Abstract
Background
The mechanical thrombectomy (MT) for endovascular clot retrieval has dramatically improved successful revascularization and clinical outcome in selected acute stroke patients. MT is typically performed via a transfemoral approach, but catheterization of the occluded vessel can be problematic in cases of extensive vessel tortuosity. We describe a case of MT with the ‘ADAPT’ technique by direct carotid access due to an inability to catheterize the ICA by a transfemoral approach for acute cerebral ischemia in the setting of left MCA occlusion. Excellent angiographic and good clinical results were obtained without any complications.
Case report
An 80-year-old woman was admitted with a stroke by occlusion of the left MCA, with an NIHSS: 11, and an ASPECT: 7 in the CT. Under sedation a transfemoral angiography was performed, but after multiple attempts, it was impossible to make a stable catheterization of the left CCA. A transcervical approach was pursued. With ultrasound guidance the CCA was catheterized. Using the ‘ADAPT’ technique, we performed a successful MT. Post-procedure angiography (at 14 minutes) demonstrated recanalization of the entire left MCA (TICI: 3), without complications. The carotid access point was closed with a percutaneous closure. Control TC at 24 h showed a slight hypodensity in the left lenticular nucleus, and loss of gray-white matter differentiation in the adjacent cortex. Neurologically, the patient presented with progressive improvement. At discharge, she had an NIHSS: 0, mRS: 0 and Barthel: 100.
Conclusions
MT by direct carotid access is an effective alternative technique in those cases where it is not accessible by a transfemoral approach.
Keywords: Thrombectomy, embolectomy, reperfusion, ADAPT, acute stroke, interventional neuroradiology
Introduction
Increasing lines of evidence have established a strong relationship between good functional outcomes after an ischemic stroke and fast reperfusion times. Mechanical thrombectomy is an important alternative strategy to restore flow, particularly in large vessel occlusive disease. Several clinical trials1–9 have demonstrated that the endovascular treatment of acute stroke patients with large artery occlusion reduces significantly the severity of post-stroke disability and increases the rate of functional independence.
The benefit of intra-arterial approaches, however, is negated by long delays in achieving reperfusion. Numerous barriers can lead to delayed revascularization including the logistics of patient transfer and the use of time-consuming advanced imaging. The standard endovascular approach to acute stroke intervention is the common femoral approach. The preference for this approach is related to the compressibility of the right common femoral artery, the potential for less dire consequences in case of femoral artery injury compared to carotid artery injury and to the fact that via this approach all brachiocephalic vessels can be catheterized and thus multiple potential sites of occlusion (e.g. anterior versus posterior circulation) can be accessed. Age and traditional cerebrovascular risk factors promote the elongation and tortuosity of the femoral, iliac, aortic, brachiocephalic and cervical arteries. Additional challenges in catheter navigation include thoracic aortic aneurysms and severe thoracic aortic atherosclerosis. Therefore once groin access is achieved, procedural times may be significantly prolonged in cases of difficult anatomy. Sometimes the target vessel cannot be quickly catheterized, or is impossible to catheterize, via the transfemoral approach, necessitating alternative access via a transcervical approach.
Case report
An 80-year-old white woman was admitted to our comprehensive stroke center 1.5 hours after the onset of right hemiparesis and aphasia. Physical examination disclosed mute aphasia, right facial paralysis and distal mild claudication of the right hand. The National Institutes of Health Stroke Scale (NIHSS) score was 11. A computed tomography (CT) scan showed a hyperdensity of the left middle cerebral artery (MCA) with hypoattenuation of the left caudate and lenticular nucleus and insula (Alberta stroke program early CT score (ASPECT): 7). CT perfusion: increased mean transit time (MTT) and decreased cerebral blood flow (CBF) in virtually all the territory of the left MCA with a cerebral blood volume (CBV) decreased in the caudate and lenticular nucleus and slightly in the left parietal subcortical white matter. Mismatch with> 20%.
