Abstract
Purpose
The efficacy and safety of aspiration thrombectomy using Penumbra in acute occlusion of intracranial artery have been proved in many previous studies. Our study aimed to retrospectively assess the efficacy and safety of a manual aspiration thrombectomy using Penumbra in patients with M1 occlusion.
Materials and methods
We conducted a retrospective review of 70 patients who underwent manual aspiration thrombectomy using Penumbra catheters for treatment of M1 occlusion between January 2012 and December 2014. We evaluated immediate angiographic results and clinical outcomes through review of patient electronic medical records.
Results
Male was the dominant sex in this study (M:F = 38:32) and median age was 72 (age range, 36–91). The rate of successful recanalization (TICI grade ≥2 b) was 91.4% (64/70). The successful recanalization rate by single Penumbra was 82.9% (58/70). Six patients were treated in combination with Solitaire stent. Median NIHSS score was 11 (range, 4–20) at admission and was 3 (range 0–23) at discharge. Favorable clinical outcomes (mRS score at three months ≤2) were seen in 42 patients (60%). Two patients were observed to have subarachnoid hemorrhage after the procedure. Another two patients died related to massive symptomatic hemorrhage, brain edema and herniation in the hospital.
Conclusion
Manual aspiration thrombectomy appears to be safe and is capable of achieving a high rate of successful recanalization and favorable clinical outcomes in patients with M1 occlusion.
Keywords: Middle cerebral artery, stroke, thrombectomy
Introduction
Early recanalization following large-vessel occlusion has been associated with improved clinical outcome in acute ischemic stroke.1–3 A recent randomized trial found that stent-based thrombectomy (SBT) with a stent retriever after intravenous recombinant tissue plasminogen activator (rtPA) improved functional outcomes at 90 days.4 Manual aspiration thrombectomy (MAT) using a flexible aspiration catheter is an alternative method of opening blocked vessels.5–7 With the introduction of easily trackable and very large aspiration catheters, recanalization rate and functional outcomes of MAT are comparable to those of SBT.8
For now, SBT and MAT are the main treatment options for endovascular therapy (EVT) in selected patients with acute ischemic stroke. Combined use of SBT and MAT as a first-line and rescue treatment has also been shown to be effective for vessel recanalization.8–10 In our hospital, the combination of MAT with a Penumbra reperfusion catheter (Penumbra, Alameda, CA, USA) as a first-line therapy and SBT with a Solitaire stent (Covidien/ev3, Irvine, CA, USA) as a rescue therapy has been used in selected patients with acute ischemic stroke since 2012.
The largest series to date describing MAT in M1 occlusions includes recent studies by Kang et al.,9 Jankowitz et al.7 and Turk et al.,8 who reported on 51, 79 and 61 cases, respectively. However, none of these studies described occlusion site-specific safety and clinical outcomes. The purpose of this study was to describe the safety and efficacy of combined use of MAT as a first-line and SBT as a rescue therapy in patients with acute M1 middle cerebral artery (MCA) occlusion in a single-center consecutive series.
Methods
Patient selection
This retrospective study was approved by our institutional review board. From January 2012 to December 2014, 70 patients with acute ischemic stroke within six hours of symptom onset caused by M1 occlusion were treated with MAT using a Penumbra catheter as a first-line EVT. All patients were initially evaluated with computed tomography (CT) or magnetic resonance (MR) imaging and their angiographic status was assessed routinely by MR angiography or three-dimensional CT angiography. Inclusion criteria for EVT were initial National Institute of Health Stroke Scale (NIHSS) ≥4, no evidence of intracerebral hemorrhage detected on the cranial CT or MRI, obvious major vessel occlusion of anterior circulation on CT or MR angiography, infarct core volume less than one-third of the MCA territory on the diffusion-weighted imaging (DWI) or non-enhanced CT, and/or perfusion deficit more than two-thirds of the MCA territory or perfusion deficit volume on MR showing more than 30% larger than lesion volume on DWI. At admission, the NIHSS score was assessed by a stroke neurologist. Eligible patients who met standard National Institute of Neurologic Disorders and Stroke (NINDS) criteria were treated with 0.9 mg/kg of intravenous rtPA. Subsequent EVT was considered within 1 h of intravenous rtPA for patients with no neurological improvement, which was defined as an unchanged NIHSS score from baseline or a worsening neurological deficit.
