1. INTRODUCTION
Long-term stability of resin-dentin bonds in a hostile environment like the oral cavity is still challenging [1,2]. Constituents of the resin-dentin bond such as the hybrid layer, the dentin adhesive layer, and collagen fibrils inadvertently left unprotected within the hybridized dentin [3], are susceptible to protease-induced degradation [4-8]. Dentinal endogenous proteases, matrix metalloproteinases (MMPs) and cysteine cathepsins (cathepsin K and B) play a significant role in resin-dentin interface collagen degradation [9-11].
Different approaches to preserve hybrid layer integrity and bond strength durability have been developed [12]. Chlorhexidine (CHX) is a nonspecific MMP inhibitor [13] that also inhibits dentin cathepsin K and B [14]. The use of CHX as a primer is effective in slowing the degradation of hybrid layers produced in vitro [6,15-16] and in vivo [5,7,17-19]. Although CHX has a protective effect in hybrid layers, adhesive interfaces produced in vitro after the application of CHX are stable for up to 2 years (16,20) while the analysis of resin-dentin bonds produced in vivo indicates that the longevity of CHX effect may be reduced over time [19]. It may occur because the binding of CHX to dentin is only electrostatic [21,22] and there is no chemical interaction between CHX molecules and collagen fibrils. This electrostatic bond may be not strong enough to prevent CHX from being leached out of the interface [19], which makes it interesting to investigate other potential enzyme inhibitors that would interact with collagen in a more stable manner.
It has been recently reported that 5% dimethyl sulfoxide (DMSO) is able to inactivate human gelatinases MMP-2 and MMP-9 [23]. Additionally, when used as a dentin primer, DMSO prevented resin-dentin bond degradation after 12 months of aging [23]. DMSO [(CH3)2SO] is a colorless liquid classified as an organosulfur complex that is capable of dissolving both polar and nonpolar compounds because it is a polar aprotic solvent. It is also miscible in several organic solvents, including those used in adhesive dentistry, and in water. The polar nature of DMSO combined with its capacity to accept hydrogen bonds and its relative small and compact structure (MW=78.13 g/mol) are responsible for its unique capability to penetrate living tissues [24]. These properties also result in the ability of DMSO to associate with water, proteins, carbohydrates, nucleic acid, ionic substances, and other constituents of living systems. DMSO has the ability to compete with water molecules in the interpeptide hydrogen bonds in collagen matrix [25] resulting in the dissociation of extracellular collagen matrix [26,27].
Because the idea of using DMSO as a MMP inhibitor [23] and as a resin-dentin bond stability promoter involves its application on dentin, it is important to evaluate the possible toxic effect of this compound against the pulp tissue. Odontoblasts are the first cells to be in contact with substances diffused through the dentinal tubules; therefore, the aim of this study was to evaluate the direct cytotoxicity of DMSO against odontoblast-like cells.
2. MATERIAL AND METHODS
2.1 Culture of odontoblast-like cells MDPC-23
Immortalized odontoblast-like MDPC-23 cells were seeded at a density of 5×104 cells/cm2 into 24-well culture plates (COSTAR 3595 - Corning Incorporated, Corning, NY, USA) in 1 mL of DMEM (Dulbecco’s Modified Eagle’s Medium; Sigma Aldrich Corp., St. Louis, MO, USA) supplemented with 10% FBS (Fetal Bovine Serum; Cultilab, Campinas, SP, Brazil) containing L-glutamine (2 mmol/L), penicillin (100 IU/ml), and streptomycin (2 mmol/L) (Gibco, Grand Island, NY, USA). The cells were kept in a humidified incubator at 37°C under a 5% CO2 and 95% air atmosphere (Isotemp Fisher Scientific, Pittsburgh, PA, USA).
2.2 DMSO solutions
After incubation for 48 h, the culture medium (DMEM) of each cell was aspirated and replaced by 1 mL of a solution containing the following concentrations of DMSO (Dimehtylsulfoxide, DMSO; Mallinckrodt Baker Inc, Phillipsburg, NJ, USA): 0.05 mM (0.0004%); 0.1 mM (0.0008%); 0.3 mM (0.0024%); 0.5 mM (0.004%); or 1 mM (0.008%) mixed in plain DMEM. The control group was represented by DMSO-free DMEM. The cell were kept in contact with the solutions for 24 h and maintained in a humidified incubator at 37°C under a 5% CO2 and 95% air atmosphere during that period of time.
