Abstract
Purpose
Tandem internal carotid and middle cerebral artery occlusion carries a grave prognosis, with intravenous and intra-arterial thrombolytics having low efficacy. Currently, endovascular therapy is a promising means for treatment in which the proximal carotid lesion can be treated with angioplasty and stenting, whilst mechanical thrombectomy can be used for the treatment of the distal occlusion. Two approaches can be used – the antegrade (proximal-to-distal) approach or the retrograde (distal-to-proximal) approach, although there has not yet been any consensus on which is the better approach.
Case report
We present two patients with tandem occlusions, one treated using the antegrade and one using the retrograde approach, with different revascularization outcomes, despite having similar functional outcome on follow-up.
Conclusion
The combined use of stent angioplasty and mechanical thrombectomy can be used to treat tandem occlusions, and with procedural modifications, the antegrade approach may more easily achieve technical success.
Keywords: Angioplasty, carotid artery, mechanical thrombectomy, stroke, tandem occlusion
Introduction
Tandem internal carotid artery (ICA) and middle cerebral artery (MCA) occlusion causing acute stroke is not rare. In one study, 17.2% of patients given intravenous tissue plasminogen activator (tPA) had a tandem occlusion of the ICA and proximal MCA.1 In another study, 25% of patients presenting acutely with an MCA occlusion had concomitant ICA occlusion.2 The proximal occlusion can be due to either underlying atherosclerotic stenosis or arterial dissection, with distal emboli to the intracranial vasculature. When tandem occlusions occur, proximal flow is impaired and the collateral supply to the ischemic area will mostly be limited to pial collaterals, so prognosis is usually poor. Intravenous thrombolysis is known to have a low recanalization rate for large vessel occlusions. Patients with such tandem occlusions given intravenous tPA had only half the chance of recanalization, but four times the risk of reocclusion, when compared to patients without tandem occlusion, leading to a worse functional outcome and higher mortality.1 Other methods include giving tPA intra-arterially past the proximal occlusion or via collaterals,3–5 but the efficacy of this method is also limited. Thrombolysis via collaterals also carries the risk of damaging the contralateral vasculature, further reducing collateral blood supply to the ipsilateral hemisphere.
With the advent of stent retrievers demonstrated to have a higher recanalization rate,6,7 mechanical thrombectomy has increasingly become the mode of treatment for distal thrombosis in recently published articles, whilst proximal lesions may be treated by angioplasty or stenting.8–10 However, there has not yet been any consensus on the optimal mode and sequence for intervention of the tandem lesions. We present here our experience with two patients with tandem occlusions of the ICA and MCA, one treated using an antegrade (proximal-to-distal) approach with technical modifications, and the second using a retrograde (distal-to-proximal) approach, with different revascularization outcomes.
