Abstract
The presence of sulcal hyperdensity in patients after endovascular procedures is not necessarily attributable to hemorrhage. It may frequently indicate the absolute or concomitant extravasation of contrast material into the subarachnoid spaces.
This case report describes the clinical case of an 84-year-old patient with 90% stenosis of the right internal carotid who presented with a diffuse gyral and sulcal hyperdensity in the right temporal-occipital and frontal lobes at routine post-carotid stenting (CAS) brain CT scan. The patient was asymptomatic and CT findings were interpreted as contrast enhancement hyperattenuation and no therapeutic decisions were made. A 24-hour follow-up brain CT demonstrated the complete resolution of the hyperdensity, confirming the diagnosis.
In this patient we considered the concomitant presence of gyral and sulcal hyperdensity as the consequence of reversible damage to the blood-brain barrier (BBB) determining a transitory extravasation of contrast material. Asymptomatic gyral and subarachnoid contrast enhancement following CAS is generally indicative of benign and transitory damage to the BBB and is not to be misinterpreted as hemorrhage.
Keywords: carotid angioplasty and stenting, contrast extravasation
Introduction
Post-procedural non-contrast brain CT scan is the most widely used method to rule out hemorrhagic complications due to cerebral hyperperfusion syndrome (CHS) in patients who have undergone endovascular treatments.1
Gyral and subarachnoid hyperdensity on plain CT scan after endovascular treatment is not necessarily indicative of a hemorrhagic complication. Hyperdense abnormalities detected on post-procedural CT scan may in fact represent transitory damage to the microvascular integrity of the brain and consequent BBB insufficiency. Reversible CT hyperdensity within subarachnoid and cisternal spaces, mimicking hemorrhage, has been described after different neurovascular procedures [i.e., diagnostic angiography, aneurysm coiling, embolization of arteriovenous malformations (AVM) and CAS].2–4 The true pathogenic mechanism for this reversible condition is still debated.5–7 Yong et al.8 postulated that injury limited to the BBB endothelial cells determines brain contrast enhancement with no hemorrhagic product, whereas damage extending to the basal lamina of the BBB causes contrast extravasation and some degree of hemorrhage. Contrast enhancement following neuroendovascular procedures is therefore considered a benign finding not associated with neurologic symptoms, and resolves radiographically by 20 to 25 hours. Conversely, contrast extravasation and hemorrhage are not expected to resolve as quickly.9,10
Case Report
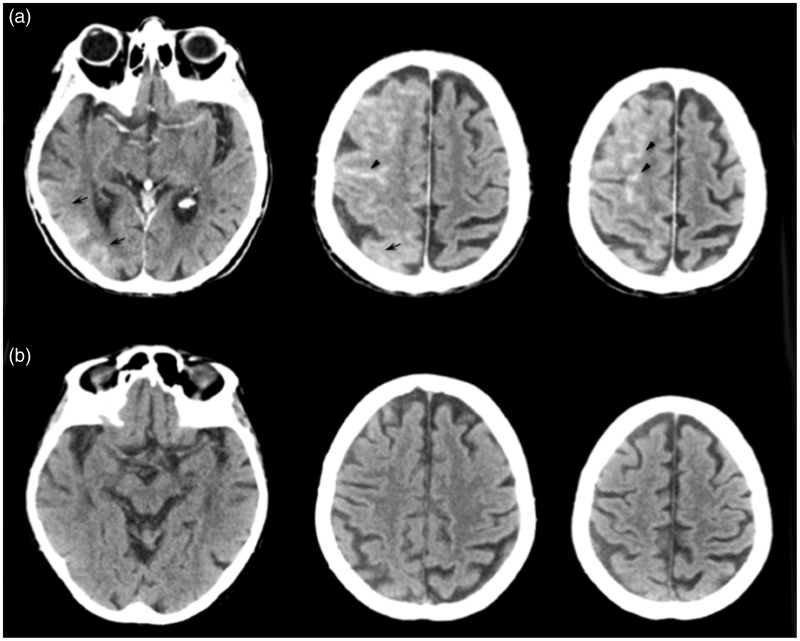
An 84-year old woman underwent right CAS for treatment of a symptomatic 90% stenosis of the right internal carotid. Her medical history included arterial hypertension, hypercholesterolemia, diabetes and two episodes of transient ischemic attacks. At admission a right carotid bruit was present, the neurological examination was normal, blood pressure level was 130/80 mmHg and a plain brain CT scan was unremarkable. After pre-treatment with heparin and clopidogrel, the CAS procedure was performed using a protection device and positioning a self-expanding stent across the stenotic plaque. The CAS procedure was complicated by tortuous arterial anatomic features, therefore a considerable amount (400 mL; 8.33 mL/Kg) of iomeprol, a monomeric nonionic contrast medium, was administered. The patient’s blood pressure was controlled during the procedure, and there was no evidence of hypertension. Undesired events did not occur during the procedure. The patient did not present any neurological symptoms postoperatively. At the control angiogram the stent was correctly positioned. A routine post-procedure brain CT scan showed a diffuse gyral and sulcal hyperdensity (<64 HU) in the right temporal-occipital and frontal lobes (Figure 1a). Due to the patient’s intact neurological status, CT findings were interpreted as related to gyral contrast enhancement and extravasation of contrast material into the subarachnoid spaces and no therapeutic decisions were made. A 24-hour follow-up brain CT demonstrated a complete resolution of the gyral and subarachnoid hyperdensity (Figure 1b).
