Abstract
We report a 67-year-old man who harboured an unruptured left basilar-superior cerebellar artery aneurysm. Cerebral angiography and cone beam computed tomography with diluted contrast medium showed that the bilateral ophthalmic arteries were not supplied from internal carotid arteries but, rather, were supplied from the middle meningeal and accessory meningeal arteries. This meant that the ophthalmic system was predominantly supplied from the dural arteries and, therefore, pterional craniotomy might cause a compromise in blood supply to the retinal artery. To avoid this complication, coil embolization was selected instead of neck clipping, and this endovascular therapy succeeded without neurological deficit. This case report shows the importance of cerebral angiography (including cone beam computed tomography) and consideration of the patterns of ophthalmic artery perfusion when selecting operative procedures for management of aneurysms that require manipulation around the sphenoid ridge.
Keywords: Ophthalmic artery, middle meningeal artery, cone beam computed tomography, endovascular treatment, recurrent meningeal artery
Background
The ophthalmic artery usually originates from the internal carotid artery, which runs through the optic canal to the orbit and retina. Although anastomosis between the ophthalmic artery and the external carotid arterial system, such as the middle meningeal artery, is often observed, it is rare to find the ophthalmic artery completely supplied from the dural artery. In such cases, craniotomy can injure the dural arterial network between the ophthalmic artery and the external carotid meningeal artery. This injury of dural arterial network may lead to vision loss.1 It is important to be aware of this anatomical background to avoid such visual complications, and endovascular treatment is an effective alternative modality in this context.
Case presentation
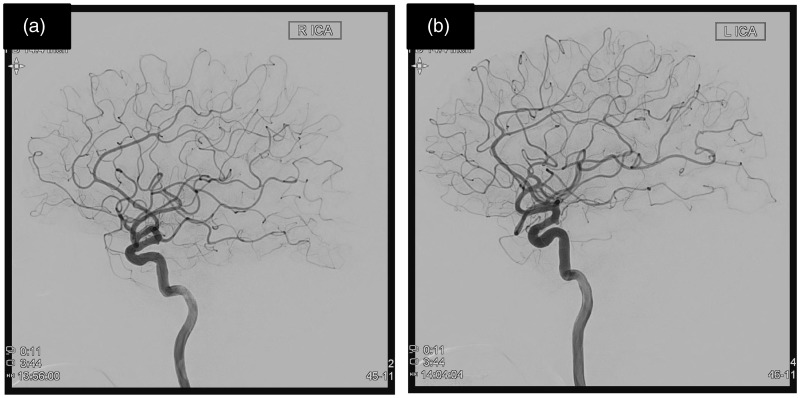
An asymptomatic 67-year-old man was incidentally diagnosed with a left basilar artery-superior cerebellar artery aneurysm that was 5.3 mm in diameter. Preoperative cerebral angiography (undertaken using a flat-detector biplane angiography unit: Allura Clarity; Philips Medical Systems) showed that the bilateral ophthalmic arteries were supplied from the external carotid artery rather than from the internal carotid artery (Figure 1).
Figure 1.
(a) Right internal carotid artery (lateral view). (b) Left internal carotid artery (lateral view).
