Abstract
Background
Endovascular treatment is an alternative choice for the treatment of distal middle cerebral artery (dMCA) aneurysm, in addition to open surgery; but is still seldom considered. We performed this retrospective study to evaluate the outcome of dMCA in patients.
Methods
During a period of 10 years, we were able to identify seven patients with a total of eight dMCA aneurysms that were treated endovascularly. They were five men and two women, with a mean age of 36.1 years. All of the aneurysms, including five infectious and three dissecting ones, were treated for the aneurysm and its parent artery’s occlusion, using coils and/or glue.
Results
The clinical follow-up (9–96 m, mean 36.8 m) showed that they all improved over baseline; except for one patient in whom a mild right hemiparesis remained, after the hematoma evacuation. Angiographic follow-up (7–24 m; mean: 14.6 m) showed that all of them were stable and without the need for recanalization.
Conclusions
Our data indicated that endovascular treatment is a safe and effective alternative for the treatment of dMCA aneurysms, and should be considered when treating these aneurysms.
Keywords: Aneurysm, case studies, catheter-based methods, coiling, distal middle cerebral artery, Glubran, glue, embolism, endovascular clot, hematoma, infectious aneurysm, intracranial aneurysm, middle cerebral artery, outcome
Introduction
Middle cerebral artery (MCA) aneurysms account for about 20% of intracranial aneurysms; however, most of them are located at the M1 segment or bifurcation of the middle cerebral arteries. Aneurysms distal to the MCA bifurcation are rare, only comprising about 1.1–7% of all MCA aneurysms.1,2 Open surgery is a classical treatment for these aneurysms, and offers variable treatment modalities, which include aneurysm clipping, aneurysm trapping, aneurysm trapping plus bypass, and so on; however, in some circumstances (such as infectious aneurysms, multiple aneurysms, intra-parenchymal aneurysms difficult to be localized, etc.), surgery may not be an optimal choice.
Endovascular treatment (EVT) is an alternative choice for the treatment of distal middle cerebral artery (dMCA) aneurysms; however, EVT of these aneurysms presents a number of challenges, because of the distant, small and tortuous route. In addition, for those peripheral MCA aneurysms, the parent arteries are usually difficult to preserve via an endovascular approach, which imposes potential ischemic risks. The treatment complications and outcomes are not clear yet, due to limited reports.
In this article, we retrospectively reviewed seven patients with eight dMCA aneurysms that occurred during a period of 10 years; plus we performed a systematic review of the literature, in order to clarify the safety and efficacy of EVT for dMCA aneurysms.
Materials and methods
Patients
In this article, dMCA aneurysm refers to aneurysms that are located distal to the MCA bifurcation, at the M2 to M4 segment, or peripheral branches of MCA according to the Gibo et al.3 classification. In this series, those aneurysms associated with anterovenous malformations or Moyamoya disease were excluded. As a result, there were nine patients with 10 dMCA aneurysms whom were identified during a period ranging from January 2003 to January 2013. This constituted about 4.1% (10/242) of all MCA aneurysms, as well as about 0.36% (10/2807) of all intracranial aneurysms which occurred at the same time. Finally, seven patients with eight dMCA aneurysms that were treated via the endovascular approach were included in this series. After approval by the Institutional Review Board (IRB) of our institution; their medical records and radiological images, such as brain computed tomography (CT) and cerebral angiographies, were retrospectively reviewed.
As is shown in Table 1, we found five men and two women, with a mean of 36.1 years of age. The presentations were: subarachnoid hemorrhage (SAH) associated with intracranial hematoma (ICH) in one patient, ICH alone in four patients and headache in one patient; while the remaining one was found incidentally, due to bleeding caused by other reasons. Emergent hematoma evacuation and decompression had been performed for two patients with massive hematoma in outside institutions, but there were no obvious aneurysms documented during the operations. These two patients came to our hospital 1 month and 1 year after their operations, respectively, while the other patients with ruptured aneurysms were all admitted and treated within 3 days after bleeding. The Hunt and Hess (HH) grade scale4 for them, when admitted, was Grade I in two patients, and Grade II and Grade III in one patient each.
