Abstract
Purpose
This study investigated the association of axial length (AL) to corneal radius of curvature (CRC) ratio with spherical equivalent (SE) in a 3-year old Asian cohort.
Methods
Three-hundred forty-nine 3-year old Asian children from The Growing Up in Singapore towards Healthy Outcomes (GUSTO) birth cohort study underwent AL and CRC measurements with a noncontact ocular biometer and cycloplegic refraction using an autorefractor. The ratio of AL to CRC (AL/CRC) was calculated for all the participants, and subsequently AL, CRC, and AL/CRC were analyzed in relationship to SE.
Results
The SE showed better correlation with AL/CRC (Spearman's correlation coefficient, ρ = −0.53; 95% confidence interval [CI]: −0.66; −0.49; P < 0.001) compared to either AL or CRC alone ([ρ = −0.36; 95% CI: −0.51 to 0.51; P = 0.01] and [ρ = 0.05; 95% CI: −0.04 to 0.17; P = 0.34], respectively). Mean AL/CRC was 2.91 ± 0.06 among myopes and decreased to 2.79 ± 0.06 among hyperopes. Axial length to corneal radius of curvature was strongly correlated with SE in myopes (ρ = −0.78; 95% CI: −3.76; −0.79; P = < 0.001), but not in emmetropes and hyperopes ([ρ = −0.39; 95% CI: −10.73; −0.57; P = 0.01] and [ρ = −0.18; 95% CI: −17.28; 12.42; P = 0.38], respectively). Linear regression adjusted for gender and ethnicity showed a 0.74-diopter shift in SE towards myopia with every 0.1 increase in AL/CRC ratio (P < 0.001, r2 = 0.33).
Conclusion
The correlation between SE and AL/CRC is stronger than that between AL or CRC alone. This suggests that in a research setting, when cycloplegic refraction is difficult to perform on 3-year-old children, AL/CRC may be the next best reference for refractive error.
Translational Relevance
In the research setting, AL/CRC may be the next best reference for refractive error over AL alone when cycloplegic refraction is unavailable in 3-year old children.
Keywords: myopia; axial length; cornea radius of curvature; AL, CRC ratio
Introduction
Myopia is the most common refractive condition in children, especially in the East Asian countries such as Singapore, China, and Hong Kong.1–3 In research studies on myopia, cycloplegic refraction is considered the gold standard in determining refractive error in children.4–7 However, based on current experiences in myopia research involving toddlers, the instillation of cycloplegic drops can be challenging, and it may not be possible to perform cycloplegic refraction in various situations due to parental objection, uncooperative infants, and in certain conditions where cycloplegia is contraindicated (e.g., Down syndrome and albinism).8–14 Although cycloplegic refraction in children cannot be replaced by any other test, it is useful to have an approximate surrogate for myopia in the absence of cycloplegic refraction to allow for the identification and subsequent classification of these study participants as myopes for the purpose of research. Considering that the refractive error of an eye is interrelated with both axial length (AL) and refractive components (such as cornea and lens) of the eye, AL to corneal radius of curvature (CRC) ratio (AL/CRC ratio) has been suggested as a proxy for refractive error in the absence of cycloplegic refraction. However, earlier studies have shown better correlation between the refractive error and AL/CRC ratio compared to AL alone15–22 in children aged 6 years to young adults aged 19 years, but not in younger children.
This study aims to investigate the correlation between AL/CRC ratio and the spherical equivalent (SE) in a 3-year-old cohort. We aim to determine if AL/CRC is a good approximation for SE in toddlers despite the lack of cycloplegic refraction.