Case report
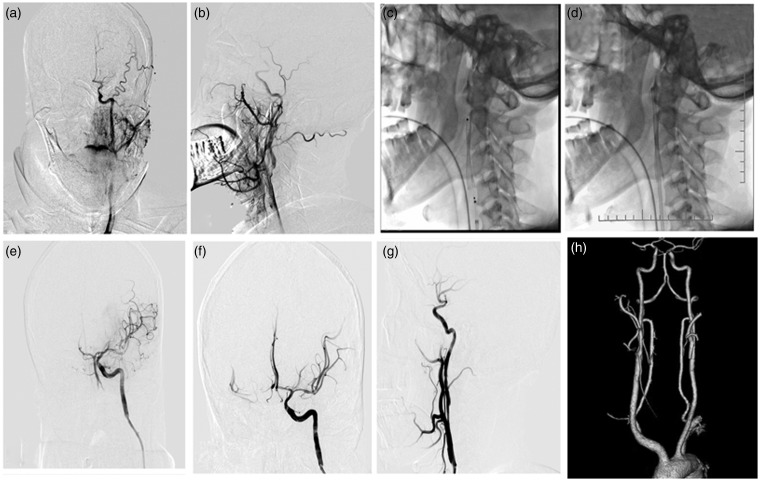
Patient 1 (Figure 1). A 51-year-old man presented with a 3-hour history of right facial palsy, mild hemiparesis and hemiparesthesia. The National Institute of Health Stroke Scale (NIHSS) score was 4. Magnetic resonance imaging (MRI) showed a small left parietal hyperintensity on diffusion weighted imaging (DWI), and poor opacification of the left ICA. Intravenous tPA was given at 3.5 hours, with initial improvement; however, the patient deteriorated 3 hours later with a decreased level of consciousness, dysphasia and dense right hemiplegia (NIHSS 14). Immediate plain computed tomography (CT) of the brain showed no intracerebral hemorrhage or large territory infarct. The patient was taken to the angiography suite, where angiography revealed a severe left C1 segment stenosis and a left M1 occlusion. Pre-operatively, the patient was given a loading dose of aspirin 300 mg and clopidogrel 300 mg. Under general anesthesia and systemic heparinization, an 8 Fr guiding catheter was advanced into the left common carotid artery (CCA). The C1 stenosis was dilated first with a 3.0 × 20 mm Aviator balloon (Cordis, NJ, USA), after which a FilterWire embolic protection device (EPD) (Boston Scientific, MA, USA) was advanced to the C2 segment, followed by deployment of a 9 × 30 mm Carotid Wallstent (Boston Scientific, MA, USA) across the stenotic area. Without withdrawal of the stent delivery shaft or use of the FilterWire retrieval device, the guiding catheter was advanced coaxially over the stent delivery shaft through the carotid stent to the distal C1 segment, and then the guiding catheter was used as the retrieval apparatus for both the stent delivery system and the FilterWire. Thrombectomy of the MCA occlusion was successfully performed with a 4 × 20 mm Solitaire AB device (eV3, MN, USA), achieving a Thrombolysis in Cerebral Infarction (TICI) grade of 3. The Solitaire device was then retrieved via the guiding catheter bypassing the stent. At 24 hours, the patient had an NIHSS score of 10; follow-up CT and computed tomography angiography (CTA) showed a small left centrum semiovale infarct and patent left ICA and MCA. After a short course of rehabilitation, the NIHSS was 3 and modified Rankin Scale (mRS) was 1 on discharge. The mRS was 1 at 3-month follow-up.
Figure 1.
Patient 1. (a, b) Angiogram showing a severe left ICA stenosis with acute thrombus formation and left MCA occlusion. (c) A 9 × 30 mm Carotid Wallstent was deployed across the left ICA origin. (d) The guiding catheter was advanced coaxially over the stent delivery shaft through the carotid stent to the distal C1 segment, and then the stent delivery system and FilterWire embolic protection device were successfully retrieved past the carotid stent via the guiding catheter. (e) Angiography via the guiding catheter showed left MCA thrombosis. (f) Good opacification of the left MCA after mechanical thrombectomy by the Solitaire device (4 × 20 mm). (g) A patent carotid stent at the left C1 origin at the conclusion of the operation. (h) Follow-up CT and CTA at 24 hours showed patent left ICA and MCA.