Table 1.
Clinical, angiographic, treatment and follow-up data of our seven case patients with eight distal middle cerebral artery aneurysms.
| Patient | Age/ gender | Presentation | Location of aneurysm | Etiology | Size of aneurysm (mm) | Treatment | Immediate result | Clinical status at discharge | Angiographic follow-up | Clinical status at follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 26/M | SAH and ICH | L M4 | Dissection | 4.8 | Glue | Complete | Good | 24 m, 1 | 96 m, good |
| 2 | 62/F | Incident | R M2-M3 | Dissection | 12.0 | Coil | Complete | Good | 34 m, 1 | 40 m, good |
| 3 | 15/M | ICH | R M3 | Dissection | 1.5 | Coil | Complete | Good | 17 m, 1 | 19 m, good |
| 4 | 29/F | ICH | R M3 | Infectious | 3.6 | Coil + glue | Complete | Good | NA | 40 m, good |
| 5 | 45/M | Headache | L M3 | Infectious | 5.0 | Coil | Complete | Good | 24 m, 1 | 33 m, good |
| R M4 | Infectious | 7.8 | Coil | Complete | Good | 24 m, 1 | 33 m, good | |||
| 6 | 28/M | ICH | L M4 | Infectious | 4.0 | Coil + glue | Complete | Hemiparesis | 6 m, 1 | 9 m, hemiparesis |
| 7 | 48/M | ICH | R M4 | Infectious | 1.0 | Glue | Complete | Good | 7 m, 1 | 24 m, good |
ICH: intracranial hemorrhage; L: left; m: months; Pat: patient; R: right; SAH: subarachnoid hemorrhage.
Aneurysm morphology and etiology
After admission, digital subtraction angiography (DSA) was performed for each of these patients. One patient harbored a concurrent ruptured anterior communicating artery aneurysm, and one patient harbored bilateral dMCA aneurysms; so a total of nine intracranial aneurysms, of which eight were dMCA aneurysms, were found in the seven patients. Of the eight dMCA aneurysms, one was at the M2-M3 junction, three were at M3 (opercula segment) and four were at M4 (cortical segment). Five were on the right side, while three were on the left side. According to their morphologies, three were fusiform and five were saccular, of which four had an irregular shape.
The aneurysm size varied from 1–12 mm, with a median size of 5.0 mm. They were further classified as tiny (<3 mm) in two cases, small (3–10 mm) in five cases, and large (≥10 mm) in one case. Of those aneurysms, four patients had a medical history of infective endocarditis and two patients had undergone mitral valve replacement before admission. Their five aneurysms were considered as infectious ones, according to the medical history and radiographic findings. The other three aneurysms were considered as a dissection.
Treatment strategy and technique
After the aneurysms were determined by DSA, clinical management decisions were made according to their etiology. Patients with infectious aneurysms were initially treated medically for 5–7 days, with appropriate antibiotics and a serial angiography. If the serial angiography revealed no improvement of the aneurysms, the patients would be treated endovascularly. For the patient with the ruptured dissecting aneurysms, endovascular treatment was performed immediately after the DSA, to reduce the risk of re-bleeding.
All procedures were performed under general anesthesia and via the transfemoral approach. A guiding catheter (6F Envoy, Cordis, Miami Lakes, FL, USA; or Chaperon, MicroVention, Columbia, CA, USA) was placed in the distal internal carotid artery. A 3-dimensional (3-D) DSA was performed, to find the best working angle for the microcatheter navigation. The microcatheter (Marathon, Covidien, USA; or Echelon-10, Covidien, USA) was then navigated under continuous road-map guidance and the selected position was reached, close to the aneurysm.
Embolization was then carried out, using detachable coils or/and glues. The glue we preferred was Glubran (GEM Srl, Viareggio, Italy), mixed with iodized oil (Lipiodol Ultra Fluide, Laboratoire Guerbet, Paris, France) in a concentration of about 33%. The coils we often used were Hypersoft coils (Hypersoft, MicroVention, Columbia, CA, USA), especially for the more distal aneurysms. Antiplatelet and anticoagulation treatment was not administered regularly, due to the potential risk of aneurysm re-bleeding.
