Abstract
Radiofrequency ablation is a valuable therapy for palliation of painful spinal metastases and local tumor control; however, accessing the vertebral body can be difficult and time consuming with traditional manual needles. Herein, we report our initial experience using a drill-assisted, fluoroscopy-guided technique for accessing the vertebral body for radiofrequency ablation.
Keywords: OnControl, drill system, radiofrequency ablation, spinal metastases
Introduction
Radiofrequency ablation (RFA) is an emerging therapy for palliation of painful spinal metastases and local tumor control.1–4 The ablation probe is percutaneously inserted into the vertebral body from a posterior approach by creating channels through one or both pedicles, and high-frequency alternating current is passed through the probe to generate cytotoxic thermal temperatures. The vertebral body has traditionally been accessed with serrated needles that are manually advanced through bone with a combination of forward pressure and rotation. However, it can be difficult to use this technique to access vertebrae previously treated with radiation therapy, because radiation induces sclerosis of normal bone surrounding the tumor. The spines of younger patients with vertebral body metastases and uninvolved pedicles of normal bone density can be similarly challenging to access. A mallet can be used to help drive the needle through dense bone, but control over the needle trajectory is compromised. This technique is also painful and often not tolerated by consciously sedated patients. As an alternative, we have begun using a battery-powered hand drill (OnControl System; Vidacare Corporation, Shavano Park, TX, USA) to access vertebrae for fluoroscopy-guided RFA. Herein, we report our initial experience with this novel technique.
Methods
Institutional review board approval was obtained to retrospectively review the electronic medical records of all patients who underwent RFA of spinal metastases between June 2012 and October 2014. Cases in which drill assistance was used to gain access to a vertebral body with fluoroscopic guidance were identified. Recorded data included patient age and gender, primary tumor histology, vertebra(e) treated, and timing of radiation therapy with respect to ablation. Procedural notes were reviewed to determine the percutaneous approach used to access the vertebral body (i.e. uni- versus bipedicular). Complications were recorded according to the Society of Interventional Radiology Standards of Practice Committee guidelines.
The OnControl System
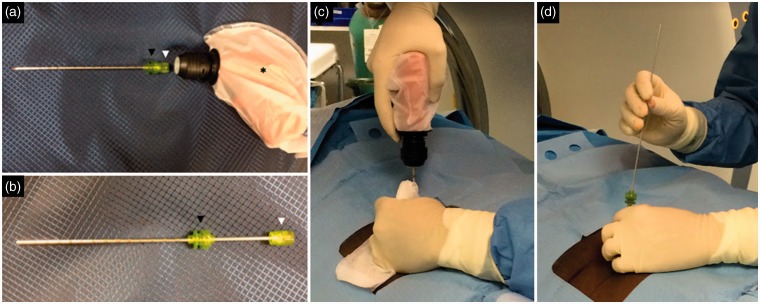
The OnControl System uses a battery-powered handheld drill and coaxial needle set. Each sterile tray includes an outer cannula, diamond-tipped inner needle for cutting through bone, hollow biopsy needle, and sterile cover for the reusable drill (Figure 1). A 10-gauge, 10-cm outer cannula and 12-gauge inner needle are used for vertebral body access. Depending on patient size, 10- or 15-cm long needle sets are typically used.
Figure 1.
(a) The reusable drill (black asterisk) is enclosed in a sterile cover provided with the needle tray. The coaxial outer cannula (black arrowhead) and inner needle (white arrowhead) are locked and ready to engage with the drill. (b) The outer cannula (black arrowhead) and inner needle (white arrowhead) have been unlocked and the inner needle partially removed. (c) The outer cannula and inner needle are locked and engaged with the drill. The right hand is holding the drill and depressing a trigger that causes the locked outer cannula and inner needle to rotate. The left hand is helping to guide the trajectory of the coaxial cannula and needle. A piece of gauze is held in the left hand to prevent the glove from being “wound up” around the rotating outer cannula. (d) The inner needle has been unlocked and removed from the outer cannula and replaced with a K-wire. The outer cannula of the OnControl system can now be exchanged over the K wire for the outer cannula of the tumor ablation system.
Vertebral body access
Written informed consent was obtained prior to all procedures. Patients were positioned prone on the fluoroscopy table and given intravenous midazolam and fentanyl for conscious sedation. An oblique view was obtained to view the pedicle en face. The skin, soft tissues, and periosteum overlying the pedicle were anesthetized with a 50/50 mixture of 1% lidocaine and 0.25% bupivacaine. A 5-mm skin incision was made and the coaxial diamond-tipped inner needle and outer cannula were manually advanced through the soft tissues until purchase was made in the posterior vertebral cortex. A lateral view was then obtained to verify that the trajectory of the needle matched that of the pedicle. The needle was then attached to the drill and advanced on the anterior-posterior (AP) view making sure that the needle tip remained lateral to the medial cortex of the pedicle. Once the vertebral body was accessed, the inner needle was exchanged for a K-wire, over which the outer cannulae of the OnControl and tumor ablation systems were exchanged (Figures 1 and 2).