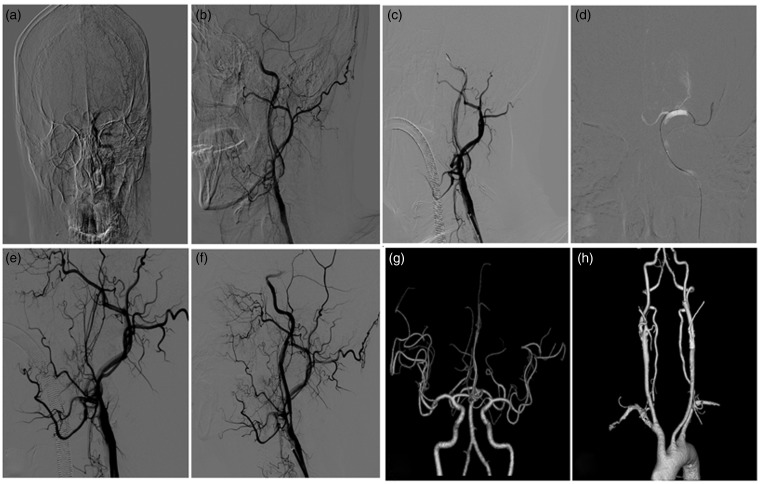
Patient 2 (Figure 2). A 70-year-old man presented with a history of dysphasia and right-sided weakness for 6 hours. On admission, the patient had gaze deviation to the left, expressive and receptive dysphasia, right facial palsy and right dense hemiplegia (NIHSS 16). MRI showed hyperintensity of left basal ganglia and corona radiata on DWI, poor opacification of the left ICA and a left M1 origin occlusion. The patient was given a loading dose of aspirin 300 mg and clopidogrel 300 mg. Under general anesthesia and systemic heparinization, immediate angiography showed a severe left C1 stenosis and left M1 origin occlusion. An 8 Fr guiding catheter was placed in the left CCA proximal to the site of stenosis. A microwire and a microcatheter were negotiated coaxially though the left ICA origin stenosis to the left distal M1. Selective angiography via the microcatheter revealed patent distal branches beyond the M1 occlusion. Thrombectomy of the M1 occlusion was attempted using a 4 × 20 mm Solitaire AB device. Angiography showed failed MCA recanalization and occlusion of the ICA origin, possibly due to dissection induced by the passage of the thrombectomy device through the carotid stenosis. A microcatheter and a microwire were advanced coaxially through the site of the ICA occlusion. After confirmation of microcatheter placement in the true lumen by selective angiography, a microwire was introduced to guide the placement of a Spider EPD (ev3, MN, USA). Pre-dilation was performed with a 3.0 × 30 mm Aviator balloon, followed by deployment of a 9 × 30 mm Carotid Wallstent across the internal carotid origin occluded segment. Post-stenting angiography showed no significant residual stenosis of the left ICA origin but persistent occlusion of the left M1 (TICI 0). As the intervention procedure had already lasted 2.5 hours, more than 8 hours past the symptom onset time, the procedure was abandoned due to possible futility of recanalization and increased risk of hemorrhage. Follow-up CTA at 24 hours showed recanalization of the left MCA. The mRS on follow-up at 3 months was 1.
Figure 2.
Patient 2. (a, b) Angiogram showing severe stenosis of the left ICA origin and occlusion of the left MCA M1 origin. (c, d) A guiding catheter was placed in the CCA and mechanical thrombectomy was attempted for the left M1 occlusion. (e) Angiogram post-mechanical thrombectomy showed left ICA C1 occlusion. (f) Angiogram after stenting of the left ICA occlusion showed a patent left C1 carotid stent and persistent occlusion of the left M1 origin. (g, h) Follow-up CTA at 24 hours showed recanalization of the left MCA and a patent left ICA stent.
Discussion
Patients with tandem occlusions are a subset of acute stroke patients that are technically more complicated to treat. Most recently published articles reported the use of angioplasty or stenting for the treatment of the proximal atherosclerotic stenoses, and mechanical thrombectomy for the distal thromboembolic MCA occlusions. Endovascular treatment for acute large vessel occlusion using stent retrievers is now supported by major trials demonstrating better recanalization rates and patient outcome.11–15 There are variations in the method of treatment, depending on lesion and vessel characteristics and the operator’s preference, with each having its own advantages and drawbacks. Methods differ in terms of what devices are used for recanalization, treatment timing (occlusions treated together versus as a staged operation) and sequence (antegrade8,10,16–19 versus retrograde18–20). For both of our patients, stent retrievers were used to recanalize the distal occlusion, and stenting was performed over the proximal carotid stenosis. We adopted a different treatment sequence for the two patients, using an antegrade approach for the first patient and a retrograde approach for the second patient, possibly contributing to their different revascularization outcomes.
