Abstract
Vertebroplasty (VP) is a percutaneous mini-invasive technique developed in the late 1980s as antalgic and stabilizing treatment in patients affected by symptomatic vertebral fracture due to porotic disease, traumatic injury and primary or secondary vertebral spine tumors. The technique consists of a simple metameric injection of an inert cement (poly-methyl-methacrylate, PMMA), through a needle by trans-peduncular, parapeduncular or trans-somatic approach obtaining a vertebral augmentation and stabilization effect associated with pain relief. The technique is simple and fast, and should be performed under fluoroscopy or CT guidance in order to obtain a good result with low complication rate. The aim of this paper is to illustrate the utility of VP, the indications-contraindications criteria, how to technically perform the technique using imaging guidance, and the results and complications of this treatment in patients affected by symptomatic vertebral compression fracture.
Keywords: Vertebroplasty, poly-methyl-methacrylate, vertebral compression fracture, cement leakage, mini-invasive percutaneous technique, cementoplasty
Introduction
Vertebroplasty (VP) is a percutaneous mini-invasive technique developed in the late 1980s; its use has increased greatly in the last 15 years as an antalgic and stabilizing treatment in patients affected by symptomatic vertebral collapse due to porotic insufficiency fracture, traumatic injury or primary and secondary vertebral spine tumors.1
The technique consists of a simple metameric injection of an inert cement (polymethyl methacrylate (PMMA)), through a needle by a trans-peduncular, parapeduncular or trans-somatic approach, obtaining a vertebral augmentation and stabilization effect associated with pain relief.2 The first account of VP was published by Galimbert et al. 1987, describing this procedure as an alternative treatment for symptomatic vertebral hemangioma of C2.3
The technique is simple and fast, and should be performed under fluoroscopy or computed tomography (CT) guidance in order to obtain a good clinical and morphological result with a low complication rate.1–3
The Assisted Technique (AT) includes numerous devices to treat the same pathology as VP, in which the cement injection is performed after the positioning of a mechanical or hydraulic system, creating a cavity within the vertebral body in order to restore vertebral height and physiological spine biomechanics.
Primary insufficiency, porotic fractures and iatrogenic osteoporotic fractures related to long-term steroid therapy are major indications for VP, with patients treated worldwide by different types of physician, including neuroradiologists, radiologists, orthopedic specialists, neurosurgeons and pain therapists.4 The rationale of the therapy is to combine analgesic and vertebral stabilization effects with or without restoration of the physiological height of the collapsed vertebral body, avoiding or reducing medical complications.
Patients are usually treated with bed rest, orthotic devices, analgesics and bisphosphonates as first-line therapy, but very often they have sleep disturbances and chronic pain that can also create psychological and depression problems, with a total mortality and morbidity rate of up to 20% of all patients.5,6
The aim of this paper is to illustrate the indications–contraindications criteria, the technique using imaging guidance, the results and the complications of the treatment in patients affected by symptomatic vertebral compression fracture (VCF) treated with VP.
Inclusion–exclusion criteria
The major indications for VP are patients affected by porotic insufficiency fracture complaining of back pain syndrome resistant to medical and physical therapy for at least 6 weeks.7 The selection criteria are based on clinical findings (pain evaluation) associated with imaging correlation based mostly on magnetic resonance (MR) abnormality.7
Pain syndrome or back pain should be intense, non-radicular, defined as axial midline vertebral pain, refractory to conventional medical treatment (bracing, analgesics and bed rest) and strongly exacerbated by digital palpation of the spinous process of the affected vertebra on clinical evaluation.8 The pain is due to stretching of the periosteal fibers along the cortical bone by the movements of the trabecular and cortical micro-fractures at the level of the collapsed soma,9 and it can be evaluated by many different methods such as the Visual Analogue Scale (VAS), the Oswestry Disability Index (ODI), SF 36 and Roland Morris questionnaire.10
Pain onset is an important parameter to consider because it can help in deciding to treat or not to treat the patient.11 The typical case history of a patient with an insufficiency porotic fracture is as follows: initially the patient refers an acute back pain at thoracic or lumbar level exacerbated by movements and respiratory acts. Usually the patient begins medical therapy (analgesics and bed rest) for a few weeks. Statistically, two-thirds of patients tend to recover and improve within 4–6 weeks from the onset of the spine pain; if the pain does not reduce or, even worse, it increases, imaging evaluation with MR should be performed to understand the reason for the back pain, and to exclude or detect VCF.12–14
The treatment decision needs a strict correlation between clinical data (type and grade of pain, the location) and imaging data. The diagnostic algorithm for the porotic patient with acute pain includes:4–6,11
Standard X-ray on AP and LL view in order to detect VCF (vertebral body collapse more then 10% compressing anterior cortex, sparing middle-posterior columns, ±kyphosis deformation)
Thoracic and lumbar MR with the following protocol: sagittal T1WI, T2WI, T2WI-STIR, which is mandatory to evaluate VCF. The sagittal T2WI-STIR sequence (or any T2WI fat suppression sequence) is necessary to decide about the treatment, showing the vertebral body hyperintensity, typical for acute VCF or for unhealed VCF due to bone marrow edema, or it can detect occult fractures not visible on plain-film X-ray (Figure 1(a–e)).
