Abstract
Spondylodiscitis is a rare complication of unwitnessed button battery ingestion in children. We report a case of a 20-month-old girl who presented to the emergency room 2 weeks after endoscopic removal of unwitnessed, impacted esophageal battery. Delayed presentation of spondylodiscitis after foreign body removal is related to local injury, pressure necrosis, and perforation. The bilaminar shape of an unknown ingested foreign body should alert the treating physician that it might be a battery rather than a coin. Prompt evaluation with magnetic resonance imaging is essential to prevent neurological deficit and/or spinal deformities.
Keywords: Spondylodiscitis, button battery ingestion, children, magnetic resonance imaging
Introduction
Foreign body ingestion occurs frequently in children younger than six years of age, with the peak between one and two years of age.1 While coin ingestion is the most common foreign body, battery ingestion in children has become more frequent recently, due to increasing use of electronic devices and its attractive shiny appearance.2 A chest radiograph with AP and lateral views including the nasopharynx superiorly is the first-line investigation of choice for suspected battery ingestion. There is a small risk (0.7%) of the battery being retained in the esophagus.2 Button battery retention in the esophagus even for a few hours can lead to burns and/or perforation, therefore emergent removal by endoscopy is indicated.3 Spondylodiscitis is a rare complication of button battery ingestion. Magnetic resonance imaging (MRI) is the investigation of choice to evaluate for spondylodiscitis. Early diagnosis and prompt treatment are essential to prevent neurological deficits and/or spinal deformities. In this paper, we present a 20-month-old girl with a delayed presentation of spondylodiscitis following endoscopic removal of a button battery and review the literature regarding prompt utilization of MRI.
Case presentation
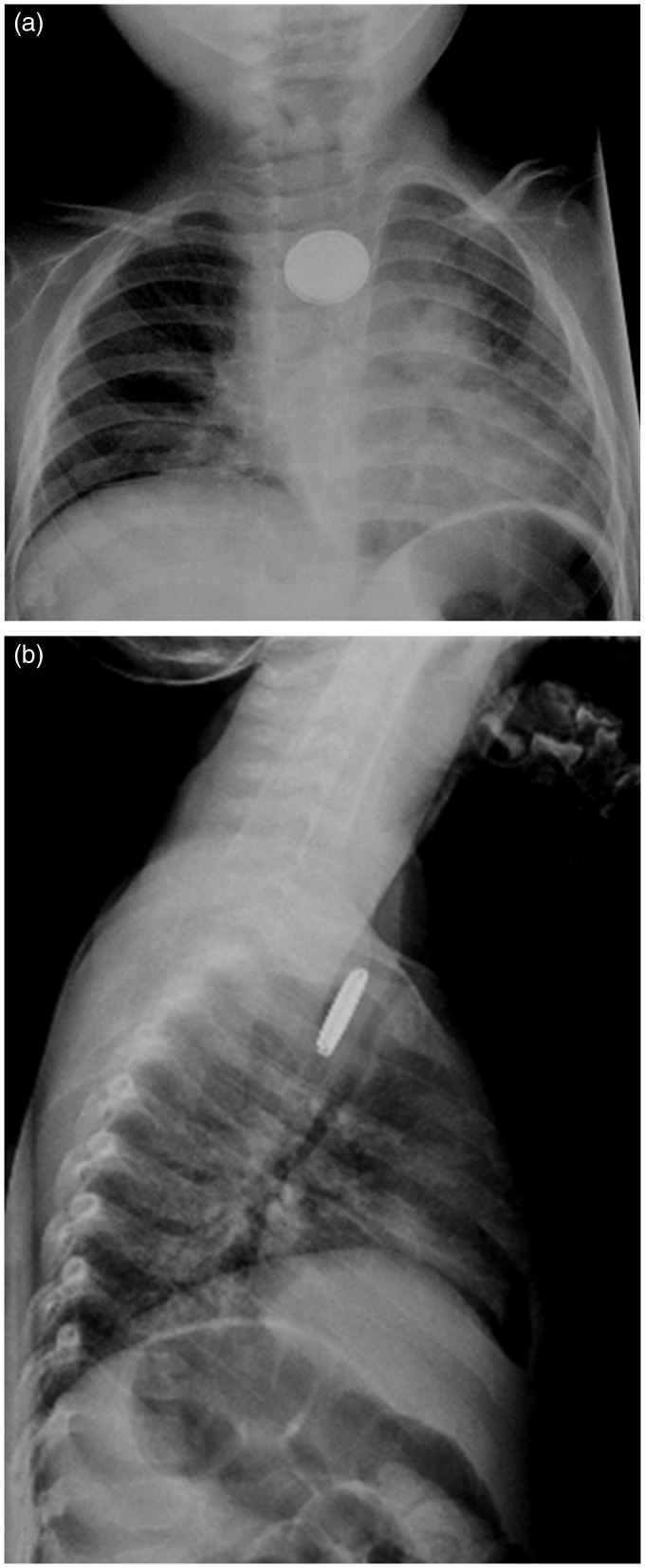
A 20-month-old girl, otherwise healthy, without witnessed foreign body ingestion presented to the emergency room with a one week history of cough and fever. She was being treated with amoxicillin for a suspected pneumonia. Chest radiograph revealed a 20 mm rounded, radiodense object with a bilaminar disk appearance at the thoracic inlet consistent with a button battery (Figure 1(a) and (b)). Emergent rigid