2.3 Cell Viability
After placing the cells in direct contact with the DMSO solutions or DMEM (control) for 24 h, the cells were incubated with 5 mg/mL MTT for 4 h. Mitochondrial dehydrogenase enzymes in living cells convert the yellow water-soluble tetrazolium salt 3-(4, 5-dimethylthia- zol-2, 5-diphenyltetrazolium bromide (MTT; Sigma Aldrich Corp., St. Louis, MO, USA) into violet formazan crystals stored in the cytoplasm of cells. Then, the culture medium with the MTT solution was aspirated and replaced by 400 μL of acidified isopropanol solution (0.04 N HCl) in each well to dissolve and extract the violet formazan crystals. After agitation and confirmation of the homogeneity of the solutions, three 100 μL aliquots of each well were transferred to a 96-well plate (Corning Incorporated, Corning, NY, USA). Cell viability was evaluated by spectrophotometry as being proportional to the absorbance measured at 570 nm wavelength using an microplate reader (Thermo Plate, Nanshan District, Shenzhen, Gandong, China). The average of the values obtained from the three aliquots was calculated as a single value for each sample for statistical analysis. For this analysis, 12 replicates were performed per group in triplicate and results were presented as percentage of the control defined as 100% of cell viability.
2.4 Viable Cell Counts
Viable cells were counted by excluding those stained with Trypan Blue dye. After 24-h contact of MDPC-23 cells with the DMSO solutions or fresh DMEM (control), trypan blue test was performed as previously described by Basso et al., (2012) [28]. In brief, the DMSO solutions and DMEM (control) in contact with the cells were aspirated and replaced by 0.12% trypsin (Invitrogen, Carlsbad, CA, USA) that was kept in contact with the cells for 10 min to detach them from the acrylic. Then 50 μL aliquots of this cell suspension were added to 50 μL of 0.04% trypan blue dye (Sigma Aldrich Corp., St. Louis, MO, USA) and left undisturbed for 2 min. Ten microliters of the solution were taken to a hemocytometer and examined with an inverted light microscope (Nikon Eclipse TS 100, Nikon Corporation, Tokyo, Japan) to determine the number of total cells and nonviable (i.e. trypan blue stained) cells. The number of viable cells was calculated by subtracting the number of nonviable cells from the number of total cells. Twelve replicates were done for each group and the analysis was done in triplicate.
2.5 Identification of cell death by necrosis (Flow cytometry)
Flow cytometry was employed to analyze necrotic cell death using propidium iodide (PI) staining. The cells were analyzed by fluorescence-activated cell sorting (FACS) in a flow cytometer (FACSCanto; BD Biosciences, San Jose, CA, USA) equipped with argon laser and Cell Quest software (BD Biosciences). MDPC-23 cells (3×104 cells/cm2) were cultured in DMEM in 24-well plates for 48 h, and then the culture medium was replaced by the DMSO solutions or fresh DMEM (control). After 24-h incubation, the cells were harvested with trypsin, centrifuged at 2,300 rcf for 2 min to remove the supernatant and resuspended in 300 μL of ligation buffer containing 10 mM HEPES pH 7.4, 150 mMNaCl, 5 mMKCl, 1mM MgCl2 and 1.8 mM CaCl2. Acquisition of cells stained positively for necrosis was made immediately after the addition of 3 μg/mL PI (Sigma-Aldrich Corp., St. Louis, MO, USA) at a concentration of 100 μg of reagent per mL of buffering solution. The samples were acquired in the FL-2 (PI) channels of the flow cytometer. Data for statistical analysis were obtained as the percentage of cells stained in relation of the total number of MDPC-23 cells identified by the flow cytometer. Eight samples per group were analyzed and the method was run in duplicate.
