Abstract
We describe a case of cerebral infarctions caused by transient vasoconstrictions in the posterior circulation 2 weeks after intraventricular hemorrhage without subarachnoid hemorrhage in a 35-year-old patient with Moyamoya disease. To our knowledge, this is the first case report where diffuse segmental vasoconstrictions of the basilar and posterior cerebral arteries were recognized after intraventricular hemorrhage in Moyamoya disease. The patient complained of severe and acute-onset headache 14 days after the intraventricular hemorrhage, which had a different character and severity from the one she complained of at the onset of intraventricular hemorrhage. Finally, headache disappeared within 1 month and vasoconstriction resolved in 2 months. Reversible cerebral vasoconstriction syndrome was under consideration for the etiology of her condition because of the “thunderclap” characteristics of the headache and the delayed timing of occurrence of the vasoconstriction. This case report informs and alerts neurologists, neurosurgeons and neuroradiologists who observe and treat patients with Moyamoya disease that vasoconstriction in the posterior circulation may occur after intraventricular hemorrhage in these patients.
Keywords: Intraventricular hemorrhage, Moyamoya disease, reversible cerebral vasoconstriction syndrome, vasoconstriction
Introduction
Cerebral infarctions following an acute hemorrhage in a patient with Moyamoya disease have been rarely reported.1–5 In this article, we describe a case of delayed cerebral infarctions caused by possible reversible cerebral vasoconstriction after intraventricular hemorrhage (IVH) in a patient with Moyamoya disease. To our knowledge, this is the first case report where diffuse segmental vasoconstrictions of the basilar and posterior cerebral arteries were recognized after IVH in such a patient, and a possible pathogenesis of this rare condition is discussed.
Case presentation
A 34-year-old female with no past history except for headaches during childhood presented to our hospital because of a severe headache. Head computed tomography (CT) revealed right thalamic hemorrhage and IVH. This patient was diagnosed with Moyamoya disease after angiography (Suzuki stage 3, bilaterally). After discharge, she was followed up in our clinic without any medication. One year later, there were no cerebral ischemic lesions on magnetic resonance imaging (MRI) and no narrowing change of intracranial arteries including posterior circulation by magnetic resonance angiography (MRA). One month after the MRI and MRA, the patient complained of severe headache and vomiting, and was again transferred to our hospital as an emergency. She was neurologically intact. A head CT revealed an IVH. There was no subarachnoid hemorrhage (SAH) in the subarachnoid space. Her blood pressure was stable in the range 110–140/70–80 mmHg without any antihypertensive agent. We administered isotonic solutions to avoid dehydration. Four days after admission, the patient’s headache improved and she recovered oral intake. However, on postictal day 14, she again started to complain of episodes of severe headaches several times in a day. The headaches were very sudden and extremely severe, returning at short periods and awaking the patient from sleep. Analgesics had only limited efficacy. On the 15th day after the IVH, her level of consciousness became gradually worse. MRI confirmed ischemic lesions in the bilateral occipital areas. There were no findings of SAH by MRI fluid-attenuated inversion recovery images in the basal cisterns, Sylvian fissures and other subarachnoid space. There were diffuse segmental vasoconstrictions on the basilar and bilateral posterior cerebral arteries on the MRA (Figure 1(a), (b)). Laboratory data showed no hemoconcentration. Her general condition improved day by day. The headache was relieved and she recovered oral intake 25 days after IVH.
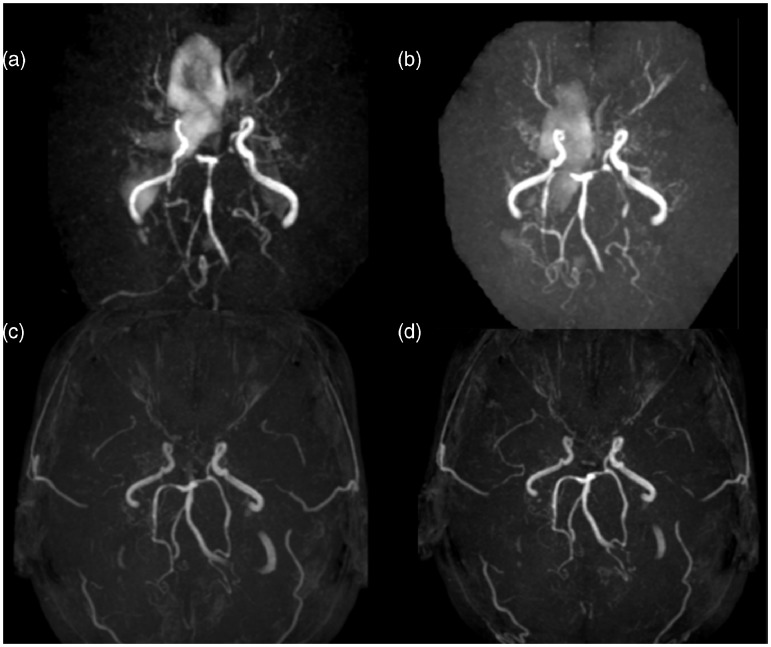
Figure 1.
Time course of magnetic resonance angiography (MRA). MRAs taken after 2 weeks from IVH, when the patient complained of her visual field deficit (a); 1 week later from B (b); 1 month later (c); and 2 months later (d). Vasoconstrictions of the vertebral and basilar arteries ameliorated after 1 month.
There was no suspicion of any infectious disease such as meningitis or encephalitis based on the clinical findings; she was afebrile with a normal count of serum white blood cells.
