Abstract
Cocaine is a widespread recreational drug that has the potential to induce neurological vascular diseases, including ischaemic and haemorrhagic stroke. Although arterial vasospasm has been suggested as a pathogenic factor in the development of neurovascular complications, it remains unclear whether cocaine users carry an increased risk to suffer iatrogenic vasospasm during endovascular procedures. We report the case of two patients with a history of cocaine abuse, who developed unusual severe vasospasms during different interventional procedures. The first case occurred in a middle-aged woman with an unruptured left internal carotid artery bifurcation aneurysm who was scheduled for treatment by remodelling assisted coiling. Just after the placement of the remodelling balloon, a severe occlusive vasospasm interrupted the procedure. The second case happened to a 46-year-old man with a non-aneurysmal subarachnoid haemorrhage and a symptomatic vasospasm in the right-sided anterior circulation who developed another occlusive vasospasm after the first attempt at transluminal balloon angioplasty. Further research is needed to establish a relation between cocaine use and increased risk of iatrogenic vasospasm in endovascular procedures, but we suggest practitioners be extremely cautious when treating this subgroup of patients.
Keywords: Cocaine, vasospasm, endovascular treatment, stroke
Introduction
Iatrogenic vasospasm is a common event in neurointerventional procedures triggered by contact of the catheterization material with the endothelium of the vessel, ensuing in a transient vessel narrowing which usually resolves easily once the stimuli is halted. Although additional measures, like vasodilator drugs, may occasionally be required to restore the vessel’s original shape, they are very rarely the cause of a major complication.
However, it remains unclear what factors, other than mechanical, could make patients more predisposed to suffer iatrogenic vasospasm.
Cocaine is a potent central nervous system sympathomimetic drug, which blocks the pre-synaptic nerve terminals inhibiting the reuptake of noradrenalin, serotonin and dopamine, with the potential to induce ischaemic and haemorrhagic stroke. Several mechanisms have been involved, such as vasospasm, cerebral vasculitis, enhanced platelet aggregation, and hypertensive peaks with altered cerebral autoregulation.1 Cocaine-induced vasospasm has been described in this subgroup of patients by means of digital subtraction angiography (DSA).2 Enhancement of dopamine levels at certain brain areas has been established as the main cause of vasospasm with blood flow reduction in patients with cocaine-related stroke.3 Nonetheless, a predisposition of cocaine users to develop neurointerventional procedure-related vasospasms is not well established in the literature.
