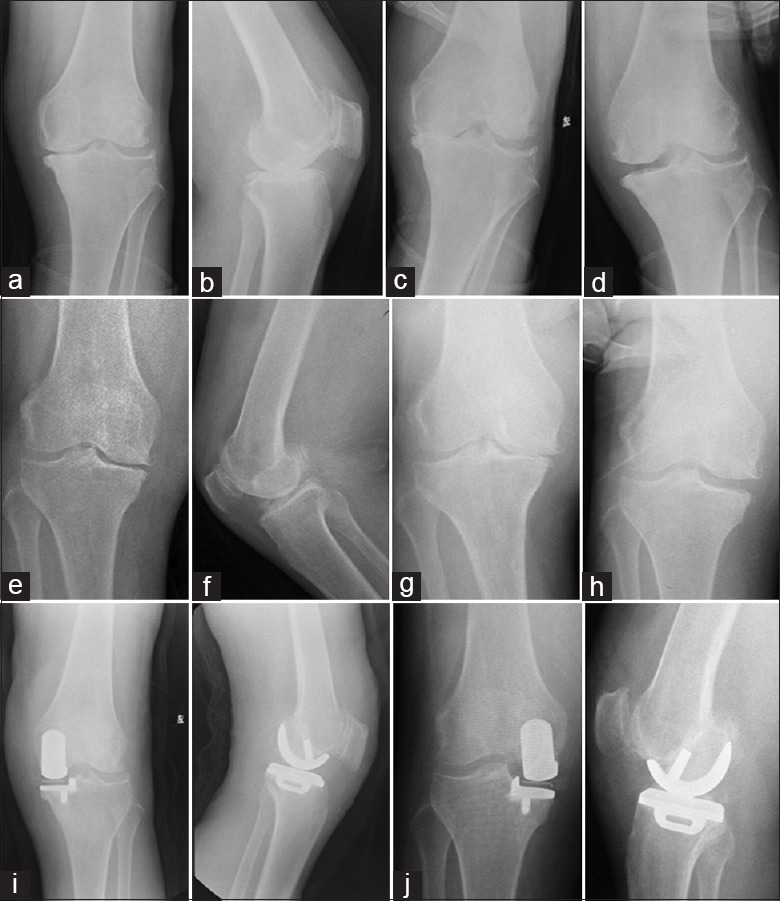
A 70-year-old female patient with bilateral medial osteoarthritis. Left knee: (a) Anteroposterior view, (b) lateral view, (c) varus stress view to confirm the full loss of cartilage in the medial compartment, (d) valgus stress view to confirm the entire correction of the deformity and the full thickness of cartilage in the lateral compartment. Right knee: (e) Anteroposterior view, (f) lateral view, (g) varus stress view, (h) valgus stress view, (i, j) X-ray showing restored components.
The selection criteria were as follow: (1) The criteria proposed by the Oxford group;[5] (2) American Society of Anesthesiologists (ASA) grade (the ASA physical status) of 3 or below; (3) Age ≤75 years. ASA is a system for assessing the fitness of cases before surgery. These are: Grade I, healthy person; Grade II, mild systemic disease; Grade III, severe systemic disease; Grade IV, severe systemic disease that is a constant threat of life; Grade V, a moribund person who is not expected to survive without the operation; and Grade VI, a declare brain-dead person.[4]
All patients underwent standard minimally invasive surgery described in the Oxford partial knee manual.[5] For an SS operation, one knee was operated on, and then the tourniquet deflated, and the wound was closed by an assistant. Concurrently, the contralateral tourniquet was then inflated, and surgery on the other leg commenced. For a TS operation, the tourniquet was deflated prior to closing the wound. The drain was extracted within 48 h. Postoperatively, all patients received chemoprophylaxis and mechanical compression boots for venous thromboembolism prevention. The same postoperative rehabilitation protocol was used for both groups. Static quadriceps exercises and continuous passive motion were started on the 1st postoperative day to achieve 90° knee flexion over 2–3 days. Walking with two crutches with weight-bearing was initiated on the same day.
