Abstract
Background
The WEB device is a recent intrasaccular flow disruption technique developed for the treatment of wide-necked intracranial aneurysms. To date, a single report on the WEB Single-Layer (SL) treatment of intracranial aneurysms has been published with 1-months' safety results. The aim of this study is to report our experience and 6-month clinical and angiographic follow-up of endovascular treatment of wide-neck aneurysm with the WEB SL.
Methods
Ten patients with 10 unruptured wide-necked aneurysms were prospectively enrolled in this study. Feasibility, intraoperative and postoperative complications, and outcomes were recorded. Immediate and 6-month clinical and angiographic results were evaluated.
Results
Failure of WEB SL placement occurred in two cases. Eight aneurysms were successfully treated using one WEB SL without additional treatment. Three middle cerebral artery, four anterior communicating artery, and one basilar artery aneurysms were treated. Average dome width was 7.5 mm (range 5.4–10.7 mm), and average neck size was 4.9 mm (range 2.6–6.5 mm). No periprocedural complication was observed, and morbi-mortality at discharge and 6 months was 0.0%. Angiographic follow-up at 6 months demonstrated complete aneurysm occlusion in 2/8 aneurysms, neck remnant in 5/8 aneurysms, and aneurysm remnant in 1/8 aneurysm.
Conclusions
From this preliminary study, treatment of bifurcation intracranial aneurysms using WEB SL is feasible. WEB SL treatment seems safe at 6 months; however, the rate of neck remnants is not negligible due to compression of the WEB SL. Further technical improvements may be needed in order to ameliorate the occlusion in the WEB SL treatment.
Keywords: Intracranial aneurysms, endovascular treatment, WEB device, outcome
Introduction
Wide-necked intracranial aneurysms were originally thought to be either untreatable or very challenging to treat by endovascular coiling because of the risk of coil protrusion into the parent vessel.1 In this situation, various endovascular devices such as balloons and stents have been developed.2–4 However, treatment of these aneurysms is associated with low rates of initial angiographic occlusion and high rates of recurrence.1,2,5–7 The WEB (Sequent Medical, Aliso Viejo, CA) is an intrasaccular braided device that disrupts the flow in the aneurysmal neck, by which it promotes aneurysmal thrombosis. Several types of WEB devices are currently available. The WEB Dual-Layer (DL), which is made of two layers held together, creating two compartments, seems to be a promising device for the endovascular treatment of intracranial aneurysms with unfavorable anatomy such as a wide neck.8–15 With their double layers, WEB DL devices contain 216 or 288 total wires, depending on device size. A given WEB DL contains two or three different-diameter wires braided into the device in a proprietary process called MicroBraid. Contrary to WEB DL, the WEB Single-Layer (SL)/Single-Layer Spheric (SLS) is a single layer device creating only one compartment. WEB SL/SLS, which received CE Mark in 2013, represents an evolution of the MicroBraid technology. Markedly different from the WEB DL, the WEB SL and SLS devices vary from 144 wires in 4-mm-diameter devices up to 216 wires in 11-mm-diameter devices. With a more spherical shape, WEB SLS is designed to treat ≈1.5–2 dome-to-neck-ratio aneurysms and aneurysms with V-shaped or tapered necks. The increasing wire count in a single, braided layer-combined with multiple wire diameters-allows the WEB SL and SLS to achieve rapid contrast stasis and to balance radial force with conformability. This uniform response may be important clinically in that small and large WEB devices must have an appropriate radial force to remain where they are deployed (i.e. WEB radial force is greater than the parent artery blood flow force) but must remain soft enough to conform safely to the aneurysm (i.e. WEB radial force is less than the compressive force on the aneurysm from the subarachnoid space). In addition, the WEB SL and SLS can be placed through a small diameter microcatheter. To date, a single published paper on an aneurysm treated with WEB SL/SLS reported its safety and efficacy at 1 month.15
The purpose of this study is to report our preliminary experience and 6-month clinical and anatomic results in the treatment of intracranial aneurysms with the WEB SL/SLS device.