esophagoscopy was performed to remove the button battery. At the time of removal, there was significant coagulative necrosis in the esophagus at the foreign body site. On direct inspection, there was no evidence of full-thickness injury, perforation, or massive hemorrhage. On postoperative day 1, an esophagram showed no evidence of a leak. Patient was discharged on postoperative day 4 in good condition.
Figure 1.
(a) Frontal and (b) Lateral chest radiographs demonstrate a round radio-dense foreign body with a bilaminar structure consistent with an ingested button battery just below the thoracic inlet.
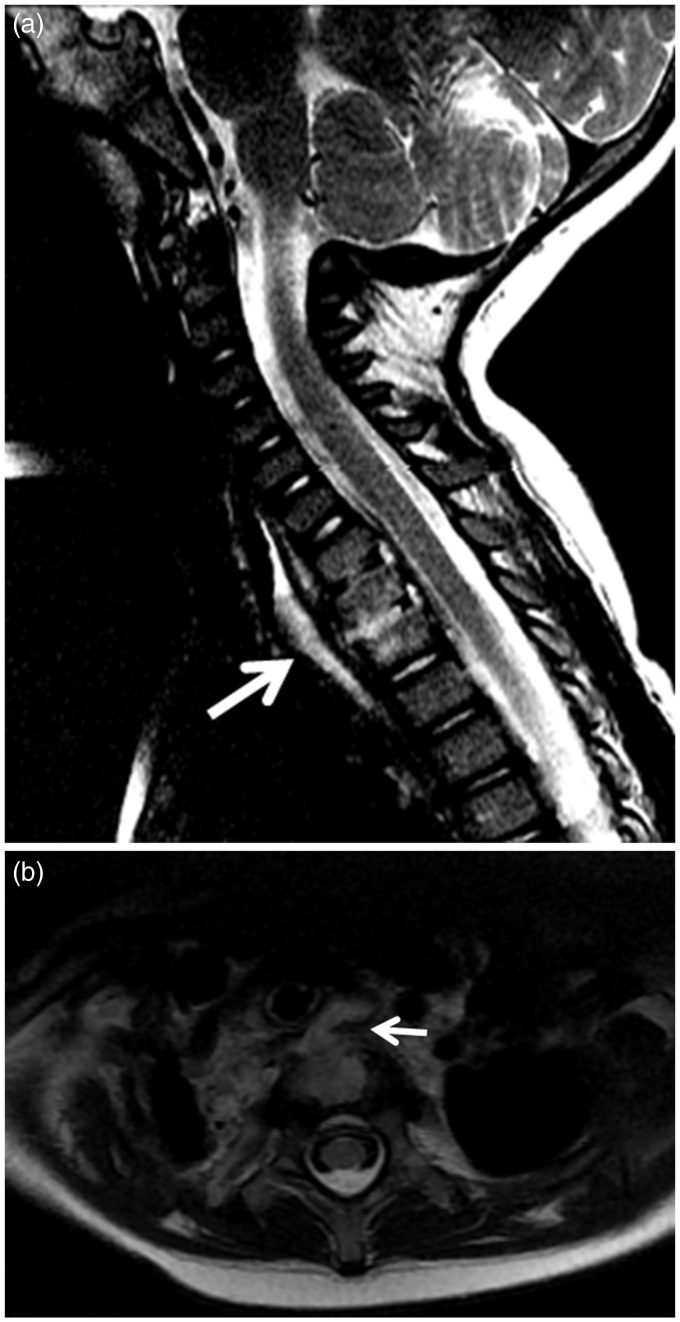
Two weeks following discharge, the patient became irritable at night and was only comfortable sitting upright. She had been complaining of neck pain that was minimally responsive to ibuprofen, restricted movement of the neck, and tenderness on palpation. She was readmitted to the emergency room and underwent further laboratory studies. Her studies showed: white blood cell count 15,870 cells/µL (differential: neutrophil 29% and lymphocytes 57%), hemoglobin concentration 11.4 g/dL, mean corpuscular volume of 82.9 fL, platelet count 474,000 cells/µL. The erythrocyte sedimentation rate was 34 mm/h (reference range, 0–10 mm/h), and the C-reactive protein was 0.4 mg/dL. Given the clinical findings/history and laboratory data, MRI of the neck and cervicothoracic spine was performed that showed classic neuroimaging findings of spondylodiscitis (Figure 2(a) and (b)). Evaluation of the mediastinal structures within the MRI field of view did not show evidence of mediastinitis. A repeat esophagram was not performed. She was placed on long-term intravenous ampicillin/sulbactam for 6 weeks. Follow-up MRI at 4 weeks and 12 weeks showed resolution of abnormal signal, contrast enhancement, and phlegmon.
Figure 2.
(a) Sagittal T2-weighted MR image demonstrates loss of normal marrow signal with hyperintensity of C7, T1, and T2 vertebral bodies compatible with bone marrow edema; T2-hyperintense signal involving T1/T2, greater than C7/T1 intervertebral discs, consistent with discitis; phlegmon is shown in the prevertebral space (arrow). (b) Axial T2-weighted MRI demonstrates contiguous inflammation and communication of the perforated esophagus and vertebral body (arrow).
Discussion