Endovascular treatment
Endovascular treatment was performed by one interventional neuroradiologist with 10 years of experience. Written informed consent for the cerebral angiography and EVT was obtained from all patients. All procedures were performed under local anesthesia via the percutaneous transfemoral route. A triple coaxial system assembled by combining an outermost 80-cm long 8 F sheath (Shuttle-SL; Cook, Bloomington, IN, USA), a middle 100-cm long 8 F guide catheter (Guider Softip; Stryker, Natick, MA, USA) and an inner 125-cm long selection catheter (Headhunter; Cook, Bloomington, IN, USA), was placed in the common carotid artery and internal carotid artery (ICA) for aspiration thrombectomy. The guiding catheter was placed in the distal ICA without vessel spasm. After complete occlusion of M1 was demonstrated by cerebral angiography, a double coaxial system assembled by combining an outer Penumbra catheter and an inner Rebar 18 microcatheter (Covidien/ev3, Irvine, CA, USA) was advanced to the level of the thrombus using a 0.014-inch micro-guidewire (Synchro; Stryker Neurovascular, Freemont, CA, USA). At the level of the thrombus, the micro-guidewire and microcatheter were advanced more distally through the thrombus up to distal M2 of the MCA in order to get sufficient support to track the Penumbra reperfusion catheter. Thereafter, we gently advanced the Penumbra catheter into the thrombus until wedged tightly. Subsequently, the microcatheter and micro-guidewire were removed and a 20 ml syringe was connected to the proximal hub of the Penumbra catheter. Continuous manual aspiration was performed with maintaining the vacuum state between the tip of Penumbra catheter and the thrombus while gently withdrawing the Penumbra catheter through the guide catheter. If angiographic recanalization was not noted after five trials, additional SBT was performed with a Solitaire stent. The details of the technique for SBT with a Solitaire stent have been described previously.11
Outcome measures
For all patients, we reviewed the medical records to collect demographic, clinical and angiographic data, retrospectively. The degree of vessel occlusion after treatment was defined by the Thrombolysis in Cerebral Infarction (TICI) scale and successful recanalization after treatment was defined as TICI scale ≥2 b. The NIHSS score was measured on admission and at discharge, and modified Rankin scale (mRS) was checked on admission and at three months for all patients, and favorable outcome was defined as an mRS of ≤2. Procedure-related symptomatic intracerebral hemorrhage (ICH) was defined as presence of hemorrhage after treatment with any point of increasing NIHSS compared to NIHSS on admission. Mortality was defined as death within 90 days from initial presentation.
Results
Patients
From January 2012 to December 2014, 114 consecutive patients with acute ischemic stroke caused by MCA occlusion were treated with MAT using a Penumbra reperfusion catheter as first-line therapy. Of these, a total of 52 were excluded for the following reasons: occlusion in the M2 superior or inferior division (N = 36); disability (mRS ≥ 3) by previous infarction at admission (N = 4); technical failure caused by tortuous course of aorta and/or common carotid artery (N = 2); and loss to follow-up and did not receive a clinical evaluation at three months (N = 2). Thus, 70 patients who underwent MAT using Penumbra as a first-line therapy were included in this study. Of these, MAT was performed with the 041 (n = 21) or 4-MAX (n = 41) models in patients with middle or distal M1 occlusion and with the 5-MAX model in eight cases with proximal M1 occlusion.
