Abstract
Cerebral venous sinus thrombosis (CVST) is an uncommon but potentially life-threatening condition. When showing resistance to treatment or a malignant progression despite anticoagulant therapy, endovascular interventional treatment is of help. The Penumbra System (PS), a novel thrombectomy device specifically designed to remove the thrombus in acute ischemic stroke, also proved to be an effective device for mechanical recanalization of CVST. We first reported two cases successfully treated using the PS in the management of intractable CVST in Asia, and analyzed the technical differences of use of the device through a systematic review of the literature.
One patient underwent mechanical thrombectomy of the thrombosed superior sagittal sinus using the 0.054-inch PS catheter when direct pharmacological thrombolysis failed. The other patient underwent mechanical thrombectomy using the 0.041-inch PS catheter with adjuvant local pharmacological thrombolysis. Literature reports on the use of the PS in patients with CVST were reviewed.
Successful venous recanalization was achieved using the PS. The patients improved symptomatically following the intervention. Literature reports showed that the PS can be successfully applied for treatment of CVST, though the methods used previously were diverse.
The PS has proved to be effective in the rapid recanalization of CVST, but different treatment techniques exist. The solution to these problems depends on more clinical trials as well as further improvements to devices.
Keywords: cerebral venous vinus thrombosis, treatment, vascular intervention, thrombectomy
Introduction
Cerebral venous sinus thrombosis (CVST) has been associated with coagulation disorders, hormonal changes, and acute and chronic systemic diseases.1 The approach to treatment includes anticoagulation (intravenous heparin or subcutaneous low molecular weight heparin), thrombolysis (systemic or local), and symptomatic treatment (including antiepileptic therapy, lowering intracranial pressure, decompressive craniectomy and so on).2,3 When the thrombosis is refractory to anticoagulation or deteriorating progressively, endovascular interventional treatment, including pharmacological thrombolysis and mechanical thrombectomy, is frequently advocated. Mechanical thrombectomy can be performed alone or in combination with pharmacological thrombolysis.4,5 In spite of limitations, mechanical devices such as balloon angioplasty, rheolytic catheters or snares have sometimes been used to disrupt and remove clot material.6–8 Recently, some researchers attempted to make use of the Penumbra System (PS; Alameda, CA, USA) in the treatment of CVST,9–13 which proved to be a novel device for the revascularization of large vessel thromboembolic occlusions in acute ischemic stroke.14 However, the techniques of treatments they adopted were varied. We report on the successful use of the PS in the management of two patients with CVST and analyze technical differences through a systematic review of the literature.
Materials and Methods
All patients or their immediate family members in our case provided informed consent using a protocol approved by our institutional ethics committees.
Case 1
The patient was a 29-year-old man with a history of hyperthyroidism. He presented to an outlying hospital with six-day history of headache and vomiting. His headache was not responding to treatment and worsening. At the time of admission to our hospital, neurological examination revealed left hemiparesis. Initial non-contrast brain computed tomography (CT), magnetic resonance imaging (MRI), and MR venography (MRV) studies demonstrated an acute hemorrhage in right parietal lobe and dural venous sinus thrombosis involving superior sagittal sinus (SSS) and the right transverse sinuses (Figure 1). Although he received anticoagulation with subcutaneous low-molecular weight heparin (90 IU/kg twice daily) and intracranial pressure lowering mannitol in drip, on day 2 he experienced obnubilation and frequent convulsions. He also developed ophthalmocele, bulbar conjunctival hyperemia, and progressively increasing intracranial pressure. On the basis of clinical deterioration, he was taken urgently for endovascular treatment.
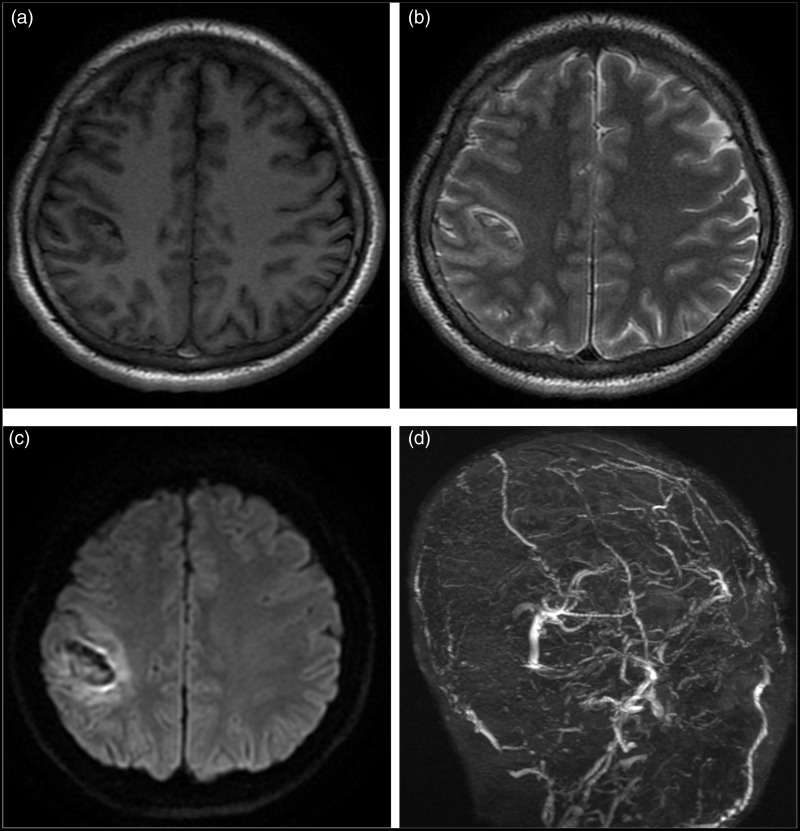
Figure 1.