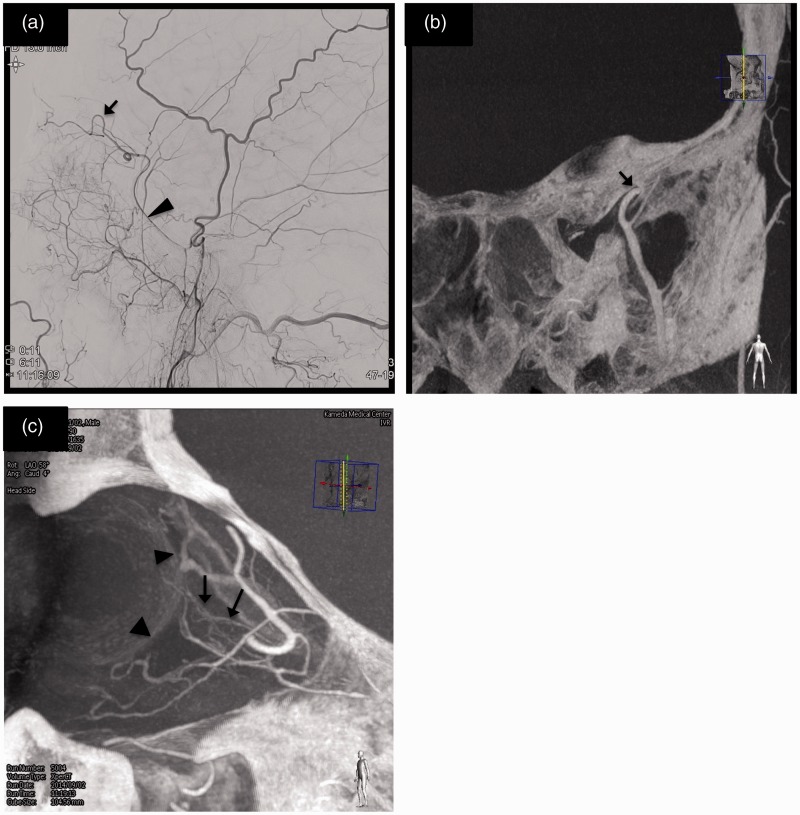
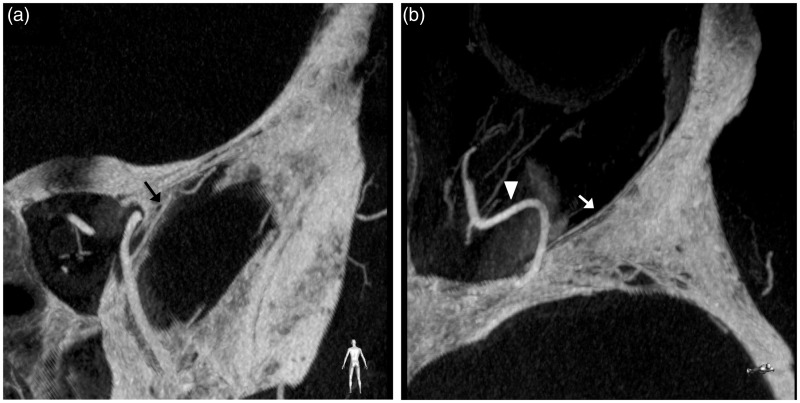
On the right side, high-resolution cone beam computed tomography (CBCT) with iodinated contrast medium diluted to a concentration of around 33% showed that the recurrent meningeal artery from the frontal branch of the middle meningeal artery contributed to the ophthalmic artery through the superior orbital fissure (Figure 2). The CBCT also showed that the right lacrimal artery arose from the recurrent meningeal artery inside of the orbit. There was no evidence of the meningo-lacrimal artery through the lacrimal foramen (Figure 3).
Figure 2.
(a) External carotid artery injection (lateral view) shows frontal branch of middle meningeal artery (arrowhead) continues to only ophthalmic systems (arrow). (b) Cone beam CT (P-A view) shows the frontal branch of middle meningeal artery passes through the superior orbital fissure (arrow). (c) Cone beam CT of right external carotid artery injection (view from the bottom left) shows the distribution of central retinal artery (arrows). Choroidal blush (arrowheads) is also seen.
Figure 3.
(a) Cone beam CT (P-A view) shows no vessels pass through lacrimal foramen (arrow). (b) The lacrimal artery (arrow) arises from the recurrent meningeal artery (arrowhead) inside of the orbit.