Methods
Participants were recruited from one of Singapore's largest and most comprehensive birth cohort studies called GUSTO (Growing Up in Singapore towards Healthy Outcomes). The main aims of GUSTO are detailed elsewhere.23 Mothers have been followed throughout pregnancy, and their offspring were followed annually until the age of 3 years. Apart from various other investigations, refraction, AL, and CRC were the parameters that were assessed at the National University Hospital, Singapore, in those who visited during the period from November 2012 to July 2014. The study was conducted in accordance with the Declaration of Helsinki and was approved by the institutional review boards of National University Hospital and KK Women's and Children's Hospital. Measurements were recorded only after obtaining a written informed consent from the parents. The children involved in this study are of Chinese, Malay, or Indian ethnicity.
Of the 631 study participants who visited the clinic, the required measurements were obtained from 349 participants (55%). Measurements of either the cycloplegic refraction or the corneal radius of curvature were not obtained on 282 participants (45%) due to various reasons (mostly due to uncooperativeness of children, unavailability of technical staff, presence of ocular disease, unwillingness of parent to give consent for cycloplegic refraction). Both eyes of 349 participants were cyclopleged using one drop of 2.5% phenylephrine and three drops of 1% cyclopentolate instilled at 5-minute intervals. A minimum of 30 minutes after installation of the last cycloplegic drop, once full cycloplegia was ascertained, three consecutive measurements of ocular refraction were obtained using a table-mounted autorefractor (RK-F1; Canon, Tokyo, Japan). The autorefractor gave conventional spherocylindrical refractions that were converted to spherical equivalent refraction (SER) calculated as spherical power plus half of cylindrical power. Keratometry and AL measurements were obtained using a biometer (IOLMaster; Carl Zeiss, Jena, Germany). A trained optometrist performed the measurements, and three consecutive measurements were acquired for both AL and anterior CRC when the participant fixated on the internal light. The mean of the three measurements was used for the analysis.
Data Analysis
There was a high correlation between right and left eye refraction (Pearson correlation coefficient, r = 0.82), thus only results of the right eye are presented. Refractive error was analyzed as SE. Myopia was defined as SE of < −0.50 diopters (D) and hyperopia as SE of > +0.50 D. The AL/CRC ratio was defined as the AL divided by the mean of anterior CRC measured in two meridians, 90° and 180°. The AL, CRC, AL/CRC, and SE were analyzed as continuous variables, and the Kolmogorov-Smirnov test was used to assess the normality of these variables. The mean and SD were calculated for normally distributed data, and otherwise the median (50th percentile) and interquartile range (IR, values between the 25th and 75th percentiles of the distribution) were used. The 95% confidence intervals (CIs) for AL/CRC were also determined in the total population. To show the correlations between SE and other variables, Spearman's rank correlation was used. Separate linear regression models were constructed with SE as the dependent variable and AL/CRC, AL, and CRC as the main covariate, respectively. A two-sided P value below 0.05 was considered statistically significant, and analysis was performed using the statistical package SPSS Statistics for Windows (Version 21.0; IBM Corp., Armonk, NY, USA). To investigate the effect of gender on AL/CRC ratio, analysis was also conducted by stratifying the data based on gender.
Results
This study comprised 192 (55.0%) Chinese, 91 (26.1%) Malay, and 66 (18.9%) Indian participants and had an equal male to female ratio (176 males and 173 females). There were no differences in either gender or ethnicity between included and excluded participants. Overall, 249 (71%) participants were hyperopic, 81 (23%) were emmetropic, and 19 (6%) participants were myopic. Mean age of participants at the time of examination was 36 ± 1 months (i.e., 3 years) ranging from 34 to 40 months with mean SE + 0.88 ± 0.93 D ranging from +4.00 to −5.43 D. The AL, CRC, or the AL/CRC values were not statistically significant different across the different ethnic groups (P > 0.05).