The patient was transferred to our Angio Suite for endovascular treatment. Under sedation a diagnostic cerebral angiography was performed, but after multiple attempts, it was impossible to make a stable catheterization of the left common carotid artery (CCA). Numerous catheters and wires could not be passaged distally in the common carotid to permit exchange of the diagnostic catheter for a shuttle sheath or a balloon-guiding catheter (Figure 1). After at least 45 minutes of procedural time, the transfemoral approach was abandoned and a transcervical approach was pursued. In the supine position, the neck was extended. A rolled sheet was placed underneath the shoulders to help facilitate positioning. The neck was sterilized with an iodine povidone solution and then prepped and draped in normal sterile fashion. After subcutaneous administration of 2% lidocaine, the left CCA was visualized with ultrasonography (US) as necessary to achieve access using an Abbocath needle. The most superficial aspect of the CCA proximal to the bifurcation was targeted (Figure 2). Once brisk arterial blood was visualized in the Abbocath needle, an angled 0.035 glidewire (Terumo, Japan) was advanced followed by a 6-Fr sheath (Terumo, Japan) with the Seldinger technique. A skin incision was necessary to facilitate catheter advancement. It should be noted that advancing the sheath through the cervical carotid is much more difficult than penetrating the femoral artery and requires significant forward pressure. The sheath (Terumo) was subsequently connected to a pressurized non-heparinized saline infusion. The introducer sheath was advanced as distally as possible over the wire (Figure 3).
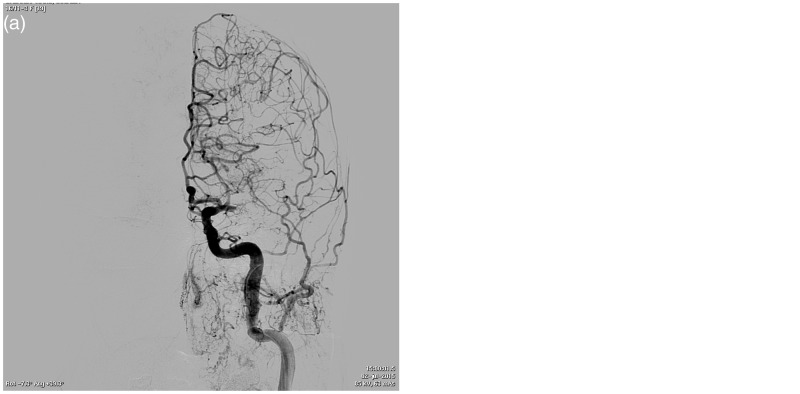
Figure 1.
(a) Aortic arch angiography showing elongated and tortuous supra-aortic trunks. (b) and (c) After multiple attempts, it was impossible to make a stable catheterization of the left common carotid artery. Numerous catheters and wires could not be passaged distally in the common carotid to permit exchange of the diagnostic catheter for a shuttle sheath or a balloon-guiding catheter.
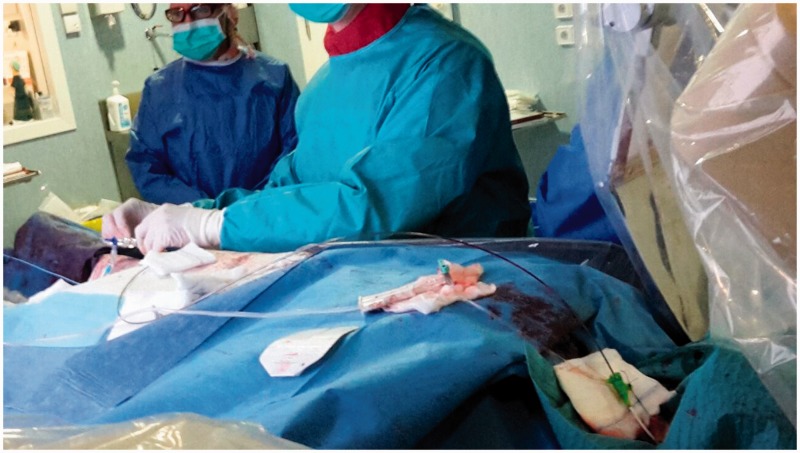
Figure 2.
Ultrasound-guided puncture of the common carotid artery.
