Abstract
We report this case to increase the awareness of magnetic resonance imaging (MRI) features of reversible white matter abnormalities in diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) maps in a patient with traumatic brain injury (TBI). An eight-year-old girl, who was hit by a truck, was brought to the emergency department by the emergency medical service (EMS). Eleven days later, she experienced cognitive impairment requiring MRI evaluation. DWI and ADC maps showed restricted diffusion in the white matter of the corpus callosum, peri-atrial white matter, and in the right centrum semiovale. There were no significant hemorrhagic foci in these regions, which showed complete resolution on follow up DWI MRI 13 days later. This reported case revealed TBI-related transient reversible intramyelinic cytotoxic edema.
Keywords: Traumatic brain injury, reversible diffusion restriction, cytotoxic edema
Introduction
Trauma is the leading cause of death and disability in the USA for individuals less than 45 years of age where more than 50% of deaths are related to head injury.1 Traumatic brain injury (TBI) occurs when an external mechanical force results in tissue and cellular damage that may lead to permanent or temporary impairment of cognitive, physical, or psychological function and diminished or altered state of consciousness.2 Diffusion Weighted Imaging (DWI) and Apparent Diffusion Coefficient (ADC) maps and diffusion tensor imaging (DTI) provide the best information on mobility and diffusivity of water molecules in tissues, and assess fiber’s connectivity. These imaging techniques have improved the detection of traumatic axonal injury (TAI), characterization of its neuropathology, and evaluation of relative prognosis.3 DTI is an imaging technique acquired on a standard magnetic resonance imaging (MRI) scanner that has been shown to be more sensitive for white matter injury than conventional MRI. It is based on the characteristic of myelin sheaths and cell membranes of white matter tracts that restrict the movement of water molecules, reflecting myelin integrity in vivo.2 This case is reported to emphasize MRI, DWI and ADC maps showed rare transient white matter cytotoxic edema as reversible DW abnormalities in a child who presented with mild traumatic brain injury.
Case report
An eight-year-old girl who was hit by a truck was brought by the emergency medical service (EMS) to the Emergency Department of the Alberta Children’s Hospital, Calgary, Canada. The Glasgow-Coma-Scale (GCS) was 5/15 when EMS team attended the scene. She suffered polytrauma with TBI resulting in intubation and was ventilated for the first two days. The computed tomography (CT) scan showed a depressed right parietal bone fracture with subarachnoid hemorrhage requiring neurosurgical intervention. Her GCS improved dramatically up to 15/15 on the sixth day. Eleven days later, she experienced cognitive impairment rendering a MRI scan necessary. This was done on a 1.5 T Siemens scanner which revealed the depressed fracture and subarachnoid hemorrhage with counter coup injury. DWI (Ech-Planar Imaging-Spin Echo (EPI-SE): Repetition Time (TR) 3100, Echo Time (TE) 76, slice thickness 5, b value = 0, 500 and 1000) and ADC maps showed restricted diffusion involving the corpus callosum, peri-atrial white matter, and right centrum semiovale. No significant hemorrhagic foci were seen on Susceptibility Weighted Imaging (SWI) (TR 48, TE 40 slice thickness 2) (Figure 1). The ADC values ranged from 0.24–0.34 × 10−3 mm2/s. On follow-up MRI scan 13 days later, there was complete resolution of the described abnormal DWI/ADC-restriction areas (Figure 2). Only a residual subtle area of gliosis in the splenium of corpus callosum was seen on T2-weighted images.
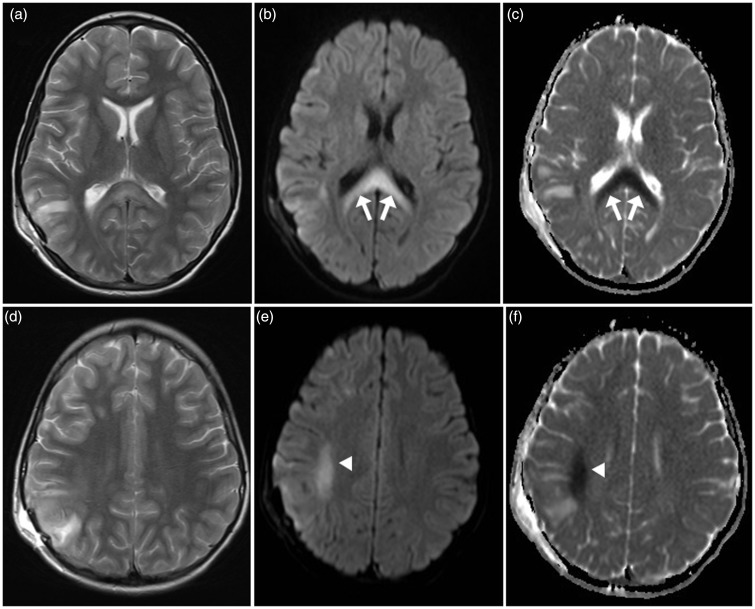
Figure 1.