In case of known MR contraindication, a bone nuclear medicine scan should be requested showing an unspecific vertebral body intense uptake requiring a multidetector CT (MDCT) correlation in order to make a diagnosis of porotic VCF.
MDCT with MPR is useful to differential benign porotic fractures versus neoplastic ones, searching for the intravertebral vacuum sign or soft tissue abnormality (Figure 2(a–e)).
In case of uncertain pattern on MDCT or MR morphology or signal intensity, a bone biopsy is mandatory to understand the nature of the lesion prior to performing VP. It is useful to perform a spine bone biopsy especially during retreatment of patients, to rule out multiple myeloma or other disease as the cause of the new vertebral collapse in an osteoporotic patient presenting a new fracture in an adjacent or distant site from the previously treated vertebral body.11
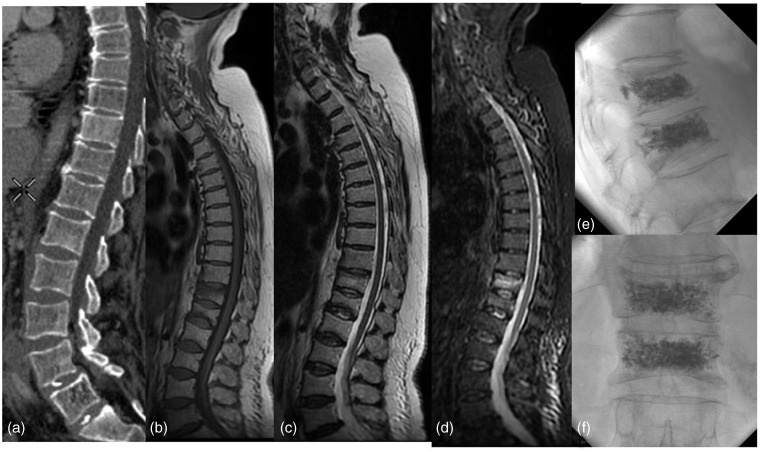
Figure 1.
A 65-year-old woman with low back pain resistant to medical therapy. (a) The sagittal MPR-MDCT showed no VCF at the thoraco-lumbar level. (b–d) VCF of T12 and L1 that appeared hypo-intense on T1WI and hyperintense on T2WI with typical sign of intra-spongious edema on T2W-STIR.
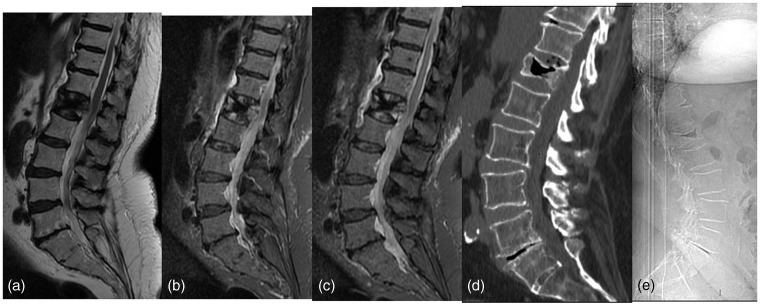
Figure 2.
Low back pain resistant to medical therapy in patient with a history of prostate carcinoma. (a–c) The sagittal T2W and T2W-STIR MR showed VCF of L1 that could mimic osteoblastic metastasis. (d, e) The sagittal MPR-MDCT and LL-X-ray film showed a vacuum sign of the soma of L1. The diagnosis was porotic VCF of L1.
There are other benign forms or uncommon locations of porotic fracture. Kummel disease is a benign form of porotic fracture, with typical vertebral osteonecrosis with intravertebral vacuum or cystic phenomenon. It occurs in approximately 10% of vertebral osteoporotic fractures, mainly in the thoraco-lumbar zone, and is accentuated on extension views. The patient with Kummel disease responds well to VP stabilization.15,16
Symptomatic vertebra plana is considered as a relative contraindication to VP. It can occur in benign porotic or non-porotic (aneurysmal bone cyst) diseases or neoplastic lesions, and a bone biopsy is often recommended. VP can be performed using a smaller needle.17
Porotic fracture can involve the sacrum as a typically painful stress fracture resistant to any medical therapy, with the evidence on T2W-STIR sequence of hyperintensity bone marrow edema and sometimes correlated to an H-shaped line fracture.18,19
The exclusion criteria are represented by: asymptomatic VCF; diffuse, non-focal pain without MR evidence of altered trabecular-bone signal; systemic or local infections; uncorrectable coagulation disorders; and allergy to PMMA.11
A patient with porotic fracture on MR imaging with hyperintensity on T2W-STIR sequence but without back pain is not indicated for this treatment. A patient with spine pain syndrome, VCF and visibility on MR of hyperintensity on T2W-STIR sequence is the one with the best and correct indication for VP.11
Technical and radiological approach to the spine
The procedure can be performed under fluoroscopy (most commonly used) or Fluoro-CT guidance with the patient in the prone position for treatment at the thoracic, thoraco-lumbar or lumbar level, while at the cervical level the supine position with a hyperextension of the neck is necessary to view the cervical metamer with open mouth technique for C1–C2 and also sometimes C3, while an antero-lateral approach is useful for C4–C7 levels with manual displacement of the vascular bundles.