Baseline clinical characteristics and preprocedural findings are summarized in Table 1. Patients were more often male (54.3%) and the median age was 72 years (age range, 36–91 years). Twelve (17.1%) had a medical history of previous stroke. The time from symptom onset to admission ranged from 10 to 300 minutes (median, 122 minutes), and the time from admission to femoral puncture ranged from 40 to 186 minutes (median, 116 minutes). Median NIHSS score at admission was 11 (range, 4 to 20). Thirty-five patients (50%) received intravenous rtPA before angiography. Initial mRS at admission ranged from 3 to 5 (median, 4).
Table 1.
Summary of patient demographics and preprocedural findings.
| Patient demographics | No (%) or median (IQR) | Range |
|---|---|---|
| Age (years) | 72 (64–78) | 36–91 |
| Male | 38 (54.3) | |
| Previous medical history | ||
| Diabetes mellitus | 9 (12.9) | |
| Hypertension | 34 (48.6) | |
| Hypercholesterolemia | 8 (11.4) | |
| Smoking | 20 (31.4) | |
| Previous stroke | 12 (17.1) | |
| Previous cardiac disease including AF | 31 (44.3) | |
| Preprocedural findings | ||
| Onset to door time (min) | 122 (60–180) | 10–300 |
| Door to needle time (min) | 116 (90–146) | 40–186 |
| NIHSS at admission | 11 (8–15) | 4–20 |
| Modified Rankin scale | 4 (4–4) | 3–5 |
| 3 | 7 (10) | |
| 4 | 49 (70) | |
| 5 | 14 (20) | |
| Received IV rtPA | 35 (50) | |
AF: atrial fibrillation; NIHSS: National Institutes of Health Stroke Scale; IV: intravenous; rtPA: recombinant tissue plasminogen activator; IQR: interquartile range.
Periprocedural findings, complications and clinical outcomes
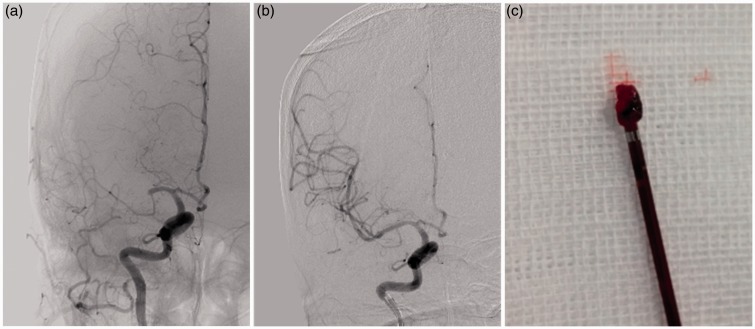
Table 2 summarizes periprocedural findings, complications and clinical outcomes. The rate of successful recanalization (TICI grade ≥2 b) was 91.4% (64/70) (Figure 1). The successful recanalization rate by single Penumbra was 82.9% (58/70). Six patients were treated in combination with a Solitaire stent. The median procedure time was 34 minutes (range, 15–129 minutes). The median time from symptom onset to recanalization was 274 minutes (130 – 560 minutes). Four patients had a tandem occlusion in the A2 anterior cerebral artery. Of these, three were treated by MAT using a Penumbra catheter and achieved recanalization of the anterior cerebral artery as TICI grade 2 b, and one was treated by mechanical thrombectomy using a microcatheter and urokinase infusion but was not recanalized. Four patients had underlying atherosclerotic stenosis of the M1; two underwent a self-expandable stent and two underwent angioplasty alone. After the procedure, 44 patients (62.8%) were classified as TICI grade 3, 20 patients (28.6%) as TICI grade 2 b, and six patients (8.6%) as TICI grade 2 a.
Table 2.
