Abstract
The severity of a patient’s illness may be detrimental for the psychological well-being of the spouse, especially for those in a particularly close relationship. Using 2 waves of data collected from a sample of 152 knee osteoarthritis (OA) patients and their spouses, we examined associations between change in patients’ illness severity and change in 3 indicators of spouses’ well-being (positive affect, depressive symptoms, and life satisfaction) over a 6-month period. We also tested the hypothesis that spouses’ perceived relationship closeness with the patient would moderate these associations. Consistent with our prediction, a high level of relationship closeness exacerbated the negative impact of increases in patient illness severity on spouses’ positive affect and depressive symptoms over 6 months. Spouses’ life satisfaction declined when patients became more ill, regardless of level of relationship closeness. Our findings highlight the value of examining change in illness as a predictor of change in spouse well-being and the potential downside of relationship closeness for couples living with chronic illness.
Keywords: arthritis, chronic illness, couples, relationship closeness
Prolonged exposure to a loved one’s physical suffering has been shown to have detrimental effects on the emotional well-being of the sufferer’s spouse (Monin & Schulz, 2009). However, most of this research has been cross-sectional in design and, as such, cannot address the effects on spouses of increases in patients’ functional limitations. In addition, little is known about the characteristics of spouses who are most vulnerable to patients’ suffering. A better understanding of these issues could lead to more targeted and impactful couple-based interventions for chronic illness (Martire, Schulz, Helgeson, Small, & Saghafi, 2010). The purpose of this study was to examine associations between change in the severity of patients’ osteoarthritis (OA) and change in their spouses’ psychological well-being (i.e., positive affect, depressive symptoms, and life satisfaction) over a 6 month period. We also examined whether these associations were stronger for spouses in a close relationship with the patient.
Prior research shows that greater illness severity is related to poorer concurrent psychological well-being in an individual’s close family members. Such associations have been shown to exist across a range of conditions including amyotrophic lateral sclerosis, multiple sclerosis, and chronic pain (e.g., Boerner & Mock, 2012; Flor, Turk, & Scholz, 1987; Lehan, Arango-Lasprilla, Macias, Aguayo, & Villaseñor, 2012; Leonard & Cano, 2006). These findings suggest that patients’ expression of their symptoms can take a toll on the emotional health of their loved ones. The effects of illness severity on close family members may be due in part to emotional contagion and appear to be independent of the level of caregiving provided. Specifically, distress in one partner can lead to distress in the spouse even when the spouse does not provide assistance with daily activities, or beyond the effects of such caregiving (Schulz et al., 2007; Siegel, Bradley, Gallo, & Kasl, 2004).
Some longitudinal research shows that spouses of patients with greater physical symptom severity tend to become more depressed over time (Schulz et al., 2009; Stephens, Martire, Cremeans-Smith, Druley, & Wojno, 2006). These two studies examined symptom severity at one time point as a predictor of spousal well-being at a later time; therefore, little is known about how spouses’ well-being may change as a function of patients’ worsening health status. Moreover, although chronic health conditions typically involve a range of symptoms that affect patients’ daily functioning, we are aware of only one prior study that has examined the effects of change in multiple indicators of illness severity on change in spouse well-being. In a sample of lung cancer patients and their spouses, Lyons and colleagues (2014) found that decreases in patient physical function were significantly associated with concurrent increases in spouses’ depressive symptoms over a 12-month period, whereas increases in patient pain severity were unrelated to change in spouse depression. Thus, broader measures of illness severity that capture patients’ functional limitations may be particularly useful in determining the overall impact of declines in patient health on spouse well-being across time. Taken together, findings from these three studies suggest that, while symptoms such as pain are an important indicator of patient functioning, an examination of change in the general severity of an illness (including physical function) may provide a more complete understanding of the long-term effects of chronic health conditions on spouses.
Targeting couple-based interventions for chronic illness at those who need them the most requires the identification of characteristics of spouses who experience the greatest emotional and health consequences (Martire & Schulz, 2012). One contextual factor that may affect the extent to which spouses are negatively impacted by their partner’s illness is the closeness of their relationship (Monin & Schulz, 2009). The self-expansion model defines closeness as including the partner in one’s concept of the self; the measure of this construct is thought to tap aspects of both subjective feelings and objective interaction (Aron & Aron, 1986; Aron, Aron, Tudor, & Nelson, 1991). For instance, a spouse who reports greater relationship closeness may feel very emotionally connected with his or her partner, and may be highly involved in the partner’s daily routines and activities. Closeness is only moderately correlated with relationship satisfaction, and the two constructs play different roles in regard to modulating the effects of one individual’s experiences on the partner’s well-being. Whereas having a satisfying relationship can buffer individuals from their partner’s daily stressors and negative mood (Saxbe & Repetti, 2010; Slatcher et al., 2010), adults who are in a very close or interconnected relationship may be the most negatively affected by a partner’s illness.
Supporting this point, a strong sense of self–other overlap, or closeness, has been shown to lead to more empathic responding (Cialdini, Brown, Lewis, Luce, & Neuberg, 1997). In addition, married older adults are more negatively impacted by each other’s depressive mood if both partners report that they are a confidant to the other, which is likely to characterize those in a close relationship (Tower & Kasl, 1995, 1996). Furthermore, contagion of negative affect between men with prostate cancer and their wives is exacerbated in couples who report working together as a team to manage the illness (Berg, Wiebe, & Butner, 2011). That is, spouses who collaborate in a manner that likely reflects a high level of relationship closeness may be most vulnerable to the adverse psychological effects of one another’s negative emotions. In a recent study focusing on daily experiences, daily OA knee pain had the strongest negative impact on spouses’ sleep among couples reporting a close relationship (Martire, Keefe, Schulz, Stephens, & Mogle, 2013). Collectively, findings from multiple studies suggest that changes in patient illness severity may have particularly strong effects on spouse well-being in the context of a close marital relationship.