Material and methods
Registry
All patients treated in the Neurological Hospital at Lyon (France) with WEB SL device for intracranial unruptured aneurysms between August 2013 and May 2014 were prospectively included. The indication for treatment and the technique chosen (surgery or endovascular) were decided by a multidisciplinary team according to the aneurysm characteristics (size, neck, and width). In case of endovascular approach, wide-neck aneurysms were treated with intrasaccular device in first intention. The protocol was approved by the French Ethics Committee. Written informed consent was obtained from each patient or legal representative prior to entry into the study.
Endovascular procedure
The procedure was performed under general anesthesia and full heparinization. Cerebral angiograms were obtained via femoral approach. Three-dimensional angiogram was performed to determine size of dome, length and neck of the aneurysm. Device size selection was decided on by one operator and one expert from Sequent Company in all cases. As recommended by the company, WEB diameter was oversized 1 mm compared with the aneurysm maximal diameter measured on two orthogonal projections. WEB length was undersized 1 mm compared with the aneurysm length. All measurements were done by three-dimensional reconstructed images.
A Via 27 microcatheter (Sequent Medical, Aliso Viejo, CA) was then inserted coaxially over a 0.014-inch microguidewire to reach within the aneurysm. The Via 27 was used for WEB SL/SLS with a width ≤9 mm, and a Via 33 for width of ≥10 mm. After adequate positioning of the WEB device inside the aneurysmal sac, a control angiogram was performed to evaluate the position of the device and the flow stagnation inside. If the position was not satisfactory, the device was resheathed and repositioned. When the size was found to be incorrect, the device was resheathed and replaced by a different sized WEB SL. At the end of the procedure, 500 mg of aspirin were administrated intravenously. Oral aspirin (75 mg) was continued for another month in order to prevent delayed thromboembolic events due to the contact between the blood and the device covering a wide neck.
Outcome evaluation
Clinical outcomes were assessed at discharge and 1 month using the modified Rankin Scale (mRS).16 Morbidity was defined as a mRS score of more than 2.
Angiographic images were obtained in anteroposterior, lateral and working projections prior to the treatment, immediately after, and at 3- or 6-month follow-up. A simplified three-point Raymond scale (total occlusion, neck remnant, aneurysm remnant) was used to assess the final result of the procedure.6 Adequate aneurysm occlusion was defined as total aneurysm occlusion or neck remnant.
Results
Ten patients (six males and four females) harboring 10 wide-necked intracranial aneurysms were prospectively included during the study period. The mean age of these patients was 54.2 ± 8.9 years (range 41–68 years). Eight out of 10 aneurysms were successfully treated with the WEB SL. Both remaining patients were excluded from further analyses.
Three aneurysms were located at middle cerebral artery (MCA) bifurcation, four at the anterior communicating artery (AcomA), one at the basilar artery tip. On working projection, the mean width of the aneurysm sac (dome) was 7.5 ± 1.9-mm (range 5.4–10.7 mm), mean transversal diameter was 6.3 ± 1.2 mm (range 4.6–8.2 mm), and the mean diameter of aneurysm neck was 4.9 ± 1.2 mm (range 2.6–6.5 mm) (Table 1).
Table 1.
Aneurysm characteristics.
| No. | Age (years), Sex | Location | D (mm) | T (mm) | N (mm) | D/N | WEB size (mm2) | WEB type |
|---|---|---|---|---|---|---|---|---|
| 1 | 45, M | AcomA | 8.9 | 5.8 | 5.3 | 1.7 | 9 × 5 | SL |
| 2 | 59, M | MCA | 6.2 | 7.5 | 5.1 | 1.2 | 7 × 5 | SL |
| 3 | 56, M | AcomA | 7.9 | 6.9 | 2.6 | 3.0 | 7 × 5 | SL |
| 4 | 53, F | MCA | 5.7 | 4.6 | 4.7 | 1.2 | 6 × 4 | SL |
| 5 | 44, F | MCA | 8.9 | 8.2 | 6.5 | 1.4 | 8 × 4 | SL |
| 6 | 59, M | Basilar tip | 6.1 | 5.9 | 4.0 | 1.5 | 7 × 4 | SLS |
| 7 | 65, M | AcomA | 10.7 | 6.4 | 5.6 | 1.9 | 6 × 3 | SL |
| 8 | 52, F | AcomA | 4.2 | 3.5 | 1.9 | 2.2 | 4 × 3 | SL |
| 9 | 41, M | MCA | 4.3 | 4.9 | 5.3 | 0.8 | 5 × 4 | SL |
| 10 | 68, F | AcomA | 5.4 | 5.1 | 5.1 | 1.1 | 7 × 6 | SL |
AcomA indicates anterior communicating artery; MCA, middle cerebral artery; D, dome; T, transverse diameter; N, neck; SL, single layer; SLS, single layer spheric.