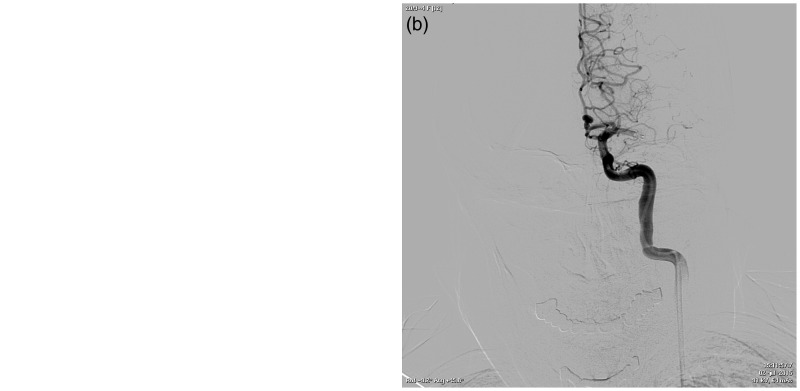
Figure 3.
(a) and (b) First angiography through the sheath in the common carotid artery, showing occlusion of the left middle cerebral artery.
With a 0.014-inch Syncro® guidewire (Stryker), the 5MAX™ ACE catheter (Penumbra) was advanced until reaching the thrombus, with an aspiration pump engaging the clot, and after gently withdrawing the device under continuous suction (Direct Aspiration First Pass Technique (ADAPT)). During this maneuver, an introducer sheath aspiration was performed with a 60 cc syringe (Figures 4 and 5). Post-procedure angiography (at 14 minutes) demonstrated successful recanalization of the entire left MCA (Thrombolysis in Cerebral Infarction scale (TICI): 3), and reperfusion with normal antegrade flow into the distal MCA branches. There was no evidence of distal emboli (Figure 6).
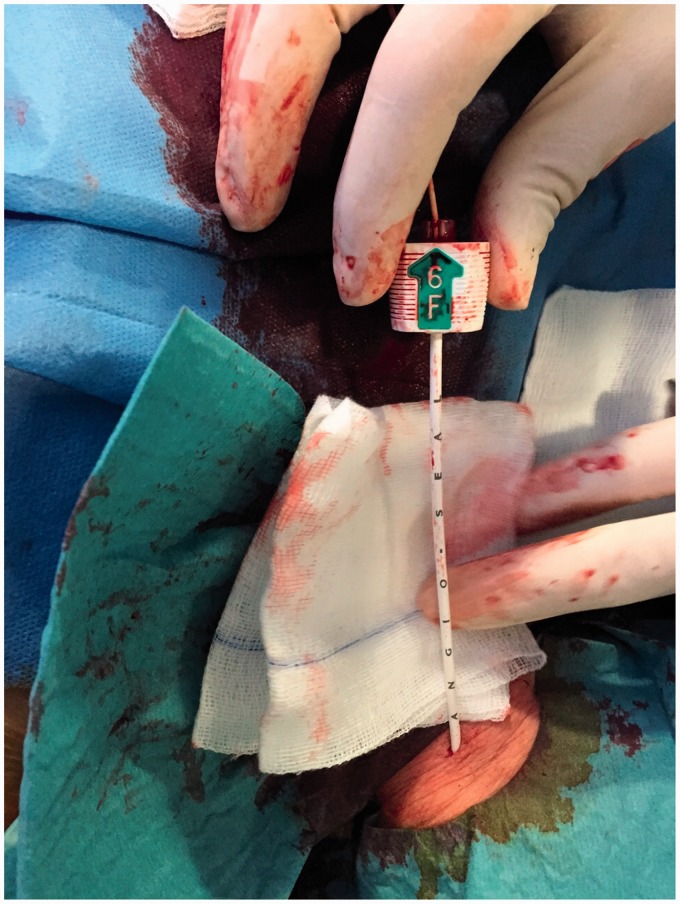
Figure 4.
This photo shows the 6F introducer (Terumo) in the CCA, and as the interventional neuroradiologist (INR) enters and navigates the 5MAX ACE™ catheter (Penumbra) until reaching the thrombus.
Figure 5.
(a) and (b) Angiography showing the 5MAX ACE™ catheter (Penumbra) trapping the thrombus.