Given that poorer psychological well-being is linked to a host of detrimental health consequences, including increased functional disability (Nyunt, Lim, Yap, & Ng, 2012; Zeiss, Lewinsohn, Rohde, & Seely 1996) and higher risk of mortality (Bogner, Morales, Reynolds, Cary, & Bruce, 2012; Geerlings, Beekman, Deeg, Twisk, & Van Tilburg, 2002), it is imperative to determine whether and under what conditions the spouse is adversely affected over time by his or her partner’s illness. The purpose of the present study was to extend the current literature by using a broader indicator of patient illness severity than previous studies, and by examining change in both illness severity and spouse well-being. Importantly, our models also controlled for the effects of patient well-being, as prior research indicates a high degree of concordance in partners’ mental health (Meyler, Stimpson, & Peek, 2007).
Using two waves of data collected from a sample of knee OA patients and their spouses, we aimed, primarily, to examine the longitudinal relationship between patient illness severity and three indicators of spouse well-being (positive affect, depressive symptoms, and life satisfaction). We predicted that increased patient illness severity over 6 months would be associated with decreased spouse well-being over the same time period. Our second aim was to evaluate whether spouse perceptions of having a close relationship with the patient exacerbated associations between change in patient illness severity and change in spouse well-being over 6 months. We used a common measure of relationship closeness created by Aron and colleagues (i.e., the Inclusion of Other in the Self Scale; IOS; Aron, Aron, & Smollan, 1992). We predicted that the negative effects of increased OA severity on spouse well-being would be stronger for spouses who reported being in a very close relationship with the patient compared to those who reported low closeness.
Method
Participants
Participants were drawn from a sample of 152 knee OA patients and their spouses who were recruited for an observational (i.e., nonintervention) study. Only relevant components of the study are described (for a detailed description of the larger study, see Martire et al., 2013). Trained staff conducted separate interviews with patients and spouses in their homes at baseline (T1), at a 6-month follow-up (T2), and at an 18-month follow-up (T3). Immediately after the T1 interview, participants completed a 22-day assessment of daily experiences related to illness management and couple interactions. For the current study, our interest was in data from the in-person interviews at T1 and T2.
Patients were eligible to participate if they had been diagnosed with OA by a physician, had typical knee pain of moderate or greater intensity, were at least 50 years of age, and were married or in a long-term relationship (self-defined) with a cohabiting spouse or partner. Patients were excluded if they reported a comorbid diagnosis of fibromyalgia or rheumatoid arthritis, used a wheelchair to ambulate, or planned to have hip or knee surgery within the next 6 months. Couples were excluded from participation if the spouse had arthritis pain of moderate or greater intensity, used a wheelchair, or required assistance with personal activities of daily living. Both partners were required to be cognitively intact, as determined through the accuracy of answers to the following questions: current date, day of the week, age, and birth date. Finally, participants were required to be free of major hearing, speech, or language problems that would interfere with the comprehension and completion of data collection procedures conducted in English.
Participants were recruited through research registries for rheumatology clinic patients and older adults interested in research participation, flyers distributed to the University of Pittsburgh staff and faculty, and by word of mouth. A total of 606 couples were screened for eligibility. Of these couples, 233 were not eligible. Frequent reasons for ineligibility were absence of OA in the knee (n = 55) or knee OA pain that was mild (n = 47). Of the remaining 373 couples, 221 declined to participate. The most common reasons were lack of interest (n = 87) or illness in the family (n = 55). The final enrolled sample consisted of 152 couples (304 individuals), which included three same-sex couples. A summary of baseline demographic characteristics for the sample is presented in Table 1.
Table 1.
Baseline Demographic Characteristics of the Sample (N = 152)
| Characteristic | M | SD | n | % |
|---|---|---|---|---|
| Spouses | ||||
| Age | 65.32 | 12.02 | ||
| Women | 62 | 41 | ||
| White | 130 | 86 | ||
| Years of education | 15.84 | 2.05 | ||
| Household income | ||||
| $19,999 or less | 15 | 10 | ||
| $20,000–39,999 | 26 | 17 | ||
| $40,000–59,999 | 32 | 21 | ||
| $60,000–79,999 | 24 | 16 | ||
| $80,000 or more | 46 | 30 | ||
| Years in relationship with patient | 34.71 | 16.89 | ||
| T1 Physical comorbiditya | 3.10 | 1.84 | ||
| T1 IADL assistance to patientb | 10.88 | 4.19 | ||
| Patients | ||||
| Age | 65.78 | 9.99 | ||
| Women | 89 | 59 | ||
| Years since OA diagnosis | 16.42 | 12.56 | ||
| T1 illness severity | 35.08 | 14.80 | ||
Note. IADL = Instrumental activities of daily living; OA = osteoarthritis; T1 = Time 1.
Assessed the presence of 24 current health problems (Martire & Scheier, 2000).
Assessed the frequency of spouse assistance in the completion of four daily activities (preparing meals, housework, laundry, and grocery shopping) over the last month, ranging from 1 (never) to 6 (several times a day).
Of the 152 couples interviewed at baseline, four dropped out of the study at T2 and five were unable to schedule the interview due to health issues or lack of time. Of the 143 couples interviewed at T2, 10 were missing data on at least one study variable. Thus, our analyses included 133 couples.