For patient 1, the proximal stenosis was recanalized first with a closed cell Carotid Wallstent, followed by advancement of the guiding catheter to the ICA past the stent and then successful intracranial mechanical thrombectomy of the MCA. This antegrade approach with stenting first has advantages over the retrograde approach, just performing angioplasty first, or treating the proximal and distal lesions separately as a staged operation. Proximal stenting decreases the risk of recurrent distal embolization from the carotid lesion and risk of reocclusion, and allows the guiding catheter to be advanced more distally to provide support for larger-bore devices for distal recanalization. A closed cell carotid stent with a small cell size was chosen for better coverage of the plaque and to facilitate the passage of devices past the stent. To circumvent the subsequent risk of the thrombectomy devices becoming entangled with the stent struts on withdrawal, the guiding catheter was advanced through the carotid stent after proximal recanalization. The stent delivery shaft was not retrieved at this stage, to provide support for the guiding catheter to advance through the deployed stent more easily. Its coaxial placement within the guiding catheter also meant a lower risk of dislodging plaques protruding through the stent cells. In patient 1, the guiding catheter was also used as the retrieval apparatus for both the stent delivery and the embolic protection devices, simplifying the steps for EPD retrieval, thus shortening the total time needed for revascularization. Malik et al.’s study16 reported a distal embolic rate of 3.9%, with most, but not all, of their 77 patients treated using an EPD. However, the study did not comment on whether distal embolic events occurred more commonly in those patients treated without the use of an EPD.16 In a study by Mpotsaris et al.,10 an EPD was not used in the nine patients with tandem occlusions of the ICA and MCA. There was no mention of distal embolic events as complications in the study.10 However, we think that the use of EPD is important, as it can protect against emboli to the anterior cerebral artery, which provides important pial collateral supply for the territory induced ischemic by the MCA occlusion.
The largest case series on endovascular treatment for tandem occlusion was by Malik et al.16 on 77 patients treated using the antegrade approach, but stent retrievers were not available at the time of that study. Instead, various other mechanical devices and intra-arterial thrombolysis were used. All the patients had successful proximal recanalization. A final Thrombolysis in Myocardial Infarction (TIMI) score of ≥2 was achieved in 57.7% and 78.8% of patients having an ICA terminus and M1 occlusion as their distal occlusion, respectively.16 The largest case series on using stent retrievers for distal thrombectomy following stenting for the proximal lesion was by Cohen et al.,8 with complete recanalization and perfusion (TIMI 3/TICI 2b) achieved in 79% of their 24 patients, and another 13% having complete recanalization but partial perfusion (TIMI 3/TICI 2a); 76% of patients had mRS ≥ 2 at 3 months. There were no technical complications.8
Some studies adopted the retrograde approach with or without prior proximal angioplasty, first tackling the distal lesion, which is regarded to be the cause of the cerebral ischemia, to restore perfusion to the at-risk tissue as early as possible.18–20 However, this approach has an increased risk of reocclusion even after initial successful mechanical thrombectomy due to the possibility of distal embolization from the untreated proximal carotid lesion, relative blood stasis due to decreased forward blood flow, and the possibility of further endothelial damage caused by devices moving against the untreated exposed atherosclerotic plaque. An untreated proximal lesion would also impede the delivery of the guiding catheter to a more distal position to provide support. The dissection and subsequent occlusion in patient 2 might have been avoided had the proximal lesion been treated first. The antegrade approach seemed to be the more favored approach amongst the reported case series due to the above-mentioned considerations.8,19
Our second patient was noted to have delayed MCA recanalization on follow-up imaging, despite only the proximal carotid occlusion being successfully recanalized during the operation, with satisfactory functional outcome on follow-up. Spontaneous recanalization was observed on serial Transcranial Colour Doppler (TCD) in 18% of patients within 6 hours and 52% after 6 hours in one study.21 In Loh et al.’s study of patients with tandem occlusions and residual obstruction of the M1 segment following endovascular revascularization, 58.3% (seven patients) in the group with partial proximal recanalization had endogenous M1 recanalization within the subsequent 24 hours, mostly within 5 hours, though none of the patients without any initial proximal recanalization had endogenous recanalization.22 It was postulated that the primary restoration of proximal ICA flow augments antegrade perfusion pressure and collateral flow, thereby increasing the likelihood of circulation of endogenous plasminogen activator and fresh substrate across the residual thrombus in the M1 segment, facilitating M1 recanalization. Loosening of the MCA thrombus after mechanical thrombectomy might also make the occlusion more liable to spontaneous lysis. The possibility of spontaneous recanalization of the distal occlusion is another reason why the antegrade approach is more favored amongst the published case series of tandem occlusion treatment.