Generally VP is performed under neuro-lepto-analgesia or skin-periostium local anesthesia. High-quality fluoroscopy guidance is preferred, especially in the case of complex, elderly porotic patients, or in patients with scoliotic curvature, in order to reduce the incidence of side effects and complications related to mal-positioning of the injecting needles.
Different approaches exist to performing VP depending on VCF morphology, metamere level and personal experience.1–11,14
A bilateral or mono-lateral trans-peduncular approach under fluoroscopic guidance is most used for thoracic and lumbar level procedures. The bi-peduncular approach guarantees the most homogeneous and complete cement distribution in the porotic fracture, while in the mono-lateral approach, the needle must reach the vertebral body in a central position for complete cement filling. Once a fluoro image is obtained in which the upper and lower endplates are perfectly aligned and the spinous processes are projected in midline, the pedicle is approached with an 11 up to 13 Gauge beveled needle between 10 and 15 cm long, with side wings to facilitate rotation. 15 G needles are mandatory to perform cervical VP.
The needle must never go over the medial wall of the pedicle; this represents an important lead marker to be checked before going through the posterior wall of the vertebral body, in order to avoid the spinal canal or spinal cord.
Other approaches are the trans-somatic, the para-peduncular, the trans-costo-transversal (for the thoracic level), the antero-lateral (for the cervical tract) or the trans-oral approach for C1 and C2. A combined CT and fluoro approach can be useful for some rare location such as lower cervical–upper thoracic spine location, or for sacral injection; in this way the needle can be positioned under CT guidance while the injection of the cement can be done under fluoroscopy.
Once inside the pedicle, the needle is advanced to the anterior third of the vertebra using lateral view control. The cement injection must be performed slowly and under continuous fluoroscopy control. If some venous leakage is seen during cement injection it is recommended to stop the injection, wait a few minutes for cement polymerization, and then to continue to fill the vertebra body.
There are no absolute rules about the amount of cement for each vertebra, which depends on metamere level and the degree of the collapsed vertebra. It is variable from 2 ml up to 8–10 ml. The rationale is that cement distribution in the fractured vertebra should be from the superior to the inferior endplate passing through the midline to guarantee the best stabilizing and biomechanical effect. It is not necessary to overfill the metamere, avoiding venous and disc leakage.
There are no definitive rules about the numbers of metameres to treat in one session, but usually a maximum of 3–4 is well accepted in the scientific community. However, in selected cases it is also possible to perform VP for up to 10–12 metamers in the same session (iatrogenic vertebral porotic fractures due to long-term steroid therapy in patients with collagenopathies, Crohn’s disease, epilepsy and allergic rhinitis) (Figure 3(a, b)).
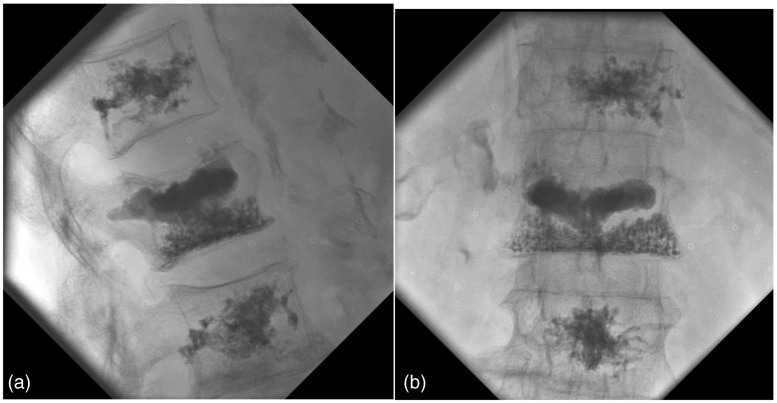
Figure 3.
72-year-old woman affected by multiple symptomatic porotic VCFs at the thoraco-lumbar level. (a, b) The PA and LL fluoroscopy control show the one-session multilevel VP.
For VP at the sacrum, it is possible to place from 1 to 4 needles (13 or15 G) under CT or fluoro guidance, checking the position and the cement distribution and avoiding diffusion to the neural sacral foramina.18,19
Preventative VP is a possible solution to prevent fractures to an adjacent metamere, especially at the level of the thoraco-lumbar junction where the axial load can be modified, creating new biomechanical forces (Figure 4(a, b)).20
Figure 4.
74-year-old woman affected by symptomatic porotic VCF at L2 level. (a, b) The LL and PA fluoroscopy control show the VP of L2 without leakage and the preventative VP of L1 and L3.