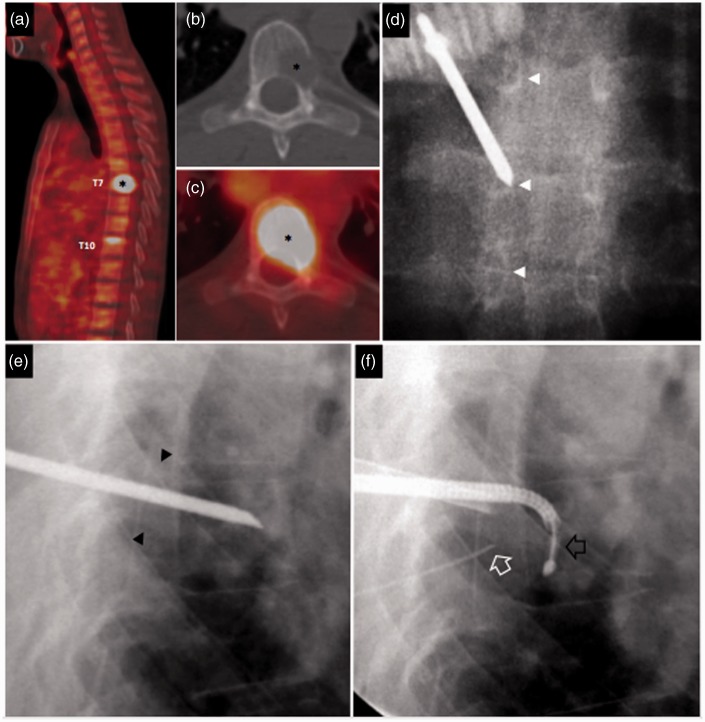
Figure 2.
A 33-year-old man with Ewing sarcoma and progressively worsening upper back pain despite receiving 20 Gy of radiation therapy in five fractions. Drill-assisted access was needed because of radiation-induced sclerosis of young, non-osteoporotic bone. (a) Sagittal positron emission tomography-computed tomography (PET-CT) shows an 18F-fluorodeoxyglucose (FDG) avid T7 metastasis corresponding to the site of his pain (black asterisk), and a smaller, asymptomatic T10 metastasis. Axial CT (b) and PET-CT (c) images show lytic destruction of the posterolateral T7 vertebral body and left pedicle by this FDG-avid metastasis (black asterisks). Anterior-posterior (d) and lateral (e) fluoroscopic images show the drill-assisted access needle within the T7 vertebral body via a transpedicular approach. Caution was exercised to ensure that the medial cortex of the pedicle (white arrowhead) and superior and inferior walls of the pedicle (black arrowheads) were not violated. When the medial cortex of the pedicle is difficult to see, the pedicles above and below can be used for reference (white arrowheads). The vertebral body was also accessed from the right vertebral body. (f) Lateral fluoroscopic image shows the radiofrequency ablation probe (black block arrow) curving into the posterior vertebral body. A 22-gauge spinal needle was placed through the neural foramen into the epidural space (white block arrow), through which dextrose 5% in water was instilled to cool the spinal cord and nerves.
Results
During the study period, drill assistance was used to access eight vertebral body metastases for RFA in seven patients. Individual patient details are presented in Table 1. The mean age of the cohort was 60.3 ± 16.0 years. In patients 4, 5, and 6, drill assistance was used because failed radiation therapy had caused sclerosis of the target vertebral body. In patient 7, two lesions were treated as part of a single procedure, and drill assistance facilitated faster access to both vertebral bodies. Patients 1, 2, and 3 were treated more recently, and drill assistance was employed at the preference of the interventionalist. A unipedicular approach was used to access the vertebral body of patient 1. All other treated vertebrae were accessed from a bipedicular approach. There were no complications from any of the procedures.
Table 1.
Cohort summary.
| Patient no/ age (y)/sex | Tumor location | Primary tumor histology |
|---|---|---|
| 1/76/W | L1 | Unknown |
| 2/39/M | T8 | Malignant peripheral nerve sheath tumor |
| 3/60/M | L2 | Pharyngeal squamous cell carcinoma |
| 4/77/M | L3 | Lung adenocarcinoma |
| 5/52/M | L5 | Renal cell carcinoma |
| 6/33/M | T7 | Ewing sarcoma |
| 7/72/M | T11, L2 | Melanoma |
y: years; W: woman; M: man.
Discussion
Percutaneous RFA is a valuable option for pain and local control of spinal metastases when traditional therapies are ineffective or contraindicated. Several case series have shown relief of metastatic bone pain after RFA,1–4 including a multicenter, retrospective study of 128 spinal metastases, in which pre-procedure pain scores (7.51/10 ± 2.46) decreased at one week (1.73/10 ± 2.28; p < 0.0001), one month (2.25/10 ± 2.44; p < 0.0001), and six months (1.75 ± 2.62; p = 0.009) after treatment.1 Important advantages of percutaneous RFA are that it can be performed under conscious sedation, requires minimal recovery, and does not hinder or delay radiation therapy or systemic chemotherapy.