There is no established consensus on the peri-operative antiplatelet regimen for emergency stenting for acute stroke. In Mpotsaris et al.’s study, patients were given eptifibatide rather than oral antiplatelets at the time of intervention, as it has a shorter half-life. Patients were switched to dual oral antiplatelets post-operatively after confirmation of no bleed or malignant cerebral edema.20 Malik et al. adopted a similar approach initially (43 patients), but later changed to just giving aspirin and clopidogrel before stenting, without eptifibatide (34 patients).16 No increased risk of symptomatic intracerebral hemorrhage (sICH) was observed with the use of glycoprotein IIb/IIIa inhibitors in these two studies.16,20 However, Heck and Brown’s study reported a higher sICH rate in their 13 patients given intraoperative intravenous abciximab (31%) compared with the 10 patients not given this treatment (10%). All patients were loaded with aspirin pre-stenting and clopidogrel post-intervention.23 In Cohen et al.’s study,8 only oral antiplatelets were given – a loading dose of aspirin intra-operatively and a loading dose of clopidogrel post-operatively. Six of 24 patients had petechial hemorrhages.8 None of these studies reported acute stent thrombosis. It would be difficult to make comparisons between studies due to the small sample size of the studies and the differences in time from symptom onset to recanalization, the regimens and timing of giving antiplatelet therapies, and whether systemic heparin, intravenous or intra-arterial thrombolytics were given.
Conclusion
Our case reports describing two different approaches for the recanalization of tandem occlusions of the ICA and MCA, one with an antegrade and the other with a retrograde approach, showed that tandem occlusions can be treated by the combined use of stent angioplasty and mechanical thrombectomy. Although we cannot conclude, with only two patients in this report, which is the better sequence for intervention, our experience suggests that the proximal-to-distal approach is feasible. With technical modifications according to the vessel and lesion characteristics, such as using EPDs, placing the guiding catheter along the shaft of the stent past the carotid stent and using the guiding catheter to retrieve the EPD, thus shortening the time to recanalization, a good technical and functional outcome can be obtained for what has in the past been a diagnosis with a grave prognosis.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
None.
References
- 1.Rubiera M, Ribo M, Delgado-Mederos R, et al. Tandem internal carotid artery/middle cerebral artery occlusion: An independent predictor of poor outcome after systemic thrombolysis. Stroke 2006; 37: 2301–2305. [DOI] [PubMed] [Google Scholar]
- 2.Christou I, Helberg RA, Demchuk AM, et al. Intravenous tissue plasminogen activator and flow improvement in acute ischemic stroke patients with internal carotid artery occlusion. J Neuroimaging 2002; 12: 119–123. [DOI] [PubMed] [Google Scholar]
- 3.Kim DJ, Kim DI, Byun JS. Intra-arterial thrombolytic therapy for hyperacute ischemic stroke caused by tandem occlusion. Cerebrovasc Dis 2008; 26: 184–189. [DOI] [PubMed] [Google Scholar]
- 4.Ozdemir O, Bussière M, Leung A, et al. Intra-arterial thrombolysis of occluded middle cerebral artery by use of collateral pathways in patients with tandem cervical carotid artery/middle cerebral artery occlusion. Am J Neuroradiol 2008; 29: 1596–1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bulsara KR, Ediriwickrema A, Pepper J, et al. Tissue plasminogen activator via cross-collateralization for tandem internal carotid and middle cerebral artery occlusion. World J Clin Cases 2013; 1: 290–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): A randomised, parallel-group, non-inferiority trial. Lancet 2012; 380: 1241–1249. [DOI] [PubMed] [Google Scholar]