Preprocedure MRI and MRV. A lesion in the right parietal lobe is isointense on axial T1WI (a), hyperintense on axial T2WI (b), and hypointense on axial T2*WI (c), demonstrating an acute hemorrhage. Occlusion of SSS and the right transverse sinuse on MRV (d).
Firstly, he received local infusion thrombolytic therapy. A 6- and a 5-Fr introducer sheath were placed in the right femoral vein and left femoral artery, respectively. A 5-Fr diagnostic catheter was used for accessing the left internal carotid artery. Contrast material injections demonstrated complete occlusion of the SSS (Figure 2). Through the femoral route, a 6-Fr guiding catheter (Boston Scientific, Natick, MA, USA) was navigated to reach the right jugular bulb. The microcatheter was then navigated coaxially through the 6-Fr guiding catheter to the thrombus of the SSS. A gentle contrast injection showed string-like venous outflow directed anteriorly. Through the microcatheter, continuous local infusion thrombolytic therapy with urokinase was initiated at a rate of 40,000 U/h.
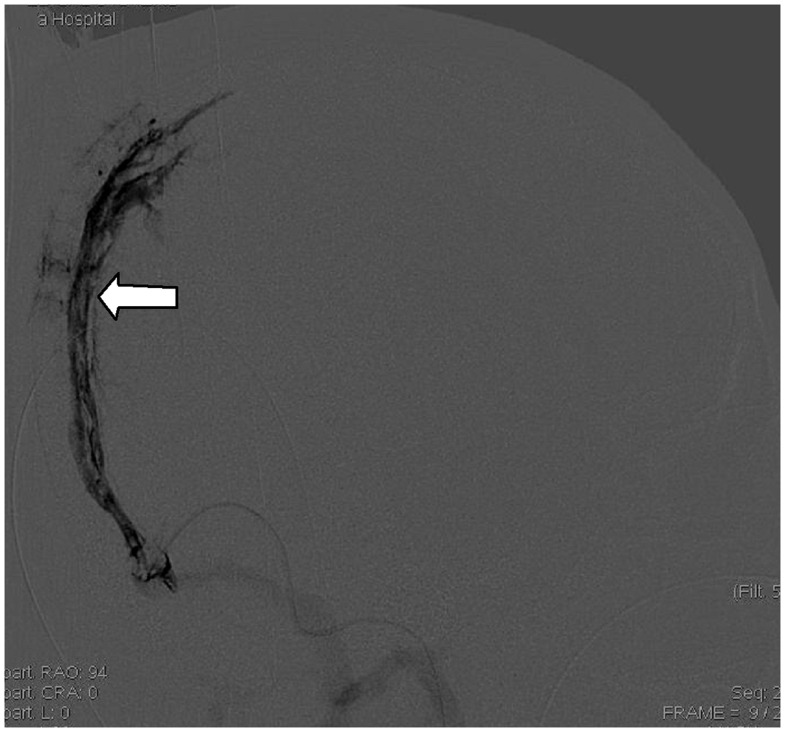
Figure 2.
Right ICA angiogram, lateral view, late venous phase, demonstrating the lack of parietal cortical veins, and complete occlusion of SSS, especially the posterior two-thirds of the SSS (white arrows).
One day later, a repeat angiogram showed no improved recanalization of the SSS and accordingly, he was referred for mechanical thrombectomy under general anesthesia. After venous guiding catheter and microcatheter were removed, the 0.054-in PS reperfusion catheter was then navigated over a 0.035-in guidewire to reach the right jugular bulb. Then, the 0.035-in guidewire was handled to enter through the thrombus in the right transverse sinus, and reached the left jugular bulb. The 0.054-in reperfusion catheter was pushed ahead under shoring of 0.035-in guidewire, and reached the right transverse sinus. The 0.035-in guidewire was exchanged for the 0.014-in microwire, and the 0.054-in reperfusion catheter was then navigated over the 0.014-in microwire through the thrombus into the posterior portion of the SSS. Lateral SSS venogram showed occlusion of the posterior two-thirds of the SSS (Figure 3). The separator was pushed into the anterior portion of the SSS. Advancing and withdrawing the separator through the reperfusion catheter continuously facilitated breaking up large pieces of clot. Mechanical thrombectomy was performed for over 30 minutes, resulting in amounts of liquefied and tremelloid clot aspirated (Figure 4). Venogram after treatment demonstrated reopening of the occlusion with some residual thrombosis (Figure 5). Four days later, repeat angiography was performed, which demonstrated total recanalization of the SSS (Figure 6). After the procedure, the same catheter was connected to the infusion pump providing a route for locally administered UK for three days. The patient’s neurological status normalized on postprocedure day 5 with the exception of 4/5 strength in the left leg.