Initial magnetic resonance imaging (MRI) at presentation: Axial T2 (a) and (d) show high signal intensity in corpus callosum and subcortical region of right parietal lobe. Axial diffusion-weighted imaging (DWI) (b) and (e) and apparent diffusion coefficient (ADC) maps (c) and (f) show restricted diffusion in the corpus callosum (arrows) and in subcortical white matter in the right centrum semiovale (arrowheads).
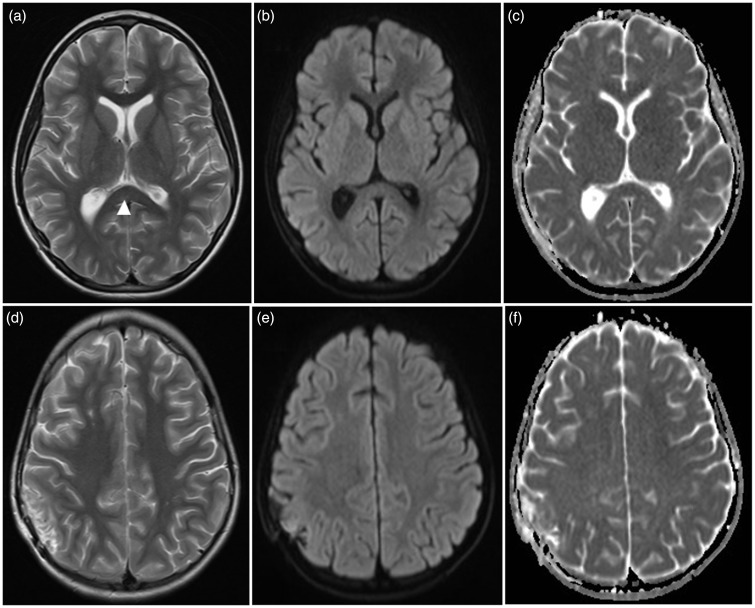
Figure 2.
Follow up imaging 13 days after initial magnetic resonance imaging (MRI). Axial T2 (a) and (d) show residual subtle T2 high signal intensity in the corpus callosum (arrowhead) denoting residual gliosis. Axial diffusion-weighted imaging (DWI) (b) and (e) and apparent diffusion coefficient (ADC) maps (c) and (f) show complete resolution of the previously seen restricted diffusion abnormalities in corpus callosum and right centrum semiovale.
Discussion
Trauma and traumatic brain injury is one of the major etiologies leading to short and long-term disability in which children and adolescents are frequently involved. It has been the focus of research for the last few decades. An exact and complete radiological work-up of patients with TBI is mandatory in guiding acute treatment to prevent or limit secondary injury. However, CT and MRI tend to underestimate the extent of diffuse axonal injury. Studies have shown progressive global cerebral atrophy on follow up after initial imaging did not show pathology or only discrete findings.1 Various disease processes result in either vasogenic or cytotoxic brain edema. DWI is an MRI technique in which images are extremely sensitive to random microscopic motions of water molecules which can define types of edema in various conditions.4 Low signal intensity in DWI and increased ADC values correspond to increased movement of water molecules in the extracellular space, i.e. increased diffusion. This finding reflects vasogenic edema which is usually reversible. High signal intensity on DWI and decreased ADC values correspond to a decreased movement of highly mobile extracellular water molecules due to their shifting into the intracellular compartment, i.e. restricted diffusion. This restricted diffusion reflects the cellular edema, which is considered to result in an irreversible lesion and cellular death. Cellular edema and swelling associated with ischemia has been designated as ‘cytotoxic’. When cellular edema and swelling occurs without ischemia, it may be defined as ‘neurotoxic’.3
Excitotoxic brain injury is considered a final common pathway for various neuropathologic conditions and causes cytotoxic edema.3,5 Glutamate, aspartate, and glycine are the dominant excitatory amino acids and the peripheral neurotransmitters in about half of all synapses in the brain. Glutamate is the most important and responsible for many neurologic functions including cognition, memory, movement and sensation. In pathologic conditions, glutamate mediates neurological injury or neuronal death, particularly through the activation of N-methyl-D-aspartate (NMDA) receptor subtypes of glutamate receptors.5 Axonal damage often occurs at the node of Ranvier, a short interval between the myelin sheaths, resulting in traumatic defect in the axonal membrane. This defect allows the leakage of glutamate into the extracellular space. The astrocytic end-foot is located on the axons at the node of Ranvier and may protect the axons.5
Few reported cases with similar findings reveal transient reversible white matter cytotoxic edema following traumatic brain injury. Hideichi et al. reported the first case of trauma-related transient cytotoxic edema involving the corpus callosum in a 24-year-old male.4 Muttikkal and his colleagues reported reversible diffusion weighted abnormalities in a 27-year-old female two weeks following trauma.6 These changes were attributed to demyelination either due to the trauma itself or following brain edema. Variant osmotic myelinolysis was proposed as a third possibility.6 The most recent case of reversible white matter restricted diffusion abnormalities following traumatic brain injury was an 18-year old male whose MRI showed cytotoxic edema in the subcortical white matter of bilateral centrum semiovali and in the splenium of corpus callosum.3