The Kolmogorov-Smirnov test indicated that the frequency distribution was normal for AL (P > 0.10), but not for CRC or AL/CRC (P < 0.05). The mean AL was 21.73 mm (SD = 0.66, 95% CI: 21.66, 21.80 mm). The median CRC and AL/CRC were 7.72 mm (IR, 7.55–7.93, 95% CI: 7.72–7.78 mm) and 2.81 mm (IR, 2.77–2.85, 95% CI: 2.80, 2.81 mm), respectively. Figure 1 (A–C) shows the scatter plots between SE and AL/CRC, AL, and CRC, respectively. The SE showed better correlation with AL/CRC (Spearman's correlation coefficient, ρ = −0.53; 95% CI: −0.66 to −0.49; P < 0.001) compared to either AL (Spearman's correlation coefficient, ρ = −0.36; 95% CI: −0.51 to −0.32; P = 0.01) or CRC (Spearman's correlation coefficient, ρ = 0.05; 95% CI: −0.04 to 0.17; P = 0.34) alone. Using the Steiger's Z test, the correlation with SE was found significantly greater for AL/CRC than for AL (z = −13.51, P < 0.001).
Figure 1.
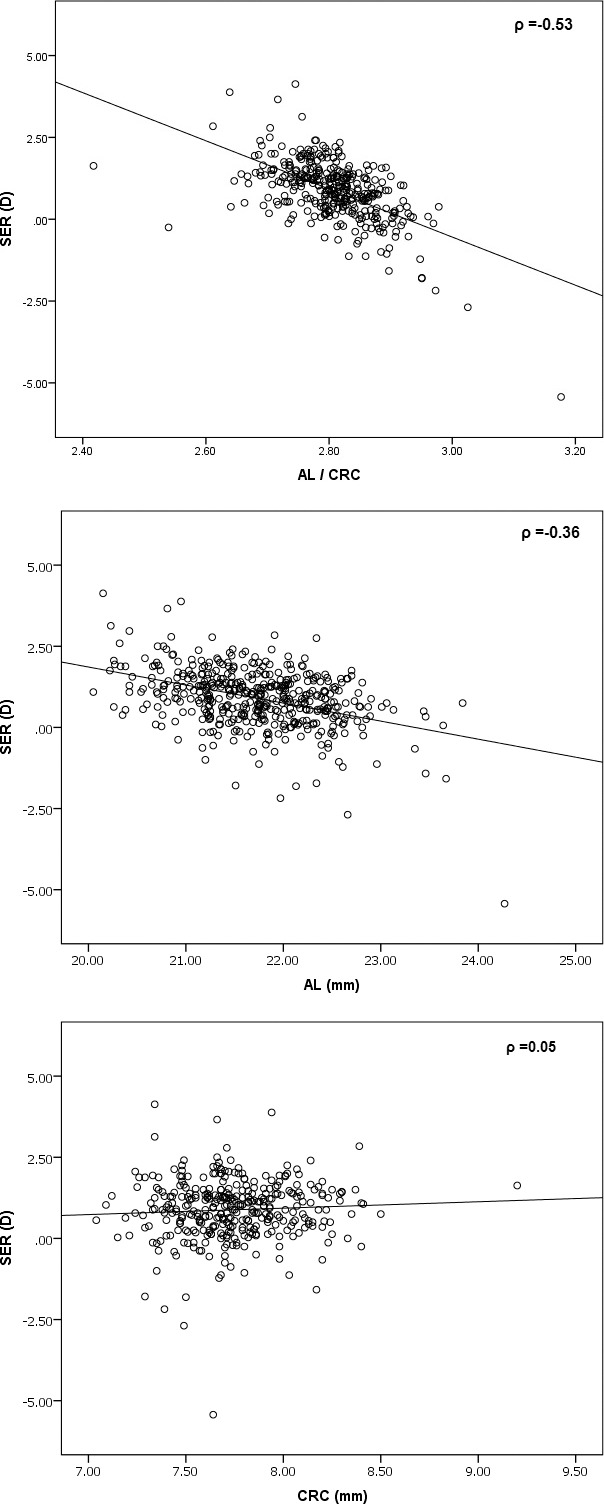
The SE of participants as a function of AL/CRC, AL, and CRC, respectively. Linear regression fit (bold line) coefficients are shown in Table 2. ρ = −0.36.