Results
Treatment results and immediate outcome
A total of all eight aneurysms, including the five infectious ones, were treated by aneurysm and parent artery occlusion (PAO). For the six of them in which the microcatheters were able to be delivered into the aneurismal sac, hypersoft coils were first introduced to occlude the aneurysm, as well as the parent artery (Figure 1). A 33% solution of diluted Glubran was added to two of the aneurysms that were not completely occluded after coiling (Figure 2). For the two aneurysms that were not able to be super-selected, or were too tiny to perform an intra-sac embolization, diluted Glubran was directly injected into the parent artery, aiming at occluding the proximal segment of the artery and the target aneurysm (Figure 3). When discharged, one patient was hemiplegic, due to initial brain injury, one was left with mild right hemiparesis after the hematoma evacuation, and the others recovered well.
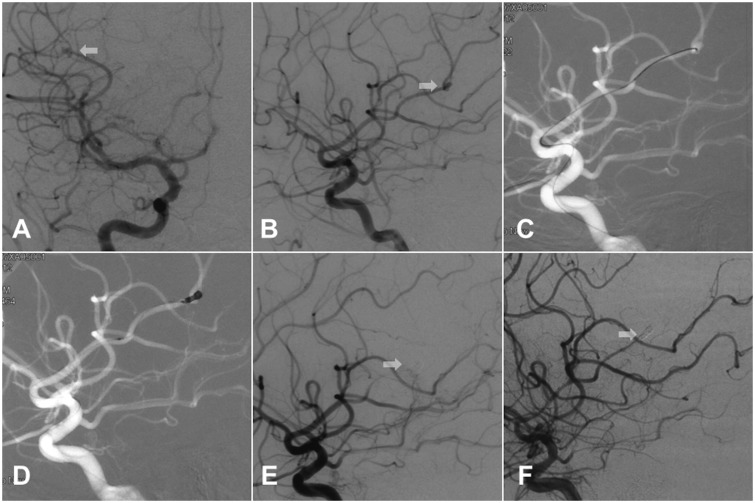
Figure 1.
Patient 3 is a 15-year-old male patient who presented with a sudden onset of severe headache, with nausea and vomiting. Digital subtraction angiography in (a) and (b) demonstrated that there was an aneurysm (white arrow) measuring 1.5 mm, located at the M3 segment of the right MCA. After navigating the microcatheter into the aneurysm (c), three coils were deployed in the aneurysm and in the proximal parent artery (d). Postoperative angiography (e) showed complete non-development of the aneurysm and the 17-month angiographic follow-up (f) showed no recanalization (white arrow).
MCA: middle cerebral artery; mm: millimeter
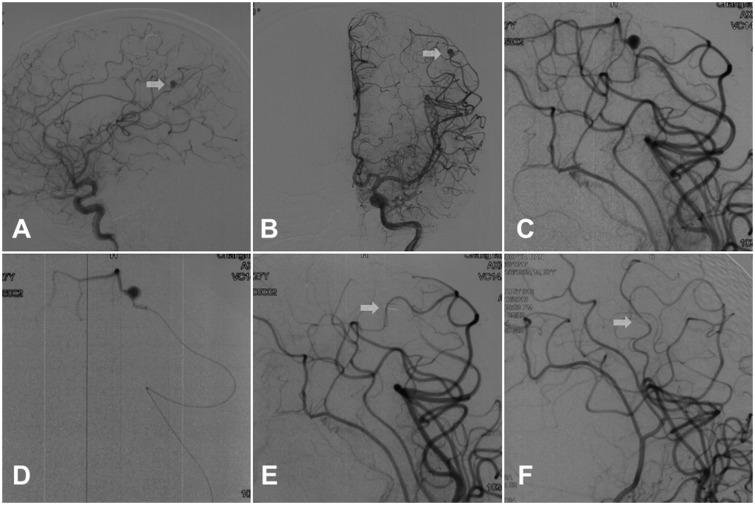
Figure 2.
