Abstract
Neurogenic tumors are the most prevalent tumors of the mediastinum, and schwannomas are the most common type of neurogenic tumor. Primary neurogenic neoplasm of the esophagus is uncommon and malignant schwannoma of the esophagus is extremely rare. We report a case of a 27-year-old female presenting with dysphagia and palpitations who was found to have a lobulated tumor in the mediastinum that was compressing the esophageal lumen. The tumor was successfully treated surgically without recurrence. The final diagnosis, on histopathological examination of the specimen, was malignant schwannoma.
Keywords: Schwannoma, Neurilemmoma, X-ray computed tomography, Esophagogastric junction
CASE REPORT
The most common benign tumor of the esophagus is leiomyoma, and primary esophageal schwannoma is extremely rare. To date, about 27 reports of esophageal schwannomas have been published in the literature, most of which are benign lesions. Malignant esophageal schwannoma is much more rare, with only three cases previously reported in the literature [1]. Esophageal schwannoma is more common in females and is mostly found in the upper and middle esophagus [2]. As the imaging appearance is similar to that of leiomyoma, preoperative diagnosis of schwannoma is difficult, and definitive diagnosis is mostly established after resection [3]. Here we present an unusual case of malignant schwannoma of the esophagus in a young female that was treated successfully with surgery.
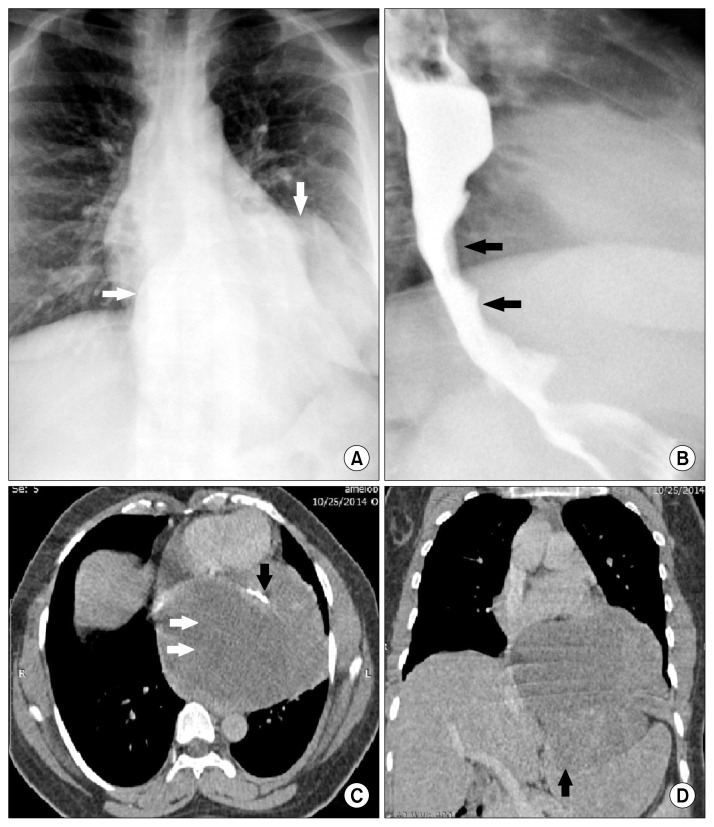
A 27-year-old female presented to our hospital with complaints of gradual onset of dysphagia for five years associated with intermittent episodes of palpitations, and weight loss without loss of appetite. Her symptoms had worsened over the preceding two months. Her medical history was otherwise unremarkable. A chest radiograph (Fig. 1A) revealed a smooth well-defined mass in the posterior mediastinum with a loss of the normal silhouette of the cardiac borders. A barium swallow was performed to evaluate the dysphagia, and a smooth extrinsic impression was seen on the distal esophagus and gastro-esophageal junction (Fig. 1B). Endoscopy showed an extrinsic bulge 30 cm distal to the incisors at the gastro-esophageal junction, with normal overlying mucosa. Subsequently, thoracic contrast-enhanced computed tomography (CT) was performed. This revealed a large lobulated low-density mass (Fig. 1C, D) in the middle mediastinum arising from the anterior and left lateral walls of the lower thoracic esophagus and containing areas of necrosis and calcification. The lesion extended into the abdomen through the esophageal hiatus and compressed the fundus of the stomach. Based on the imaging studies a diagnosis of leiomyoma of the esophagus was made. Laboratory parameters, including pulmonary function tests, were unremarkable.