Feasibility
All procedures required only one WEB SL implant with no additional devices. Treatment failed in two patients (Patient 8 and 9). One patient had a left MCA bifurcation aneurysm with a 4.9 mm width a 4.3 mm dome, and a 5.1 mm neck. The WEB SL protruded into the parent artery since the device was not stable within the aneurysmal sac. A different sized WEB was tried with no success. The aneurysm was subsequently treated with stenting and coiling. In the second patient, the aneurysm was located at the ACOM with a 3.5 mm width and a 4.2 mm dome. The failure was due to the acute angle between the axis of the delivery microcatheter tip and the long axis of the aneurysm, causing the catheter tip to be too adjacent to the aneurysm wall, making it impossible for the WEB to safely deploy. The aneurysm was than treated with coiling alone.
Short-term clinical outcome
No intraoperative rupture or thromboembolic events were observed. All patients had normal neurologic examination findings at discharge, and at 1- and 6-month follow-up. The mortality and morbidity rates were 0% and 0%, respectively.
Short-term anatomic outcome
Anatomic outcome is detailed in Table 2. Immediate post-treatment angiograms showed one complete occlusion, one neck remnant, and six incomplete occlusions.
Table 2.
Clinical and angiographic outcome after WEB-SL treatment.
| No. | WEB failure | Location | Clinical results |
Angiographic results |
WEB compression | |||
|---|---|---|---|---|---|---|---|---|
| Initial | Discharge | 6 month | Immediate | 6 month | ||||
| 1 | AcomA | 0 | 0 | 0 | AR | NR | No | |
| 2 | MCA | 1 | 1 | 1 | C | AR | Yes | |
| 3 | AcomA | 0 | 0 | 0 | AR | NR | Yes | |
| 4 | MCA | 0 | 0 | 0 | AR | NR | Yes | |
| 5 | MCA | 0 | 1 | 0 | NR | NR (w) | Yes | |
| 6 | Basilar tip | 0 | 0 | 0 | AR | C | No | |
| 7 | AcomA | 0 | 0 | 0 | AR | C | No | |
| 8 | Yes | AcomA | 0 | 0 | 0 | C | C | - |
| 9 | Yes | MCA | 1 | 1 | 1 | NR | NR (w) | - |
| 10 | AcomA | 0 | 0 | 0 | AR | NR | Yes | |
AcomA indicates anterior communicating artery; MCA, middle cerebral artery; C, complete aneurysm occlusion; NR, neck remnant; AR, aneurysm remnant; w, worsening.
Angiographic follow-up at 6 months was obtained in all patients and included two complete occlusions, five neck remnants, and one incomplete aneurysm occlusion. Adequate aneurysm occlusion (total occlusion or neck remnant) was observed in 7/8 cases. No retreatment was performed.
Illustrative case 1
A 59-year-old male (patient 2, Figure 1) presented with an unruptured left middle cerebral artery aneurysm which measured 6.2 mm long with a 5.1 mm neck. Treatment was performed by 7 × 5 mm2 WEB SL placement. Immediate control angiogram revealed complete stasis of flow within the aneurysm starting at distal fundus and patency of the parent vessel. No complication was observed during the procedure and the patient was discharged after 3 days. Angiographic control at 6 months shows an aneurysm remnant. We observed a compaction of the WEB SL device at the fundus of the aneurysm.
Figure 1.