To the best of the authors’ knowledge, the patient reported on here is the youngest reported case of post-traumatic reversible white matter restricted diffusion abnormalities. However, the changes on DWI-MRI of this eight-year old girl have resolved completely with no residual imaging abnormalities in follow-up scanning. An interesting note is the involvement of the corpus callosum in most of these cases, except for the case reported by Muttikkal et al.6 All of the scans show complete resolution after clinical stabilization. This finding emphasizes that the NMDA-receptors are abundant in the corpus callosum leading to the expected sequel of intracellular calcium entry.
Several hypotheses have been proposed by Muccio et al. for the presence of white matter cytotoxic edema in traumatic brain injury.3 They include axonal damage with release of glutamate, cellular edema, microscopic hemorrhages with membrane fragmentation, post-traumatic demyelination, hypoxia, and hypotension mimicking trauma-related ischemia. In this case, a possible pathophysiologic explanation might be the presence of subtle focal corpus callosum injury which results in release of glutamate in the surrounding fibers and in the right side of centrum semiovale. The excessive extracellular glutamate is taken by the myelin sheath and the astrocyte resulting in intramyelinic edema. These cells protect the axon from death due to the abundant intracellular glutamate leading to reversibility. The residual focal area of gliosis on follow up T2-weighted images probably represents the initial subtle area of injury. The absence of hemosiderin deposition in SWI precludes diffuse axonal injury microhemorrhages as a cause for the cytotoxic edema. The extent and distribution of the DWI abnormality does not confine to an arterial territory rendering trauma-related vascular ischemia unlikely.
Conclusion
Transient reversible intramyelinic white matter cytotoxic edema is a rare entity that can occur in traumatic brain injury. Diffusion-weighted MRI would be helpful to detect the abnormality and to document the reversibility.
Acknowledgment
This case was presented electronically in the 52nd annual meeting of American Society of North America that was held during the period from 19–22 May 2014 in Montreal, Canada. The authors appreciate the help of Lauran Cole who gave valuable input in editing this paper.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
None declared.
References
- 1.Hergan K, Schefer PW, Sorensen AG, et al. Diffusion-weighted MRI in diffuse axonal injury of the brain. Eur Radiol 2002; 12: 2536–2541. [DOI] [PubMed] [Google Scholar]
- 2.Maxwell WL. Traumatic brain injury in the neonate, child and adolescent human: An overview of pathology. Int J Devl Neurosci 2012; 30: 167–183. [DOI] [PubMed] [Google Scholar]
- 3.Muccio CF, De Simone M, Esposito G, et al. Reversible post-traumatic bilateral extensive restricted diffusion of the brain. A case study and review of the literature. Brain Inj 2009; 23: 466–472. [DOI] [PubMed] [Google Scholar]
- 4.Takayama H, Kobayashi M, Sugishita M, et al. Diffusion-weighted imaging demonstrates transient cytotoxic edema involving the corpus callosum in a patient with diffuse brain injury. Clin Neurol Neurosurg 2000; 102: 135–139. [DOI] [PubMed] [Google Scholar]
- 5.Moritani T, Smoker WR, Sato Y, et al. Diffusion-weighted imaging of acute excitotoxic brain injury. AJNR Am J Neuroradiol 2005; 26: 216–228. [PMC free article] [PubMed] [Google Scholar]
- 6.Muttikkal TJ, Ashebu SD, Ben-Nakhl A, et al. Isolated bilateral pyramidal tract lesions? An unusual case of demyelination following trauma, a case report. Neuroradiol J 2008; 21: 817–823. [DOI] [PubMed] [Google Scholar]