How to avoid systemic and procedure-related complications
In order to reduce complications and perform a correct clinical evaluation prior to treatment, a hematologic analysis is suggested to avoid general contraindications, checking blood count, PT, PTT and fibrinogen. Anti-coagulant therapies must be interrupted at least for 1 week before the procedure, switching to low weight molecular heparin with less medical risky treatment.4,9
A preventative bolus of wide-spectrum antibiotic is suggested to be infused i.v. before and during the treatment in order to avoid or reduce infectious complications.9
The complications of this treatment are rare compared with the number of procedures performed worldwide, and they can be divided into systemic and procedure-related complications. Systemic complications include infections and bleeding, while procedure-related complications include local trauma and cement leakage with diffusion into the pre/paravertebral venous plexus, which can lead rarely to consequent compression of nervous structures and spinal cord. Rare cases of paraplegia or death have also been described.9
Disc leakage with the potential complication of increased risk of re-fracture to adjacent levels after treatment is questionable, and many authors agree that this depends upon the type of cement distribution causing different axial loads.21–23 However, these potential complications should be correlated and compared with the natural history of porotic patients, which includes a yearly potential risk of 20% of new fracture in patients with a first VCF.24–29 Cement leakage occurs during the injection, and it can involve the venous plexus or paravertebral space, epidural space, or disc structures, but it is important to remember that the majority of the time it is completely asymptomatic.4–9
The risk of cement leakage is lower in AT compared with VP, while the incidence of new vertebral fractures to adjacent or distant metameres is the same, and is mostly related to the porotic disease itself.30,31 The first AT described was balloon kyphoplasty (KP), in which a dilation with balloon tamp preceded cement injection. It is well demonstrated that both VP and AT provide significant improvement in VAS pain scores, and while VP has a significantly greater improvement in pain scores it has also statistically greater risk of cement leakage (19.7% for VP versus 7.0% for KP, symptomatic leakage 1.6% for VP, 0.3% for KP) and new fracture (17.9% for VP, 14.1% for KP).32
Three factors described by Lador et al.33 influence cement leakage as well as cement flow within a vertebral body:
bone morphology and fracture patterns;
cement properties (viscosity);
injection method (speed, pressure, needle placement).
Bone- and fracture-related parameters may play a dominant role in explaining variations between patients. Because of the wide range of indications for vertebral augmentation, the procedure is applied to a wide range of bone densities and porosities and a wide range of fracture morphologies.
With respect to cement properties, it has been suggested that the cement should spread through the vertebral body in a controlled way that appears fluoroscopically as a ‘uniformly expanding cloud.’ VP cement leakage is due to high-pressure injection in PMMA diffusion, unlike the low-pressure condition of KP, where the cavity created by balloon tamp systems guarantees a lower rate of incidence.33
Vascular leakage is frequent and remains mostly asymptomatic, but can be a cause of pulmonary embolism in about 2–10% of cases for porotic patients.9 Disc leakage is related to higher incidence of fracture to an adjacent vertebral body. If it occurs, it is suggested to perform VP to the metamere below or above as preventative treatment.20
Epidural or endocanalar PMMA diffusion can potentially cause dramatic complications such as paraplegia or tetraplegia. This may be due to incorrect needle and working cannula positioning, or incorrect posteroanterior X-ray working-projection without considering the two important anatomical landmarks: the posterior wall of the vertebral body – that should never be passed by cement opacity – and the medial wall of the pedicle, which the needle should never go over in order to avoid the spinal canal.4–11
Two major points must be understood to reduce leakage: the whole procedure should be performed with a technology system (digital subtraction angiography (DSA) or CT-fluoro CT), and a viscous and dense cement with a slow injection rate should be used.9
Cement viscosity is directly related to the degree to which the cement has polymerized, which is a time and temperature-dependent reaction. Conventional cements routinely pass through a high-viscosity stage as they polymerize, but are only usable for a relatively short period of time before becoming too viscous to deliver. There are now available multiple types of cement with high viscosity and prolonged working times of up to 26 minutes.
To reduce extravasation, achieve a significantly lower rate of cement leakage and optimize cement distribution during treatment of VCFs, different systems and devices have been developed. For example, the radiofrequency-targeted vertebral augmentation (RF-TVA) technique may provide an approximately 50% reduction in leakage rate, using the combination of controlled delivery of radiofrequency-activated (high-viscosity) cement at a fixed, low rate of delivery into site-specific channels created using a rotational osteotome.34
The cause of vertebral re-fractures at distant or adjacent metameres remains controversial and complex. Even if re-fractures are the natural evolution of osteoporotic diseases, with a 19.2% risk of developing new fractures in the year following the first VCF,28,29 they could be made evident by the post-VP spinal biomechanical modification, which increases according to the different properties and stiffness grade of the cement used.21,22 PMMA is the most used commercially available cement for vertebral augmentation. Its proven effectiveness in reducing pain from vertebral collapse almost immediately is considered to reside not only in its fracture-stabilizing action, but also in the secondary local nerve damage as a consequence of its high setting temperature and chemical toxicity. The available data in the scientific literature on PMMA setting-induced heat–chemical toxicity damage on surrounding nerve structures is ambiguous. However, data on its mechanical and bone integration properties are clear. PMMA Young’s modulus (1.8–3.1 GPa) is significantly higher than normal bone, thus interfering mechanically with load stresses and preventing surrounding bone remodeling; in the case of osteoporotic bone, PMMA strength is 8–40 times higher. Such high stiffness may account for the risk of re-collapse of the spared, not impregnated, cancellous bone of the same vertebral body, and for the risk of incidental adjacent fractures.7
New biodegradable bone cement substitutes with different activity and different grades of viscosity have been developed as alternatives for PMMA, which can reduce or influence VP complication rates thanks to their bio-compatibly or absorbability and stiffness or mechanical or bone-remodeling proprieties,6,7 but because of high costs their use in porotic patients cannot be justified.