Fig. 1.
(A) Chest radiograph showing a well-defined retrocardiac soft tissue mass (white arrows) with intra-abdominal extension. (B) Barium swallow showing smooth luminal narrowing of the distal esophagus and gastroesophageal junction due to extrinsic compression by the mass (black arrows). (C) Axial contrast-enhanced CT image showing a large lobulated hypodense well-defined mass (white arrows) containing areas of calcification (black arrow). (D) Coronal reformat of CT scan showing the mass extending through the esophageal hiatus and compressing the fundus of the stomach (black arrow). CT, computed tomography.
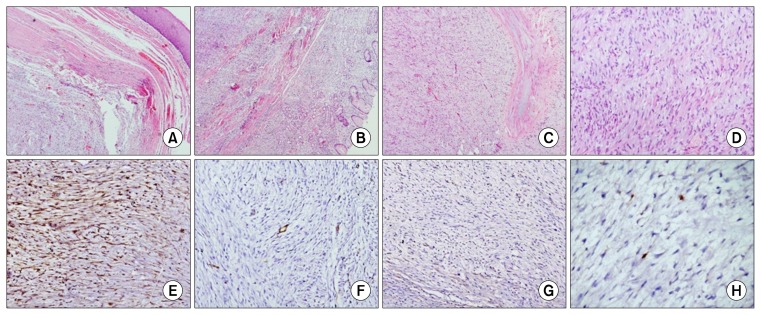
The patient was prepared for surgery. The esophagus was approached through a left thoraco-abdominal incision. A large firm to hard mass was seen arising from the mid- and distal thoracic esophagus and adherent to the diaphragm, pericardium, and aorta. Esophagectomy was performed and a gastric conduit was brought into the neck through the posterior mediastinal route. A tumor measuring 12×10×10 cm was seen adherent to the serosal aspect of the resected specimen of esophagus. A cut section of the tumor was solid and homogeneous with areas of whorling. Histopathology showed a lobulated spindle cell tumor with a focally infiltrative peripheral margin and atypical mitoses in 4/10 high power fields (Fig. 2). Spindle cells were immunopositive for S100 and negative for Dog1, CD117, CD34, and SMA. The Ki-67 labeling index was 2%–3% (Fig. 2). The dissected lymph node showed reactive features. Based on the above features, a diagnosis of low-grade malignant schwannoma of the esophagus was made.
Fig. 2.
Photomicrographs show (A) a well-circumscribed spindle cell lesion arising from the lower end of the esophagus (H&E, ×40) and (B) reaching up to the gastric fundus (H&E, ×40). (C) The mass is lobulated (H&E, ×40) and (D) shows fascicles with spindle cells showing hyperchromasia and nuclear buckling on a myxoid background (H&E, ×100). On immunohistochemistry, (E) these cells were positive for S100 protein (S100, ×40) and (F, G) negative for CD34 and DOG 1 stains (CD34 and DOG-1, ×100). (H) The Ki67 labeling index is low (Ki67, ×100).
Postoperatively, the patient had right recurrent laryngeal nerve palsy, possibly due to injury during dissection of the cervical esophagus. This was managed conservatively and the patient was discharged on the 17th postoperative day. A follow-up CT scan one year after surgery showed no evidence of tumor recurrence. The patient remained clinically asymptomatic 18 months after surgery.