Left unruptured MCA aneurysm in a 59-year-old man (patient 2). (a) Right internal carotid angiograms, working projection, demonstrating the aneurysm arising from the right middle cerebral artery bifurcation. (b) Plain X-ray, working projection, showing the WEB SL device with proximal and distal markers. (c) Immediate control angiogram, working projection, showing the total occlusion of the MCA aneurysm. (d) Plain X-ray, working projection, showing the compaction of the device. (e) 6-month control angiogram demonstrating residual aneurysm.
Illustrative case 2
A 53-year-old male (patient 4, Figure 2) presented with an unruptured anterior communicating artery aneurysm, 10.7 mm long with 5.6 mm neck. Treatment was performed by 6 × 3 mm2 WEB SL deployed inside the aneurysm. Immediate control angiogram demonstrated complete occlusion of the aneurysm and patency of the parent vessel. The procedure was uneventful. Angiographic follow-up at 6 months revealed complete aneurysm occlusion.
Figure 2.
Anterior communicating artery aneurysm in a 65-year-old man (patient 7). (a) Left internal carotid angiogram, working projection, showing the aneurysm arising from the anterior communicating artery. (b, c) Immediate control angiogram, working projection, demonstrating good position of the device and adequate occlusion of the aneurysm (neck remnant). (d) 6-month control angiogram demonstrating complete aneurysm occlusion.
Illustrative case 3
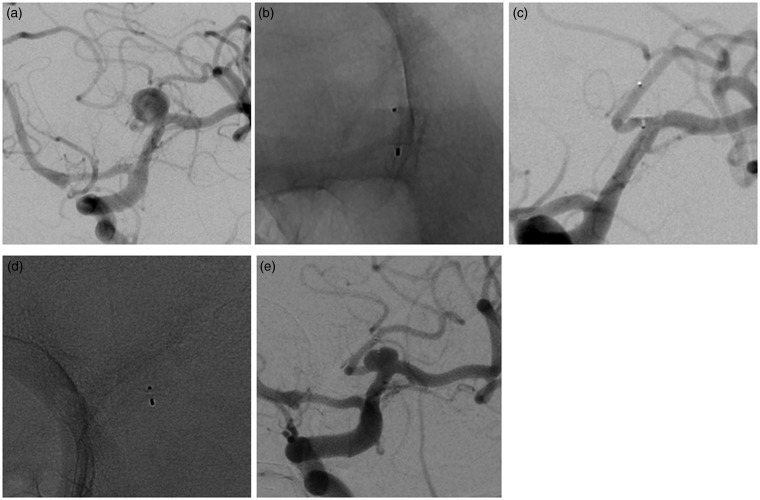
A 53-year-old woman (patient 4, Figure 3) presented with an unruptured right MCA aneurysm with unfavorable anatomy for standard endovascular treatment. Endovascular treatment was performed by WEB SL 6 × 4 mm2 placement. Final control angiogram showed an adequate placement of the WEB device. Angiographic 6-month follow-up demonstrated significant neck remnant secondary to compression of the device.
Figure 3.
Right unruptured MCA aneurysm in a 53-year-old woman (patient 4). (a) Right internal carotid angiogram, working projection, showing the aneurysm with unfavorable anatomy for standard endovascular treatment. (b, c) Final control angiogram, working projection, showing the adequate occlusion of the aneurysm (neck remnant). (d, e) 6-month follow up angiogram demonstrating significant neck remnant secondary to compaction of the device.
Discussion
This preliminary series of 10 patients shows that endovascular WEB SL/SLS flow disruption in wide-necked bifurcation aneurysms is feasible, and safe at 6-month follow-up.
Feasibility of WEB SL endovascular treatment and patient selection
We have found that treatment of intracranial aneurysms with a WEB SL/SLS device is feasible; however, selection of patients is a key element that must be taken into account before treatment, as previously reported.10 Compared with a series using the WEB DL device, our rate of failure is high, probably related to the aneurysm/patient selection. In a recent large, multicenter, prospective series, technical success was achieved in 77 patients with 79 aneurysms (92.9%).12 In a study of WEB DL flow disruption of middle cerebral artery aneurysms, the treatment failed in one of the 34 aneurysms owing to a lack of appropriate device size.13 In the series of 19 patients with 20 unruptured wide-neck bifurcation aneurysms reported by Lubicz et al.,11 failure of WEB DL placement occurred in one case because of unavailability of a suitably sized device.