Measures
Patient illness severity
The 24-item Western Ontario Mc-Master Universities Index was used to measure patient illness severity (WOMAC; Bellamy, Buchanan, Goldsmith, Campbell, & Stitt, 1988). Patients were asked to rate their OA symptoms or related physical difficulties experienced in the past month on a scale, ranging from 0 (none) to 4 (extreme), with higher scores indicating greater illness severity. The WOMAC includes 5 questions regarding level of pain during daily activities (e.g., on stairs, rising from bed), 2 questions regarding stiffness (e.g., after sitting), and 17 questions regarding physical functioning (e.g., difficulty standing, getting in/out of car). Items were summed to create total scores, which could range from 0 to 96. Mean total scores for this measure were 35.08 at T1 (SD = 14.80, range = 3–82, α = .94) and 31.84 at T2 (SD = 15.80, range = 4–87, α = .95).
Spouse positive affect
Spouse positive affect over the past week was assessed using the four positive mood items (happy, joyful, pleased, enjoyment) from a mood rating scale (Thomas & Diener, 1990). Responses for each item range, ranging from 0 (not at all) to 6 (extremely), with higher scores indicating greater positive affect. Total scores were determined by summing the scores across items, and range from 0 to 24. Mean total scores were 16.78 at T1 (SD = 3.95, range = 4–24, α = .86) and 15.34 at T2 (SD = 4.68, range = 2–24, α = .90).
Spouse depressive symptoms
Spouse depressive symptoms were assessed using a 10-item short form of the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) that has been validated for use with older adult populations (Andresen, Malmgren, Carter, & Patrick, 1994). Items assess the degree to which participants experienced feelings and behaviors related to depression over the past week (e.g., being bothered by things that aren’t usually a bother or not being able to get “going”). Item responses range from 0 (rarely or none of the time; less than one day) to 3 (most of the time; 5–7 days). Total summed scores range from 0 to 30, with higher scores indicating greater depressive symptoms. Mean total scores were 5.97 at T1 (SD = 4.57, range = 0–19, α = .77) and 6.59 at T2 (SD = 5.39, range = 0–23, α = .82).
Spouse life satisfaction
The 5-item Satisfaction with Life Scale (SWLS; Diener, Emmons, Larsen, & Griffin, 1985) was used to assess spouse life satisfaction. Items assess the extent of agreement or disagreement with each statement regarding satisfaction with life (e.g., how ideal the respondent considers the conditions of his or her life). Responses for each item range from 1 (strongly disagree) to 7 (strongly agree) and summed scores range from 0 to 35, with higher scores indicating greater life satisfaction. Mean total scores were 26.77 at T1 (SD = 6.23, range = 5–35, α = .87) and 26.30 at T2 (SD = 6.25, range = 6–35, α = .88).
Relationship closeness
The Inclusion of Other in the Self Scale (IOS; Aron et al., 1992) was used to assess spouse perceptions of relationship closeness with the patient. Spouses were shown seven sets of circles on paper (one representing the spouse and the other representing the patient) that depict progressive degrees of overlap and were asked to choose the set of circles that best describes the degree of closeness they feel in their relationship. Response options range from 1 (least close) to 7 (most close). This scale was administered at T2 only. The mean score was 5.08 (SD = 1.48, range = 1–7).
Covariates
Our analyses examined change in each outcome from T1 to T2. Each analysis controlled for the T1 level of the outcome in order to model change while holding constant the initial level of the outcome. We also controlled for patient well-being at baseline. For example, the model predicting change in spouse positive affect from T1 to T2 controlled for spouses’ and patients’ T1 positive affect. At T1, patient and spouse reports were marginally correlated for positive affect (r = .14, p = .079) and significantly correlated for life satisfaction, r = .32, p < .001 and depressive symptoms (r = .24, p = .008). To account for the variance in spouse well-being that is explained by changes in spouses’ own physical health, change in spouse self-rated health was included as a covariate in each model. Spouse self-rated health was assessed with a measure adapted from the Medical Outcomes Study 36-item Short-Form Health Survey (MOS SF-36; Ware, Snow, Kosinski, & Gandek, 1993). Spouses were asked to rate their general physical health on a scale, ranging from 1 (excellent) to 5 (poor), with higher scores reflecting poorer health. Mean scores were 2.65 at T1 (SD = 0.93, range = 1–5) and 2.71 at T2 (SD = 0.97, range = 1–5). We calculated change scores from T1 to T2 by subtracting T1 scores from T2 scores.
Additional baseline variables were examined as potential covariates based on our expectation that they would be related to change in spouse well-being outcomes. These variables included spouse sociodemographic characteristics (e.g., age, gender, race, years of education, household income), patient illness characteristics (i.e., spouse IADL assistance [Lawton & Brody, 1969], years since physician diagnosis of OA), and relationship characteristics (i.e., years married to the patient, spouse marital satisfaction).
We conducted a partial correlation procedure in which we examined the statistical significance (p < .05) of partial correlations between each potential covariate and change in spouse well-being from T1 to T2 while controlling for the baseline level of the outcome. Covariates for the positive affect change model include spouse age (r = .28, p = .001) and T1 spouse marital satisfaction (r = .37, p < .001). None of the potential covariates were significantly correlated with change in spouse depressive symptoms. For the life satisfaction change model, covariates include spouse age (r = .29, p = .001), T1 spouse marital satisfaction (r = .23, p = .001), and marital duration (r = .19, p = .032). Spouse marital satisfaction was assessed using the 10-item Satisfaction subscale of the Dyadic Adjustment Scale (DAS; Spanier, 1976). Scores range from 0 to 50, with higher scores indicating greater satisfaction, and the mean score for this sample was 39.06 (SD = 6.42, range = 10–49, α = .87).