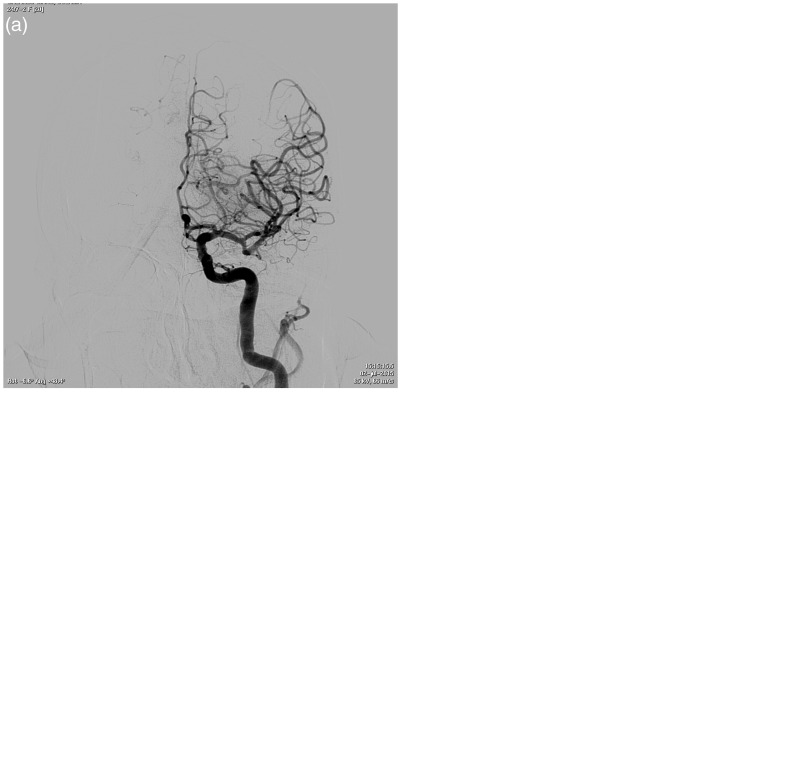
Figure 6.
(a)–(d) Post-procedure angiography (at 14 minutes) demonstrated successful recanalization of the entire left middle cerebral artery (MCA) (Thrombolysis in Cerebral Infarction scale (TICI): 3), and reperfusion with normal antegrade flow into the distal MCA branches. There was no evidence of distal emboli.
Finally, the carotid access point was closed with a percutaneous closure (Angio-Seal™ Evolution™ vascular closure device, St. Jude Medical, St. Paul, MN, USA) (Figure 7).
Figure 7.
The carotid access point was closed with a percutaneous closure (Angio-Seal™ Evolution™ vascular closure device, St. Jude Medical, St. Paul, MN, USA).
Control CT at 24 h showed a slight hypodensity in the left lenticular nucleus, and loss of gray-white matter differentiation in the adjacent cortex.
Neurologically, the patient presented with progressive improvement. After thrombectomy, she had an NIHSS: 4, and at discharge, NIHSS: 0, modified Rankin scale (mRS): 0 and Barthel: 100.
Discussion
Persistent large vessel occlusive disease is associated with high rates of mortality and morbidity. The use of the new techniques of mechanical thrombectomy for the revascularization of acute stroke patients has significantly improved efficacy and safety; moreover, they have led to a revolution in the management of stroke patients with large artery occlusion, since they can dramatically reduce disability without increasing the rate of adverse events with respect to intravenous thrombolysis.1–9
While transfemoral access remains the preferred approach, in some cases, difficult catheter access can lead to lower rates of recanalization and ultimately poor clinical outcomes. These patients may benefit the most from an alternative approach as transcervical access.
Transcervical access has been a successful alternate strategy for carotid stenting10 and aneurysm coiling.11
The transfemoral approach has been associated with increasingly fast rates of groin access to recanalization, particularly with the advent of retrievable stents, “stentrievers.” Also, once transcervical access was achieved, recanalization was similarly observed at ultrafast rates (25 ± 14 min).12 In our case, we spent 14 minutes.