The other conventional endovascular techniques, particularly intracranial stenting, present a higher success rate. In the recent prospective SOLARE study dealing with 63 patients, we reported a rate of successful stent delivery in 98.5% of cases.3 This could be related to the difficulty associated with navigation of larger WEB microcatheter within the intracranial circulation. Fortunately, the WEB SL is fully retrievable once deployed, and it may be exchanged for a more optimal device if sizing is not correct. Nevertheless, the patient selection is crucial with the WEB device. In some cases, the aneurysm planned to be treated with a WEB device could have been treated by coiling alone, as illustrated this series (one patient) or in the series of Papagiannaki et al. (one patient).12
As shown previously, one of the major risks of WEB deployment derives from the position of the microcatheter within the aneurysm sac, which can cause the distal tip of the device to immediately attach to the aneurysm wall, with a risk of procedural aneurysm perforation. It was reported in 1 out of 18 patients (5.5%) in the series of Lubicz et al.,11 and occurred in only 1 out of 77 patients (1.3%) in recent large series.12
Clinical outcome
WEB SL/SLS endovascular procedure seems a safe technique for endovascular treatment of wide-neck intracranial aneurysms. The safety profile of the WEB SL/SLS device seems to show a similar small rate as the WEB DL-related morbidity and mortality.8–15 In our small series, no procedural complications were noticed and no device-related morbi-mortality occurred. In the only report concerning WEB SL/SLS results, morbidity was similar in both groups (WEB DL, 3.3%; WEB SL/SLS, 3.1%), and mortality was 0% in both groups.15 Concerning the WEB DL, the rate of periprocedural complication was 18.7% in the European multicenter series with 34 wide-necked middle cerebral artery aneurysms.13 In 1 of the 32 patients (3.1%), intraoperative rupture was observed after the WEB was deployed in a daughter sac. In 5 out of 32 patients (15.6%), thromboembolic events were observed. In the recent series of Papagiannaki et al.,12 perioperative complications occurred in 10/77 patients (13.0%) during the treatment of 11 aneurysms and procedure-related mortality and permanent-morbidity (mRS ≤ 2) rates were 0.0% and 1.3%, respectively. These results could be explained by the fact that four patients were presented with an acute subarachnoid hemorrhage. In our series, no patients have been treated in this context. As shown previously,16,17 periprocedural complications seem to be significantly more frequent in this situation. To date, the safety profile of WEB flow disruptor in the setting of subarachnoid hemorrhage is not well known. In a small series of 6 patients with ruptured intracranial wide-necked aneurysms, procedural thromboembolic events occurred in two cases and were treated with intra-arterial administration of antiplatelet agents without any clinical consequences, and all patients have mRS 0 at discharge.17,18 It should be emphasized that one of the major advantages of WEB treatment is that a double antiplatelet therapy is not mandatory.
In the specific situation of challenging aneurysms with unfavorable anatomy at middle cerebral artery or anterior communicating artery locations, stent-assisted and balloon-assisted coiling are two well-established techniques.2–4 Compared to balloon-assisted coiling, stent-assisted coiling was found to yield higher rates of aneurysm obliteration and progression of occlusion at follow-up.16–20 However, intracranial stenting seems associated with a risk of complication, in part because of the dual antiplatelet therapy. In a recent prospective study of 120 non-selected patients with middle cerebral artery aneurysms, the odds of developing complications were 4.8 times greater when stents were used.18,19
Anatomic outcome
In this series, the WEB SL/SLS device achieved adequate aneurysm occlusion (total occlusion or neck remnant) in 7 of 8 cases (87.5%). However, the rate of neck remnants is not negligible since it represents the major type of aneurysm occlusion. To date, no data exist regarding the 6-months' efficacy of WEB SL device. Using WEB DL device, published results show superior anatomic outcomes. Papagiannaki et al. reported 92.3% rate of adequate aneurysm occlusion (total occlusion or neck remnant) after treatment of 65 aneurysms that had an imaging control (mean follow-up, 5.3 months),12 with 37 (56.9%) presented with complete occlusion, 23 (35.4%), with a neck remnant, and 5 (7.7%), with an aneurysm remnant. Lubicz et al. noted adequate occlusion in 89.5% of cases after flow disruption of 19 aneurysms (Table 3).11 Similar findings were also reported in the series of Pierot et al. dealing with 33 treated middle cerebral artery aneurysms with unfavorable anatomy.13
Table 3.
