Abstract
Purpose
Primary orbital varix is a rare lesion but difficult to treat. Our main aim was to demonstrate the varices and their central venous communication and to explore the feasibility of embolization of these lesions.
Method
In four patients with clinical suspicion of varix, in whom MRI showed retro-global vascular channels, microcatheter digital subtraction angiography (DSA) of the varices was performed using femoral venous access. Embolization was carried out in two patients.
Results
In all four patients orbital varices could be accessed with a microcatheter through inferior petrosal sinus and ophthalmic vein (superior or inferior) route. Microcatheter angiography showed opacification of varices and demonstrated their central venous communication. Two patients were treated with coil embolization. Complete resolution of symptoms was seen in one patient and partial relief in the other.
Conclusion
The study presents microcatheterization of orbital varices via the inferior petrosal sinus–cavernous sinus–ophthalmic vein route with injections into distal ophthalmic veins for demonstration of these variceal sacs and their central venous connection. Coiling to disconnect the venous communication should be the primary goal of embolization.
Keywords: Orbital varix, embolization, neuro-ophthalmology
Introduction
Vascular lesions are uncommon in the orbit, and their classification depends upon histological composition, with a few characteristic patterns on imaging.1,2 For uniform nomenclature, a consensus statement on terminology of orbital vascular lesions was issued by the Orbital Society in 1999. Lesions were divided into three types: type 1 lesions are no-flow lesions, including lymphangiomas; type 2 are venous flow lesions, which also include mixed no-flow and venous flow lesions, apart from venous ectasias and varices; and type 3 are arterial flow lesions that include arteriovenous malformation.3
Orbital venous varices consist of single or multiple ectatic dilated venous structures that are in communication with the systemic vasculature. They are of two types: primary and secondary. Primary varices are congenital, idiopathic and mostly confined to the orbit. Secondary varices are acquired because of high flow due to arteriovenous malformation or due to any cause resulting in drainage via the orbit, leading to secondary orbital varices.1–3 For secondary varices, the cause of the increased blood flow needs to be treated. Orbital venous varices of the primary idiopathic type are rare lesions, and these generally present with intermittent proptosis, mainly during Valsalva maneuver and postural changes,1–3 but