We describe the cases of two consecutive patients with a common history of chronic cocaine abuse, who developed severe life-threatening iatrogenic vasospasm during endovascular procedures.
Case 1
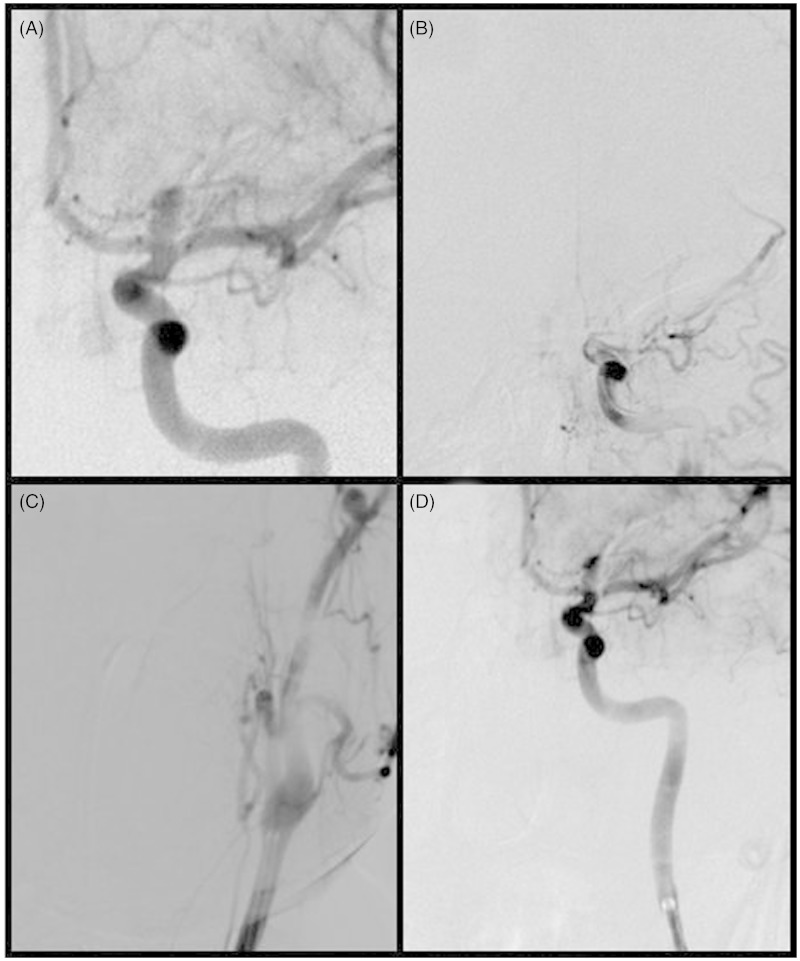
The first case occurred in a 41-year-old woman with a medical history of hypertension, dyslipidaemia and chronic cocaine abuse, who was diagnosed with a non-ruptured aneurysm in the left internal carotid artery (ICA) bifurcation, while admitted to our hospital with a left middle cerebral artery (MCA) minor ischaemic stroke. Remodelling assisted coiling was scheduled once the patient fully recovered a month later. Once the remodelling balloon was placed in the MCA, complete occlusion of the ICA with signs of vasospasm was detected. Combined venous and intra-arterial infusion of nimodipine was used, followed by gradual retrieval of the catheters. The vasospasm did not resolve until the guide catheter was fully removed from the common carotid artery (CCA). Subsequent control angiographic runs showed no rupture of the aneurysm or other complications, and the treatment was concluded without aneurysm embolization due to safety concerns (Figure 1). The patient did not suffer clinical or radiological complications (follow-up CT scan and MRI excluded haemorrhage or infarction).
Figure 1.
A) Basal DSA run shows a saccular aneurysm at the left ICA bifurcation. B) Severe vasospasm following the placement of the remodelling balloon in the left MCA. C) The guide-catheter run shows vasospasm comprising the origin of the left ICA. D) The final DSA run demonstrates resolution of the vasospasm after complete retrieval of the guide catheter from the CCA.
Case 2
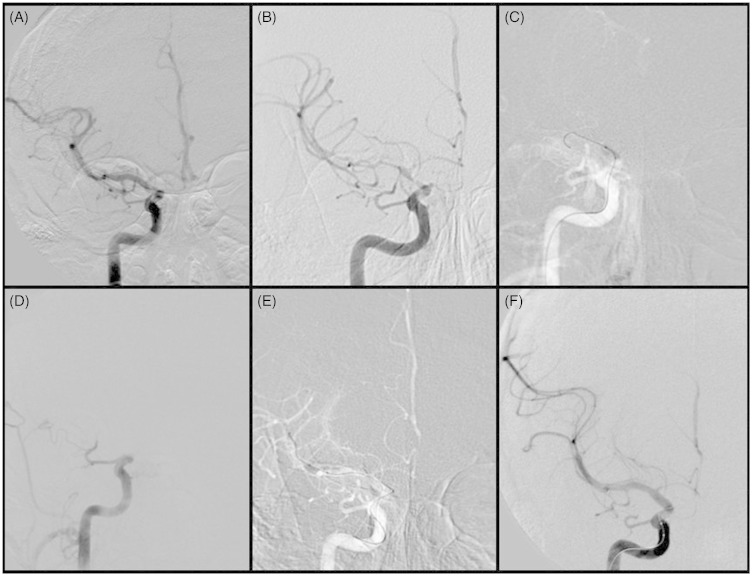
The second case occurred in a 46-year-old male smoker and sporadic cocaine abuser, with a medical history of paroxysmal atrial fibrillation with no medical treatment, who was admitted into our institution due to a subarachnoid haemorrhage (SAH) Fisher II, Hunt-Hess II. Urgent initial acute angiographic examination was normal. IV nimodipine was started right after SAH diagnosis was established. Nevertheless, seven days later symptomatic vasospasm was suspected as the patient developed mild left-sided hemiparesis, thus urgent endovascular treatment was initiated according to our institutional protocol. Severe vasospasm affecting the right-sided intracranial anterior circulation was diagnosed. In order to perform transluminal balloon angioplasty (TBA), a microguidewire was smoothly placed into the MCA, immediately after which, a complete ICA/MCA occlusion was observed. While using vasodilator drugs, multiple attempts with TBA were required to resolve the vasospasm (Figure 2). After the procedure the patient improved completely, although the follow-up MRI showed a right MCA acute infarction.