Percutaneously accessing the vertebral body for RFA of spinal metastases poses unique challenges in comparison with other minimally invasive spinal interventions, such as vertebral augmentation of osteoporotic fractures. Oncology patients are frequently debilitated. Hence, the depth and duration of conscious sedation for the procedure should be minimized to avoid complications. Additionally, many of these patients have failed radiation therapy, which eventually causes the normal bone surrounding the metastasis to become sclerotic and difficult to cut with manual techniques. Creating a channel through young, non-osteoporotic bone can be equally challenging and time consuming. Lastly, patients may undergo ablation of multiple painful spinal metastases as part of a single procedure, and in these cases it is important to treat each individual vertebra as quickly as possible to minimize the overall procedure duration.
The OnControl System was initially marketed for bone marrow core biopsy and aspiration. Prospective randomized studies found that compared with manual bone marrow biopsy devices, experienced operators obtained specimens of greater volume more quickly and with less pain.5,6 Subsequent studies performed in teaching hospitals yielded similar results.7 Use of drill assistance has since expanded to include percutaneous biopsy of the axial and appendicular skeleton.8,9 Lee et al.5 compared 25 pairs of drill-assisted and manual computed tomography (CT)-guided biopsies, 13 of which were of vertebral bodies. The drill-assisted biopsies required less time (10.5 ± 3.5 versus 19.4 ± 7.5 minutes; p = 0.03) and radiation exposure to the patient (164 ± 35 versus 270 ± 48 mGy; p = 0.04). All drill-assisted biopsies obtained in this study were histologically adequate and no complications were reported.9
This case series illustrates that the drill-assisted technique can also be used to safely gain access to vertebral bodies for RFA of spinal metastases under fluoroscopic guidance. The power of the drill allows the interventionalist to quickly create a transpedicular channel through dense bone, thus reducing procedure time. Use of fluoroscopy, as opposed to CT guidance, also reduces procedure time, because the needle trajectory can be adjusted in real time. The limitation of fluoroscopy is that the needle cannot be localized within the pedicle on a single cross-sectional image. However, neural injury is avoided by ensuring that the needle does not violate the medial cortex of the pedicle on the AP view, or the superior or inferior cortex of the pedicle on the lateral view. In our experience, drill assistance allows the interventionalist to use fine motor movements to better control the needle trajectory, as opposed to using gross movements to manually push the needle forward.
Conclusion
A drill-assisted, coaxial needle set can be used to safely and efficiently access vertebral bodies for percutaneous RFA.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: JWJ is a speaker panelist and consultant for DFINE Inc. The other authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Anchala PR, Irving WD, Hillen TJ, et al. Treatment of metastatic spinal lesions with a navigational bipolar radiofrequency ablation device: A multicenter retrospective study. Pain Physician 2014; 17: 317–327. [PubMed] [Google Scholar]
- 2.Wallace AN, Greenwood TJ, Jennings JW. Radiofrequency ablation and vertebral augmentation for palliation of painful spinal metastases. J Neurooncol. Epub ahead of print 29 May 2015. [DOI] [PubMed] [Google Scholar]
- 3.Wallace AN, Greenwood TJ, Jennings JW. Use of imaging in the management of metastatic spine disease with percutaneous ablation and vertebral augmentation. AJR Am J Roentgenol. In press. [DOI] [PubMed] [Google Scholar]
- 4.Hillen TJ, Anchala P, Friedman MV, et al. Treatment of metastatic posterior vertebral body osseous tumors by using a targeted bipolar radiofrequency ablation device: Technical note. Radiology 2014; 273: 261–267. [DOI] [PubMed] [Google Scholar]
- 5.Lee RK, Ng AW, Griffith JF. CT-guided bone biopsy with a battery-powered drill system: Preliminary results. AJR Am J Roentgenol 2013; 201: 1093–1095. [DOI] [PubMed] [Google Scholar]
- 6.Reed LJ, Raghupathy R, Strakhan M, et al. The OnControl bone marrow biopsy technique is superior to the standard manual technique for hematologists-in-training: A prospective, randomized comparison. Hematol Rep 2011; 3: e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schnapauff D, Streitparth F, Jöhrens K, et al. CT-guided radiofrequency ablation of osteoid osteoma using a novel battery-powered drill. Skeletal Radiol 2014; 44: 695–701. [DOI] [PubMed] [Google Scholar]
- 8.Swords RT, Anguita J, Higgins RA, et al. A prospective randomised study of a rotary powered device (OnControl) for bone marrow aspiration and biopsy. J Clin Pathol 2011; 64: 809–813. [DOI] [PubMed] [Google Scholar]
- 9.Swords RT, Kelly KR, Cohen SC, et al. Rotary powered device for bone marrow aspiration and biopsy yields excellent specimens quickly and efficiently. J Clin Pathol 2010; 63: 562–565. [DOI] [PubMed] [Google Scholar]