While transcervical access may facilitate faster and higher rates of recanalization in a subset of patients, many challenges remain. The most important is difficulty achieving hemostasis with resultant neck hematoma. This can lead to elective intubation for airway protection, although surgical hematoma evacuation is not always necessary. Previous series have reported a 4–7% rate of neck hematoma after sheath removal.13 An open surgical exposure may be superior in achieving hemostasis as it mitigates the need for manual compression or a closure device; however, open surgical exposure may not be readily feasible in the acute stroke setting. Although manual compression alone has also been used with good success, even in cases of patients on dual antiplatelet therapy,14 at present, the use of closure devices for this technique is limited but it has a promising future. The ideal closure device would be exclusively extravascular and avoid the need for leaving behind an intravascular foreign body with subsequent risk of distal embolization. However, a previous paper described the use of the Mynx® closure device (Access Closure Inc, Mountain View, CA, USA) without good success for carotid artery closure.12 The use of alternative transfemoral closure devices such as Angio-Seal™ (St. Jude’s Medical Inc)15 and StarClose® (Abbott) may lead to superior results. In our case we used the Angio-Seal ™ Evolution ™ vascular closure device, with an excellent result. The use of Perclose ProGlide® (Abbott) or Exoseal™ (Cordis) for this purpose has not been described.
Today, technological and technical advances allow us to treat patients with acute ischemic stroke whose difficult anatomical structure prevents or hinders the treatment commonly used in patients with normal anatomical arrangement.
Conclusions
Difficult catheter access of the target vessel by transfemoral access can limit successful and timely recanalization in a subset of patients with acute stroke. The transcervical approach is a feasible and efficacious strategy to achieve fast recanalization once the carotid artery is accessed. Future studies should focus on early triage of patients most likely to require transcervical access to further limit procedural times as well as improving methods of achieving hemostasis.
Acknowledgments
All the co-authors have reviewed and approved the final version of the manuscript. All co-authors had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
We acknowledge the work and cooperation of the vascular neurologists, residents, anesthetists and neurointerventional nurses in the management of these patients.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
Dr Castaño is a Covidien consultant. All other authors have nothing to declare.
References
- 1.Castaño C, Serena J, Davalos A. Use of the new Solitaire™ AB device for mechanical thrombectomy when Merci clot retriever has failed to remove the clot. Interv Neuroradiol 2009; 15: 209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Castaño C, Dorado L, Guerrero C, et al. Mechanical thrombectomy with Solitaire AB device in large artery occlusions of the anterior circulation: A pilot study. Stroke 2010; 41: 1836–1840. [DOI] [PubMed] [Google Scholar]
- 3.Pereira VM, Gralla J, Davalos A, et al. Prospective, multicenter, single-arm study of mechanical thrombectomy using Solitaire Flow Restoration in Acute Ischemic Stroke (STAR study). Stroke 2013; 44: 2802–2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): A randomised, parallel-group, non-inferiority trial. Lancet 2012; 380: 1241–1249. [DOI] [PubMed] [Google Scholar]
- 5.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 6.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 7.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. [DOI] [PubMed] [Google Scholar]
- 8.Saver JL, Goyal M, Bonafé A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 9.Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372: 2296–2306. [DOI] [PubMed] [Google Scholar]
- 10.Matsuda Y, Terada T, Masuo O, et al. The clinical results of transcervical carotid artery stenting and frequency chosen as the approach route of carotid artery stenting in 1,067 consecutive cases. Acta Neurochir (Wien) 2013; 155: 1575–1581. [DOI] [PubMed] [Google Scholar]
- 11.Nii K, Kazekawa K, Onizuka M, et al. Direct carotid puncture for the endovascular treatment of anterior circulation aneurysms. AJNR Am J Neuroradiol 2006; 27: 1502–1504. [PMC free article] [PubMed] [Google Scholar]
- 12.Jadhav AP, Ribo M, Grandhi R, et al. Transcervical access in acute ischemic stroke. J Neurointerv Surg 2014; 6: 652–657. [DOI] [PubMed] [Google Scholar]
- 13.Blanc R, Piotin M, Mounayer C, et al. Direct cervical arterial access for intracranial endovascular treatment. Neuroradiology 2006; 48: 925–929. [DOI] [PubMed] [Google Scholar]
- 14.Mathieu X, Piret V, Bergeron P, et al. Choice of access for percutaneous carotid angioplasty and stenting: A comparative study on cervical and femoral access. J Cardiovasc Surg (Torino) 2009; 50: 677–681. [PubMed] [Google Scholar]
- 15.Blanc R, Mounayer C, Piotin M, et al. Hemostatic closure device after carotid puncture for stent and coil placement in an intracranial aneurysm: Technical note. AJNR Am J Neuroradiol 2002; 23: 978–981. [PMC free article] [PubMed] [Google Scholar]