Results and discussion
The rationale of this mini-invasive procedure is to stabilize the movements of the trabecular and cortical micro-fractures of the collapsed vertebra, responsible for the pain caused by stretching of nerve fibers along the cortical bone, obtaining an antalgic effect by PMMA or other type of injection into the vertebral body.3,4
The primary endpoint of the technique is pain relief in patients affected by VCF, and this has been well established by several studies and trials in recent years comparing VP outcome versus conservative medical treatment.1–5
The technique had been recognized as a safe, efficacious, and durable procedure in patients with VCFs refractory to medical therapy by the consensus statement developed by the American Society of Interventional and Therapeutic Neuroradiology, Society of Interventional Radiology, American Association of Neurological Surgeons/Congress of Neurological Surgeons, and American Society of Spine Radiology in 2007.35
In 2009, two randomized trials on porotic vertebral fracture versus sham procedure were published, stimulating discussion, criticism and doubts about the clinical results of VP,7,8 while other randomized controlled trials confirmed the efficacy and safety of balloon KP and also of VP (Vertos) versus medical therapy.36
The Vertos I study proved that there are no absolute rules about timing for performing VP in porotic patients. In patients with VCF, performing VP within a few weeks of the acute onset of symptomatology produces better results than bed rest and optimal pain medication, but it is still worthwhile to perform VP after 6 months if the patient is still in pain and MR shows the typical T2 STIR abnormality. It has been published that statistically two-thirds of vertebral porotic fractures improve clinically within 6–8 weeks of the onset of the pain, so usually if there is still pain after 2 months with the presence abnormal MR findings, this is a correct indication for cementoplasty.36
The Vertos II open-label prospective randomized multi-center trial demonstrated that the pain relief after VP is immediate, is sustained for at least a year, and is significantly greater than that achieved with conservative treatment, at an acceptable cost.37
The incidence of new VCFs is not different after VP compared with conservative therapy after a mean of 11.4 months of follow-up. The only risk factor for new VCFs is the number of VCFs at baseline. VP contributed to preservation of stature by decreasing both the incidence and severity of further height loss in treated vertebrae.38
The Vertos III study evaluated the pain course in conservatively treated patients with back pain and a VCF on spine radiograph. It showed that more than half of conservatively treated patients with back pain and VCF had sufficient pain relief at 12 months, with most pain decrease in the first 3 months. However, there are no predictors for the development of chronic pain, and patients with continuing pain ≥3 months using significantly more analgesics than others after diagnosis of VCF may be candidates for VP.39
The Investigational Vertebroplasty Safety and Efficacy Trial (INVEST), a blinded, randomized controlled trial, investigated the 1-year effectiveness of VP in the treatment of osteoporotic VCFs including 131 participants (68 in the VP group and 63 in the control group). Patients in both groups showed improvements in pain and function at 1 year, and VP may provide a modest reduction in pain at 1 year compared with a control procedure.40,41
By a MEDLINE research, using the keywords “Vertebral augmentation technique for porotic vertebral compression fracture” there are more than 1400 papers about VP treatment reporting a success rate of over 80% with a level III of evidence.
Anselmetti et al.42 performed VP in 1634 patients affected by painful osteoporotic VCFs with a long-term follow-up, reporting a significant improvement of VAS and ODI, registering 34.3% PMMA leakages and 13.1% new painful fractures (a distant fracture occurred in 36.4%, and 63.6% had a new fracture in a contiguous vertebra) complication rates.
Muto et al.11,14 reported their experience on 805 vertebral bodies in 485 patients affected by osteoporosis (310), metastasis (160) and vertebral hemangioma. In patients treated with VP, the success rates at 24–72 h was 90% for osteoporotic fractures, 100% for vertebral hemangiomas and 77% for metastatic fractures. Extravertebral vascular or discal leakage of cement occurred in 39 patients, but only two of them reported radicular pain due to epidural involvement. Osteoporotic patients developed new vertebral fractures at adjacent levels in 25 cases and at distal levels in 19 cases.
Kim et al.43 registered a pain level according to VAS reduced by a value of 4.9 from the preoperative mean of 7 to the perioperative mean of 2.1. A total of 46% of the patients reported a level of 5 or more for reduction and maintenance of their pain level; 33 cases of newly developed vertebral fracture were reported in the vertebral bodies of 22 patients, which signified 32% newly developed vertebral fractures.
Kotwica and Saracen44 reported very significant relief of pain in 85% of patients; on the 7th and 30th day a very good treatment result was reported in 96%. The same result was noted in 92% of patients at the 6th month, and in 90% of patients at the 12th month. Among the 80 patients followed for 2 years, three patients reported recurrence of pain and were subsequently diagnosed with new osteoporotic fractures.