Patient 6 was a 28-year-old patient who presented with a sudden onset of headache and unconsciousness. The patient underwent mitral valve replacement 6 months before. Emergency CT revealed a massive hematoma in the left fronto-parietal lobe and it received evacuation. Digital subtraction angiography showed an aneurysm located at the M4 segment of the left MCA ((a) and (b)). A hypersoft coil was introduced into the proximal segment of the aneurysm first, and then about 0.1 ml of Glubran glue was injected ((c) and (d)). Postoperative angiography (e) showed complete non-development of the aneurysm (white arrow). The 6-month follow-up angiography (f) showed the aneurysm was still completely occluded.
CT: computed tomography; MCA: middle cerebral artery
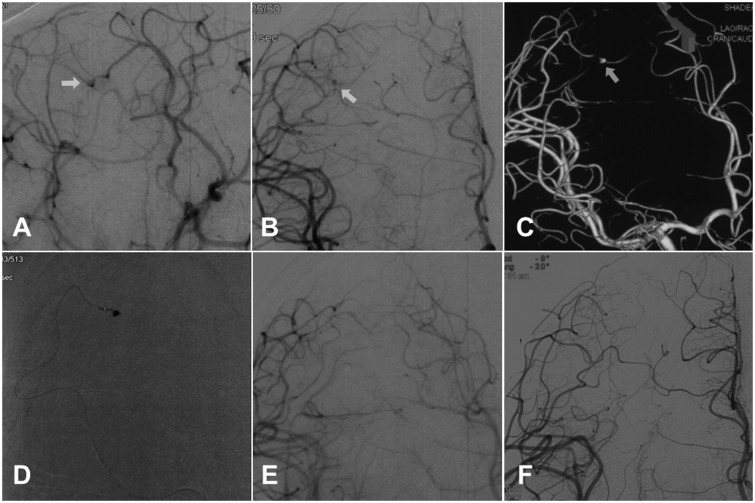
Figure 3.
Patient 7 was a 48-year-old male patient with bacterial endocarditis who presented with a severe headache and aphasia. Emergency CT demonstrated an intracranial hematoma in right frontal lobe. Digital subtraction angiography ((a) and (b)) with a 3-dimensional reconstruction (c) showed an aneurysm (white arrow) located at the M4 segment of the right MCA. The microcatheter was navigated to the proximal parent artery, but failed to be placed into the aneurysm. Therefore, diluted Glubran was directly injected into the parent artery (d). After 0.2 ml of the Glubran was injected, the aneurysm was completely occluded (e). The 7-month angiography (f) showed no recanalization.
CT: computed tomography; MCA: middle cerebral artery
Follow-up outcome
Clinical follow-up was achieved for all patients within a mean period of 36.8 months (ranging from 9–96 months), and all of the patients improved back to their pre-operative baseline, except for the patient with mild right hemiparesis after the hematoma evacuation. Angiographic follow-up was obtained for seven of the aneurysms, within a period ranging from 7–24 months (mean: 14.6 months). All of them remained stable without recanalization.
Discussion
A dMCA aneurysm is a rare entity. According to published articles, incidence ranges from 1.1–7% among all MCA aneurysms.2,5–7 The incidence in our series was 4.1%, which was also similar to previous reports. As reported before, these distal aneurysms were usually caused by other etiologies rather than hemodynamics, including infectious emboli caused by infective endocarditis, vasculitis, tumor emboli, brain trauma, etc.8–10 We encountered five aneurysms from infective endocarditis; however, in contrast to the Joo et al.6 description, most of the dMCA aneurysms we observed were saccular in shape, but the size and shape varied greatly.