Statistical Analyses
Our first aim was to examine the effects of change in patient illness severity on change in spouse well-being. Second, we aimed to determine whether relationship closeness moderated the associations between change in patient illness severity and change in spouse well-being. Consistent with previous research (Beach et al., 2000), we used a change score regression approach (Kessler & Greenberg, 1981) to examine these aims. Change scores from T1 to T2 (6 months) were calculated by subtracting T1 scores from T2 scores for patient illness severity and spouse well-being. Hierarchical regression analyses were conducted for each spouse change score outcome. In the first step, T1 outcome scores for spouses were entered, along with the same outcome for the patient at T1 and other covariates. In the second step, T1 patient illness severity and T2 relationship closeness were entered. The third step added change in patient illness severity from T1 to T2 (i.e., the change score). In the fourth and final step we added the interaction term (Illness severity change × Closeness) to assess the effects of relationship closeness as a moderator. In order to facilitate interpretation of model estimates, all covariates, predictors, and the moderator were mean centered (Aiken & West, 1991). To examine the nature of significant interactions, we plotted the associations between change in illness severity and change in spouse well-being at one standard deviation above and below the mean of T2 relationship closeness to represent high and low levels of closeness, respectively (Aiken & West, 1991).
Results
Prior to testing our hypotheses, we conducted descriptive analyses to characterize change in patient illness severity and spouse well-being from T1 to T2. Increases and decreases in these measures were operationalized as change scores greater than and less than zero, respectively. As shown in Table 2, a slight majority of patients showed a decrease in illness severity over the 6-month period. The majority of spouses reported decreases in positive affect and life satisfaction, and nearly half reported increases in depressive symptoms.
Table 2.
Change in Patient Illness Severity and Spouse Well-Being Over 6 Months
| Variable | Increased n (%) |
Decreased n (%) |
No change n (%) |
|---|---|---|---|
| Patients | |||
| Illness severity | 52 (39) | 75 (56) | 6 (5) |
| Spouses | |||
| Positive affect | 37 (28) | 78 (59) | 18 (13) |
| Depressive symptoms | 63 (47) | 50 (38) | 20 (15) |
| Life satisfaction | 42 (32) | 71 (53) | 20 (15) |
Note. Values represent the number and percentage of participants who displayed increases, decreases, or no change in scores from baseline (Time 1) to 6 months (Time 2).
Associations Between Change in Patient Illness Severity and Change in Spouse Well-Being Across 6 Months
Table 3 displays results of regression analyses examining associations between change in patient illness severity and change in each spouse well-being outcome from T1 to T2. Standardized coefficients, standard errors, and accounted variance are presented for each change outcome at the last step of the analyses.
Table 3.
Associations Between Changes in Patient Illness Severity and Spouse Well-Being and the Moderating Effects of Relationship Closeness
| Predictor | T1–T2 Positive affect change
|
T1–T2 Depressive symptom change
|
T1–T2 Life satisfaction change
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| β | SE | ΔR2 | β | SE | ΔR2 | β | SE | ΔR2 | |
| Step 1 | .31*** | .10** | .26*** | ||||||
| T1: Spouse well-being | −.44*** | .08 | −.24** | .09 | −.53*** | .09 | |||
| T1: Patient well-being | .24** | .08 | .36*** | .10 | .11 | .09 | |||
| Step 2 | .01 | .03 | .01 | ||||||
| T1: Patient illness severity | −.07 | .08 | −.17† | .10 | .001 | .09 | |||
| T2: Relationship closeness | .07 | .09 | .07 | .09 | −.05 | .09 | |||
| Step 3 | .002 | .01 | .03* | ||||||
| T1–T2: Illness severity change | −.04 | .08 | .11 | .09 | −.20* | .08 | |||
| Step 4 | .02* | .03* | .004 | ||||||
| Illness severity change × Closeness | −.16* | .08 | .17* | .08 | .07 | .08 | |||
| Total R2 | .35 | .17 | .30 | ||||||
Note. T1 = Time 1; T2 = Time 2; T1–T2 = change in scores from T1 to T2. All models controlled for change in spouse self-rated health from T1–T2. The model for positive affect change also controlled for spouse age and T1 spouse marital satisfaction. The model for life satisfaction change also controlled for spouse age, T1 spouse marital satisfaction, and marital duration.
p < .10.
p < .05.
p < .01.
p < .001.
In line with our prediction, greater increases in patient illness severity were significantly associated with greater decreases in spouse life satisfaction over 6 months (β = −.20, p = .020). Contrary to our prediction, however, change in illness severity was not related to change in spouses’ positive affect (β = −.04, p = .658) or depressive symptoms (β = .11, p = .223).