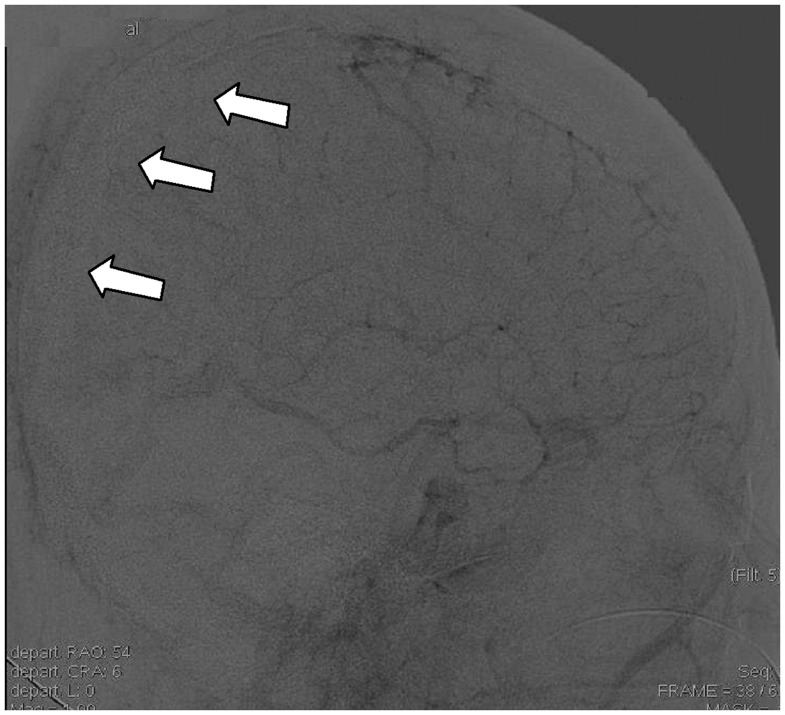
Figure 3.
Lateral superior sagittal sinus venogram showing occlusion of the posterior two-thirds of the SSS (white arrow) and 0.054-in Penumbra reperfusion catheter in the posterior SSS (black arrow).
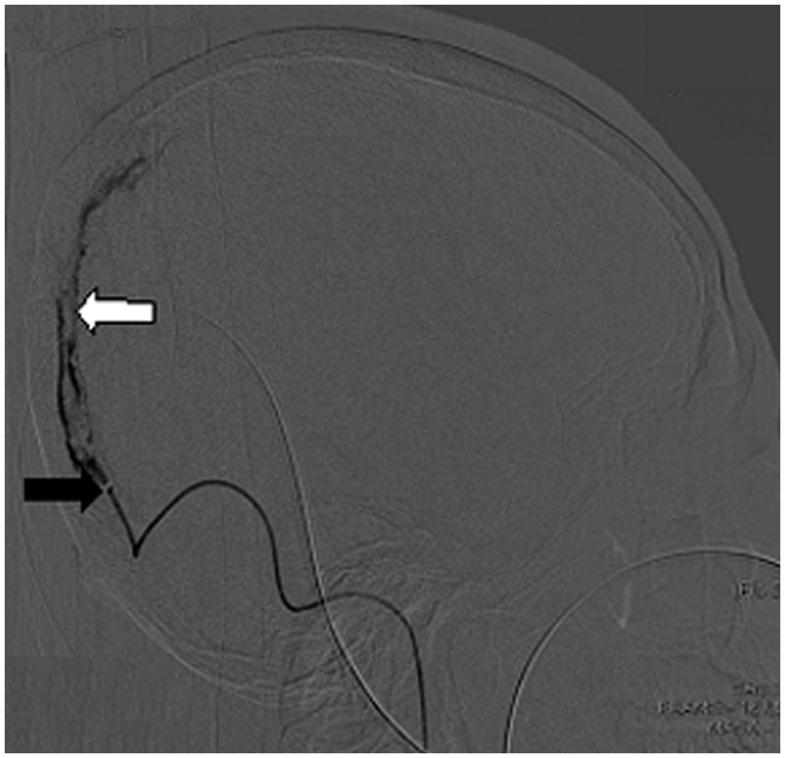
Figure 4.
Tremelloid and liquefied clot retrieved from the Penumbra reperfusion catheter.