are also the most common cause of spontaneous orbital hemorrhage. Treatment of these primary orbital venous varices is challenging, and only a few case reports of their successful endovascular treatment exist.4–6 We investigated four cases of orbital varices using microcatheter venography through the inferior petrosal sinus–cavernous sinus–ophthalmic ophthalmic vein route under general anesthesia. Improved imaging and microcatheter technology allows catheterization through this route more easily than before. We highlight the importance of selective microcatheterization of these varices and the demonstration of their central venous communication. This was followed by coil embolization in two cases in this study.
Case description
Case 1
This 28-year-old female presented with intermittent left eye proptosis, which occurred on bending forward, and on straining. This was associated with orbital pain and diplopia. On examination, there was no bruit or pulsation. Ophthalmologic examination revealed normal visual acuity and no field or fundus defect. Ocular movements were normal.
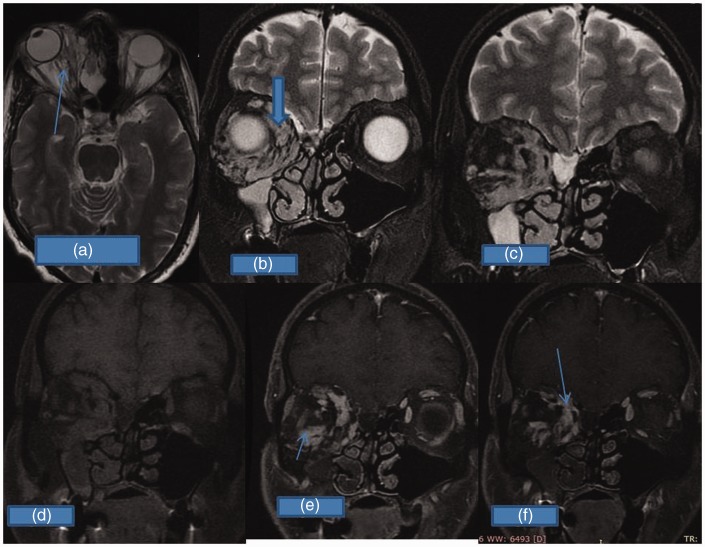
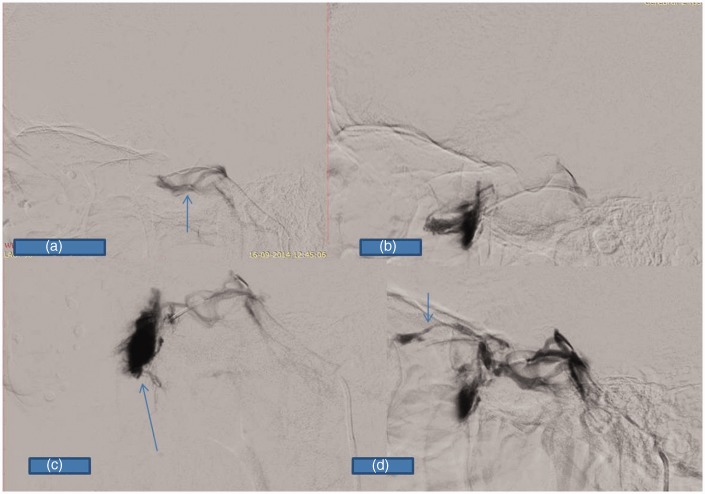
MRI showed an intraconal hypo- to isointense mass (Figure 1(a) to (c)), which showed delayed intense contrast enhancement (Figure 1(d) to (f)). Under general anesthesia, venography/phlebography through the right femoral venous route was performed. A microcatheter (Progreat, Terumo Corporation, Belgium) was placed through the left inferior petrosal sinus (Figure 2(a) and (b)) via the cavernous sinus and superior ophthalmic vein into the orbital variceal sac (Figure 2(c) and (d)). A few detachable coils were deployed in the sac (Figure 2(e)); however, dense packing was avoided. Despite this, a small leak was identified at the time of coiling. This was followed by coiling of the distal part of the superior ophthalmic vein, which was communicating with these varices (Figure 2(f)). After embolization, there was no filling of these varices from the cavernous sinus. The inferior ophthalmic vein showed no communication with these sacs and was left patent (Figure 2(f)). On follow up, this patient showed excellent relief of her symptoms within a month of the procedure, and was symptom free when she came for follow up after a year.
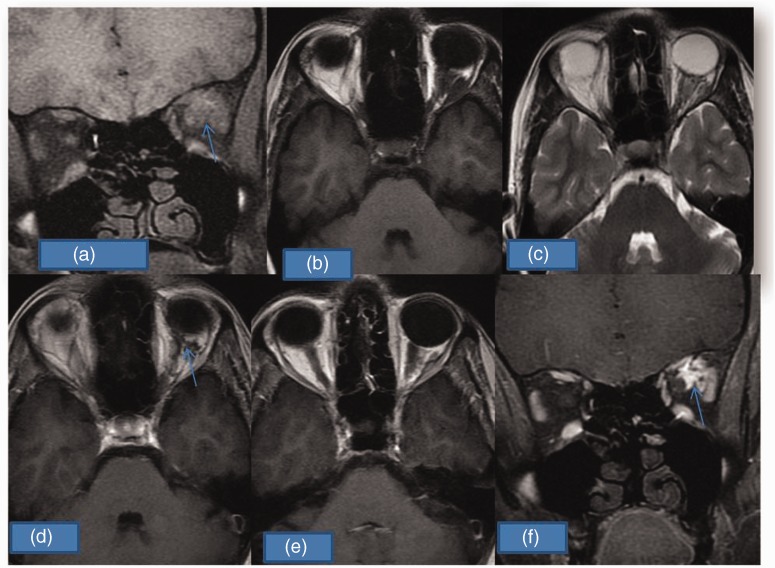
Figure 1.
(a) Coronal Fat Sat T1W shows intraconal hypointense mass (arrow) on left side. (b) Mass is also hypointense on axial T1W. (c) Hypointense mass on T2W axial scan. (d) and (e) Post-contrast minimal enhancement (arrow). (f) This becomes more intense (arrow) on delayed coronal post-gadolinium scan.