Moderating Effects of Relationship Closeness
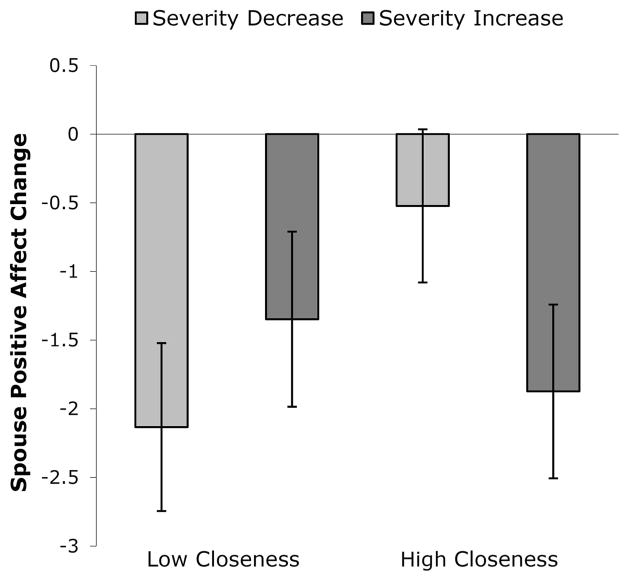
As predicted, relationship closeness significantly moderated the association between change in patient illness severity and change in spouses’ positive affect (β = −.16, p = .049). As depicted in Figure 1, when closeness was high (+1 SD), greater increases in patient illness severity were marginally associated with greater decreases in spouse positive affect (β = −.06, p = .094). In contrast, when closeness was low (−1 SD), change in illness severity was not associated with change in spouse positive affect (β = .04, p = .365).
Figure 1.
The significant moderating effect of relationship closeness on the association between change in patient illness severity and change in spouse positive affect from T1 to T2. Error bars represent the standard error for each point estimate.
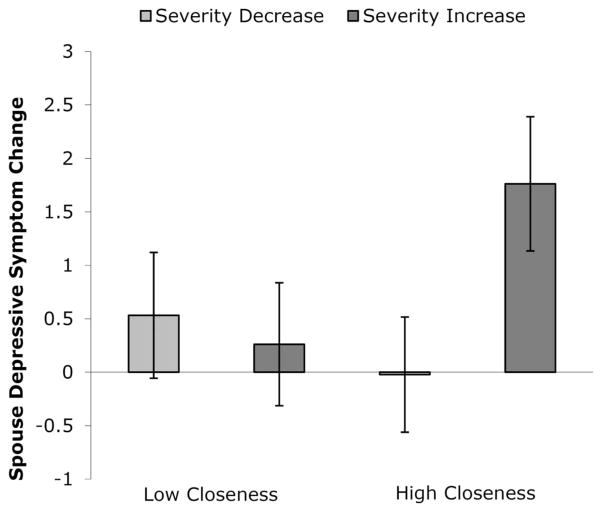
Relationship closeness also significantly moderated the association between change in patient illness severity and change in spouses’ depressive symptoms (β = .17, p = .048). As shown in Figure 2, when closeness was high (+1 SD), greater increases in patient illness severity were significantly associated with greater increases in spouse depressive symptoms (β = .08, p = .027). Conversely, when closeness was low (−1 SD), change in illness severity was unrelated to change in depressive symptoms (β = −.01, p = .738).
Figure 2.
The significant moderating effect of relationship closeness on the association between change in patient illness severity and change in spouse depressive symptoms from T1 to T2. Error bars represent the standard error for each point estimate.
Relationship closeness did not moderate the association between change in patient illness severity and change in spouse life satisfaction (β = .07, p = .410).
Discussion
Longitudinal relationships between changes in patient illness severity and spouse well-being have received little empirical attention. The current study extends prior research by demonstrating that change in OA patients’ illness severity is adversely associated with change in spouses’ life satisfaction over 6 months, as well as change in positive affect and depressive symptoms for spouses reporting an especially close relationship with the patient. Our findings support research suggesting that exposure to patients’ physical suffering is a potential pathway to explain adverse psychological outcomes in family members (Monin & Schulz, 2009) and indicate the importance of examining long-term, concurrent change in health-related measures among patients and spouses managing chronic illness. Further, this study suggests that such changes should be considered within the context of relationship characteristics that may serve to either attenuate or amplify these associations.
In partial support of our hypothesis, change in spouse life satisfaction was significantly associated with change in OA severity, with greater increases in illness severity related to greater decreases in life satisfaction across 6 months. As our life satisfaction measure assessed global perceptions of the conditions and events of one’s life, it is possible that increased illness severity in the patient may be linked to spouses’ greater feelings of dissatisfaction with their daily experiences over time. In coping with the patient’s worsening OA, these experiences may include changes such as increased activity restrictions due to the patient’s symptoms and the restructuring of routines to accommodate more frequent physician visits. Therefore, increases in patient illness severity may have a negative impact on spouses’ satisfaction with their everyday lives. Contrary to our prediction, there were no significant associations between change in patient illness severity and changes in spouses’ positive affect or depressive symptoms.
The lack of a significant relationship between changes in patient illness severity and spouse depressive symptoms is somewhat surprising, given prior research indicating that initial levels of patients’ physical symptoms (Schulz et al., 2009; Stephens et al., 2006) and change in physical functioning (Lyons et al., 2014) are associated with subsequent increases in depression among older spouses. However, moderation analyses revealed that increases in illness severity were related to increases in depressive symptoms for spouses reporting a high level of relationship closeness with the patient (but not for spouses reporting a low level of closeness). We found a similar association between greater increases in illness severity and greater decreases in positive affect among spouses reporting high relationship closeness.
In accordance with our hypothesis, these findings indicate that relationship closeness may exacerbate associations between patients’ physical suffering and spouse well-being. Our findings also extend prior research showing that spouses who feel close to their partner are more adversely impacted by their partner’s daily pain (Martire et al., 2013). It is likely that other factors affect changes in spouse well-being, such as patients’ mood, spouses’ own physical health, daily activities, and life events. In order to account for some of these other influences, our analyses controlled for baseline patient well-being and change in spouse self-rated health across the 6-month study period. Therefore, in the context of a close marital relationship, the current study suggests that the effects of patient illness severity change on spouse well-being are independent of the effects of emotional contagion from the patient and changes in spouses’ own health that may have a detrimental impact on their psychological adjustment over time.