Traditional treatment of these aneurysms is open surgery, aimed at evacuating the hematoma and obliterating the aneurysm. Some articles show good results following surgery. Horiuchi et al.2 report on nine patients treated with surgical repair: Eight patients recovered well and one had moderate disability; however, secondary brain edema, cerebral ischemia and post-operative seizure may potentially enhance the risk of neurological deterioration. Joo et al.6 report on eight similar patients (five clipping, two trapping, and one trapping with end-to-end bypass). Two of these patients died from severe brain swelling. In a series containing 28 patients, Calvacante et al.8 found favorable outcomes (modified Rankin Scale 0–2) in 19 of 28 patients (68.1%), a definitive morbidity in seven patients (24.9%) and death for two patients (7.2%). Also, aneurysms beyond the M2 segment are difficult to find without neuronavigation techniques: The aneurysm and parent artery are usually inside one of the compartments of the distal sylvian cistern, hidden by the frontal or the temporal operculum.7 It would be difficult to perform hematoma evacuation and aneurysm clipping at the same time, especially because some of them are tiny aneurysms, as in our series. Two patients in our series were treated via open surgery, but when the surgeons failed to find the aneurysms, only hematoma evacuation was performed.
Endovascular treatment is an alternative treatment to surgery for intracranial aneurysms, but reports are rare for dMCA aneurysms. In this series, we treated the eight dMCA aneurysms via the endovascular approach. The patients’ treatment consideration was based on:
Infectious aneurysms, responding poorly or not at all to appropriate antibiotic treatment;
Patients with previous anticoagulation or antiplatelet therapy;
Multiple aneurysms, with intent to treat at one stage; or
Some aneurysms that were difficult to be localized, due to their tiny size and/or parenchymal location.
We believe these would be indications for the use of EVT on these dMCA aneurysms.
Most of our cases were located more distally than they were previously reported1; however, our experience showed that EVT is still feasible for this entity, despite the fact that the route is far and tortuous, for reaching these aneurysms. For aneurysms beyond the M2 segment, the parent arteries are difficult to preserve. In our practice, for the aneurysms in which microcatheters may be able to be delivered into the aneurismal sac, the microcatheters we chose were mostly echelon-10, via which we would be able to introduce the coils and also inject the glue.
The hypersoft coils are soft and impose little radical force to the aneurismal wall, which is safe for intra-saccular embolization techniques. Using coils to occlude the aneurysm and parent artery also minimized the effects on the parent artery, as compared with the glue.
For the aneurysms that were not able to be super-selected or were too tiny to perform intra-saccular embolization, we would prefer the Marathon microcatheter, so that the microcatheter could be navigated as far as possible. When navigated far enough, the microcatheter would temporarily block blood flow, which helps to control the glue injection. The parent artery distal to the aneurysm was preserved as much as we possibly could, so that pial collaterals could supply adequate blood, to prevent neurological deficits.
The Glubran used in a concentration of about 33% was a good choice for these aneurysms, as it permitted simultaneous sealing of the aneurysms, while minimizing the reflux. Furthermore, a combination of a coil and glue was used to avoid migration of the glue, so that leptomeningeal collaterals could take over the distal vasculature. Recently, the application of Onxy 18/34 on distal intracranial aneurysms has also been reported by Chalouhi et al.11, who believe that has the advantages of having a non-adhesive nature and ease of use, which would allow for longer, slower and more controlled injections.
The main concerns about EVT for dMCA aneurysms were: Perforator injury during microcatheter navigation and ischemic complications caused by PAO. Perforator injury was seldom reported before; however, neurologic deficits following PAO have been reported.12,13 Based on this consideration, some authors suggest performing provocative tests when treating these aneurysms, using balloon, detachable coils or amobarbital14,15; however, we did not perform any of these for those aneurysms receiving PAO, since the parent arteries were difficult to preserve, regardless of the use of EVT or surgery. We believe that the test would not change the treatment. Luckily, ischemic complications are not often encountered when performing PAO for these distal aneurysms. The pial collaterals’ supply seems to prevent neurological deficits. Baltacioglu et al.1 report on 11 dMCA aneurysms that were treated via the endovascular approach, including seven aneurysms which were treated with aneurysmal sac and parent artery coiling. They found that if the parent artery could not be preserved, the pial collaterals would supply adequate blood for prevention of neurological deficits. Endovascular treatment, regardless of the use of selective aneurysm embolization or PAO, seemed to be safe for dMCA aneurysms.
Since these dMCA aneurysms are mostly caused by other etiologies, rather than by hemodynamics, recanalizations are seldom observed in these aneurysms treated via the endovascular approach. As in this series, none of the aneurysms treated experienced recanalization.