Recently a new type of osteoconductive cement has been developed as bone substitute (Cerament), inducing the formation of new normal bone and lower rate of new fracture, as an alternative to PMMA. It comprises 60% alpha-calcium sulfate (α-CaS) and 40% hydroxyapatite (HA). It can be resorbed at a rate equal to new bone ingrowth, achieving complete bone remodeling and healing, while being able to tolerate the motion–load stresses the spine usually undergoes. The strength of calcium sulfate alone is too weak compared with that of cancellous bone, and its rate of reabsorption is too high to allow new bone ingrowth. It has been demonstrated that this type of cement is a lower-stiffness alternative to PMMA for immediate and long-term stabilization of osteoporotic collapsed vertebral bodies, with lower incidence rate of new VCF.45
VP has no specific properties and techniques for high augmentation effect and kyphosis restoration, as kyphoplasty has. By VP this could be happen anyway, especially in the case of ‘vertebral mobile fracture’, but with a lower rate compared with AT (Figure 5(a–e)).46,47
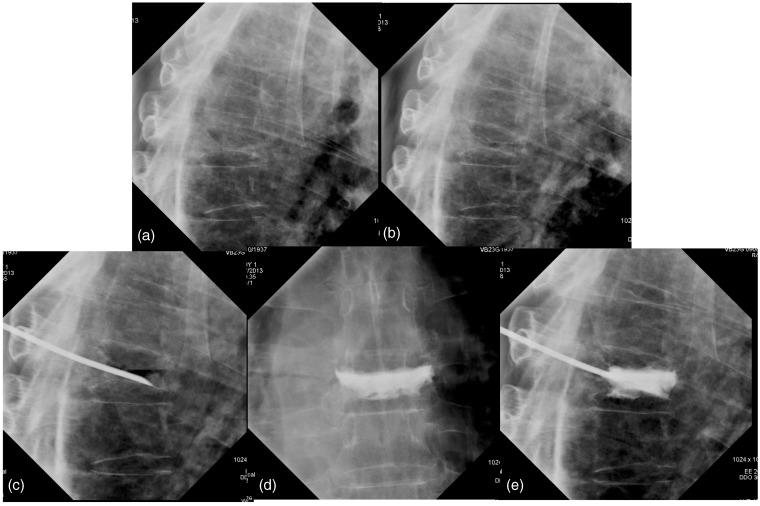
Figure 5.
77-year-old man affected by symptomatic porotic vertebra plana of D8. (a) The LL X-ray film shows a vertebra plana of T8. (b) The LL X-ray film in breathing position shows the “vertebral mobile fracture” during breathing. (c) The LL fluoroscopy control shows the needle placement into D8 soma by mono-peduncular approach with vacuum effect into the soma. (d, e) The PA and LL fluoroscopy control after VP of D8 with good cement distribution and augmentation effect of D8.
The European VErtebroplasty RESearch Team (E.VE.RES.T),48 a multi-center study with a large series of patients, prospectively evaluated results and complications of VP performed in 4547 patients (3211 females and 1336 males; mean age 70.2 years) for a total of 13.437 treated vertebrae. Of 4547 patients, 4004 (88.0%) reported significant pain relief (difference ≥2 points in pain evaluated with an 11-point VAS; p < 0.0001) within 48 h: an average of 7.7 ± 0.4, which dropped to 1.8 ± 0.6 in osteoporotic patients. Some 430 osteoporotic patients (13%) were retreated for a subsequent fracture; in 302/430 patients (70.2%), the new fracture occurred in the contiguous vertebra. No major neurologic complications were reported and the most frequent minor complication was venous leakage (20.5%).
Conclusions
Vertebroplasty is a safe and effective technique for the treatment of spine pain due to porotic VCF, with a high rate of successful clinical results and a low rate of complications. It is very important to perform a correct clinical-imaging diagnostic approach, especially with MR examination, to exclude other pathologies. The technique is simple, fast and safe, and should be performed under the best imaging guidance available to avoid clinical complications. New materials are now also available to obtain the best cement distribution and reduce or avoid disc and venous leakage. No significant difference in terms of pain relief exists between AT and VP. In osteoporosis, VP stabilizes the metamere, leading to the early mobilization of the patient and achieving pain relief in 80–95%, according to published papers.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
None declared.