This study has important implications for the broader literature on marriage and health. Our study extends current knowledge of the role of relationship closeness in the context of chronic illness management and how this facet of the marital relationship may impact spouses’ well-being over time. We used a measure of closeness that is believed to encompass aspects of objective partner interactions as well as subjective feelings of interconnectedness. Therefore, it likely taps into processes distinct from relationship satisfaction and other qualitative measures of marital functioning. Our findings suggest that relationship closeness represents a significant contextual factor for examination in future research on couples managing chronic health conditions. As Robles and colleagues (2014) recently noted in a review of marriage and health, a particularly important direction for future research is to determine how and for whom relationship closeness may influence health outcomes.
Our findings raise the question of whether change in patients’ physical health may only be consequential for particular subgroups of spouses. In addition to relationship closeness, it will be important for future research to examine how other relationship characteristics and spouse attributions may influence the extent to which spouses’ well-being is negatively affected by change in patient health status. For instance, spouses who believe that the patient suffers from health-related distress may experience greater decreases in well-being compared to spouses who believe that the patient is adjusting well to changes in his or her illness. Alternatively, when spouses perceive a negative change in their marital interactions as a consequence of patients’ deteriorating health, they may be more adversely affected than spouses who do not perceive such changes or those who perceive positive relationship changes (e.g., finding meaning or benefit in the illness experience). Along with identifying subgroups of spouses who may be most in need of intervention, further consideration of such factors may facilitate the development of more targeted interventions to treat and prevent declines in well-being among couples coping with chronic health conditions.
Strengths of this study include our novel research questions, a robust test of our hypotheses that controlled for baseline levels of illness severity and well-being among both spouses and patients, and the examination of concurrent change in patient health and spouse well-being across a 6-month period while controlling for the effects of change in spouses’ physical health. Importantly, we used patient reports of illness severity and spouse reports of their well-being, so our analyses avoided shared method variance that occurs when all variables are reported by the same partner. Further, our illness severity measure assessed multiple aspects of patients’ health that may affect the spouse (pain, stiffness, and physical functioning). Despite these attributes, our study has several limitations. First, relationship closeness was measured at T2 only (i.e., 6 months after baseline). Nevertheless, as couples in our sample were married for an average of 34 years, we anticipate this construct to be stable over this time period. Second, the majority of patients in our sample had been diagnosed with OA for several years, and spouses reported high overall levels of relationship closeness. As such, results may not generalize to couples in relationships that are perceived as less close or those in which patients are more recently diagnosed. Finally, the sample consisted of primarily White, middle-class couples, and so it is unknown whether the current findings would generalize to a more ethnically and socioeconomically diverse sample.
Our findings inform clinical practice with older couples managing chronic health conditions in several ways. The assessment of relationship closeness may help to identify spouses at greater risk of negative psychological effects related to partners’ suffering as well as associated physical health consequences. In our study, spouses who reported a high level of closeness with the patient had greater decreases in positive affect and greater increases in depressive symptoms over 6 months. Increased depressive symptoms in older adults are linked to greater functional disability (Nyunt et al., 2012; Zeiss et al., 1996), higher health care utilization (Feng, Yap, Kua, & Ng, 2009; Huang et al., 2000; Press, Tandeter, Romem, Hazzan, & Farkash, 2012), and an elevated risk of mortality (Bogner et al., 2012; Geerlings et al., 2002). Conversely, positive affect in later life has been linked to greater self-reported health, fewer physical symptoms, better health practices (e.g., higher sleep quality, more exercise), lower levels of stress hormones, and reduced incidence of stroke (Cohen & Pressman, 2006). Thus, adverse changes in psychological well-being may have important implications for spouses’ long-term health outcomes in addition to daily behaviors and experiences. Further, decreases in spousal well-being that are concurrent with increases in patient illness severity may in turn have detrimental effects on the quality of spousal support and patients’ psychological health (Martire, Schulz, Wrosch, & Newsom, 2003).
Chronic health problems are highly prevalent in later life. Four out of five American adults aged 50 years and older have at least one chronic condition (AARP, 2009), and over two thirds of Medicare beneficiaries report two or more chronic conditions (Centers for Medicare and Medicaid Services, 2012). The majority of older adults are married and living with their spouses (U.S. Census Bureau, 2013), and many chronic illnesses last for years and tend to become progressively more severe. Thus, it is critical to examine the impact of worsening illness severity and related effects on the health and well-being of spouses over time. The present study demonstrates that greater increases in OA severity have long-term negative effects on spouses’ psychological well-being, and that effects on positive affect and depressive symptoms are particularly strong for spouses reporting a close relationship with the patient.
Acknowledgments
This research was funded in part by Grant R01 AG026010 from the National Institute on Aging awarded to Lynn M. Martire and the Joseph and Jean Britton Graduate Fellowship awarded to Courtney A. Polenick.
Contributor Information
Courtney A. Polenick, The Pennsylvania State University
Lynn M. Martire, The Pennsylvania State University
Rachel C. Hemphill, The Pennsylvania State University
Mary Ann Parris Stephens, Kent State University.
References
- AARP. Chronic conditions among older Americans. Chronic care: A call to action for health reform. 2009 Retrieved from http://assets.aarp.org/rgcenter/health/beyond_50_hcr_conditions.pdf.