The pre- and post-operative data of the clinical examinations and radiographs were recorded. Afterward, the clinical follow-up was assessed in the outpatient clinic at different increasing time intervals: 1 month, 3 months, 6 months, 1 year, and once per year. Each follow-up consisted of physical examination, registration of pain and complications, and a standard series of radiographs. Pain, function, and health-related quality of life were evaluated pre- and post-operatively by patient- and assessor-based outcome scores. The Oxford Knee Score (OKS) was used, which involved grading of pain and function, ranging from 12 to 60, with 12 being the best outcome.[6] The complications, operative times, tourniquet times, the amount of drainage, and hemoglobin (Hb) concentrations were evaluated. The patient was considered to need blood transfusion when the value of Hb content in the blood dropped below 80 g/L.
X-ray analysis was performed by an independent investigator who had not been involved into the surgical procedure. Subsidence, dislocation, loosening, and osteonecrosis changes in the lateral compartment were observed.
Statistical analysis
The data obtained were expressed as mean ± standard deviation (SD) or n, and analyzed using SAS 8.1 (SAS Institute, NC, USA). The gender and the grades of the ASA classification were compared between different groups via the Chi-square test. The complications were compared by using the Fisher's exact test. The pre- and post-operative OKS were juxtaposed through the paired t-test. The differences in the values of age, BMI, OKS, operative times, tourniquet times, amount of drainage, and Hb levels between different groups were compared by the grouped t-test. The significance level was set at P ≤ 0.05.
RESULTS
No significant differences between SS and TS group were found in terms of gender, age, BMI, and ASA grade [Table 1].
The average operation time for SS and TS group was 113.5 and 133.0 min (t = 9.26, P < 0.01). The mean tourniquet time for SS and TS group was 94.1 and 96.2 min (t = 1.17, P = 0.24). The amount of drainage was 175.5 ± 30.3 and 181.4 ± 37.7 (t = 0.76, P = 0.45). There were no significant differences between SS and TS group regarding the pre- and post-operative Hb levels. The lowest postoperative Hb concentration was 85 g/L, and no patient required blood transfusion [Table 2].
Table 2.
Clinical results of all patients undergoing medial UKAs in the two groups
| Variables | SS group | TS group | t/χ2 | P |
|---|---|---|---|---|
| Duration of anesthesia (min) | 113.5 ± 8.7 | 133.0 ± 9.9 | 9.26 | 0.00† |
| Tourniquet time (min) | 94.1 ± 7.5 | 96.2 ± 8.4 | 1.17 | 0.24† |
| Amount of drainage (ml) | 175.5 ± 30.3 | 181.4 ± 37.7 | 0.76 | 0.45† |
| Hb* (g/L) | ||||
| Preoperation | 127.6 ± 9.0 | 128.8 ± 9.1 | 0.64 | 0.53† |
| Postoperation | 105.4 ± 11.4 | 110.8 ± 15.9 | 1.69 | 0.10† |
| Total complications (n) | 3 | 5 | 0.73‡ | |
| Bearing dislocation | 1 | 1 | ||
| Lateral compartment osteoarthritis | 0 | 1 | ||
| Superficial infection | 1 | 1 | ||
| Vein thrombosis | 1 | 2 |
Data were expressed as mean ± standard deviation or n. *Hb is the average value of the two operations, the rest are a total of the two operations; †Grouped t-test; ‡Fisher’s exact test. Hb: Hemoglobin; UKAs: Unicompartmental knee arthroplasties.