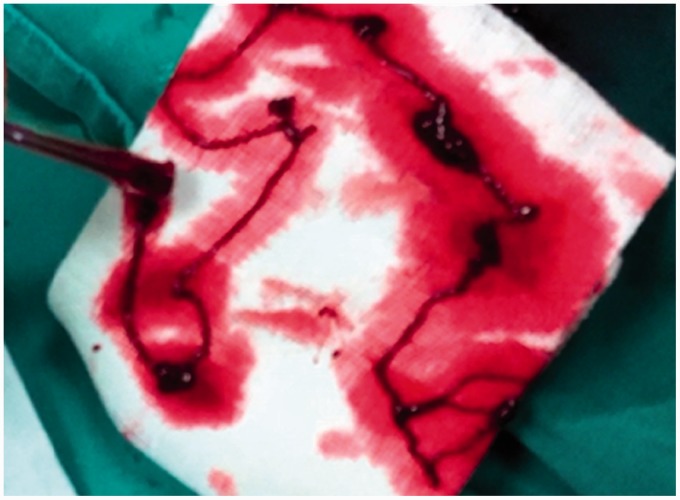
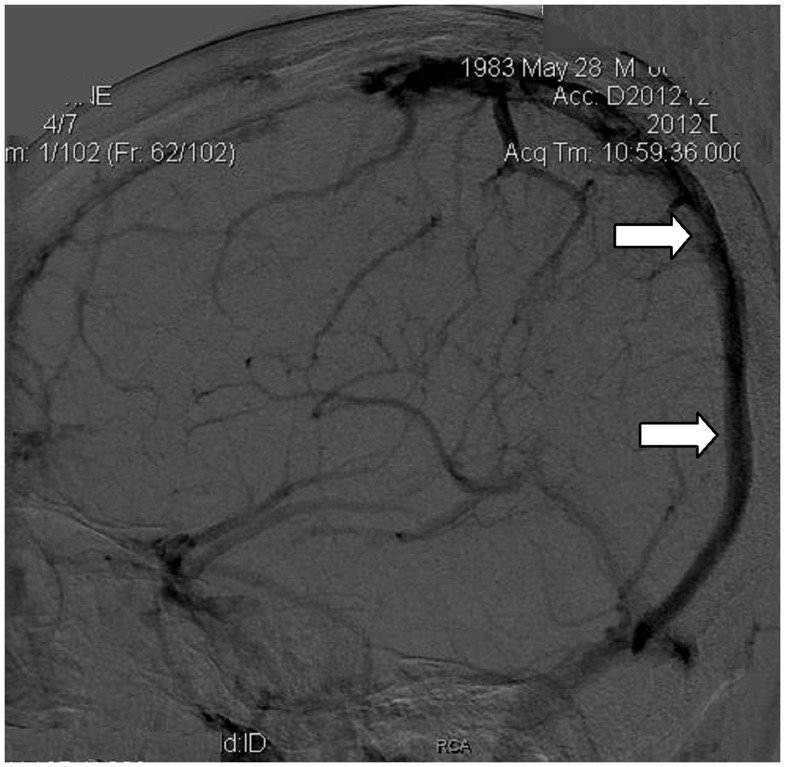
Figure 5.
Lateral superior sagittal sinus venogram after treatment with the Penumbra system showing reopening of the occlusion with some residual thrombosis (white arrow).
Figure 6.
Postprocedure left ICA-angiogram 4 days later, lateral view, late venous phase demonstrating patency of the SSS with satisfactory flow(white arrows).
Case 2
A 27-year-old woman presented to our hospital with ten-day history of progressively worsening headache and vomiting ten days after abortion. Neurological examination demonstrated paresis of the right limb. MRI and MRV demonstrated an infarction in the left frontal lobe and occlusion of the SSS (Figure 7). Continuous anticoagulation with subcutaneous low-molecular weight heparin for three days did not result in symptom control. Local infusion thrombolytic therapy with urokinase also failed to relieve her intractable headache. Due to the signs of impending uncal herniation with a dilated right pupil and change of consciousness, she was referred for endovascular mechanical thrombectomy.