- 7.Nogueira RG, Lutsep HL, Gupta R, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): A randomised trial. Lancet 2012; 380: 1231–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen JE, Gomori JM, Rajz G, et al. Extracranial carotid artery stenting followed by intracranial stent-based thrombectomy for acute tandem occlusive disease. J Neurointerv Surg 2014; 7: 412–417. [DOI] [PubMed] [Google Scholar]
- 9.Stampfl S, Ringleb PA, Möhlenbruch M, et al. Emergency cervical internal carotid artery stenting in combination with intracranial thrombectomy in acute stroke. Am J Neuroradiol 2014; 35: 741–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mpotsaris A, Bussmeyer M, Buchner H, et al. Clinical outcome of neurointerventional emergency treatment of extra- or intracranial tandem occlusions in acute major stroke: Antegrade approach with wallstent and solitaire stent retriever. Clin Neuroradiol 2013; 23: 207–215. [DOI] [PubMed] [Google Scholar]
- 11.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 12.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 13.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. [DOI] [PubMed] [Google Scholar]
- 14.Saver JL, Goyal M, Bonafe A, et al. Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke. N Engl J Med. Epub ahead of print 17 Apr 2015. DOI: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 15.Jayaraman MV, Hussain MS, Abruzzo T, et al. Embolectomy for stroke with emergent large vessel occlusion (ELVO): Report of the Standards and Guidelines Committee of the Society of NeuroInterventional Surgery. J Neurointerv Surg 2015; 7: 316–321. [DOI] [PubMed] [Google Scholar]
- 16.Malik AM, Vora NA, Lin R, et al. Endovascular treatment of tandem extracranial/intracranial anterior circulation occlusions: Preliminary single-center experience. Stroke 2011; 42: 1653–1657. [DOI] [PubMed] [Google Scholar]
- 17.Spiotta AM, Lena J, Vargas J, et al. Proximal to distal approach in the treatment of tandem occlusions causing an acute stroke. J Neurointerv Surg 2015; 7: 164–169. [DOI] [PubMed] [Google Scholar]
- 18.Cohen JE, Gomori M, Rajz G, et al. Emergent stent-assisted angioplasty of extracranial internal carotid artery and intracranial stent-based thrombectomy in acute tandem occlusive disease: Technical considerations. J Neurointerv Surg 2013; 5: 440–446. [DOI] [PubMed] [Google Scholar]
- 19.Puri AS, Kühn AL, Kwon HJ, et al. Endovascular treatment of tandem vascular occlusions in acute ischemic stroke. J Neurointerv Surg 2015; 7: 158–163. [DOI] [PubMed] [Google Scholar]
- 20.Machi P, Lobotesis K, Maldonado IL, et al. Endovascular treatment of tandem occlusions of the anterior cerebral circulation with solitaire FR thrombectomy system. Initial experience. Eur J Radiol 2012; 81: 3479–3484. [DOI] [PubMed] [Google Scholar]
- 21.Molina CA, Montaner J, Abilleira S, et al. Timing of spontaneous recanalization and risk of hemorrhagic transformation in acute cardioembolic stroke. Stroke 2001; 32: 1079–1084. [DOI] [PubMed] [Google Scholar]
- 22.Loh Y, Liebeskind DS, Shi ZS, et al. Partial recanalization of concomitant internal carotid-middle cerebral arterial occlusions promotes distal recanalization of residual thrombus within 24 h. J Neurointerv Surg 2011; 3: 38–42. [DOI] [PubMed] [Google Scholar]
- 23.Heck DV, Brown MD. Carotid stenting and intracranial thrombectomy for treatment of acute stroke due to tandem occlusions with aggressive antiplatelet therapy may be associated with a high incidence of intracranial hemorrhage. J Neurointerv Surg. 2015; 7: 170–175. [DOI] [PubMed] [Google Scholar]