The mean follow-up was 50 months (range: 12–84 months). No complications of death, fat embolism, pulmonary embolism, and prosthetic infections were established. No subsidence and loosening were observed in the X-ray test results. Bearing dislocations occurred in 2 cases, and we changed it, providing a thicker bearing. Lateral compartment osteoarthritis occurred in 1 case. It was revised and converted to TKA. Superficial infections occurred in 2 cases. Three patients had a distal vein thrombosis [Table 2]. At the final follow-up, the mean OKS improved from 39.48 ± 5.69 to 18.83 ± 3.82 (P < 0.01). One month after the operation, the mean OKS in the SS group was worse than that in the TS group (second operation) (P = 0.03). There were no significant differences between the SS and the TS group (second operation) at the other follow-up time after operation [Table 3].
Table 3.
OKS for all patients undergoing medial UKAs
| Groups | Preoperation | 1 month | 3 months | 6 months | Final follow-up |
|---|---|---|---|---|---|
| SS UKA | 40.8 ± 5.9 | 25.1 ± 3.2 | 20.0 ± 2.2 | 19.2 ± 2.7 | 18.3 ± 3.1 |
| TS UKA* | 40.5 ± 5.1 | 23.2 ± 4.0 | 19.7 ± 2.2 | 18.8 ± 2.5 | 18.0 ± 3.3 |
| t | 0.22 | 2.26 | 0.60 | 0.66 | 0.65 |
| P | 0.82 | 0.03 | 0.55 | 0.51 | 0.52 |
Data were expressed as mean ± standard deviation. *Second operation in TS group. UKAs: Unicompartmental knee arthroplasties; OKS: Oxford Knee Score.
DISCUSSION
Controversy still exists surrounding the performance of simultaneous versus staged arthroplasty in bilateral osteoarthritis. Osteoarthritis affects the joint bilaterally, causing pain and deformity to both knee joints. Simultaneous bilateral arthroplasty is advantageous in terms of a single anesthesia, a short hospital stay, low medical costs, and enhanced patient convenience.[3,7,8]
The safety and efficacy of the simultaneous versus the staged TKA continues to be debated.[3,9,10] More investigations evidenced that the simultaneous approach increased the acute blood loss, transfusion-related problems, and complications. Myocardial ischemia occurred 4–6 times more frequently in SS bilateral TKA patients than in unilateral TKA patients.[4,11] The risk of pulmonary embolism increased to 50–80% in patients undergoing bilateral TKA.[12,13] SS TKA increased also perioperative mortality.[4,14] Some points are to be considered in the SS TKA: Extreme age, ASA >3, pulmonary hypertension, chronic lung diseases, coronary artery disease, previous PE, and coagulopathies should be used as exclusion criteria.[15]
Compared to TKA, UKA has less-invasive procedure; the blood loss is lower and the procedure is less-invasive to the medullary canals, facilitating the faster recovery, short operative, and anesthetic times. All these advantages are important points since they lead to decreased rates of complications and mortalities in TKA.[15] UKA may be more appropriate for SS surgery due to the less-invasive nature of the procedure and the shorter surgical and anesthetic times.
The present studies reported that single-staged UKA offers the benefits of a single anesthesia, reduced total anesthetic time, shorter total hospital stay, diminished costs, and absence of necessity for an increase in blood transfusion rates.[16,17,18,19,20] In our research, we obtained similar results. The average operation time in the SS group was shorter than that in the TS group. There were no significant differences between the SS and TS groups in the values of the mean tourniquet time and Hb concentrations after the operation. No patient required a blood transfusion.