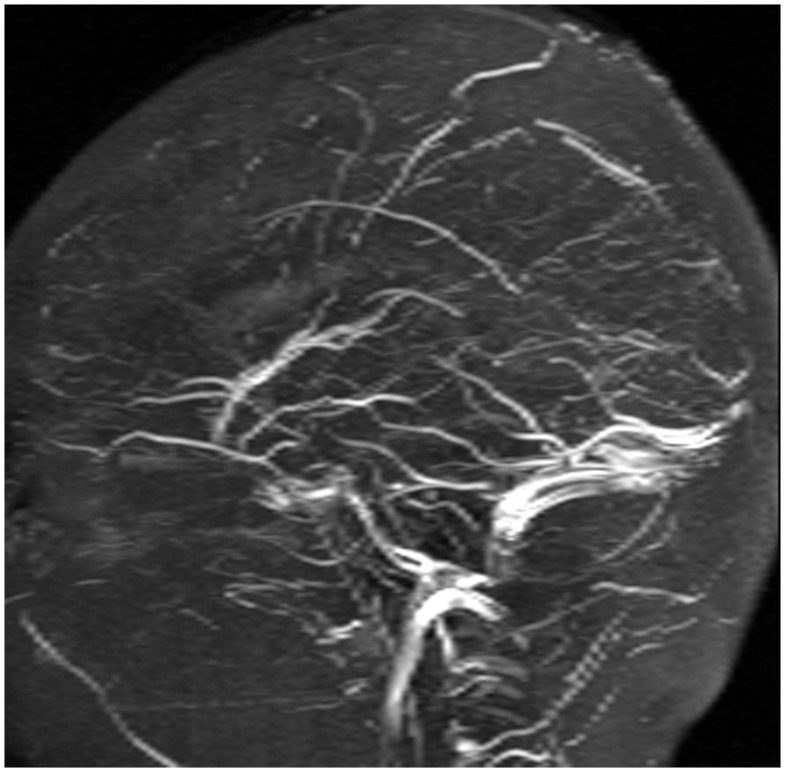
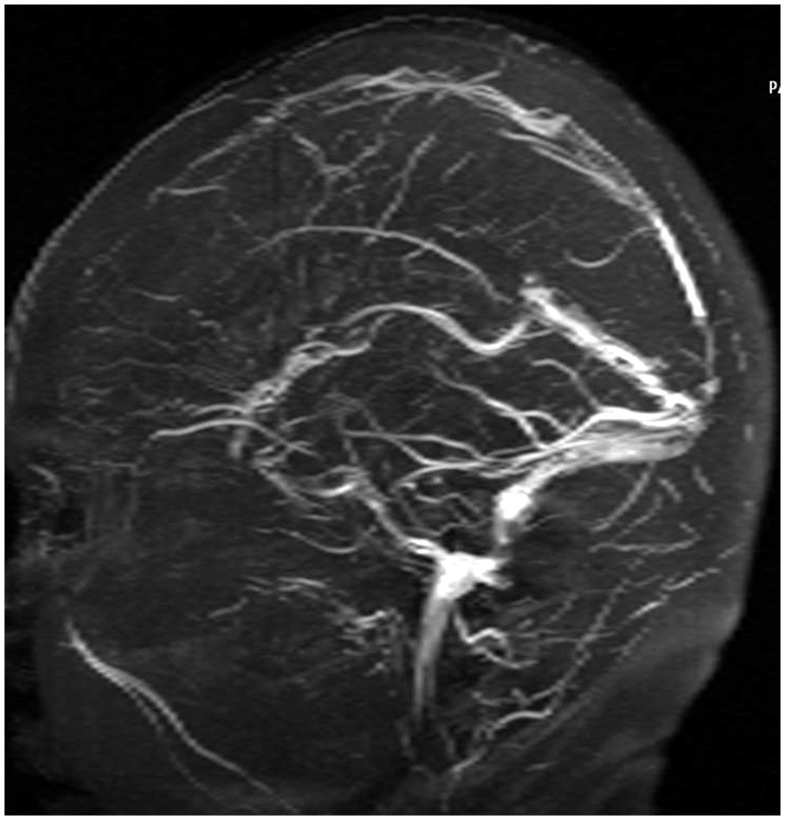
Figure 7.
Preprocedure MRV, demonstrating occlusion of the SSS.
Contrast material injections demonstrated complete occlusion of the SSS (Figure 8). The 0.041-in PS reperfusion catheter was then navigated over a 0.035-in guidewire to reach the right jugular bulb. The 0.035-in guidewire was exchanged for the 0.014-in microwire. The 0.041-in. reperfusion catheter was then navigated over the 0.014-in microwire through the thrombus into the posterior portion of the SSS. Mechanical thrombectomy was performed for over 30 minutes with to and fro movement of the separator through the reperfusion catheter, resulting in a small granular and solid clot aspirated. Repeat angiography demonstrated recanalization of a small part of the SSS. She remained on local infusion urokinase via reperfusion catheter after the procedure. The patient’s headache was relieved on post-procedure day 4, and MR venography (MRV) studies demonstrated subtotal recanalization of the SSS (Figure 9). The patient was doing well without any neurological symptoms and referred for outpatient follow-up.
Figure 8.
Left ICA angiogram after continuous anticoagulation with subcutaneous low-molecular weight heparin for 3 days, demonstrating complete occlusion of the SSS.