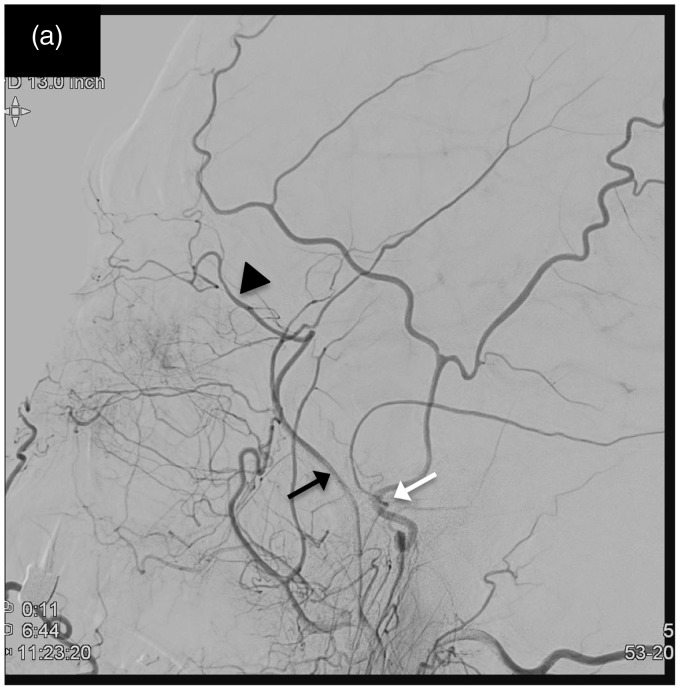
On the left side, the accessory meningeal artery contributed to the region of the frontal branch of the middle meningeal artery and the ophthalmic artery via the recurrent meningeal artery (Figure 4). Based on this anatomical variation, ipsilateral retinal ischemia leading to vision loss was anticipated if the accessory meningeal artery was injured due to surgical manipulation around the sphenoid ridge and paraclinoid dural membrane. Therefore, endovascular treatment was performed, and the aneurysm was successfully embolized without neurological sequelae. The visual acuity of the patient was intact, and he was discharged home 3 days after embolization. Magnetic resonance imaging 6 months after the procedure showed complete obliteration of aneurysm and preservation of the superior cerebellar artery.
Figure 4.
Left external carotid artery injection (lateral view) shows the accessory meningeal artery (black arrow) contributing to the region of frontal branch of middle meningeal artery and the ophthalmic systems (arrowhead) via recurrent meningeal artery. Foramen spinosum (white arrow) is behind the accessory meningeal artery.
Discussion
Usually, the ophthalmic artery arises from the supraclinoid portion of the internal carotid artery and passes through the optic canal and contributes to the central retinal artery.
In the human embryo, the primitive ophthalmic artery passing through the optic canal and the orbital artery arising from the supraorbital branch of the stapedial artery run in the orbit.2 The orbital artery passes through the superior orbital fissure and divides into the anterior ethmoidal artery and the meningo-lacrimal branch.2 The anterior ethmoidal artery anastomoses with the primitive ophthalmic artery around the optic nerve and forms the arterial ring.2 At the stage of 24–40 mm, the trans-sphenoidal part of the orbital artery regresses and the primitive ophthalmic artery takes over the orbital branch of the stapedial artery.2 Thus, the ophthalmic artery is completed.2 If the proximal part of the primitive ophthalmic artery regresses instead of the orbital branch of the stapedial artery, the ophthalmic artery arises from the middle meningeal artery.2 Hayreh and Dass reported various origins of the ophthalmic artery, such as the middle meningeal artery, facial artery, infraorbital artery, anterior deep temporal artery, etc.3 They found two cases out of 170 specimens originated completely from the middle meningeal artery.3 The right ophthalmic artery in our case exhibited the same pattern as seen in those two cases.
Lasjaunias et al. described the network between the accessory meningeal artery and the ophthalmic artery, which ran through the superior orbital fissure.2 They reported that the disappearance of the ventral ophthalmic artery instead of the dorsal ophthalmic artery with the accessory meningeal artery dominance caused such a variant.2 This anatomical feature corresponds with the left ophthalmic artery of the present case.