Summary of main studies looking at treatment using a WEB device.
| Study, Year | Patients/ aneurysms | Ruptured/ unruptured | Failure n(%) | Complications n(%) | Morbidity rate% | Mortality rate% | Immediate adequate occlusion% | Mean follow-up (months) | Adequate occlusion at follow-up% |
|---|---|---|---|---|---|---|---|---|---|
| Pierot et al.,14 2012 | 20/21 | 1/20 | 0 | 2/20 (10.0) | 4.8 | 0 | 60 | 5.9 | 80 |
| Lubicz et al.,11 2013 | 19/20 | 0/20 | 1/20 (5) | 2/18 (11.1) | 11.1 | 0 | 73.7 | 6 | 89.5 |
| Pierot et al.,13 2013 | 33/34 | 2/32 | 1/34 (2.9) | 6/32 (18.7) | 3.1 | 0 | - | 7.2 | 83.3 |
| Papagiannaki et al.,12 2014 | 83/85 | 4/81 | 6/85 (7.2) | 10/77 (13.0) | 1.3 | 0 | - | 5.3 | 92.3 |
| Pierot et al.,15 2015 | 62/63 | - | - | - | 0 | _ | 1 | - | |
| Lyon WEB-SL series | 10/10 | 0/10 | 2/10 (20) | 0 | 0 | 0 | 25 | 6 | 100 |
Morbidity was defined as a modified Rankin Scale (mRS) score of more than 2, and adequate aneurysm occlusion as a total occlusion or neck remnant.
Our high rate of neck remnants seems to be at least partially explained by the compression and the deformation of the WEB SL device (Figures 1 and 3). The degree of the compression of the WEB SL is being compared to the WEB DL device but in fact, since the WEB SL is only one layered compartment device, as opposed to the WEB DL, the influence of the different technology on the angiographic outcome is yet to be revealed. A long-term follow-up is still needed to evaluate the efficacy of this treatment. Although several articles have already been published, WEB device shape modification with WEB compression was rarely reported. To date, a single paper on aneurysm treated with WEB described this phenomenon.9 Same device size selection was used, as recommended by Sequent Medical. In a series of 15 consecutive large-neck bifurcation aneurysms (12 WEB DL and 3 WEB SL), a compression of the WEB cage was observed at first follow-up (3–6 months) in 8 of 14 (57.2%) and in an additional 3 of 7 cases (42.8%) at second control (18 ± 3 months).9 To date, the mechanism of the WEB compression is unclear, but may probably be related to the initial sizing of the device. It will be essential to prove if the WEB oversizing decreases the risk of compression.