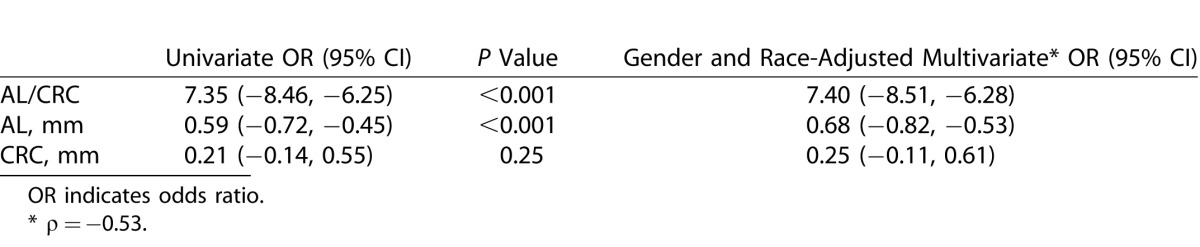
Table 1 shows the distribution of ocular biometry and AL/CRC according to the categories of refractive status of participants. Axial length was significantly longer (P < 0.001) in myopes (mean ± SD: 22.28 ± 0.66 mm) compared to emmetropes (21.90 ± 0.59 mm) and hyperopes (21.61 ± 0.59 mm). The AL/CRC ratio was also significantly higher in myopes compared to emmetropes and hyperopes (P < 0.001). Mean AL/CRC was 2.91 ± 0.06 among myopes and decreased to 2.79 ± 0.06 among hyperopes. Spearman's rank correlation coefficient between mean SE and AL/CRC was the highest in myopes (ρ = −0.78 95% CI: −3.76; −0.79; P = <0.001), followed by hyperopes (ρ = −0.39; 95% CI: −10.73; −0.57; P = 0.01) and not significant in emmetropes (ρ = −0.18; 95% CI: −17.28; 12.42; P = 0.38). There was a significant correlation between SE and AL only for hyperopes (ρ = −0.28; 95% CI: 0.43 – 11.04; P < 0.001), but not for either emmetropes or myopes. Also there was no statistical significance for the correlation between SE and CRC in all refractive groups (P > 0.05). The SE was not significantly different between males and females (+0.83 D ± 0.88 vs. +0.92 D ± 0.98, P = 0.38). Linear regression adjusted for gender and ethnicity showed a 0.74-D shift in SE toward myopia with every 0.1 increase in AL/CR ratio (P < 0.001, r2 = 0.33) (Table 2).
Table 1.
Values of Ocular Biometry and Their Respective Correlations with SER According to Refractive Status
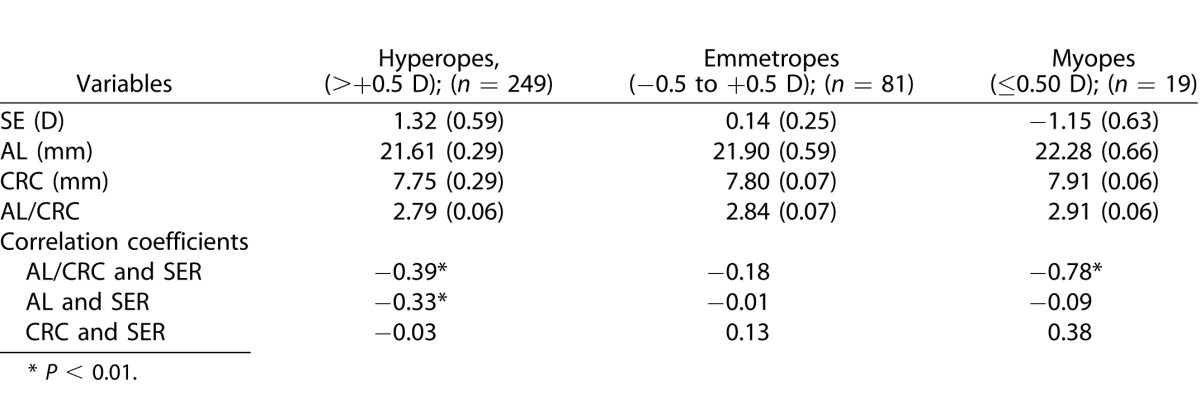
Table 2.