The key point is whether single-staged surgery increase complications and mortalities in UKA. Recent reports found no significant difference in morbidity and mortality between SS and TS UKA. Berend et al.[16] retrospectively compared 141 patients (282 knees) treated with staged UKA with 35 patients (70 knees) treated with simultaneous UKA. No patient experienced deep venous thrombosis, pulmonary embolism, confusion, or death. None needed blood transfusions or intensive care admissions. Though the staged group had more complications than the simultaneous group, there was no significant difference in the results of the statistical analysis. In a report by Akhtar et al.,[17] 38 patients (76 knees) underwent SS UKA. ASA grade of 3 or below was the only mandatory patient selection index. There were no morbidity and complications. Only 3 complications (7.9%) happened. One of them was a tibial plateau fracture, and two were superficial suture granulomas. There was also no significant difference between the rate of complications of the SS bilateral UKA and unilateral UKA, as evidenced by the findings of Boniforti and Romagnoli[18] and Pandit et al.[19] Chan et al.[20] promulgated a different opinion. In their investigation, 159 patients (318 knees) had one-stage and 80 patients (160 knees) were subjected to TS bilateral UKAs. The ASA grades of all patients were 3 or below, and the oldest patient was 85 years old. Major complications were diagnosed in 13 patients (8.2%) with one-stage operations, but none were encountered in the TS group. The researchers advocated caution before undertaking a one-stage operation by UKA because of the significantly higher risk of major complications. In their study, no chemoprophylaxis was used for the prevention of deep venous thrombosis, which could be correlated with the 11 cases of major complications caused by thrombosis. In comparison, we employed low-molecular-weight heparin and orally administered rivaroxaban to prevent venous thrombosis. None of the patients involved in the investigation had major complications, including death, fat embolism, pulmonary embolism, or myocardial ischemia. There were one bearing dislocation, one superficial infection, and one distal vein thrombosis which occurred in SS group. No significant difference was exhibited between the complications in the SS and TS group. Except the less-invasive nature of the procedure and the shorter surgical times in UKA, a selection bias (age ≤75 years, ASA ≤3) may have contributed to the diminished rate of complications in the SS group.
There are few studies focusing specifically on the benefit in the functional outcome of SS bilateral UKA. In the study conducted by Berend et al.,[16] the mean Knee Society Function Scores (87.9 vs. 72.9, P < 0.0001) and lower extremity activity score (11.3 vs. 10.2, P < 0.001) in the simultaneous group were higher than those of the staged group at the most recent follow-up. They assumed that some potential functional benefit of simultaneous UKA existed. In our research, the mean OKS in the SS group was worse than that in the TS group (second operation) at the 1-month point; there were no significant differences at the other follow-up times. Because interval windows between the first and the second operation exist in staged UKA (3–6 months in our experiments), we concluded that SS bilateral UKA can shorten the overall rehabilitation time compared with that of the TS bilateral UKA.
Our study had several limitations. First, the selection criteria were limited to patients in a younger age and good condition. Second, our patients were not routinely screened for venous thromboembolism postoperatively, which may have caused the increase in the reported rate. Third, objective factors, such as the range of movement, were not recorded, while a single scoring system was used.
In conclusion, single-staged UKA offers the benefits of a single anesthesia, reduced total anesthetic time, and decreased overall rehabilitation time compared with TS bilateral UKA. Based on patients’ selection, including age and physical condition, single-staged UKA can be performed without increasing perioperative mortality or complications.