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, London: Sage; 1991. [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Aron A, Aron EN. Love and the expansion of self: Understanding attraction and satisfaction. New York: Hemisphere Publishing Corporation/Harper & Row Publishers; 1986. [Google Scholar]
- Aron A, Aron EN, Smollan D. Inclusion of other in the self scale and the structure of interpersonal closeness. Journal of Personality and Social Psychology. 1992;63:596–612. http://dx.doi.org/10.1037/0022-3514.63.4.596. [Google Scholar]
- Aron A, Aron EN, Tudor M, Nelson G. Close relationships as including other in the self. Journal of Personality and Social Psychology. 1991;60:241–253. http://dx.doi.org/10.1037/0022-3514.60.2.241. [Google Scholar]
- Beach SR, Schulz R, Yee JL, Jackson S. Negative and positive health effects of caring for a disabled spouse: Longitudinal findings from the caregiver health effects study. Psychology and Aging. 2000;15:259–271. doi: 10.1037//0882-7974.15.2.259. http://dx.doi.org/10.1037/0882-7974.15.2.259. [DOI] [PubMed] [Google Scholar]
- Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW the Validation study of WOMAC. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. The Journal of Rheumatology. 1988;15:1833–1840. [PubMed] [Google Scholar]
- Berg CA, Wiebe DJ, Butner J. Affect covariation in marital couples dealing with stressors surrounding prostate cancer. Gerontology. 2011;57:167–172. doi: 10.1159/000318642. http://dx.doi.org/10.1159/000318642. [DOI] [PubMed] [Google Scholar]
- Boerner K, Mock SE. Impact of patient suffering on caregiver well-being: The case of amyotrophic lateral sclerosis patients and their caregivers. Psychology Health and Medicine. 2012;17:457–466. doi: 10.1080/13548506.2011.613942. http://dx.doi.org/10.1080/13548506.2011.613942. [DOI] [PubMed] [Google Scholar]
- Bogner HR, Morales KH, Reynolds CF, III, Cary MS, Bruce ML. Course of depression and mortality among older primary care patients. The American Journal of Geriatric Psychiatry. 2012;20:895–903. doi: 10.1097/JGP.0b013e3182331104. http://dx.doi.org/10.1097/JGP.0b013e3182331104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Chronic conditions among Medicare beneficiaries. Baltimore, MD: U. S. Department of Health and Human Services; 2012. Retrieved from http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/Downloads/2012Chartbook.pdf. [Google Scholar]
- Cialdini RB, Brown SL, Lewis BP, Luce C, Neuberg SL. Reinterpreting the empathy-altruism relationship: When one into one equals oneness. Journal of Personality and Social Psychology. 1997;73:481–494. http://dx.doi.org/10.1037/0022-3514.73.3.481. [PubMed] [Google Scholar]
- Cohen S, Pressman SD. Positive affect and health. Current Directions in Psychological Science. 2006;15:122–125. http://dx.doi.org/10.1111/j.0963-7214.2006.00420.x. [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. http://dx.doi.org/10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Feng L, Yap KB, Kua EH, Ng TP. Depressive symptoms, physician visits and hospitalization among community-dwelling older adults. International Psychogeriatrics. 2009;21:568–575. doi: 10.1017/S1041610209008965. http://dx.doi.org/10.1017/S1041610209008965. [DOI] [PubMed] [Google Scholar]
- Flor H, Turk DC, Scholz OB. Impact of chronic pain on the spouse: Marital, emotional and physical consequences. Journal of Psychosomatic Research. 1987;31:63–71. doi: 10.1016/0022-3999(87)90099-7. http://dx.doi.org/10.1016/0022-3999(87)90099-7. [DOI] [PubMed] [Google Scholar]
- Geerlings SW, Beekman AT, Deeg DJ, Twisk JW, Van Tilburg W. Duration and severity of depression predict mortality in older adults in the community. Psychological Medicine. 2002;32:609–618. doi: 10.1017/s0033291702005585. http://dx.doi.org/10.1017/S0033291702005585. [DOI] [PubMed] [Google Scholar]
- Huang BY, Cornoni-Huntley J, Hays JC, Huntley RR, Galanos AN, Blazer DG. Impact of depressive symptoms on hospitalization risk in community-dwelling older persons. Journal of the American Geriatrics Society. 2000;48:1279–1284. doi: 10.1111/j.1532-5415.2000.tb02602.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Greenberg DF. Linear panel analysis: Models of quantitative change. New York: Academic Press; 1981. [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. http://dx.doi.org/10.1093/geront/9.3_Part_1.179. [PubMed] [Google Scholar]
- Lehan T, Arango-Lasprilla JC, Macias MÁ, Aguayo A, Villaseñor T. Distress associated with patients’ symptoms and depression in a sample of Mexican caregivers of individuals with MS. Rehabilitation Psychology. 2012;57:301–307. doi: 10.1037/a0030764. http://dx.doi.org/10.1037/a0030764. [DOI] [PubMed] [Google Scholar]
- Leonard MT, Cano A. Pain affects spouses too: Personal experience with pain and catastrophizing as correlates of spouse distress. Pain. 2006;126:139–146. doi: 10.1016/j.pain.2006.06.022. http://dx.doi.org/10.1016/j.pain.2006.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons KS, Bennett JA, Nail LM, Fromme EK, Dieckmann N, Sayer AG. The role of patient pain and physical function on depressive symptoms in couples with lung cancer: A longitudinal dyadic analysis. [Advance online publication] Journal of Family Psychology. 2014;28:692–700. doi: 10.1037/fam0000017. http://dx.doi.org/10.1037/fam0000017. [DOI] [PubMed] [Google Scholar]