References
- 1.Wong X, Reiley MA, Garfin S. Vertebroplasty/kyphoplasty. J Women Imaging 2000; 2: 117–124. [Google Scholar]
- 2.Pflugmacher R, Kandziora F, Schroder R, et al. Vertebroplasty and kyphoplasty in osteoporotic fractures of vertebral bodies: A prospective 1-year follow-up analysis. Rofo 2005; 177: 1670–1676. [DOI] [PubMed] [Google Scholar]
- 3.Galimbert P, Deramond H, Rosat P, et al. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987; 33: 166–168. [PubMed] [Google Scholar]
- 4.Gangi A, Guth S, Imbert JP, et al. Percutaneous vertebroplasty: Indications, technique, and results. Radiographics 2003; 23: 10–20. [DOI] [PubMed] [Google Scholar]
- 5.Mathis JM, Barr JD, Belkoff SM, et al. Percutaneous vertebroplasty: A developing standard of care for vertebral compression fractures. Am J Neuroradiol 2001; 22: 373–381. [PMC free article] [PubMed] [Google Scholar]
- 6.Muijs SP, van Erkel AR, Dijkstra PD. Treatment of painful osteoporotic vertebral compression fractures: A brief review of the evidence for percutaneous vertebroplasty. J Bone Joint Surg Br 2011; 93: 1149–1153. [DOI] [PubMed] [Google Scholar]
- 7.Kallmes DF, Heagerty PJ, Turner JA, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009; 361: 569–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guglielmi G, Andreula C, Muto M, et al. Percutaneous vertebroplasty: Indications, contraindications, technique and complications. Acta Radiol 2005; 46: 256–268. [DOI] [PubMed] [Google Scholar]
- 9.Mathis JM, Barr JD, Belkoff SM, et al. Percutaneous vertebroplasty: A developing standard of care for vertebral compression fractures. Am J Neuroradiol 2001; 22: 373–381. [PMC free article] [PubMed] [Google Scholar]
- 10.Grotle M1, Brox JI, Vøllestad NK. Concurrent comparison of responsiveness in pain and functional status measurements used for patients with low back pain. Spine 2004; 29: E492–E501. [DOI] [PubMed] [Google Scholar]
- 11.Muto M, Guarnieri G, Lavanga A, et al. Vertebroplasty and kyphoplasty: Friends or foes? Radiol Med 2008; 113: 1171–1184. [DOI] [PubMed] [Google Scholar]
- 12.Legrain V, Iannetti GD, Plaghki L, et al. The pain matrix reloaded: A salience detection system for the body. Prog Neurobiol 2011; 93: 111–124. [DOI] [PubMed] [Google Scholar]
- 13.Mouraux A, Diukova A, Lee MC, et al. A multisensory investigation of the functional significance of the “pain matrix”. Neuroimage 2011; 54: 2237–2249. [DOI] [PubMed] [Google Scholar]
- 14.Ambrosanio G, Lavanga A, Vassallo P, et al. Vertebroplasty in the treatment of spine disease. Interv Neuroradiol 2005; 11: 309–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pappou IP, Papadopoulos EC, Swanson AN, et al. Osteoporotic vertebral fractures and collapse with intravertebral vacuum sign (Kümmel’s disease). Orthopedics 2008; 31: 61–66. [DOI] [PubMed] [Google Scholar]
- 16.van der Schaaf I1, Fransen H. Percutaneous vertebroplasty as treatment for Kummell’s disease. JBR-BTR 2009; 92: 83–85. [PubMed] [Google Scholar]
- 17.Pedicelli A1, Capozzi A, Colosimo C, et al. Vertebra plana: Reappraisal of a contraindication to percutaneous vertebroplasty. Eur J Radiol 2013; 82: 2303–2308. [DOI] [PubMed] [Google Scholar]
- 18.Pereira LP, Clarençon F, Le Jean L, et al. Safety and effectiveness of percutaneous sacroplasty: A single-centre experience in 58 consecutive patients with tumours or osteoporotic insufficient fractures treated under fluoroscopic guidance. Eur Radiol 2013; 23: 2764–2772. [DOI] [PubMed] [Google Scholar]
- 19.Frey ME, Depalma MJ, Daitch JS. Percutaneous sacroplasty for osteoporotic sacral insufficiency fractures: A prospective, multicenter, observational pilot study. Spine J 2008; 8: 367–373. [DOI] [PubMed] [Google Scholar]
- 20.Yen CH, Teng MM, Yuan WH, et al. Preventive vertebroplasty for adjacent vertebral bodies: A good solution to reduce adjacent vertebral fracture after VP. Am J Neuroradiol 2012; 33: 826–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim JM, Lindsey DP, Hannibal M, et al. Vertebroplasty versus kyphoplasty: Biomechanical behavior under repetitive loading conditions. Spine 2006; 31: 2079–2084. [DOI] [PubMed] [Google Scholar]
- 22.Wilke HJ, Mehnert U, Claes LE, et al. Biomechanical evaluation of vertebroplasty and kyphoplasty with polymethyl methacrylate or calcium phosphate cement under cyclic loading. Spine 2006; 31: 2934–2941. [DOI] [PubMed] [Google Scholar]
- 23.Nouda S, Tomita S, Kin A, et al. Adjacent vertebral body fracture following vertebroplasty with polymethylmethacrylate or calcium phosphate cement biomechanical evaluation of the cadaveric spine. Spine 2007; 34: 2613–2618. [DOI] [PubMed] [Google Scholar]
- 24.Uppin AA, Hirsch JA, Centenera LV, et al. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology 2003; 226: 119–124. [DOI] [PubMed] [Google Scholar]
- 25.Kim SH, Kang HS, Choi JA, et al. Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Acta Radiol 2004; 45: 440–445. [DOI] [PubMed] [Google Scholar]
- 26.Trout AT, Kallmes DF, Kaufmann TJ. New fractures after vertebroplasty: Adjacent fractures occur significantly sooner. Am J Neuroradiol 2006; 27: 17–23. [PMC free article] [PubMed] [Google Scholar]