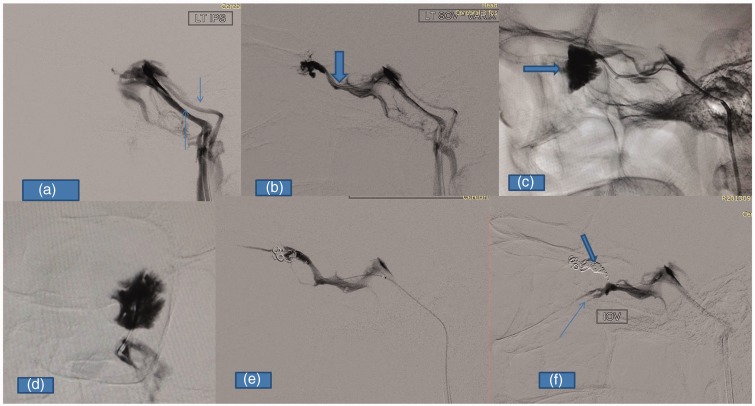
Figure 2.
(a) Lateral angiogram from the origin of the left inferior petrosal sinus shows opacification of both inferior petrosal sinus (arrow) with opacification of the cavernous sinus. (b) Angiogram taken using a microcatheter placed proximally into the superior ophthalmic vein via the cavernous sinus (thick arrow). (c) Opacification of the lobulated venous variceal mass (thick arrow). (d) Similar findings in postero-anterior projection. (e) Few detachable coils are placed inside the variceal mass, but the superior ophthalmic vein is still opacified. (f) The superior ophthalmic vein is coiled (thick arrow) to cut off varices completely from the central venous system, and the inferior ophthalmic vein (thin arrow) is well opacified but does not show any communication with these varices.
Case 2
This was a case of a 19-year-old female who presented with proptosis on the left side on straining and bending forward, which was associated with retro-orbital pain. Her ophthalmological examination, including visual acuity, ocular movements, field and fundus, was unremarkable. MRI of the orbits revealed a T2 hyperintense (Figure 3(a) and (b)) and a T1 hypo- to isointense intra- and extraconal mass lesion (Figure 3(c) and (d)) with delayed contrast enhancement (Figure 3(e) and (f)) suggestive of varices. She underwent microcatheterization through the right femoral venous route, going through the same route via the left inferior petrosal sinus (Figure 4(a)). Microcatheter angiography in the superior ophthalmic vein showed communication with the distended venous sacs (Figure 4(b) and (c)). The patient underwent embolization with detachable coils. A few coils were placed in the sac and the rest in the distal superior ophthalmic vein so as to cut off its central venous communication (Figure 4(d) to (f)). On follow up, the patient showed partial relief of her symptoms with preserved normal visual acuity.
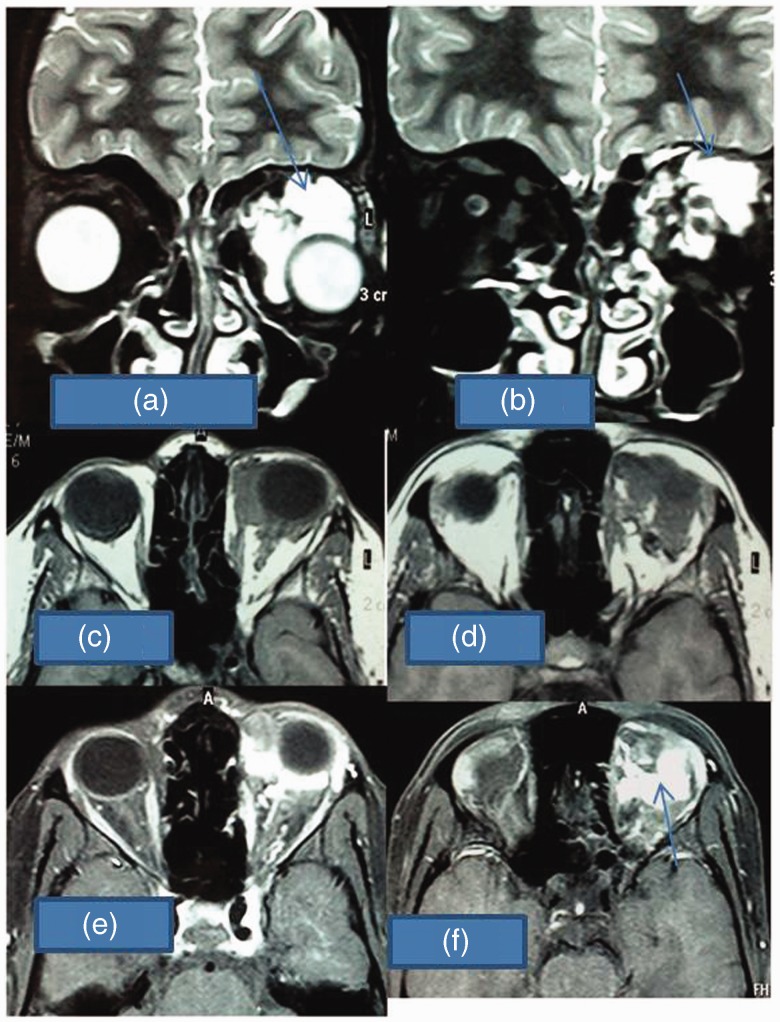
Figure 3.