- Martire LM, Keefe FJ, Schulz R, Stephens MAP, Mogle JA. The impact of daily arthritis pain on spouse sleep. Pain. 2013;154:1725–1731. doi: 10.1016/j.pain.2013.05.020. http://dx.doi.org/10.1016/j.pain.2013.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Scheier MF. Physical comorbidity index. School of Medicine, University of Pittsburgh; Pittsburgh, PA: 2000. Unpublished instrument. [Google Scholar]
- Martire LM, Schulz R. Caregiving and care receiving in later life: Health effects and promising interventions. In: Baum A, Revenson TA, Singer J, editors. Handbook of health psychology. New York: Taylor and Francis; 2012. pp. 293–307. [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine. 2010;40:325–342. doi: 10.1007/s12160-010-9216-2. http://dx.doi.org/10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Wrosch C, Newsom JT. Perceptions and implications of received spousal care: Evidence from the Caregiver Health Effects Study. Psychology and Aging. 2003;18:593–601. doi: 10.1037/0882-7974.18.3.593. http://dx.doi.org/10.1037/0882-7974.18.3.593. [DOI] [PubMed] [Google Scholar]
- Meyler D, Stimpson JP, Peek MK. Health concordance within couples: A systematic review. Social Science & Medicine. 2007;64:2297–2310. doi: 10.1016/j.socscimed.2007.02.007. http://dx.doi.org/10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Monin JK, Schulz R. Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging. 2009;24:681–695. doi: 10.1037/a0016355. http://dx.doi.org/10.1037/a0016355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyunt MS, Lim ML, Yap KB, Ng TP. Changes in depressive symptoms and functional disability among community-dwelling depressive older adults. International Psychogeriatrics. 2012;24:1633–1641. doi: 10.1017/S1041610212000890. http://dx.doi.org/10.1017/S1041610212000890. [DOI] [PubMed] [Google Scholar]
- Press Y, Tandeter H, Romem P, Hazzan R, Farkash M. Depressive symptomatology as a risk factor for increased health service utilization among elderly patients in primary care. Archives of Gerontology and Geriatrics. 2012;54:127–130. doi: 10.1016/j.archger.2011.02.009. http://dx.doi.org/10.1016/j.archger.2011.02.009. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital quality and health: A meta-analytic review. Psychological Bulletin. 2014;140:140–187. doi: 10.1037/a0031859. http://dx.doi.org/10.1037/a0031859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxbe D, Repetti RL. For better or worse? Coregulation of couples’ cortisol levels and mood states. Journal of Personality and Social Psychology. 2010;98:92–103. doi: 10.1037/a0016959. http://dx.doi.org/10.1037/a0016959. [DOI] [PubMed] [Google Scholar]
- Schulz R, Beach SR, Hebert RS, Martire LM, Monin JK, Tompkins CA, Albert SM. Spousal suffering and partner’s depression and cardiovascular disease: The Cardiovascular Health Study. The American Journal of Geriatric Psychiatry. 2009;17:246–254. doi: 10.1097/JGP.0b013e318198775b. http://dx.doi.org/10.1097/JGP.0b013e318198775b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Hebert RS, Dew MA, Brown SL, Scheier MF, Beach SR, Nichols L. Patient suffering and caregiver compassion: New opportunities for research, practice, and policy. The Gerontologist. 2007;47:4–13. doi: 10.1093/geront/47.1.4. http://dx.doi.org/10.1093/geront/47.1.4. [DOI] [PubMed] [Google Scholar]
- Siegel MJ, Bradley EH, Gallo WT, Kasl SV. The effect of spousal mental and physical health on husbands’ and wives’ depressive symptoms, among older adults: Longitudinal evidence from the Health and Retirement Survey. Journal of Aging and Health. 2004;16:398–425. doi: 10.1177/0898264304264208. http://dx.doi.org/10.1177/0898264304264208. [DOI] [PubMed] [Google Scholar]
- Slatcher RB, Robles TF, Repetti RL, Fellows MD. Momentary work worries, marital disclosure, and salivary cortisol among parents of young children. Psychosomatic Medicine. 2010;72:887–896. doi: 10.1097/PSY.0b013e3181f60fcc. http://dx.doi.org/10.1097/PSY.0b013e3181f60fcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. http://dx.doi.org/10.2307/350547. [Google Scholar]
- Stephens MAP, Martire LM, Cremeans-Smith JK, Druley JA, Wojno WC. Older women with osteoarthritis and their caregiving husbands: Effects of pain and pain expression on husbands’ well-being and support. Rehabilitation Psychology. 2006;51:3–12. http://dx.doi.org/10.1037/0090-5550.51.1.3. [Google Scholar]
- Thomas DL, Diener E. Memory accuracy in the recall of emotions. Journal of Personality and Social Psychology. 1990;59:291–297. http://dx.doi.org/10.1037/0022-3514.59.2.291. [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses and the moderating effect of marital closeness. Psychology and Aging. 1995;10:625–638. doi: 10.1037//0882-7974.10.4.625. http://dx.doi.org/10.1037/0882-7974.10.4.625. [DOI] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses: Longitudinal influences. Psychology and Aging. 1996;11:683–697. doi: 10.1037//0882-7974.11.4.683. http://dx.doi.org/10.1037/0882-7974.11.4.683. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. America’s families and living arrangements. 2013 Retrieved from http://www.census.gov/hhes/families/data/cps2013A.html.
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health survey manual and interpretation guide. Boston, MA: Nimrod Press; 1993. [Google Scholar]
- Zeiss AM, Lewinsohn PM, Rohde P, Seeley JR. Relationship of physical disease and functional impairment to depression in older people. Psychology and Aging. 1996;11:572–581. doi: 10.1037//0882-7974.11.4.572. http://dx.doi.org/10.1037/0882-7974.11.4.572. [DOI] [PubMed] [Google Scholar]