Summary of periprocedural findings, complications, and clinical outcomes after three months.
| Patient demographics | No (%) or median (IQR) | Range |
|---|---|---|
| Periprocedural findings | ||
| Tandem occlusion of ACA territory | 4 (5.7) | |
| Combined recanalization using Solitaire | 6 (8.6) | |
| Procedure duration (min) | 34 (26–50) | 15–129 |
| Onset to recanalization (min) | 272 (235–360) | 130–560 |
| TICI grade | ||
| ≤2 a | 6 (8.6) | |
| 2 b | 20 (28.6) | |
| 3 | 44 (62.8) | |
| Complications | ||
| Procedure-related SAH | 3 (4.3) | |
| ICH | 10 (14.3) | |
| Symptomatic ICH | 4 (5.7) | |
| Follow-up evaluation | ||
| NIHSS at discharge | 3 (1–6) | 0–17 |
| mRS at three months | 1 (0–3) | 0–6 |
| 0 | 18 (25.8) | |
| 1 | 19 (27.1) | |
| 2 | 5 (7.1) | |
| 3 | 13 (18.5) | |
| 4 | 11 (15.7) | |
| 5 | 2 (2.9) | |
| 6 | 2 (2.9) | |
| Favorable outcome (mRS 0–2) | 42 (60) | |
| Mortality | 2 (2.9) | |
ACA: anterior cerebral artery; TICI: Thrombolysis in Cerebral Infarction; SAH: subarachnoid hemorrhage; ICH: intracerebral hemorrhage; NIHSS: National Institutes of Health Stroke Scale; mRS: modified Rankin scale.
Figure 1.
A 73-year-old man with complete occlusion of the right M1. (a) Initial cerebral angiogram shows complete occlusion of the right M1. (b) Final cerebral angiogram after manual aspiration thrombectomy using a Penumbra catheter shows complete revascularization (TICI 3). We performed three aspiration thrombectomies. (c) Image of the clot retrieved by manual aspiration thrombectomy. TICI: Trombolysis in Cerebral Infarction.
Procedure-related subarachnoid hemorrhage was observed in two patients, and both showed complete absorption of the hemorrhage at discharge. However, two patients (2.9%) died during their hospitalization of massive symptomatic hemorrhage, brain edema and herniation. Therefore, the overall mortality rate was 2.9%.
At discharge, the median NIHSS score of the surviving patients was 3 (range, 0 – 17). All but four patients demonstrated improved NIHSS score at discharge. However, 28 patients (40%) had unfavorable functional outcomes (mRS > 2, including the two mortality cases). The remaining 42 patients had favorable clinical outcomes (mRS ≤ 2).
Discussion
To our knowledge, this report is the largest and first consecutive case series describing the safety and outcome of MAT as a first-line EVT only for acute M1 occlusion. Previous reports have also described MAT as a first-line or rescue therapy, but specific results regarding M1 occlusion were not provided until this study.5–8,10 In our study, successful recanalization (TICI grade 2 b or 3) with MAT was achieved in 58 of 70 (82.9%) patients. Adding SBT as a rescue therapy increased the overall recanalization rate to 91.4% (64/70), and 60% (42/70) of patients had a favorable clinical outcome (mRS 0–2). On average, recanalization was achieved within 34 min of groin puncture.
Just two years ago, three initial randomized trials of endovascular therapy (Interventional Management of Stroke III (IMS-3),11 Local Versus Systemic Thrombolysis for Acute Ischemic Stroke (SYNTHESIS)12 and Mechanical Retrieval and Recanalization of Stroke Clots Using Embolectomy (MR RESCUE)13) all failed to show the benefit of various intra-arterial approaches over standard care alone. However, more recent trial results have been positive, with improved outcomes of EVT using stent retrievers.4,14–16 Compared with the most recent outcomes of stent-retriever thrombectomy, the MAT technique we used displayed promising results in recanalization rate, favorable functional outcome and safety (Table 3).4–8,10 In the most recently reported Solitaire with the Intention for Thrombectomy as Primary Endovascular Treatment (SWIFT PRIME) trial,4 TICI 2 b–3 recanalization was achieved with SBT in 88% of cases and 60% had a good functional outcome (mRS 0–2). In the initial stage of introduction of the MAT technique, successful recanalization rate and functional outcome were inferior to the SBT technique.7,9 Kang et al.9 reported a series of 74 patients with acute ischemic stroke who were treated with a combination of MAT and SBT. They reported a primary successful recanalization (TICI 2 b or 3) rate of 53% (39/74) with MAT, which is inferior to that of SBT in the SWIFT PRIME trial. Jankowitz et al.7 described similar results in a retrospective examination of 112 stroke cases with MAT as the first-line therapy and an adjunctive device such as the Merci retriever, Solitaire or Trevo as rescue therapy. Successful recanalization (TICI 2 b or 3) with first-line MAT was achieved in 59% of cases.7
Table 3.