In children less than 5 years of age, ingestion of batteries with a diameter of 20 mm or larger may be complicated by esophageal impaction, which can cause local esophageal damage.4 Local injury in the esophagus from impaction may be secondary to any combination of the following: (1) caustic injury from alkali leakage, (2) pressure necrosis, (3) absorption of toxic substances, and (4) electrical discharge from the cathode to anode, which can produce mucosal burns.3 The complications resulting from battery ingestion and esophageal impaction are rare. The complications include esophageal perforation, esophageal stenosis requiring repeated dilation, fistula formation, esophageal strictures, esophageal scarring, vocal cord paralysis from recurrent laryngeal nerve damage, tracheal stenosis or tracheomalacia, aspiration pneumonia, empyema, lung abscess, tracheoesophageal fistula, and death.2 Spondylodiscitis is a rare complication associated with a delayed clinical presentation following endoscopic removal of the battery.
Spondylodiscitis is an infection of an intervertebral disc and the two adjacent vertebrae. Spondylodiscitis is rare in children. It may be secondary to hematogenous spread (most common due to vascularized discs), direct introduction (iatrogenic) or contiguous contamination. Local mucosal injury from caustic burns and/or esophageal microperforation may act as a port of entry of contiguous spread of infection in children with battery ingestion. The clinical symptoms are variable and often non-specific, which may delay the diagnosis.5 As in our patient, a stiff neck or dysphagia may be the presenting symptom secondary to the involvement of the cervicothoracic spine.
MRI is the test of choice in evaluating for spondylodiscitis in children. Radiography has a limited role due to its low soft tissue resolution and consequent low sensitivity and specificity. The typical MRI findings in spondylodiscitis includes: (1) T2 hyperintense signal of the intervertebral disc reflecting discitis, (2) T1 postcontrast enhancement of the intervertebral disc, (3) T1 hypointense and T2 hyperintense marrow signal of the adjacent vertebral end plates consistent with inflammatory edema, (4) T1 postcontrast enhancement of the adjacent vertebral end plates, and (5) T2 hyperintense soft tissue signal with enhancement along the anterior and/or lateral contour of the vertebral column consistent with inflammatory phlegmon. Phlegmon may evolve into an abscess and demonstrate peripheral enhancement post gadolinium.