2.6 Cell adhesion (Crystal Violet staining)
The solutions in contact with the cells were aspirated after 24 h and the cells were fixed with 2.5% (v/v) glutaraldehyde (Sigma-Aldrich Corp., St Louis, MO, USA) for 60 min. Then, cells were dyed with 0.1% crystal violet for 15 min followed by two repeated rinsing with deionized water. Cell adherence was analyzed in a light microscope (Olympus BX51, Miami, FL, USA) connected to a computer. Images (Olympus C5060, Miami, FL, USA) were taken from four randomly selected areas of each well with 10x magnification. Images were evaluated using an imaging software (Image J 1.45S, Wayne Rasband, National Institutes of Health, USA). Data (n=12 per group) were presented as % of the control (defined as 100%) and performed in triplicate.
2.7 Quantification of Total Protein
Total protein (TP) production was evaluated as previously described by Basso et al., (2013) [29] and was performed simultaneously with the MTT assay. After 24 h incubation in contact with the cells, the solutions were aspirated and the cells were washed three times with 1 mL PBS at 37°C. One mL of 0.1% sodium lauryl sulphate in water (Sigma Aldrich Corp., St. Louis, MO, USA) was added to each well and maintained for 40 min at room temperature to produce cell lysis. The samples were homogenized and an aliquot of 1 mL of each well was transferred to Falcon tubes while the blank tube received 1 mL of deionized water. One mL of Lowry reagent solution (Sigma Aldrich Corp., St. Louis, MO, USA) was added to all samples and the tubes were agitated for 10 s in a tube shaker (Phoenix AP 56, Araraquara, SP, Brazil). After 20 min at room temperature, 500 μL of Folin-Ciocalteau’s phenol reagent solution (Sigma Aldrich Corp., St. Louis, MO, USA) were added to each sample and homogenized. After 30 min, three 100-μL aliquots of each tube were transferred to a 96-well culture plate and the absorbance of the test was measured at 655 nm wavelength with the ELISA plate reader (Thermo Plate). The average of the three values was calculated for statistical analysis. The absorbance of the control was set as 100% and the results were presented as percentage of the control. Twelve samples were performed for TP quantification and the analysis was run in triplicate.
2.8 Mineralized nodule formation (Alizarin Red)
Only for this protocol, DMSO solutions were prepared using DMEM enriched with ascorbic acid, β-glycerophosphate (Sigma- Aldrich Corp., St Louis, MO, USA) and FBS. The solutions (1 mL) were replenished every three days and the cells were maintained in a humidified incubator at 37°C under a 5% CO2 and 95% air atmosphere. Then, on the seventh day, the solutions were aspirated and the cells were fixed with 70% ethanol for 60 min. The fixed cells were stained with 1% Alizarin red (Sigma- Aldrich Corp., St Louis, MO, EUA) diluted in deionized water for 20 min under agitation. The remaining dye was carefully aspirated and the cells were washed with deionized water for three consecutive times. 10% cetylpyridinium chloride in PBS was added to the wells (500 μL) and left under agitation for 15 min. Three 100-μL aliquots from each well were transferred to wells of a 96-well culture plate and the absorbance was read in a microplate reader (Thermo Plate) at 562 nm wavelength [30]. The analysis was performed in triplicate (n=12) and the results presented as absolute values.
2.9 Statistical analyses
Data from cell number, adhesion, viability and total protein production were normally distributed and presented homoscedasticity. Therefore, data were submitted to one-way ANOVA (“concentration of DMSO”) complemented by Tukey’s test for pairwise comparisons. Data from mineralized nodules formation and cell death by necrosis did not adhere to the normal curve and were analyzed by Kruskal-Wallis and Mann-Whitney tests. Additionally, Spearman’ or Pearson’s tests were applied to correlate the concentration of DMSO with the response variables of the study. For all statistical tests a p<0.05 was taken as statistically significant.
3. RESULTS
MDPC-23 cell number, cell adhesion (Figure 1) and percentage of cell death by necrosis (Figure 2) were not affected by DMSO at any concentration, with no statistical significant difference among the groups (Figure 1). Cell viability was increased when the cells were treated with 0.1 and 0.3 mM of DMSO (Table 1) and a significant although weak correlation was seen between DMSO concentration and the viability of odontoblast-like cells (Spearman’s coefficient r=0.245, p=0.038) (Figure 3a). A slight but significant reduction in total protein production was observed when 0.3, 0.5 and 1.0 mM of DMSO solution was used in comparison to the control. That reduction varied between 15 and 21% (Table 1). A significant correlation (Spearman’s coefficient r=-0.564, p=0.001) was also seen between the concentration of DMSO and the production of total protein (Figure 3b). Finally, mineralized nodules formation was similar to control group with all DMSO concentrations, except for 1.0 mM, which significantly increased mineral nodule formation (Table 1).