We acknowledge that the major limitation of this study was its limited number of cases in one single institution; however, this report of eight cases has been one of the largest series reported around the world. Our data, combined with the literature review, showed that endovascular treatment is a safe and effective alternative for the treatment of dMCA aneurysms, so it should be considered when treating these aneurysms.
Conclusions
Our data indicated that endovascular treatment is a safe and effective method for distal middle cerebral artery aneurysms.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Science and Technology Commission of Shanghai Municipality (grant numbers 13411950300 and 10441901902), the Changhai Hospital (1255 Project number CH125520100) and the National Natural Science Foundation of China (grant number 81400979).
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Baltacioglu F, Cekirge S, Saatci I, et al. Distal middle cerebral artery aneurysms. Endovascular treatment results with literature review. Interv Neuroradiol 2002; 8: 399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horiuchi T, Tanaka Y, Takasawa H, et al. Ruptured distal middle cerebral artery aneurysm. J Neurosurg 2004; 100: 384–388. [DOI] [PubMed] [Google Scholar]
- 3.Gibo H, Carver CC, Rhoton AL Jr, et al. Microsurgical anatomy of the middle cerebral artery. J Neurosurg 1981; 54: 151–169. [DOI] [PubMed] [Google Scholar]
- 4.Hunt WE and Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg 1968; 28: 14--20. [DOI] [PubMed]
- 5.Rinne J, Hernesniemi J, Niskanen M, et al. Analysis of 561 patients with 690 middle cerebral artery aneurysms: Anatomic and clinical features as correlated to management outcome. Neurosurgery 1996; 38: 2–11. [DOI] [PubMed] [Google Scholar]
- 6.Joo SP, Kim TS, Choi JW, et al. Characteristics and management of ruptured distal middle cerebral artery aneurysms. Acta Neurochir 2007; 149: 661–667. [DOI] [PubMed] [Google Scholar]
- 7.Dashti R, Hernesniemi J, Niemela M, et al. Microneurosurgical management of distal middle cerebral artery aneurysms. Surg Neurol 2007; 67: 553–563. [DOI] [PubMed] [Google Scholar]
- 8.Calvacante T, Derrey S, Curey S, et al. Distal middle cerebral artery aneurysm: A proposition of microsurgical management. Neurochirurgie 2013; 59: 121–127. [DOI] [PubMed] [Google Scholar]
- 9.Chen Z, Yang Y, Miao H, et al. Endovascular treatment of ruptured peripheral intracranial aneurysms. Neurosciences 2012; 17: 133–138. [PubMed] [Google Scholar]
- 10.Dhomne S, Rao C, Shrivastava M, et al. Endovascular management of ruptured cerebral mycotic aneurysms. Br J Neurosurg 2008; 22: 46–52. [DOI] [PubMed] [Google Scholar]
- 11.Chalouhi N, Tjoumakaris S, Gonzalez LF, et al. Endovascular treatment of distal intracranial aneurysms with onyx 18/34. Clin Neurol Neurosurg 2013; 115: 2528–2532. [DOI] [PubMed] [Google Scholar]
- 12.Andreou A, Ioannidis I, Mitsos A. Endovascular treatment of peripheral intracranial aneurysms. Am J Neuroradiol 2007; 28: 355–361. [PMC free article] [PubMed] [Google Scholar]
- 13.Mitsos AP, Corkill RA, Lalloo S, et al. Idiopathic aneurysms of distal cerebellar arteries: Endovascular treatment after rupture. Neuroradiology 2008; 50: 161–170. [DOI] [PubMed] [Google Scholar]
- 14.Douds GL, Kalapos P, Cockroft KM. Temporary test occlusion of distal middle cerebral artery using gdc coil. J Neuroimaging 2010; 20: 183–186. [DOI] [PubMed] [Google Scholar]
- 15.Wang Q, Chen G, Gu Y, et al. Provocative tests and parent artery occlusion in the endovascular treatment of distal middle cerebral artery pseudoaneurysms. J Clin Neurosci 2011; 18: 1741–1743. [DOI] [PubMed] [Google Scholar]