Financial support and sponsorship
This study was supported by grants from the Shanghai Municipal Science and Technology Commission (No. 134119b1400) and the Shanghai Municipal Public Health and Family Planning Commission (No. 2013040).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yuan-Yuan Ji
REFERENCES
- 1.Price AJ, Waite JC, Svard U. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2005;(435):171–80. doi: 10.1097/00003086-200506000-00024. [DOI] [PubMed] [Google Scholar]
- 2.Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW. Minimally invasive Oxford phase 3 unicompartmental knee replacement: Results of 1000 cases. J Bone Joint Surg Br. 2011;93:198–204. doi: 10.1302/0301-620X.93B2.25767. [DOI] [PubMed] [Google Scholar]
- 3.Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty.A survival analysis. J Bone Joint Surg Am. 2003;85-A:1532–7. doi: 10.2106/00004623-200308000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Ritter M, Mamlin LA, Melfi CA, Katz BP, Freund DA, Arthur DS. Outcome implications for the timing of bilateral total knee arthroplasties. Clin Orthop Relat Res. 1997;(345):99–105. [PubMed] [Google Scholar]
- 5.Goodfellow JW, O’Connor JJ, Dodd CA, Murray DW. New York: Oxford University Press; 2006. Unicompartmental Arthroplasty with the Oxford Knee. [Google Scholar]
- 6.Whitehouse SL, Blom AW, Taylor AH, Pattison GT, Bannister GC. The Oxford Knee Score; problems and pitfalls. Knee. 2005;12:287–91. doi: 10.1016/j.knee.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Husted H, Troelsen A, Otte KS, Kristensen BB, Holm G, Kehlet H. Fast-track surgery for bilateral total knee replacement. J Bone Joint Surg Br. 2011;93:351–6. doi: 10.1302/0301-620X.93B3.25296. [DOI] [PubMed] [Google Scholar]
- 8.Leonard L, Williamson DM, Ivory JP, Jennison C. An evaluation of the safety and efficacy of simultaneous bilateral total knee arthroplasty. J Arthroplasty. 2003;18:972–8. doi: 10.1016/s0883-5403(03)00282-1. [DOI] [PubMed] [Google Scholar]
- 9.Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br. 2009;91:64–8. doi: 10.1302/0301-620X.91B1.21320. [DOI] [PubMed] [Google Scholar]
- 10.Memtsoudis SG, Ma Y, González Della Valle A, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, et al. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111:1206–16. doi: 10.1097/ALN.0b013e3181bfab7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bullock DP, Sporer SM, Shirreffs TG., Jr Comparison of simultaneous bilateral with unilateral total knee arthroplasty in terms of perioperative complications. J Bone Joint Surg Am. 2003;85-A:1981–6. doi: 10.2106/00004623-200310000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Barrett J, Baron JA, Losina E, Wright J, Mahomed NN, Katz JN. Bilateral total knee replacement: Staging and pulmonary embolism. J Bone Joint Surg Am. 2006;88:2146–51. doi: 10.2106/JBJS.E.01323. [DOI] [PubMed] [Google Scholar]
- 13.Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty.A meta-analysis. J Bone Joint Surg Am. 2007;89:1220–6. doi: 10.2106/JBJS.F.01353. [DOI] [PubMed] [Google Scholar]
- 14.Parvizi J, Sullivan TA, Trousdale RT, Lewallen DG. Thirty-day mortality after total knee arthroplasty. J Bone Joint Surg Am. 2001;83-A:1157–61. doi: 10.2106/00004623-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Vulcano E, Memtsoudis S, Della Valle AG. Bilateral total knee arthroplasty guidelines: Are we there yet? J Knee Surg. 2013;26:273–9. doi: 10.1055/s-0032-1329721. [DOI] [PubMed] [Google Scholar]
- 16.Berend KR, Morris MJ, Skeels MD, Lombardi AV, Jr, Adams JB. Perioperative complications of simultaneous versus staged unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2011;469:168–73. doi: 10.1007/s11999-010-1492-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akhtar KS, Somashekar N, Willis-Owen CA, Houlihan-Burne DG. Clinical outcomes of bilateral single-stage unicompartmental knee arthroplasty. Knee. 2014;21:310–4. doi: 10.1016/j.knee.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 18.Boniforti F, Romagnoli S. Bilateral sequential unicompartmental knee replacement. J Bone Joint Surg (Br) 2006;88-B Supp III:423. [Google Scholar]
- 19.Pandit H, Jenkins C, Barker K, Dodd CA, Murray DW. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br. 2006;88:54–60. doi: 10.1302/0301-620X.88B1.17114. [DOI] [PubMed] [Google Scholar]
- 20.Chan WC, Musonda P, Cooper AS, Glasgow MM, Donell ST, Walton NP. One-stage versus two-stage bilateral unicompartmental knee replacement: A comparison of immediate post-operative complications. J Bone Joint Surg Br. 2009;91:1305–9. doi: 10.1302/0301-620X.91B10.22612. [DOI] [PubMed] [Google Scholar]