Figure 1.
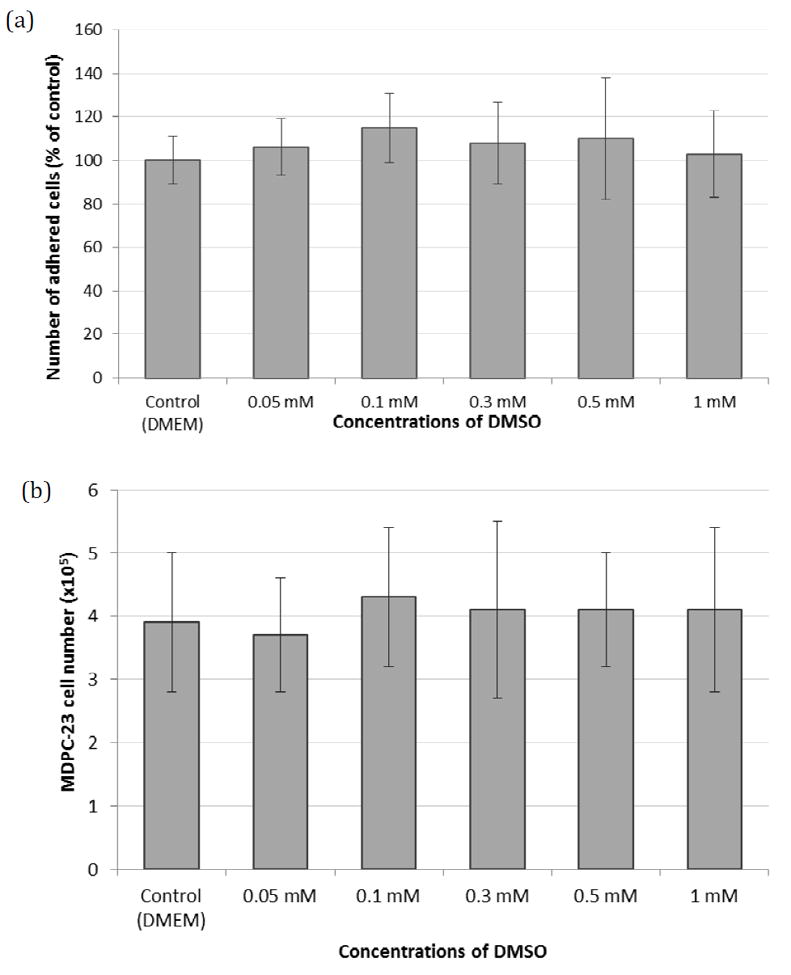
(a) Adhesion and (b) number of MDPC-23 cells kept in direct contact with different concentrations of DMSO or DMEM (control). Means and standard deviations (n=12). There was no statistically significant difference among groups (ANOVA, Cell adhesion, p=0.674 and cell number, p=0.805).
Figure 2.
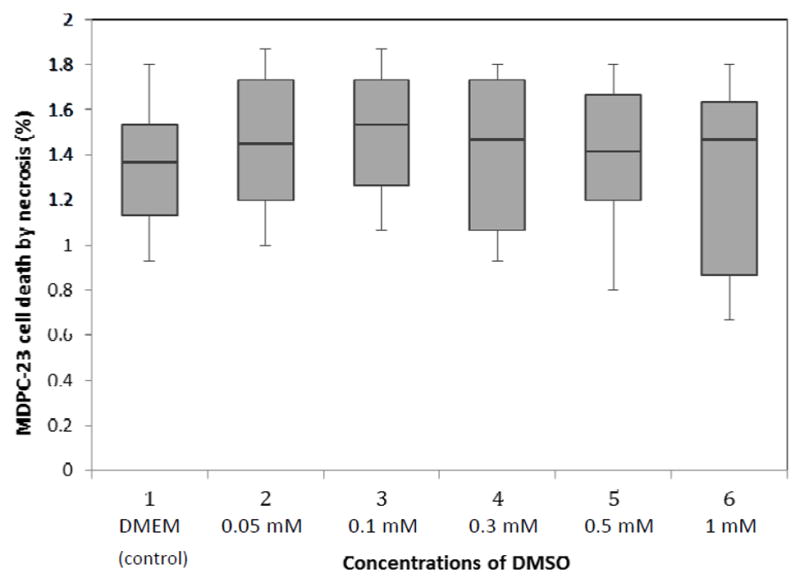
Percentage of cell death by necrosis after contact with DMSO. Results are presented as box plot graphs (n=12). The line in the middle of the box represents the median. No difference was found among groups (Kruskal-Wallis, p=0.997).