DISCUSSION
Malignant schwannoma of the esophagus is a rare neoplasm. Patients usually present with dysphagia and dyspnea; however, a wide range of presentations have been reported, including chest pain, cough, and palpitations, with symptoms becoming worse as the size of the tumor increases [4]. Usually located in the proximal third of the esophagus, schwannomas are often described as hypo- or iso-attenuating with a homogeneous texture on CT scan and may contain areas of calcification that differentiate them from leiomyomas. Malignant schwannoma appears heterogeneous in non-contrast and contrast-enhanced CT scans and may have an ill-defined infiltrating border. A striking feature of gastrointestinal stromal tumors, in comparison with schwannomas, is the presence of hemorrhage, necrosis, and cystic changes, which give them a more heterogeneous appearance on CT. On magnetic resonance imaging, benign schwannomas are iso- or slightly hyperintense relative to muscles in T1-weighted images, and have a target appearance in T2-weighted images with a peripheral hyperintense rim and central low intensity [5]. Intense contrast enhancement is usually seen in most cases of schwannoma. The typical target appearance may not be present in malignant schwannomas.
Endoscopic ultrasonography with sufficient resolution can determine the tissue layer of origin of the tumor and a guided biopsy is helpful for diagnosis and management. A 18-fluoro-deoxyglucose uptake is seen in normal Schwann cells due to normal glucose uptake for axon repolarization, and is thus less useful for differentiating benign and malignant schwannomas [1]. On immunohistochemistry, the diagnosis of schwannoma is based on immunopositivitity for S100 protein and negative staining for CD-34, CD-117, and muscle specific actin (MSA) [6]. CD-34 and CD-117 are positive in gastrointestinal stromal tumors and desmin and MSA are positive in leiomyomas. Surgery is the only treatment option in schwannomas, as chemotherapy and radiotherapy are ineffective. Enucleation with video-assisted thoracoscopic surgery is ideal for small schwannomas less than 2 cm in size [3]. However, for larger tumors, esophagectomy with esophago-gastrostomy is usually performed [7,8].
In conclusion, preoperative diagnosis of primary esophageal neurogenic tumors is challenging, as their imaging appearance mimics leiomyoma. A high index of clinical suspicion is necessary because of the rarity of these tumors, their non-specific imaging appearance and vague clinical features, and the difficulty in sampling the tumor due to its submucosal position.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Wang S, Zheng J, Ruan Z, Huang H, Yang Z, Zheng J. Long-term survival in a rare case of malignant esophageal schwannoma cured by surgical excision. Ann Thorac Surg. 2011;92:357–8. doi: 10.1016/j.athoracsur.2011.01.045. [DOI] [PubMed] [Google Scholar]
- 2.Saito R, Kitamura M, Suzuki H, Ogawa J, Sageshima M. Esophageal schwannoma. Ann Thorac Surg. 2000;69:1947–9. doi: 10.1016/S0003-4975(00)01282-0. [DOI] [PubMed] [Google Scholar]
- 3.Park BJ, Carrasquillo J, Bains MS, Flores RM. Giant benign esophageal schwannoma requiring esophagectomy. Ann Thorac Surg. 2006;82:340–2. doi: 10.1016/j.athoracsur.2005.09.042. [DOI] [PubMed] [Google Scholar]
- 4.Byun JH, Park SD. Benign schwannoma of the esophagus: surgical experience of two cases. Korean J Thorac Cardiovasc Surg. 2005;38:589–93. [Google Scholar]
- 5.Anil G, Tan TY. Imaging characteristics of schwannoma of the cervical sympathetic chain: a review of 12 cases. AJNR Am J Neuroradiol. 2010;31:1408–12. doi: 10.3174/ajnr.A2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kobayashi N, Kikuchi S, Shimao H, et al. Benign esophageal schwannoma: report of a case. Surg Today. 2000;30:526–9. doi: 10.1007/s005950070120. [DOI] [PubMed] [Google Scholar]
- 7.Davis EA, Heitmiller RF. Esophagectomy for benign disease: trends in surgical results and management. Ann Thorac Surg. 1996;62:369–72. doi: 10.1016/0003-4975(96)00235-4. [DOI] [PubMed] [Google Scholar]
- 8.Dutta R, Kumar A, Jindal T, Tanveer N. Concurrent benign schwannoma of oesophagus and posterior mediastinum. Interact Cardiovasc Thorac Surg. 2009;9:1032–4. doi: 10.1510/icvts.2009.216440. [DOI] [PubMed] [Google Scholar]