(a) and (b) Coronal T2W image showing hyperintense (arrow) lobulated mass on left side. (c) and (d) Mass is hypointense on T1W axial scans. (e) and (f) Mass shows intense enhancement on post-gadolinium T1W scans (arrow), suggestive of venous varix on left side.
Figure 4.
(a) Lateral angiogram from the left inferior petrosal sinus ostia showing opacification of cavernous sinus (thick arrow) and inferior petrosal sinus (arrow). (b) Angiogram taken by the microcatheter placed inside the cavernous sinus with opacification of the superior ophthalmic vein, but not the varices. (c) The varices are opacified only when the angiogram is taken from the superior ophthalmic vein itself (thick arrow). (d) and (e) Few coils are placed inside the varix (thick arrow). (f) Complete cut off of these varices from the central venous system after superior ophthalmic vein is coiled (arrow).
Case 3
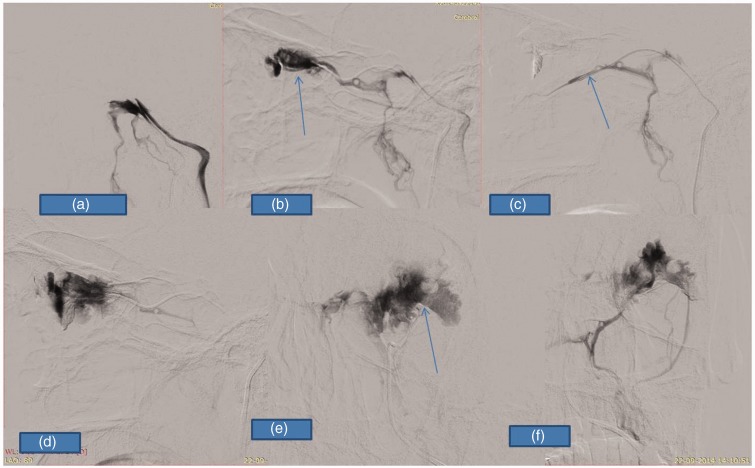
This 38-year-old male had similar complaints of proptosis on straining, but no significant retro-orbital pain. On MRI, there was a loculated lesion in the right orbit involving both intra- and extraconal compartments (Figure 5(a) to (d)). No intracranial extension of the lesion was seen, and there was a bright enhancement of loculated components in post-gadolinium scans (Figure 5(e) and (f)). We performed phlebography in this patient through a similar right femoral venous route, with selective catheterization of the right inferior petrosal sinus using a 5 F catheter (Figure 6(a)); further catheterization of the cavernous sinus and ophthalmic vein was done with a Progreat microcatheter (Terumo Corporation, Belgium). Multiple distended sacs were demonstrated on selective catheterization, which were communicating with the inferior ophthalmic vein (Figure 6(b) and (c)), with no sac seen to be communicating with the superior ophthalmic vein (Figure 6(d)). This patient has so far not undergone any therapeutic procedure.
Figure 5.
(a) Axial T2W and (b) and (c) coronal T2W images showing lobulated hypointense mass in the intra- and extraconal compartment on the right side (arrow (a) and thick arrow (b)). (d) T1W coronal scan also showing a hypointense mass. (e) and (f) Mass showed delayed enhancement on post-gadolinium scan (arrows).