Table 1.
Effect of DMSO direct contact with odontoblast-like cells (MDPC-23) on cell viability, total protein production and mineralized nodules formation.
| DMSO concentration (mM) | Cell event/product
|
||
|---|---|---|---|
| Viability* | Total protein* | Mineralized nodules formation** | |
| 0 | 100±3 b | 100±5 ab | 100.3 (96.4-104.1) b |
| 0.05 | 103±3 ab | 113±9 a | 98.6 (94.3-100.7) b |
| 0.1 | 107±6 a | 98±1 bc | 99.7 (94.3-101.9) b |
| 0.3 | 108±7 a | 81±9 d | 99.4 (98.6-102.4) b |
| 0.5 | 105±8 ab | 85±1 cd | 102.4 (99.9-105.4) b |
| 1 | 105±4 ab | 79±9 d | 136.3 (111.9-141.9) a |
numbers are mean±standard-deviation, n=12;
numbers are median (percentile 25-percentile 75), n=12. All values represent percentage related to the control (no DMSO = 100%)
within each column, groups identified by the same letter are no statistically different (p>0.05).
Figure 3.
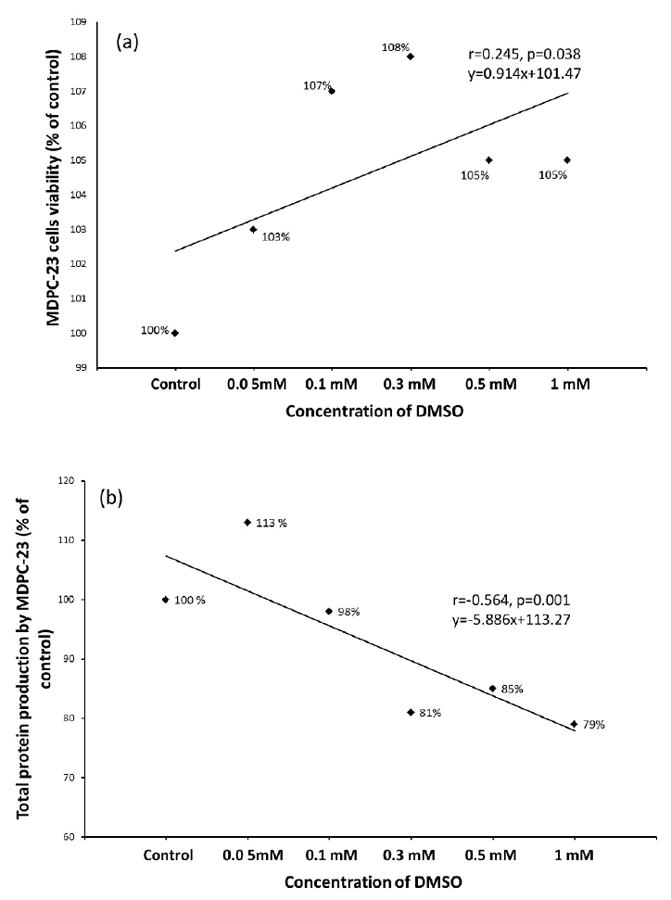
Linear relationship between concentration of DMSO (mM) and (a) percentage of MDPC-23 cells viability; or (b) total protein production by MDC-23 cells.
4. DISCUSSION
The DMSO concentrations assessed in this study were chosen based on the results obtained by Tjäderhane et al., 2013 [23], where the authors found that the use of 0.5 mM (0.004%) DMSO as a primer for 30 s prior to adhesive application rendered resin-dentin bonds resistant to degradation and preserved the bond strength for 12 months in vitro [23]. The other concentrations The authors of the only paper published using DMSO previously to bonding procedures speculated that the outcome could be attributed to three main effects of DMSO: (1) enhancement of collagen wetting by adhesives, improving collagen encasement within the polymerized matrix, (2) improvement of monomeric conversion, turning the adhesive less prone to water-mediated degradation, and (3) inactivation of MMPs, at least gelatinases MMP-2 and MMP-9 [23].