Comparison of the present study with reported endovascular therapy results.
| Saver et al.4 (2015) | Kang et al.9 (2013) | Jankowitz et al.7 (2015) | Turk et al.8 (2014) | Present study | |
|---|---|---|---|---|---|
| Case number | 98 | 74 | 112 | 98 | 70 |
| Endovascular therapy (First-line/rescue) | SBT/– | MAT/SBT | MAT/various methods | MAT/SBT | MAT/SBT |
| First-line TICI 2 b/3 (%) | 88 | 53 | 59 | 78 | 82.9 |
| Final TICI 2 b/3 (%) | 88 | 85.1 | 86.6 | 95 | 91.4 |
| mRS 0–2 (%) | 60 | 67.6 | 46 | 40 | 60 |
| Mortality (%) | 9 | NR | 31 | 19 | 2.9 |
| Occlusion site | ICA, MCA | ICA, MCA, BA | ICA, MCA, VBA | ICA, MCA, BA | Only M1 MCA |
| Time from groin puncture to recanalization (min) | 24 | 68 | 70 | 37 | 34 |
| Time from onset to groin puncture (min) | 224 | NR | 267 | 510 | 238 |
| Time from onset to recanalization (min) | 252 | 338.5 | NR | NR | 272 |
ICA: internal carotid artery; MCA: middle cerebral artery; BA: basilar artery; VBA: vertebrobasilar artery; NR: not reported; mRS: modified Rankin scale; TICI: Thrombolysis in Cerebral Infarction; MAT: manual aspiration thrombectomy; SBT: stent-based thrombectomy.
More recently, introduction of the newest generation of large-bore aspiration catheters has yielded improved recanalization rates in MAT. In a study by Turk et al.,8 MAT with a large-bore aspiration catheter was a first-line EVT that was successful in achieving TICI 2 b or 3 recanalization in 78% of cases. The additional use of SBT improved the TICI 2 b/3 recanalization rate to 95%. In their study, the average time from groin puncture to at least TICI 2 b recanalization was 37 min, which was faster than those in the studies of previous generations of catheter, specifically 68 min and 70 min by Kang et al.9 and Jankowitz et al.,7 respectively. In our study, the advanced results of the newest generation of large-bore aspiration catheter were confirmed and extended to acute M1 occlusion. The MAT-only successful recanalization (TICI 2 b–3) rate was high in our study (82.9%) and greater than that observed by Turk et al.8 (78%). The frequency of good outcome (mRS 0–2) was 60% in our study, which was greater than that of Turk et al.8 (40%) and the same as that observed in the SWIFT PRIME trial4 (60%).