- 27.Furtado N, Oakland RJ, Wilcox RK, et al. A biomechanical investigation of vertebroplasty in osteoporotic compression fractures and in prophylactic vertebral reinforcement spine. 2007; 32: E480–E487. [DOI] [PubMed] [Google Scholar]
- 28.Lindsay R, Silvermann LS, Seeman E, et al. Risk of new vertebral fracture in the year following a fracture. JAMA 2001; 285: 320–323. [DOI] [PubMed] [Google Scholar]
- 29.Voormolen MH, Lohle PN, Lampmann LE. The risk of new osteoporotic vertebral compression fractures in the year after percutaneous vertebroplasty. J Vasc Interv Radiol 2006; 17: 71–76. [DOI] [PubMed] [Google Scholar]
- 30.Teng MM, Wei CJ, Wei LC, et al. Kyphosis correction and height restoration effects of percutaneous vertebroplasty. Am J Neuroradiol 2003; 24: 1893–1900. [PMC free article] [PubMed] [Google Scholar]
- 31.Matthew J, Parker SJ, Wolinsky JP, et al. Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: An evidenced-based review of the literature. Spine J 2009; 9: 501–508. [DOI] [PubMed] [Google Scholar]
- 32.Eck JC, Nachtigall D, Humphreys SC, et al. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: A meta-analysis of the literature. Spine J 2008; 8: 488–497. [DOI] [PubMed] [Google Scholar]
- 33.Lador R, Dreiangel N, Ben-Galim PJ, et al. A pictorial classification atlas of cement extravasation with vertebral augmentation. Spine J 2010; 10: 1118–1127. [DOI] [PubMed] [Google Scholar]
- 34.Georgy BA. Comparison between radiofrequency targeted vertebral augmentation and balloon kyphoplasty in the treatment of vertebral compression fractures: Addressing factors that affect cement extravasation and distribution. Pain Physician 2013; 16: E513–E518. [PubMed] [Google Scholar]
- 35.Jensen ME, McGraw JK, Cardella JF, et al. Position statement on percutaneous vertebral augmentation: A consensus statement developed by the American Society of Interventional and Therapeutic Neuroradiology, Society of Interventional Radiology, American Association of Neurological Surgeons/Congress of Neurological Surgeons, and American Society of Spine Radiology. Am J Neuroradiol 2007; 28: 1439–1443. [PMC free article] [PubMed] [Google Scholar]
- 36.Voormolen MH, Mali WP, Lohle PN, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: Short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. Am J Neuroradiol 2007; 28: 555–560. [PMC free article] [PubMed] [Google Scholar]
- 37.Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): An open-label randomised trial. Lancet 2010; 376: 1085–1092. [DOI] [PubMed] [Google Scholar]
- 38.Klazen CA, Muller A, Fransen H, et al. Percutaneous vertebroplasty is not a risk factor for new osteoporotic compression fractures: Results from VERTOS II. Am J Neuroradiol 2010; 31: 1447–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Venmans A, Lohle PN, van Rooij WJ. Pain course in conservatively treated patients with back pain and a VCF on the spine radiograph (VERTOS III). Skeletal Radiol 2014; 43: 13–18. [DOI] [PubMed] [Google Scholar]
- 40.Comstock BA, Sitlani CM, Jarvik JG, et al. Investigational vertebroplasty safety and efficacy trial (INVEST): Patient-reported outcomes through 1 year. Radiology 2013; 269: 224–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gray LA, Jarvik JG, Heagerty PJ, et al. INvestigational Vertebroplasty Efficacy and Safety Trial (INVEST): A randomized controlled trial of percutaneous vertebroplasty. BMC Musculoskelet Disord 2007; 8: 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anselmetti GC, et al. Percutaneous vertebroplasty in osteoporotic patients: An institutional experience of 1.634 patients with long-term follow-up. J Vasc Interv Radiol 2011; 22: 1714–1720. [DOI] [PubMed] [Google Scholar]
- 43.Kim JH, Yoo SH, Kim JH. Long-term follow-up of percutaneous vertebroplasty in osteoporotic compression fracture: Minimum of 5 years follow-up. Asian Spine J 2012; 6: 6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kotwica Z, Saracen A. Early and long-term outcomes of vertebroplasty for single osteoporotic fractures. Neurol Neurochir Pol 2011; 45: 431–435. [DOI] [PubMed] [Google Scholar]
- 45.Masala S, Marcia S, Muto M, et al. Osteoporotic vertebral compression fractures augmentation by injectable partly resorbable ceramic bone substitute (Cerament™|SPINE SUPPORT): A prospective nonrandomized study. Neuroradiology 2012; 54: 589–596. [DOI] [PubMed] [Google Scholar]
- 46.McKiernan F1, Jensen R, Faciszewski T. The dynamic mobility of vertebral compression fractures. J Bone Miner Res 2003; 18: 24–29. [DOI] [PubMed] [Google Scholar]
- 47.McKiernan F1, Faciszewski T, Jensen R. Does vertebral height restoration achieved at vertebroplasty matter? J Vasc Interv Radiol 2005; 16: 973–979. [DOI] [PubMed] [Google Scholar]
- 48.Anselmetti GC, Marcia S, Saba L, et al. Percutaneous vertebroplasty: Multi-centric results from EVEREST experience in large cohort of patients. Eur J Radiol 2012; 81: 4083–4086. [DOI] [PubMed] [Google Scholar]