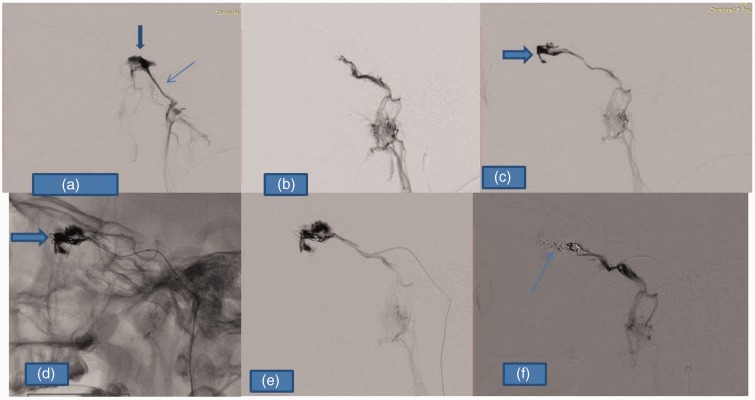
Figure 6.
(a) Lateral angiogram taken from distal right inferior petrosal sinus showing opacification of the cavernous sinus (arrow). (b) and (c) Opacification of varices (arrow (c)) when angiogram is taken from the distal inferior ophthalmic vein. (d) Superior ophthalmic vein (arrow) does not show any communication with these varices.
Case 4
This was a case of a 20-year-old female with complaints of proptosis on the left side, especially during forward bending. She had contrast CT of the orbit, which revealed a lobulated tortuous lesion involving the intraconal compartment. We performed venography through the same route (Figure 7(a) and (b)) and demonstrated multiple distended sacs (Figure 7(d) to (f)) communicating with the superior ophthalmic vein, with no sacs seen to be communicating with the inferior ophthalmic vein (Figure 7(c)). This patient also has so far not undergone any therapeutic procedure.
Figure 7.
(a) Lateral angiogram taken from the left inferior petrosal sinus showing opacification of the cavernous sinus, but not of the superior ophthalmic vein and the varices. (b) Varices are opacified only when the angiogram is taken with the microcatheter placed inside the distal superior ophthalmic vein (arrow points toward the varices). (c) Opacification of the inferior ophthalmic vein (arrow), which does not show any communication with the varices. (d) Lateral angiogram showing opacification of varices when angiogram is taken from inside the varix reached via superior ophthalmic vein route. (e) and (f) Postero-anterior projection images showing opacification of these varices (arrow (e)).
In all the four cases, we found that injection into the cavernous sinus with a microcatheter did not allow the opacification and demonstration of the varix. Selective injection of the superior and inferior ophthalmic veins was necessary to fill the varix and to demonstrate the communication. Varices were found to communicate with the superior ophthalmic vein in three of our cases and with the inferior ophthalmic vein in one of the cases.
Discussion
The orbital venous system normally consists of superior and inferior orbital veins as the main venous drainage system, which communicate with the cavernous sinus either together or separately. Among the inconstant veins, the middle and medial ophthalmic veins and collateral veins joining the superior and inferior system are described. The intraorbital venous system communicates anteriorly with the facial and frontal veins, posteriorly with the cavernous sinus and the pterygoid plexus, and medially with the ethmoid veins.7
Primary orbital varix is a rare lesion, which consists of dilated tortuous veins in the intraorbital location and is considered to be a developmental malformation, thought to have developed due to post-capillary venous wall weakness.1 It does have communication with native orbital veins, but is often in a collapsed state. The varix gets distended in a forward-bending posture or Valsalva-like maneuver, especially when communication with the native venous system is large.8,9 The literature is not clear on which of the venous components are involved in the formation of an orbital varix. It is also not clear whether the varix also communicates with the extraorbital venous system directly, or whether it does so exclusively through the main ophthalmic veins, and whether the communication exists at a single site or multiple sites. We found communication through the superior ophthalmic vein in the majority of cases. When this central communication is small, these orbital varices present with sudden thrombosis or orbital hemorrhage, causing intense pain with more sustained proptosis.1,2 On cross-sectional imaging such as CT and MRI, they appear as a tangled mass of vessels in the intraconal compartment and show delayed intense enhancement. Orbital venogram using forehead venous puncture has been an important diagnostic investigation in the past. However, CT/MRI and the clinical picture are often adequate for diagnostic purposes. Orbital venographic opacification of the varix may not adequately demonstrate the communication site with the main orbital veins. Optimal digital subtraction angiography imaging may not be feasible with this technique, which involves manual compression of angular veins.