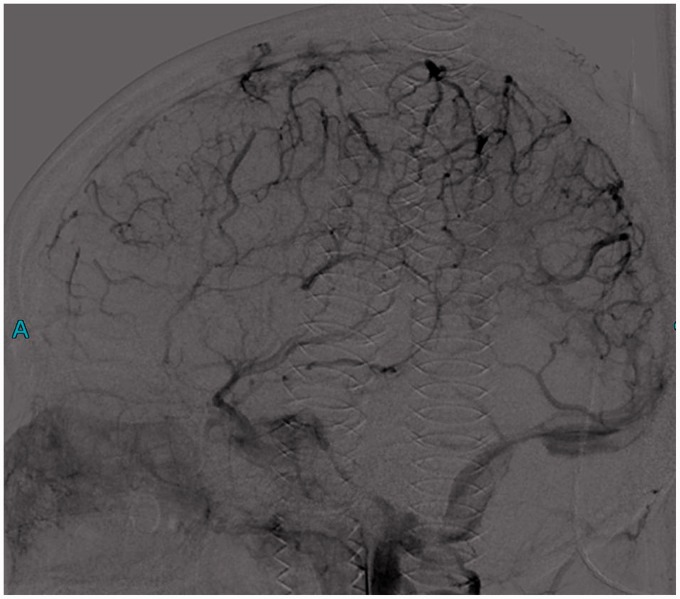
Figure 9.
Postprocedure day 4, MRV, demonstrating subtotal recanalization of the SSS.
Discussion
Cerebral venous sinus thrombosis (CVST) is an uncommon but potentially life-threatening condition.9 One large multicenter prospective observational study found an 8.3% overall mortality rate. Anticoagulation therapy has mostly been accepted to date for CVST, which may be efficient in 90% of cases.15 However, some researchers believe it may not be the best choice for each and every patient. When showing a malignant progression despite anticoagulant therapy, endovascular treatment might provide an ideal solution.
There are several different approaches to endovascular treatment of CVST, including transjugular and transfemoral approach. Transjugular endovascular treatment of CVST includes pharmacological thrombolysis and mechanical thrombectomy. In pharmacological thrombolysis, a microcatheter is advanced via a retrograde approach to the cerebral dural sinuses, and thrombolytic agents such as rt-PA or urokinase are administered as a bolus or with infusion over a period of time. Mechanical thrombectomy is done with different types of catheters, balloons, stents, or snares to disrupt the thrombus,6 such as AngioJet Rheolytic catheter, balloon angioplasty or stenting, microsnare, Fogarty embolectomy catheter balloon, etc.16--21 Theoretically, mechanical thrombectomy has an immediate recanalization effect, lowering intracranial pressure more promptly and facilitating pharmacological thrombolysis.22,23 Rheolytic thrombectomy utilizes the Venturi effect which creates a negative pressure fragmenting and aspirating the cerebral venous thrombus.24 Endovascular thrombolysis, with or without mechanical clot removal, may be beneficial for a subgroup of patients with CVST who have a poor prognosis despite treatment with heparin. Published experience with endovascular thrombolysis is promising, though based on case series and not on controlled trials.25
Recently, technological advances have yielded mechanical devices with improved handling properties and effectiveness for the treatment of acute cerebral vascular obstruction. The PS, a novel thrombectomy device specifically designed to remove the thrombus in acute ischemic stroke,2,26 proved to be an effective device for mechanical recanalization of CVST combined with local pharmacologic thrombolysis.
The PS is composed of two main components: a reperfusion catheter (0.054, 0.041, 0.032 and 0.026 in.) and a separator. Reperfusion catheters come with a relatively larger internal diameter and a distal end of greater flexibility, ensuring access to the target vessel. The separator provides an aspiration-debulking approach for recanalization, and is atraumatic to the vessel walls. Repeated to and fro movement of the separator is used to fragment the thrombus. Recently, some researchers attempted to make use of the PS in mechanical thrombectomy of CVST. Kulcsar et al. performed serial mechanical thrombectomies using the PS in combination with local infusion of urokinase to successfully recanalize a thrombosed SSS in a female patient.9 Siddiqui et al. and Blackham reported simultaneous use of the PS in conjunction with intrasinus rt-PA infusion for multifocal venous sinus thrombosis.10,11 Choulakian et al. described patients with CVST who underwent mechanical thrombectomy using the PS plus adjuvant balloon angioplasty, achieving satisfactory flow without the use of direct pharmacologic thrombolysis.12 Raychev et al. used the PS in combination with the Solitaire FR clot retrieval device to completely revascularize the occluded sinus.27 Direct thrombectomy using the PS without adjuvant local pharmacologic thrombolysis or additional mechanical interventions was detailed by Velat et al.13 Although the conclusions that the PS is helpful for recanalization of thrombosed venous sinus were drawn from previous reports, the methods they took were different (Table 1) such as whether to use adjuvant local pharmacologic thrombolysis and additional mechanical interventions or not, select tPA or urokinase as thrombolysis agent, select the 0.041-inch or 0.054-inch PS catheter as the reperfusion catheter, navigate guiding catheter into the transverse sinus or jugular bulb, as well as whether to use the guiding catheter or not.
Table 1.