Possible explanations for the favorable outcomes of this study include the use of an optimized multiple coaxial catheter system and the shortened time from onset to recanalization. In endovascular therapy of acute ischemic stroke, vascular tortuosity is a major cause of difficulty or failure in treating intracranial lesions. Thus, a catheter system for accessing the target lesion and providing stable support are essential for successful mechanical thrombectomy. Triple or quadruple coaxial catheter systems were already demonstrated to be safe and efficient for mechanical thrombectomy in acute ischemic stroke.17 Therefore, proper selection of the appropriate catheter and wire for MAT is at the operator’s discretion. In our study, the combination of an 80-cm long 8 F (0.113-inch inner diameter) sheath and 100-cm long 8 F guide catheter (0.106-inch outer diameter and 0.086-inch inner diameter) provided proper proximal mechanical support from the groin to the level of the common carotid or ICA. In addition to the mechanical support of this system, the 8 F guide catheter provided easy access to the proximal part of various Penumbra catheters, which is larger than the distal part. Moreover, the 8 F guide catheter also allowed access for stent retrieval when the MAT technique failed. The combination of a Rebar 18 microcatheter and Synchro 0.014-inch wire was effective for advancing more distally through the thrombus up to distal M2 of the MCA. Only two of our patients were excluded for a tortuous course of aorta and/or common carotid artery. In our study, time from stroke onset to recanalization was 274 min, which is considerably faster than that observed in previous MAT studies,7–9 and similar to that observed in the SWIFT PRIME trial (252 min).4 Therefore, the substantially improved outcome of this study may be explained in part by rapid recanalization.
Our study had several limitations. First, this study was based on a single-center experience, and therefore lacks strong power to confirm the efficacy and safety of MAT. Second, we did not compare MAT with other EVTs or medical therapy.
Conclusion
In selected patients with acute ischemic stroke due to M1 MCA occlusion, MAT was effective as a first-line EVT in achieving recanalization and favorable outcome without serious complications. Further well-designed, prospective randomized trials should provide reasonable evidence of benefit with this approach compared with other EVTs or medical therapy.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: A meta-analysis. Stroke 2007; 38: 967–973. [DOI] [PubMed] [Google Scholar]
- 2.Nogueira RG, Lutsep HL, Gupta R, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): A randomised trial. Lancet 2012; 380: 1231–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): A randomised, parallel-group, non-inferiority trial. Lancet 2012; 380: 1241–1249. [DOI] [PubMed] [Google Scholar]
- 4.Saver JL, Goyal M, Bonafé A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 5.Kang DH, Hwang YH, Kim YS, et al. Direct thrombus retrieval using the reperfusion catheter of the Penumbra system: Forced-suction thrombectomy in acute ischemic stroke. AJNR Am J Neuroradiol 2011; 32: 283–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jankowitz B, Aghaebrahim A, Zirra A, et al. Manual aspiration thrombectomy: Adjunctive endovascular recanalization technique in acute stroke interventions. Stroke 2012; 43: 1408–1411. [DOI] [PubMed] [Google Scholar]
- 7.Jankowitz B, Grandhi R, Horev A, et al. Primary manual aspiration thrombectomy (MAT) for acute ischemic stroke: Safety, feasibility and outcomes in 112 consecutive patients. J Neurointerv Surg 2015; 7: 27–31. [DOI] [PubMed] [Google Scholar]
- 8.Turk AS, Frei D, Fiorella D, et al. ADAPT FAST study: A direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg 2014; 6: 260–264. [DOI] [PubMed] [Google Scholar]
- 9.Kang DH, Kim YW, Hwang YH, et al. Switching strategy for mechanical thrombectomy of acute large vessel occlusion in the anterior circulation. Stroke 2013; 44: 3577–3579. [DOI] [PubMed] [Google Scholar]
- 10.Kim SK, Yoon W, Moon SM, et al. Outcomes of manual aspiration thrombectomy for acute ischemic stroke refractory to stent-based thrombectomy. J Neurointerv Surg 2014; 7: 473–477. [DOI] [PubMed] [Google Scholar]
- 11.Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013; 368: 893–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ciccone A, Valvassori L, Nichelatti M, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med 2013; 368: 904–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 2013; 368: 914–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berkhemer OA, Fransen PSS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 15.Campbell BCV, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 16.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. [DOI] [PubMed] [Google Scholar]
- 17.Kulcsár Z, Yilmaz H, Bonvin C, et al. Multiple coaxial catheter system for reliable access in interventional stroke therapy. Cardiovasc Intervent Radiol 2010; 33: 1205–1209. [DOI] [PubMed] [Google Scholar]