Erturk et al. reported that the orbital branch of the middle meningeal artery was found in 48 of 74 specimens from 37 cadavers: 32 (43.2%) passed through the lacrimal foramen, 12 (16.2%) passed through the superior orbital fissure and four (5.4%) passed through both lacrimal foramen and superior orbital fissure.4 The lacrimal foramen is located 4–12 mm lateral to the superior orbital fissure.5,6 Therefore, the meningo-lacrimal artery passing through the lacrimal foramen is at greater risk of being injured during pterional craniotomy for clipping surgery than the recurrent meningeal artery passing through the superior orbital fissure.
Obliteration of these dural arteries during the surgeries of patients like the present case may cause perfusion failure of the ophthalmic artery system. Shima et al. described three cases whose ophthalmic arteries arose completely from the middle meningeal artery. In one case, the ophthalmic artery was occluded after removing the sphenoid ridge during pterional craniotomy, resulting in vision loss.1 In other cases, the middle meningeal arteries were carefully preserved during removal of the sphenoid ridge.1
In the present case, high-resolution CBCT showed very fine images around the right orbit. It showed that there was neither ophthalmic artery from the internal carotid artery nor meningo-lacrimal artery through the lacrimal foramen. Furthermore, the central retinal artery arising completely from the recurrent meningeal artery was clearly revealed. These findings were not only of great interest, but also very helpful for planning treatment strategy. Coil embolization is applied widely to the treatment of cerebral aneurysm, especially in the case of the posterior circulation aneurysms like the present case. In treating anterior circulation aneurysms, surgical neck clipping is also taken into account, but neglecting the perfusion pattern of ophthalmic artery may result in vision loss. Based on this functional anatomy of ophthalmic artery associated with anastomosis, endovascular treatment is the optimal management in terms of preservation of visual acuity. Selection of the operative procedure based on accurate interpretation of cerebral angiography (including CBCT) is essential.
Conclusion
Although uncommon, some patients have ophthalmic arteries that arise completely from the dural arteries. In these cases, injury of the dural arteries that contribute to the ophthalmic arteries during removal of the sphenoid ridge may cause retinal ischemia, resulting in vision loss. Endovascular treatment is an effective procedure to avoid vision loss. We should consider the perfusion pattern of ophthalmic arteries when selecting the operative procedure in cases which require manipulation around the sphenoid ridge in the open surgery. Cerebral angiography should be considered when we cannot identify the ophthalmic arteries on computed tomographic angiography or magnetic resonance angiography, and CBCT contributes a great deal to anatomical understanding and planning of the treatment strategy.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Shima K, Kawasaki T, Shimizu A, et al. An ophthalmic artery occlusion after a craniotomy using the pterional approach: A report of three cases, one resulting in blindness. Jpn J Neurosurg 1995; 4: 163–169. [Google Scholar]
- 2.Lasjannias P, Ter Brugge KG, Berenstein A. Surgical Neuroangiography Vol 1, 2nd ed Berlin, Heidelberg, New York, Tokyo: Springer Verlag, 1986, pp. 426–427, 450–451. [Google Scholar]
- 3.Hayreh SS, Dass R. The ophthalmic artery. Br J Ophthalmol 1962; 46: 65–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erturk M, Kayalioglu G, Govsa F, et al. The cranio-orbital foramen, the groove on the lateral wall of the human orbit, and the orbital branch of the middle meningeal artery. Clin Anat 2005; 18: 10–14. [DOI] [PubMed] [Google Scholar]
- 5.Liu Q, Rhoton AL., Jr Middle meningeal origin of the ophthalmic artery. Neurosurgery 2001; 49: 401–407. [DOI] [PubMed] [Google Scholar]
- 6.Perrini P, Cardia A, Fraser K, et al. A microsurgical study of the anatomy and course of the ophthalmic artery and its possibly dangerous anastomosis. J Neurosurgery 2007; 106: 142–150. [DOI] [PubMed] [Google Scholar]