Figure 1.
a) A post-procedure plain head-CT shows diffuse hyperdensity (<64 HU) of the cortical ribbon and within the subarachnoid space of the right fronto-temporo-parietal region, ipsilateral to the treated carotid. b) 24-hour CT follow-up shows a complete resolution of all findings in A.
Discussion
Gyral and subarachnoid CT hyperdensity following endovascular treatments often represents a condition connected to a unique pathogenic mechanism related to a reversible and of varying degree BBB damage.
The gyral and sulcal hyperdensity after the prolonged procedure to CAS in this case could be due to different pathological causes. The first possible explanation consists in a subarachnoid hemorrhage secondary to rupture of a vascular malformation. The fact that the patient did not show any aneurysm or AVM at the angiographic study, along with the normal arterial blood pressure level and neurological status and a extremely rapid resolution of the hyperdensity at 24-hour CT follow-up weighed against this hypothesis. Furthermore the gyral hyperdensity we observed was unlikely to represent an enhancing subacute infarct, as we did not identify any hypodense infarcts on the follow-up CT.
Therefore, we suggest that in this patient the gyral and sulcal hyperdensity following carotid stenting and administration of a large dose of contrast medium was the consequence of transient BBB damage with secondary contrast extravasation. As opposed to hemorrhage, Brisma et al.9 defined the presence of contrast enhancement after endovascular treatment as a benign and reversible finding (by 24 hours) directly correlated to the amount of contrast material administered during the procedure (relative to body weight), microcatheter time, total balloon inflation time, number of balloon inflations and antiplatelet agent therapy. The same authors indicated a cut-off value of <70 HU to distinguish contrast enhancement from hemorrhage since contrast enhancement has a lower attenuation than hemorrhage. In this patient the hyperdensity of 64 HU was indicative of contrast enhancement more than hemorrhage and the absence of neurological symptoms reinforced this hypothesis which was definitively confirmed by the complete reversibility of the CT findings at 24-hour follow-up.
Gyral and sulcal hyperdensity following CAS in an asymptomatic patient may both represent a benign and fully reversible condition which is not to be misinterpreted as hemorrhage and which does not require additional diagnostic procedures or therapy. The rapid resolution of the sulcal hyperdensity in our patient was likely due to the presence of contrast material and not blood in the subarachnoid spaces, as confirmed by the relatively low density (64 HU).
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Tavares A, Caldas JG, Castro CC, et al. Changes in perfusion-weighted magnetic resonance imaging after carotid angioplasty with stent. Interv Neuroradiol 2010; 16: 161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kawabata Y, Fumihiko H, Miyake H, et al. Follow-up outcomes of self-expanding stents for carotid artery angioplasty at a single hospital. Neuroradiol J 2010; 23: 622–628. [DOI] [PubMed] [Google Scholar]
- 3.Leonardi M, Dall'Olio M, Raffi L, et al. Carotid stenting without angioplasty and without protection. The advantages of a less invasive procedure. Interv Neuroradiol 2008; 14: 153–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gado MH, Phelps ME, Coleman RE. An extravascular component of contrast enhancement in cranial computed tomography. Part I. The tissue-blood ratio of contrast enhancement. Radiology 1975; 117: 589–593. doi: 10.1148/117.3.589. [DOI] [PubMed] [Google Scholar]
- 5.Eckel TS, Breiter SN, Monsein LH. Subarachnoid contrast enhancement after spinal angiography mimicking diffuse subarachnoid hemorrhage. Am J Roentgenol 1998; 170: 503–505. doi: 10.2214/ajr.170.2.9456974. [DOI] [PubMed] [Google Scholar]
- 6.Sharma P, Poppe AY, Eesa M, et al. Extravasating contrast material on angiography following carotid angioplasty and stenting: not necessarily subarachnoid hemorrhage. J Neuroimaging 2010; 20: 180–182. doi: 10.1111/j.1552-6569.2008.00316.x. [DOI] [PubMed] [Google Scholar]
- 7.Sharp S, Stone J, Beach R. Contrast agent neurotoxicity presenting as subarachnoid hemorrhage. Neurology 1999; 52: 1503–1505. doi: 10.1212/WNL.52.7.1503. [DOI] [PubMed] [Google Scholar]
- 8.Yoon W, Seo JJ, Kim JK, et al. Contrast enhancement and contrast extravasation on computed tomography after intra-arterial thrombolysis in patients with acute ischemic stroke. Stroke 2004; 35: 876–881. doi: 10.1161/01.STR.0000120726.69501.74. [DOI] [PubMed] [Google Scholar]
- 9.Brisman JL, Jilani M, McKinney JS. Contrast enhancement hyperdensity after endovascular coiling of intracranial aneurysms. Am J Neuroradiol 2008; 29: 588–593. doi: 10.3174/ajnr.A0844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Payabvash S, Qureshi MH, Khan SM, et al. Differentiating intraparenchymal hemorrhage from contrast extravasation on post-procedural noncontrast CT scan in acute ischemic stroke patients undergoing endovascular treatment. Neuroradiology 2014; 56: 737–744. doi: 10.1007/s00234-014-1381-8. [DOI] [PubMed] [Google Scholar]