Association between AL/CRC, AL, and CRC with SER (D)
Discussion
In this study we found better correlation between the AL/CRC ratio with SER in 3-year-old children compared to that of SE, AL, or CRC alone. The AL/CRC ratio is correlated with cycloplegic refraction in myopes, but not in emmetropes and hyperopes. A higher AL/CRC ratio is found in myopes compared to nonmyopes. Linear regression adjusted for gender and ethnicity showed a 0.74-D shift in SE toward myopia with every 0.1 increase in AL/CRC ratio. Hence, in the setting of research, when one is unable to obtain cycloplegic refraction for the study participant, the utility of the AL/CRC in 3-year-olds might be the next best reflection of their refractive error.
The results from this study in showing significant correlation of AL/CRC ratio with SER corroborate with other studies performed in relatively older children and young adults.15–21 The AL/CRC value associated with the development of myopia, such as from the COMET study of myopic children, reported a mean AL/CRC ratio at baseline of 3.18.24 In our study of 3-year-old children, AL/CRC ratios obtained were all below 3 (2.89 for myopes, 2.79 for hyperopes, and 2.85 for emmetropes), consistent with the predominantly hyperopic refractive status in children before the age of 5 years.
Full cycloplegic refraction, which relaxes accommodation completely, remains the gold standard in the diagnosis of true refractive status; AL/CRC alone cannot replace the gold standard cycloplegic refraction. The ratio of AL to CRC alone accounts for only 33% of the variability in refraction.25 Thus, the usefulness of AL/CRC is limited to an initial screening tool and in the setting of certain research studies. In clinical practice, however, where one has access to proper refraction equipment, full-refraction examination for the child should still be carried out. We recognized a problem encountered during research studies involving cycloplegic refraction carried out in toddlers, where some toddlers had missing cycloplegic refraction due to the challenge of instilling eye drops in these children or the parental fear of eye drops. Wherever this is not possible, for example, in a rural setting or in very young children who refuse cycloplegia in a research study, the AL/CRC ratio could be used as the next best reference of refraction, as this index may be more accurate than AL.
The primary limitation of our study is the relatively small sample size of myopic participants (N = 19) compared to previous studies. Although it is reassuring that the trends/associations reported here are consistent with the previous studies involving relatively older children and young adults, the results from this study should be interpreted with caution. Another potential limitation of the study is the unavailability of other ocular biometry measurements from the study participants that change during the process of emmetropization (such as lens thickness and anterior chamber and vitreous depth), hence the correlations between AL/CRC ratio and other ocular variables were not investigated. Lastly, a major limitation of this study is the cross-sectional nature of the study, which does not delineate exact temporal relationships between myopia and the AL/CRC ratio.
In conclusion, with the ease for determining the AL and corneal curvature using noncontact partial coherence interferometry instruments, the AL/CRC ratio could possibly be used as the next best reference of refraction over AL. It is important to emphasize that the AL/CRC ratio should not be substituted for refractive error in the clinical setting.