To the best of our knowledge, five cases of battery ingestion related spondylodiscitis have been reported in the literature.6–10 Table 1 summarizes the age of the patient, size of button battery, time of MRI in relation to removal, and salient clinical findings. The reported five cases in the literature and our patient had a unique presentation of unwitnessed foreign body ingestion. Furthermore, this emphasizes the morbidity related to prolonged exposure to a lodged button battery in the esophagus. The diagnosis of esophageal impaction was made in all cases using a radiograph. MRI was performed between 1 and 6 weeks after removal of impacted esophageal button battery in our patient and in the reported literature. Neck pain, stiffness, extension, and tenderness were the key clinical findings as shown in Table 1. All the patients, including ours, were subsequently managed with long-term IV antibiotics. MRI findings were localized to the C7–T3 region, consistent with common sites of esophageal impaction at the cricopharyngeus muscle (C7) and level of aortic arch (T3).
Table 1.
Demographic data, clinical signs, battery size, and timing of MRI.
| Reference (year) | Age in months | Battery size in mm | MRI timing after removal | Clinical presentation |
|---|---|---|---|---|
| This article (2015) | 20 | 20 | 2 weeks | Neck pain, restricted movement, tenderness |
| Kieu et al.10 (2014) | 14 | 20 | 1 week | Neck hyperextension, inspiratory stridor |
| Eshaghi et al.9 (2013) | 10 | NS | 4 weeks | Neck hyperextension, resistance to passive movement |
| Jarugula and Dorofaeff8 (2011) | 5 | 12.4 | 2 weeks | Noisy breathing, difficulty feeding |
| Tan et al.7 (2011) | 14 | 20 | 4 weeks | Restricted movement, neck tenderness |
| Sudhakar et al.6 (2008) | 18 | NS | 6 weeks | Neck pain, stiffness, restricted movement |
NS, not specified.
Spondylodiscitis is a rare complication associated with a delayed endoscopic removal of an impacted button battery in the esophagus of children. In the clinical scenario of an unwitnessed battery ingestion and status post endoscopic removal, it is imperative to be aware of this potential complication, which typically occurs between 1 and 6 weeks after ingestion. Early diagnosis and prompt treatment of spondylodiscitis are essential to prevent neurological deficits and/or spinal deformities. The clinical presentation in our patient and recent literature demonstrate the importance of evaluating the spine utilizing MRI in children with unwitnessed battery ingestion after removal. In addition, the shape of the foreign body with the characteristic bilaminar appearance, denser outer rim, and step-off at the edge help differentiating a battery from a typical coin.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
None declared.
References
- 1.Litovitz T, Whitaker N, Clark L. Preventing battery ingestions: an analysis of 8648 cases. Pediatrics 2010; 125: 1178–1183. [DOI] [PubMed] [Google Scholar]
- 2.Litovitz T, Schmitz BF. Ingestion of cylindrical and button batteries: an analysis of 2382 cases. Pediatrics 1992; 89: 747–757. [PubMed] [Google Scholar]
- 3.Samad L, Ali M, Ramzi H. Button battery ingestion: hazards of esophageal impaction. J Pediatr Surg 1999; 34: 1527–1531. [DOI] [PubMed] [Google Scholar]
- 4.Marom T, Goldfarb A, Russo E, et al. Battery ingestion in children. Int J Pediatr Otorhinolaryngol 2010; 74: 849–854. [DOI] [PubMed] [Google Scholar]
- 5.Fucs PM, Meves R, Yamada HH. Spinal infections in children: a review. Int Orthop 2012; 36: 387–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sudhakar PJ, Al Dossary J, Malik N. Spondylodiscitis complicated by the ingestion of a button battery: a case report. Korean J Radiol 2008; 9: 555–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan A, Wolfram S, Birmingham M, et al. Neck pain and stiffness in a toddler with history of button battery ingestion. J Emerg Med 2011; 41: 157–160. [DOI] [PubMed] [Google Scholar]
- 8.Jarugula R, Dorofaeff T. Oesophageal button battery injuries: think again. Emerg Med Australas 2011; 23: 220–223. [DOI] [PubMed] [Google Scholar]
- 9.Eshaghi H, Norouzi S, Heidari-Bateni G, et al. Spondylodiscitis: a rare complication of button battery ingestion in a 10-month-old boy. Pediatr Emerg Care 2013; 29: 368–370. [DOI] [PubMed] [Google Scholar]
- 10.Kieu V, Palit S, Wilson G, et al. Cervical spondylodiscitis following button battery ingestion. J Pediatr 2014; 164: 1500– e1. [DOI] [PubMed] [Google Scholar]