Functionally, the orbital varix is probably not a very important structure for venous drainage of the orbital tissues. Surgical treatment comprises removal of the tangle of veins of the variceal abnormality. Surgical experience has shown that removal of the varix apparently does not significantly affect the venous drainage of the orbit. Surgery would theoretically seem to be the ideal curative treatment, but is plagued with problems, such as bleeding at the time of surgery, incomplete removal, injury to neural structures, and post-operative scarring.10–12 The Orbital Society divided these varices into distensible and non-distensible, and the consensus was that the non-distensible ones should be treated by surgical excision and the distensible ones by endovascular embolization, with the main goal of isolating these channels proximally and distally.3,12
However, there are only a few case reports, and no large series has been published so far. Hence, no definite treatment protocol has been established. Only symptomatic varices need active treatment. There are two main indications for intervention in these patients: intractable orbital pain and cosmetic disfigurement.13 As the surgical risks are greater, endovascular management is the procedure of choice for distensible, deeply located and symptomatic orbital varices.12 One of the earliest cases treated with the endovascular approach was described by Takechi et al.,5 who took the same route as we did and successfully coiled the varices. They also mentioned that reaching the varices is not always easy. A few case reports exist in which surgical access to these sacs was followed by endovascular coiling.4 There is one case report in which a facial venous route was used to reach the orbital varices.6 In all these cases, the inferior petrosal sinus was hypoplastic or was replaced by multiple venous channels and not amenable to catheterization. Apart from surgical excision and endovascular coil embolization, a few other treatment options have been tried in orbital varices. Electrothrombosis of a superior ophthalmic vein varix is described in one case report, but further experience with this technique is not reported anywhere, and the procedure may have limitations in large varices.14 Surgical exposure and direct puncture venography with compression over both orbital fissures to control flow is also described. This was followed by cyanoacrylate glue injection before excision.15 Using a liquid sclerosing agent such as absolute alcohol is also described, but injecting it without fluoroscopic controls appears to be risky.
It is common knowledge that bending forward or the Valsalva maneuver leads to an increase in the volume of orbital varices, especially the distensible type. Apart from gravity, diversion of venous drainage via the cavernous sinus appears to be an important factor leading to the distension of the varix in these situations. Apparently this happens in those lesions that have a relatively large communication with the cavernous sinus through the main ophthalmic veins. Our diagnostic procedure is to define this communication in order to plan how to close it.
In our cases, the inferior petrosal sinuses were small in size, but microcatheterization was possible. In our experience, cavernous sinus injection does not readily opacify these varices. A selective ophthalmic venous injection not only opacifies these varices but also shows their central venous communication site. We feel that communication with the cavernous sinus contributes to the progression and symptomatology in this condition, as it connects the high-pressure intracranial venous system with the low-pressure extracranial venous system.
The endovascular approach and coiling through the inferior petrosal sinus does theoretically have risks, such as venous rupture and bleeding, but with due care, these can be avoided. Fortunately, the malformation is low pressure and the hemorrhage is likely to be self contained. Thrombosis of the cavernous sinus or inferior petrosal sinus may be another theoretical possibility. Procedures such as inferior petrosal sinus sampling for Cushing’s microadenoma and cavernous sinus coiling for the indirect type of carotid cavernous fistula are frequently performed, and do not suggest significant thrombotic complications involving the inferior petrosal sinus. Hence, this procedure can be safely undertaken through the inferior petrosal sinus route.
Only one case report mentions compressive optic neuropathy and vision loss after coil embolization. Apparently, in this case, dense packing of the varices led to thrombosis and enlargement of these sacs.16 To prevent this, dense packing of these sacs is to be avoided, and the distal superior ophthalmic vein is sealed with coils so as to cut their central venous connection, thus limiting their distension. In addition, the walls are very fragile in the varix and may cause extravasation during attempted dense packing. It has been proposed that embolization would be useful only in cases of saccular venous dilatation, but not in entangled venous plexus.12 We advocate coiling of the distal central venous segment to disconnect the varix. We feel that coiling of the variceal sacs is not as important as disruption of its connection with the central venous system. In addition, embolization does not preclude a future surgical procedure if required. As a preliminary experience, we planned the diagnostic and embolization procedures separately. However, with experience, these can be performed in the same setting. We feel that the procedure is reasonably safe. The long-term efficacy of this approach, however, needs further evaluation. Taking a cue from the report by Lacey et al.,15 if a good seal of the varix outlet/inlet from the cavernous sinus side can be obtained with either coiling or a balloon catheter, the varix can also be embolized with Onyx (EVOH, EV3, USA) or a similar material. The seal will prevent it from leaking toward the cavernous sinus, and the embolic agent in the channels of the varix may provide a more lasting result. This approach needs to be explored. Embolization may not have any role in thrombosed varices or in hemorrhage.