Figure 2.
A) Urgent cerebral angiogram shows normal intracranial vessels anatomy. B) Study repeated seven days after development of left-sided mild hemiparesis shows moderate to severe vasospasms comprising the distal segment of the right ICA and M1 and M2 segments of the right MCA. C) Road mapping fluoroscopic snapshot during balloon angioplasty in the distal segment of the ICA. D) Severe iatrogenic occlusive vasospasm of the ICA following initial TBA. E) Subsequent TBAs in the occluded segments were performed accompanied with vasodilator drugs infusion. F) Final DSA after multiple TBA attempts demonstrated complete restoration of the vessel caliber and blood flow.
Discussion
Cocaine is a widespread recreational drug with potent neurostimulant effects. Its use has been associated with an increased risk of brain infarction, intracerebral haemorrhage and aneurysmal subarachnoid haemorrhage (aSAH). One of the main mechanisms of cocaine-induced brain ischemia is a predisposition to vasospasm, probably due to an increase in extracellular dopamine level,1 however its role in patients with cocaine-associated aSAH is not clear. Besides being younger than controls, patients with cocaine-associated aSAH have a higher proportion of anterior circulation aneurysms.4 Thus, results regarding the incidence of aSAH-related vasospasm and the clinical outcome in this subgroup of patients are contradictory. While Conway et al. described a higher risk of symptomatic vasospasm with no significant difference in the prognosis,4 Chang et al. found a higher risk of aneurysm re-rupture and in-hospital mortality with no significant risk of symptomatic vasospasm.5 Moreover, another study could not find a higher risk of vasospasm or a worse clinical outcome in these patients.6 However the rate of endovascular periprocedural complications among this population remains unexplored. Despite the lack of data on this question, we hypothesize that chronic exposure to cocaine may induce vessel wall hyper-reactivity, which could make this population prone to suffering vasospasm-mediated complications during endovascular procedures.
Conclusion
Further research is needed to establish a significant predisposition in cocaine users to develop iatrogenic vasospasms during endovascular interventions. Until this question is answered, and taking our experience into account, we recommend practitioners be especially cautious when treating these patients, considering the least aggressive techniques for their interventions, such as intra-arterial vasodilator drugs for vasospasm or simple coiling without remodelling balloon or stent for aneurysm embolization when possible.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Treadwell SD, Robinson TG. Cocaine use and stroke. Postgrad Med J 2007; 83(980): 389–394doi: 10.1136/pgmj.2006.055970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacobs IG, Roszler MH, Kelly JK, et al. Cocaine abuse neurovascular complications. Radiology 1989; 170(1 Pt 1): 223–227. [DOI] [PubMed] [Google Scholar]
- 3.Johnson B, Lamki L, Fang B, et al. Demonstration of dose-dependent global and regional cocaine-induced reductions in brain blood flow using a novel approach to quantitative single photon emission computerized tomography. Neuropsychopharmacology 1998; 18(5): 377–384doi: 10.1016/S0893-133X(97)00168-1. [DOI] [PubMed] [Google Scholar]
- 4.Conway JE, Tamargo RJ. Cocaine use is an independent risk factor for cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Stroke 2001; 32(10): 2338–2343doi: 10.1161/hs1001.097041. [DOI] [PubMed] [Google Scholar]
- 5.Chang TR, Kowalski RG, Caserta F, et al. Impact of acute cocaine use on aneurysmal subarachnoid hemorrhage. Stroke 2013; 44(7): 1825–1829doi: 10.1161/STROKEAHA.111.000749. [DOI] [PubMed] [Google Scholar]
- 6.Alaraj A, Wallace A, Mander N, et al. Effect of acute cocaine use on vasospasm and outcome in aneurysmal subarachnoid hemorrhage. World Neurosurg 2010; 73(4): 357–60doi: 10.1016/j.wneu.2010.01.011. [DOI] [PubMed] [Google Scholar]