Summary of case reports on the penumbra system for treatment of venous sinus thrombosis.
| Author | Year of report | No. of Cases | Adjuvant treatment | Size of Penumbra catheter | Location of guiding catheter | Outcome |
|---|---|---|---|---|---|---|
| Kulcsar et al9. | 2009 | 1 | Local thrombolysis with urokinase | 0.041-in | Right jugular bulb | Complete patency of SSS |
| Siddiqui et al. [10] | 2012 | 2 | Local thrombolysis with tPA | 0.054-in | Unknown | Remarkable clinical recovery |
| Blackham [11] | 2011 | 1 | Local thrombolysis with tPA | 0.041-in | Unknown | Complete resolution of the dural venous thrombus |
| Choulakian et al. [12] | 2010 | 4 | Three patients underwent balloon angioplasty | 0.041-in | Right transverse sinus | Neurologic improvement in all patients |
| Velat et al. [13] | 2011 | 1 | No use | 0.054-in | Left transverse sinus | Returned to work without additional seizures |
| Raychev et al. [27] | 2014 | 1 | Combined with Solitaire FR retrieval device | 0.054-in | Unknown | Excellent recovery |
| Our reports | 2014 | 2 | Local infusion of urokinase | 0.054-in (case 1), 0.041-in (case 2) | No use | Patency of SSS, Patient’s neurological status normalized |
We first report here two cases successfully treated using the PS for mechanical venous sinus thrombectomy with adjuvant local infusion of urokinase in Asia. The technique of the treatment we adopted was also not the same as those of above reports. In order to reduce the danger of damaging and perforating the venous sinus, we successfully introduced the PS reperfusion catheter into the posterior portion of the SSS, without using a guiding catheter in the transverse sinus, which has not been reported previously. We also found that when the guiding catheter was placed in the jugular bulb, it was difficult for the PS reperfusion catheter to reach the SSS because it is only about 40 cm longer than the guiding catheter. Therefore, we believe that if the reperfusion catheter is designed longer, it would be more suitable to recanalize thrombosed venous sinuses. In addition, we compared the recanalization effect of the 0.054-inch reperfusion catheter with that of the 0.041-inch. The 0.054-inch catheter with a larger separator allows for stronger fragmentation and aspiration of thrombus, and more rapid and complete sinus recanalization, although it was more difficult to handle through the intracranial venous sinus.
Conclusions
The Penumbra System proved to be effective in the rapid recanalization of cerebral venous sinus thrombosis, however, there exists a diversity in treatment techniques. The solution to these problems depends on more clinical trials as well as further improvement of devices.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (No.81000596) and Postdoctoral Science Foundation of China (No. 2013M531815).
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med 2005; 352: 1791–1798. doi: 10.1056/NEJMra042354. [DOI] [PubMed] [Google Scholar]
- 2.Filippidis A, Kapsalaki E, Patramani G, et al. Cerebral venous sinus thrombosis: review of the demographics, pathophysiology, current diagnosis, and treatment. Neurosurg Focus. 2009; 27: E3 doi: 10.3171/2009.8.FOCUS09167. [DOI] [PubMed] [Google Scholar]
- 3.Schultz DW, Davis SM, Tress BM, et al. Recanalisation and outcome cerebral venous thrombosis. J Clin Neurosci. 1996; 3: 133–138. doi: 10.1016/S0967-5868(96)90006-5. [DOI] [PubMed] [Google Scholar]
- 4.Wasay M, Bakshi R, Kojan S, et al. Nonrandomized comparison of local urokinase thrombolysis versus systemic heparin anticoagulation for superior sagittal sinus thrombosis. Stroke. 2001; 32: 2310–2317. doi: 10.1161/hs1001.096192. [DOI] [PubMed] [Google Scholar]
- 5.Borhani Haghighi A, Mahmoodi M, Edgell RC, et al. Mechanical thrombectomy for cerebral venous sinus thrombosis: A Comprehensive Literature Review. Clin Appl Thromb Hemost. 2013; 20(5): 507–515. [Epub ahead of print]doi: 10.1177/1076029612470968. [DOI] [PubMed] [Google Scholar]
- 6.Baker MD, Opatowsky MJ, Wilson JA, et al. Rheolytic catheter and thrombolysis of dural venous sinus thrombosis: a case series. Neurosurgery. 2001; 48: 487–493. doi: 10.1097/00006123-200103000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Caso V, Billeci AM, Leys D. Interventional neuroradiology in the treatment of cerebral venous thrombosis. Front Neurol Neurosci 2008; 23: 144–160. [DOI] [PubMed] [Google Scholar]
- 8.Renowden S. Cerebral venous thrombosis: local thrombolysis. J R Soc Med 2000; 93: 241–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kulcsár Z, Marosfoi M, Berentei Z, et al. Continuous thrombolysis and repeated thrombectomy with the Penumbra System™ in a child with hemorrhagic sinus thrombosis: technical note. Acta Neurochir (Wien). 2010; 152: 911–916. doi: 10.1007/s00701-009-0570-4. [DOI] [PubMed] [Google Scholar]