Conclusion
Symptomatic orbital varices need aggressive management. Surgical excision is preferable where hemorrhage or thrombosis has occurred and also in superficial non-distensible lesions. In the distensible type of lesions, where anatomy is suitable, coil embolization through the central venous route appears to be the preferred option. Alternative treatment modalities can be kept as backup options where inferior petrosal or cavernous sinus cannulation is not possible. We emphasize microcatheterization of orbital varices via the inferior petrosal sinus–cavernous sinus–ophthalmic veins route with injections into distal ophthalmic veins. This is not only to demonstrate these venous sacs, but mainly to show the connection of these varices with superior or inferior ophthalmic veins. It is important to demonstrate this in order to undertake the embolization treatment. General anesthesia is preferable to make the procedure pain free and to give the necessary anatomical detail. Coiling to disconnect the venous communication should be the primary goal of embolization.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Smoker WR, Gentry LR, Yee NK, et al. Vascular lesions of the orbit: More than meets the eye. Radiographics 2008; 28: 185–204. [DOI] [PubMed] [Google Scholar]
- 2.Lebedis CA, Sakai O. Nontraumatic orbital conditions: Diagnosis with CT and MRI imaging in emergent setting. Radiographics 2008; 28: 1741–1753. [DOI] [PubMed] [Google Scholar]
- 3.Harris GJ. Orbital vascular malformations: A consensus statement on terminology and its clinical implications. Am J Ophthalmol 1999; 127: 453–455. [DOI] [PubMed] [Google Scholar]
- 4.Weill A, Cognard C, Castaings L, et al. Embolization of an orbital varix after surgical exposure. Am J Neuroradiol 1998; 19: 921–923. [PMC free article] [PubMed] [Google Scholar]
- 5.Takechi A, Uozumi T, Kiya K, et al. Embolisation of orbital varix. Neuroradiology 1994; 36: 487–489. [DOI] [PubMed] [Google Scholar]
- 6.Mavilio N, Pau A, Pisani R, et al. Embolisation of orbital varix via the superficial temporal vein. Interv Neuroradiol 2000; 6: 137–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayreh SS. Orbital vascular anatomy. Eye 2006; 20: 1130–1144. [DOI] [PubMed] [Google Scholar]
- 8.Rubin PA, Bilyk JR, Dunya IM, et al. Spiral CT of an orbital venous malformation. AJNR Am J Neuroradiol 1995; 16: 1255–1257. [PMC free article] [PubMed] [Google Scholar]
- 9.Rubin PA, Remulla HD. Orbital venous anomalies demonstrated by spiral computed tomography. Ophthalmology 1997; 104: 1463–1470. [DOI] [PubMed] [Google Scholar]
- 10.Beyer R, Levine MR, Sternberg I. Orbital varices: a surgical approach. Ophthal Plast Reconstr Surg 1985; 1: 205–210. [DOI] [PubMed] [Google Scholar]
- 11.Song G, Tian W, Qiang DF, et al. Surgical treatment of orbital varices. Chin Med J 1979; 92: 723–728. [PubMed] [Google Scholar]
- 12.Arat YO, Mawad ME, Boniuk M. Orbital venous malformations: Current multidisciplinary treatment approach. Arch Ophthalmol 2004; 122: 1151–1158. [DOI] [PubMed] [Google Scholar]
- 13.Miller NR. Walsh and Hoyt’s clinical neuro-ophthalmology, 4th ed Baltimore: Williams & Wilkins, 1988, pp. 1503–1508. [Google Scholar]
- 14.Handa H, Mori K. Large varix of the superior ophthalmic vein: Demonstration by angular phlebography and removal by electrically induced thrombosis. J Neurosurg 1968; 29: 202–205. [DOI] [PubMed] [Google Scholar]
- 15.Lacey B, Rootman J, Marotta TR. Distensible venous malformations of the orbit: Clinical and hemodynamic features and a new technique of management. Ophthalmology 1999; 106: 1197–1209. [DOI] [PubMed] [Google Scholar]
- 16.Hwang CS, Lee S, Yen MT. Optic neuropathy following endovascular coiling of an orbital varix. Orbit 2012; 31: 418–419. [DOI] [PubMed] [Google Scholar]