Acknowledgments
We thank the GUSTO participants, staff, and study group for their contributions. The GUSTO study group includes Pratibha Agarwal, Arijit Biswas, Choon Looi Bong, Birit F. P. Broekman, Shirong Cai, Jerry Kok Yen Chan, Yiong Huak Chan, Cornelia Yin Ing Chee, Helen Y. H. Chen, Yin Bun Cheung, Audrey Chia, Amutha Chinnadurai, Chai Kiat Chng, Mary Foong-Fong Chong, Yap-Seng Chong, Shang Chee Chong, Mei Chien Chua, Chun Ming Ding, Eric Andrew Finkelstein, Doris Fok, Marielle Fortier, Peter D. Gluckman, Keith M. Godfrey, Anne Eng Neo Goh, Yam Thiam Daniel Goh, Joshua J. Gooley, Wee Meng Han, Mark Hanson, Christiani Jeyakumar Henry, Joanna D. Holbrook, Chin-Ying Hsu, Hazel Inskip, Jeevesh Kapur, Kenneth Kwek, Ivy Yee-Man Lau, Bee Wah Lee, Yung Seng Lee, Ngee Lek, Sok Bee Lim, Yen-Ling Low, Iliana Magiati, Lourdes Mary Daniel, Michael Meaney, Cheryl Ngo, Krishnamoorthy Naiduvaje, Wei Wei Pang, Anqi Qiu, Boon Long Quah, Victor Samuel Rajadurai, Mary Rauff, Salome A. Rebello, Jenny L. Richmond, Anne Rifkin-Graboi, Seang-Mei Saw, Lynette Pei-Chi Shek, Allan Sheppard, Borys Shuter, Leher Singh, Shu-E Soh, Walter Stunkel, Lin Lin Su, Kok Hian Tan, Oon Hoe Teoh, Mya Thway Tint, Hugo P. S. van Bever, Rob M. van Dam, Inez Bik Yun Wong, P. C. Wong, Fabian Yap, George Seow Heong Yeo.
Supported by the National Medical Research Council (NMRC) grants NMRC/TCR/004-NUS/2008, NMRC/TCR/012-NUHS/2014, and CNIG11nov012. Additional funding is provided by the Singapore Institute for Clinical Sciences – A*STAR.
Disclosure: V. Foo, None; P. Verkicharla, None; M. Ikram, None; S. Chua, None; S. Cai, None; C. Tan, None; Y.-S. Chong, None; K. Kwek, None; P. Gluckman, None; T.Y. Wong, None; C. Ngo, None; S. Mei Saw, None
References
- 1. Saw SM,, Chan B,, Seenyen L,, Yap M,, Tan D,, Chew SJ. Myopia in Singapore kindergarten children. Optometry. 2001; 72: 286 –2. [PubMed] [Google Scholar]
- 2. Seet B,, Wong TY,, Tan DT,, et al. Myopia in Singapore: taking a public health approach. Br J Ophthalmol. 2001; 85: 521 –52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pan C,, Ramamurthy D,, Saw S. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012; 32: 3–16. [DOI] [PubMed] [Google Scholar]
- 4. Wong TY,, Foster PJ,, Johnson GJ,, Seah SK. Refractive errors, axial ocular dimensions, and age-related cataracts: the Tanjong Pagar survey. Invest Opthalmol Vis Sci. 2003; 44: 1479 –14. [DOI] [PubMed] [Google Scholar]
- 5. Saw SM,, Gazzard G,, Shih-Yen EC,, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005; 25: 381 –3. [DOI] [PubMed] [Google Scholar]
- 6. Lim MC,, Gazzard G,, Sim EL,, Tong L,, Saw SM. Direct costs of myopia in Singapore. Eye. 2009; 23: 1086 –108. [DOI] [PubMed] [Google Scholar]
- 7. Ingram RM,, Barr A. Refraction of 1-year-old children after cycloplegia with 1% cyclopentolate: comparison with findings after atropinisation. Br J Ophthalmol. 1979; 63: 348 –3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stone RA,, Quinn GE,, Francis EL,, et al. Diurnal axial length fluctuations in human eyes. Invest Ophthalmol Vis Sci. 2004; 45: 63–70. [DOI] [PubMed] [Google Scholar]
- 9. Robinson BE. Factors associated with the prevalence of myopia in 6-year-olds. Optom Vis Sci. 1999; 76: 266 –2. [DOI] [PubMed] [Google Scholar]