Conclusion
From this preliminary study, treatment of wide-neck intracranial aneurysms using WEB SL is feasible. WEB SL treatment seems safe at 6 months; however, the rate of neck remnants is not negligible due to compression of the device. Further technical improvements may be needed in order to ameliorate the occlusion in the WEB SL treatment.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Gory B, Turjman F. Endovascular treatment of 404 intracranial aneurysms treated with nexus detachable coils: short-term and mid-term results from a prospective, consecutive, European multicenter study. Acta Neurochir 2014; 156: 831–837. [DOI] [PubMed] [Google Scholar]
- 2.Gory B, Kessler I, Seizem Nekiri G, et al. Initial experience of intracranial aneurysm embolization using the balloon remodeling technique with Scepter C, a new double-lumen balloon. Interv Neuroradiol 2012; 18: 284–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gory B, Klisch J, Bonafé A, et al. Solitaire AB stent-assisted coiling of wide-necked intracranial aneurysms: short-term results from a prospective, consecutive, European multicentric study. Neuroradiology 2013; 55: 1373–1378. [DOI] [PubMed] [Google Scholar]
- 4.Gory B, Klisch J, Bonafé A, et al. Solitaire AB stent-assisted coiling of wide-necked intracranial aneurysms: mid-term results from a prospective, consecutive, European multicentric study. Neurosurgery 2014; 75: 215–219. [DOI] [PubMed] [Google Scholar]
- 5.Linfante I, DeLeo MJ, 3rd, Gounis MJ, et al. Cerecyte versus platinum coils in the treatment of intracranial aneurysms: packing attenuation and clinical and angiographic midterm results. Am J Neuroradiol 2009; 30: 1496–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raymond J, Guilbert F, Weill A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke 2003; 34: 1398–1403. [DOI] [PubMed] [Google Scholar]
- 7.Shapiro M, Becske T, Sahlein D, et al. Stent-supported aneurysm coiling: a literature survey of treatment and follow-up. Am J Neuroradiol 2012; 33: 159–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colla R, Cirillo L, Princiotta C, et al. Treatment of wide-neck basilar tip aneurysms using the Web II device. Neuroradiol J 2013; 26: 669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cognard C, Januel AC. Remnants and recurrences after the use of the WEB intrasaccular device in large-neck bifurcation aneurysms. Neurosurgery 2015; 76: 522–530. [DOI] [PubMed] [Google Scholar]
- 10.Gherasim DN, Gory B, Sivan-Hoffmann R, et al. Endovascular treatment of wide-neck anterior communicating artery aneurysms using WEB-DL and WEB-SL: short-term results in a multicenter study. Am J Neuroradiol. Epub ahead of print 19 March 2015. DOI:10.3174/ajnr.A4282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lubicz B, Mine B, Collignon L, et al. WEB device for endovascular treatment of wide-neck bifurcation aneurysms. Am J Neuroradiol 2013; 34: 1209–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papagiannaki C, Spelle L, Januel AC, et al. WEB intrasaccular flow disruptor-prospective, multicenter experience in 83 patients with 85 aneurysms. Am J Neuroradiol 2014; 35: 2106–2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pierot L, Klisch J, Cognard C, et al. Endovascular WEB flow disruption in middle cerebral artery aneurysms: preliminary feasibility, clinical, and anatomical results in a multicenter study. Neurosurgery 2013; 73: 27–34. [DOI] [PubMed] [Google Scholar]
- 14.Pierot L, Liebig T, Sychra V, et al. Intrasaccular flow-disruption treatment of intracranial aneurysms: preliminary results of a multicenter clinical study. Am J Neuroradiol 2012; 33: 1232–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pierot L, Moret J, Turjman F, et al. WEB treatment of intracranial aneurysms: feasibility, complications, and 1-month safety results with the WEB DL and WEB SL/SLS in the French observatory. Am J Neuroradiol 2015; 36: 922–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonita R, Beaglehole R. Recovery of motor function after stroke. Stroke 1988; 19: 1497–1500. [DOI] [PubMed] [Google Scholar]
- 17.Bodily KD, Cloft HJ, Lanzino G, et al. Stent-assisted coiling in acutely ruptured intracranial aneurysms: A qualitative, systematic review of the literature. Am J Neuroradiol 2011; 32: 1232–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caroff J, Mihalea C, Dargento F, et al. Woven Endobridge (WEB) device for endovascular treatment of ruptured intracranial wide-neck aneurysms: A single-center experience. Neuroradiology 2014; 56: 755–761. [DOI] [PubMed] [Google Scholar]
- 19.Gory B, Rouchaud A, Saleme S, et al. Endovascular treatment of middle cerebral artery aneurysms for 120 nonselected patients: A prospective cohort study. Am J Neuroradiol 2014; 35: 715–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chalouhi N, Starke RM, Koltz MT, et al. Stent-assisted coiling versus balloon remodeling of wide-neck aneurysms: comparison of angiographic outcomes. Am J Neuroradiol 2013; 34: 1987–1992. . [DOI] [PMC free article] [PubMed] [Google Scholar]