One month later, MRA showed improvement of the vasoconstriction (Figure 1(c)), and finally it disappeared within 2 months of the IVH (Figure 1(d)). The bilateral visual deficit continued, persisting 1 year later.
Conclusions
To our knowledge, this is the first report of a case with cerebral infarctions due to vasoconstriction in the basilar and posterior cerebral arteries (PCAs) after IVH in patients with Moyamoya disease. Cerebral infarctions following intracranial hemorrhage in patients with Moyamoya disease are rarely reported in the literature (Table 1).1–5 Some authors regarded the causes of the infarction as the result of increased intracranial pressure and dehydration.1,2,4,5 Only Nakai et al. highlighted vasospasm of the collateral pathways as pathogenesis of cerebral infarction.3
Table 1.
Summary of patients with Moyamoya disease who suffered from cerebral infarctions after intraventricular hemorrhage.
| Authors | Age | Sex | First stroke | Second stroke | Interval (day) | Cause of the second stroke |
|---|---|---|---|---|---|---|
| Iwama et al.1 | 10 | F | IVH | CI (left parieto-occipital region) | 14 | Dehydration by the hyperosmotic drugs |
| 18 | M | IVH | CI (left parietal, right frontal lobes) | 16 | Dehydration by the hyperosmotic drugs | |
| 46 | F | Caudate hemorrhage, IVH | CI (left parieto-occipital region) | 11 | Dehydration by the hyperosmotic drugs | |
| Nagasaka et al.2 | 9 | F | Caudate hemorrhage, IVH | CI (right frontal lobe) | 0 (concomitant CI and IVH) | Rupture and shrinkage of Moyamoya vessels |
| Nakai et al.3 | 29 | F | IVH | CI (right parietal lobe) | 11 | Vasospasm of the collateral pathways including Moyamoya vessels |
| Rafay et al.4 | 10 | F | IVH | CI (right frontal and occipital lobes) | 15 | Increased ICP |
| 11 | M | ICH, IVH | CI (right parietal and occipital lobes) | 2 | Increased ICP | |
| Su et al.5 | 29 | M | IVH | CI (bifrontal regions) | 15 | Dehydration, hypotension |
| Our case | 35 | F | IVH | CI (bifrontal parieto-occipital lobes) | 15 | Vasoconstriction of bilateral PCAs and basilar arteries |
IVH: intraventricular hemorrhage; CI: cerebral infarction; ICH: intracerebral hemorrhage; ICP: intracranial pressure; PCAs: posterior cerebral arteries
In Moyamoya disease, headache is a frequently encountered symptom.6 However, our case might be presenting the so-called “thunderclap” headache which can be seen in reversible cerebral vasoconstriction syndrome (RCVS), rather than the usual headache of Moyamoya disease or IVH. Most patients with RCVS complain of headaches being of a multiple, recurrent “thunderclap” type, with severe and sudden onset, reaching maximum intensity in less than a minute.7 Although there are no accepted diagnostic criteria for RCVS,7 cerebrospinal analysis findings are considered to be necessary to exclude central nervous system vasculitis, an important confounder of RCVS. We avoided cerebrospinal fluid examination in our patient because of suspected high intracranial pressure. Although in our case RCVS is not definitely the diagnosis, it has to be under consideration as a pathophysiological mechanism. The development of such mechanisms after IVH in Moyamoya disease should be a complication deserving recognition and attention by the observing and treating neurologists, neurosurgeons and neuroradiologists.
Acknowledgements
We thank Kostadin L. Karagiozov, M.D., Ph.D., for his advice and reviewing the paper, and the staff of the departments of Neurosurgery, Tokyo Wome’s Medical University, in preparing this paper.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Iwama T, Kotani Y, Yamakawa H, et al. Cerebral ischemic complications following intracranial bleeding in patients with moyamoya disease – three case reports. Neurol Med Chir (Tokyo) 2001; 41: 450–453. [DOI] [PubMed] [Google Scholar]
- 2.Nagasaka T, Hayashi S, Naito T, et al. Concomitant cerebral infarction and intraventricular hemorrhage in moyamoya disease. Case report. J Neurosurg 2007; 106: 388–390. [DOI] [PubMed] [Google Scholar]
- 3.Nakai Y, Hyodo A, Yanaka K, et al. Fatal cerebral infarction after intraventricular hemorrhage in a pregnant patient with moyamoya disease. J Clin Neurosci 2002; 9: 456–458. [DOI] [PubMed] [Google Scholar]
- 4.Rafay MF, Smith SE, Dirks P, et al. Hemorrhage predisposing to cerebral infarction in children with moyamoya disease. Pediatr Neurol 2006; 34: 400–404. [DOI] [PubMed] [Google Scholar]
- 5.Su IC, Yang CC, Wang WH, et al. Acute cerebral ischemia following intraventricular hemorrhage in moyamoya disease: Early perfusion computed tomography findings. J Neurosurg 2008; 109: 1049–1051. [DOI] [PubMed] [Google Scholar]
- 6.Okada Y, Kawamata T, Kawashima A, et al. The efficacy of superficial temporal artery-middle cerebral artery anastomosis in patients with moyamoya disease complaining of severe headache. J Neurosurg 2012; 116: 672–679. [DOI] [PubMed] [Google Scholar]
- 7.Velez A, McKinney JS. Reversible cerebral vasoconstriction syndrome: A review of recent research. Curr Neurol Neurosci Rep 2013; 13: 319. [DOI] [PubMed] [Google Scholar]