- 10. Hashemi H,, Rezvan F,, Ostadimoghaddam H,, Abdollahi M,, Hashemi M,, Khabazkhoob M. High prevalence of refractive errors in a rural population: ‘Nooravaran Salamat' Mobile Eye Clinic experience. Clin Experiment Ophthalmol. 2013; 41: 635 –6. [DOI] [PubMed] [Google Scholar]
- 11. Guggenheim JA,, McMahon G,, Northstone K,, et al. Birth order and myopia. Ophthalmic Epidemiol. 2013;20. doi: 20:10.3109/09286586.2013.848457. [DOI] [PMC free article] [PubMed]
- 12. Guggenheim JA,, Northstone K,, McMahon G,, et al. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest Ophthalmol Vis Sci. 2012; 53: 2856 –28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Williams C,, Miller L,, Northstone K,, Sparrow JM. The use of non-cycloplegic autorefraction data in general studies of children's development. Br J Ophthalmol. 2008; 92: 723 –72. [DOI] [PubMed] [Google Scholar]
- 14. Williams C,, Northstone K,, Howard M,, Harvey I,, Harrad RA,, Sparrow JM. Prevalence and risk factors for common vision problems in children: data from the ALSPAC study. Br J Ophthalmol. 2008; 92: 959 –9. [DOI] [PubMed] [Google Scholar]
- 15. Grosvenor T. High axial length/corneal radius ratio as a risk factor in the development of myopia. Am J Optom Physiol Opt. 1988; 65: 689 –6. [DOI] [PubMed] [Google Scholar]
- 16. Grosvenor T,, Scott R. Role of the axial length/corneal radius ratio in determining the refractive state of the eye. Optom Vis Sci. 1994; 71: 573 –57. [DOI] [PubMed] [Google Scholar]
- 17. Osuobeni EP. Ocular components values and their intercorrelations in Saudi Arabians. Ophthalmic Physiol Opt. 1999; 19: 489 –4. [DOI] [PubMed] [Google Scholar]
- 18. Ojaimi E,, Rose KA,, Morgan IG,, et al. Distribution of ocular biometric parameters and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci. 2005; 46: 2748 –27. [DOI] [PubMed] [Google Scholar]
- 19. Iyamu E,, Iyamu J,, Obiakor CI. The role of axial length-corneal radius of curvature ratio in refractive state categorization in a Nigerian population. ISRN Ophthalmol. 2011; 2011. [DOI] [PMC free article] [PubMed]
- 20. Hashemi H,, Khabazkhoob M,, Miraftab M,, et al. Axial length to corneal radius of curvature ratio and refractive errors. J Ophthalmic Vis Res. 2013; 8: 220 –22. [PMC free article] [PubMed] [Google Scholar]
- 21. Guo Y,, Liu LJ,, Xu L,, et al. Myopic shift and outdoor activity among primary school children: one-year follow-up study in Beijing. PLoS One. 2013; 8: e75260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hussain RN,, Shahid F,, Woodruff G. Axial length in apparently normal pediatric eyes. Eur J Ophthalmol. 2014; 24: 120 –12. [DOI] [PubMed] [Google Scholar]
- 23. Soh SE,, Lee SSM,, Hoon SW,, et al. The methodology of the GUSTO cohort study: a novel approach in studying pediatric allergy. Asia Pac Allergy. 2012; 2: 144 –14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Saw S-M,, Chua W-H,, Hong C-Y,, et al. Height and its relationship to refraction and biometry parameters in Singapore Chinese children. Invest Ophthalmol Vis Sci. 2002; 43: 1408 –14. [PubMed] [Google Scholar]
- 25. Shufelt C,, Fraser-Bell S,, Ying-Lai M,, Torres M,, Varma R. Refractive error, ocular biometry, and lens opalescence in an adult population: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2005; 46: 4450–4460. [DOI] [PubMed] [Google Scholar]