- 10.Siddiqui FM, Pride GL, Lee JD. Use of the Penumbra system 054 plus low dose thrombolytic infusion for multifocal venous sinus thrombosis. A report of two cases. Interv Neuroradiol 2012; 18: 314–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blackham KA. Extensive dural sinus thrombosis: successful recanalization with thrombolysis and a novel thrombectomy device. J Neurosurg. 2011; 114(1): 133–135. doi: 10.3171/2010.2.JNS091186. [DOI] [PubMed] [Google Scholar]
- 12.Choulakian A, Alexander MJ. Mechanical thrombectomy with the penumbra system for treatment of venous sinus thrombosis. J Neuro Intervent Surg 2010; 2: 153–156. [DOI] [PubMed] [Google Scholar]
- 13.Velat GJ, Skowlund CJ, Waters MF, et al. Direct thrombectomy using the Penumbra thromboaspiration catheter for the treatment of cerebral venous sinus thrombosis. World Neurosurg 2012; 77: 591.e15–8. [DOI] [PubMed] [Google Scholar]
- 14.Bose A, Henkes H, Alfke K, et al. The Penumbra System: a mechanical device for the treatment of acute stroke due to thromboembolism. Am J Neuroradiol. 2008; 29: 1409–1413. doi: 10.3174/ajnr.A1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferro JM, Canhão P, Stam J, et al. ISCVT Investigators.Prognosis of cerebral vein and dural sinus thrombosis: results of the international study on cerebral vein and dural sinus thrombosis (ISCVT). Stroke. 2004; 35: 664–670. doi: 10.1161/01.STR.0000117571.76197.26. [DOI] [PubMed] [Google Scholar]
- 16.Soleau SW, Schmidt R, Stevens S, et al. Extensive experience with dural sinus thrombosis. Neurosurgery. 2003; 52: 534–544. doi: 10.1227/01.NEU.0000047815.21786.C1. [DOI] [PubMed] [Google Scholar]
- 17.Baker MD, Opatowsky MJ, Wilson JA, et al. Rheolytic catheter and thrombolysis of dural venous sinus thrombosis: a case series. Neurosurgery. 2001; 48: 487–494. doi: 10.1097/00006123-200103000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Curtin KR, Shaibani A, Resnick SA, et al. Rheolytic catheter thrombectomy, balloon angioplasty, and direct recombinant tissue plasminogen activator thrombolysis of dural sinus thrombosis with preexisting hemorrhagic infarctions. Am J Neuroradiol 2004; 25: 1807–1811. [PMC free article] [PubMed] [Google Scholar]
- 19.Kirsch J, Rasmussen PA, Masaryk TJ, et al. Adjunctive rheolytic thrombectomy for central venous sinus thrombosis: technical case report. Neurosurgery. 2007; 60: E577–578. doi: 10.1227/01.NEU.0000255339.26027.68. [DOI] [PubMed] [Google Scholar]
- 20.Zhang A, Collinson RL, Hurst RW, et al. Rheolytic thrombectomy for cerebral sinus thrombosis. Neurocrit Care. 2008; 9: 17–26. doi: 10.1007/s12028-008-9058-y. [DOI] [PubMed] [Google Scholar]
- 21.Khan SH, Adeoye O, Abruzzo TA, et al. Intracranial dural sinus thrombosis: novel use of a mechanical thrombectomy catheter and review of management strategies. Clin Med Res. 2009; 7: 157–165. doi: 10.3121/cmr.2009.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bishop FS, Finn MA, Samuelson M, et al. Endovascular balloon angioplasty for treatment of posttraumatic venous sinus thrombosis. Case report. J Neurosurgery. 2009; 111: 17–21. doi: 10.3171/2009.2.JNS08491. [DOI] [PubMed] [Google Scholar]
- 23.Barnwell SL, Clark WM, Nguyen TT, et al. Safety and efficacy of delayed intraarterial urokinase therapy with mechanical clot disruption for thromboembolic stroke. Am J Neuroradiol 1994; 15: 1817–1822. [PMC free article] [PubMed] [Google Scholar]
- 24.Caso V, Billeci AM, Leys D. Interventional neuroradiology in the treatment of cerebral venous thrombosis. Front Neurol Neurosci 2008; 23: 144–160. [DOI] [PubMed] [Google Scholar]
- 25.Coutinho JM1, Ferro JM, Zuurbier SM, et al. Thrombolysis or anticoagulation for cerebral venous thrombosis: rationale and design of the TO-ACT trial. Int J Stroke. 2013; 8: 135–140. doi: 10.1111/j.1747-4949.2011.00753.x. [DOI] [PubMed] [Google Scholar]
- 26.Psychogios MN, Kreusch A, Wasser K, et al. Recanalization of large intracranial vessels using the Penumbra System: A single-center experience. Am J Neuroradiol. 2012; 33: 1488–1493. doi: 10.3174/ajnr.A2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raychev R, Tateshima S, Rastogi S, et al. Successful treatment of extensive cerebral venous sinus thrombosis using a combined approach with Penumbra aspiration system and Solitaire FR retrieval device. J Neurointerv Surg. 2014; 6(5): e32 doi: 10.1136/neurintsurg-2013-010866.rep. [DOI] [PubMed] [Google Scholar]