The present study demonstrated that the direct contact of 0.05 mM (0.0004 %) to 1 mM (0.008 %) DMSO did not affect the number, adherence and cell death by necrosis of odontoblast-like MDPC-23 cells. An increase in cell viability (mitochondrial metabolism) was observed with 0.3 and 0.5 mM DMSO. Previous studies have shown DMSO (0.01% and higher) to alter the attachment of human embryonic stem cells, together with a significant reduction in cell viability in a dose-dependent manner [31]. However, Adler et al., [32], using different embryonic stem cell line, demonstrated no changes in viability up to 0.5% DMSO concentration: with other cell lines, viability remained unchanged up to 1% of DMSO concentration [32]. Others have demonstrated cell type-dependent reduction [33] and induction [34-36] of apoptosis with DMSO. Together, these contradictory findings signify the importance of using dental pulp-related cells to examine the potential toxicity of DMSO when it is considered to be used in adhesive dentistry. It must also be noted that all these studies tested DMSO at much higher concentrations (ranging between 0.01% to 15%, or 1.25 mM to 1875 mM) than those used in this paper.
The amount of total protein in cultured cells was slightly, but significantly reduced by 0.3 to 1.0 mM DMSO, the highest reduction (21%) being seen with the 1.0 mM concentration. At the same time, mineralized nodules formation increased significantly with 1.0 mM DMSO compared to all the other groups. Similar results were previously observed for preosteoblastic MC3T3-E1 cells, together with a significant and dose-dependent increase in ALP activity [37]. The authors also demonstrated the DMSO-induced increase in osteoblast-specific transcription factors, Runx2 and Osx, confirming that DMSO effectively induces osteoblastic differentiation of preosteoblastic MC3T3-E1 cells to osteoblasts [37]. Our findings indicate that low-concentration DMSO may have a similar effect on odontoblast-like MDPC-23 cells. It may be speculated that when used during adhesive procedures in deep cavities, low-concentration DMSO might actually increase the rate of secondary dentin formation rather than damage the dentin-pulp complex cells. However, this assumption should be tested in in vivo conditions before final conclusions.
Since DMSO may preserve hybrid layer integrity, it could serve as an alternative to CHX. CHX has been extensively studied as a non-specific MMP inhibitor to preserve dentin bond strength [4-7,12,17-19]. The main concern about the use of CHX as an adjunctive in dentin bond is the duration of its effect on inactivation of dentin enzymes (MMPs and cathepsins) due to its weak interaction with collagen. In this study, 0.5 mM (0.004%) DMSO that has been shown to preserve the hybrid layer integrity and dentin bond strength up to 12 months [23], caused only slight (15%) reduction in the amount of total proteins, with no other measurable signs of toxicity against the same odontoblast-like MDPC-23 cells.
DMSO is commonly used as a cryprotective agent during freezing of cells for storage at a concentration of 10 vol%, although more recent literature suggests that 4-5% may be more effective [38]. DMSO has also been extensively used as a vehicle for several drugs [24,39]. However, so far the potential effects of this solvent as a coadjuvant for adhesive systems improvement have not been studied. However, DMSO has also been used as a solvent for resin monomers in toxicity studies. Geurtsen et al., (1998) [40] used DMSO as a solvent to test the cytotoxicity of 35 resin composite components. While DMSO alone did not affect cell viability in comparison to the untreated controls, the toxicity of tested components varied significantly. The authors concluded that for several highly cytotoxic components, less toxic alternatives are available [40]. The experiments also demonstrate that DMSO is compatible with large number of contemporary adhesive monomer components, and in general does not have toxic effect on the tested cell lines [40-41]. 0.1% DMSO or ethanol ease TEGDMA entrance into the cells, thus improving its cytotoxic potency, while again the solvents alone did not affect the tested cells [41]. Together these studies indicate that even if DMSO itself does not harm pulp tissue, it may have monomer- or adhesive-dependent increasing effect on cytotoxicity of resin adhesive components, which should be taken into account especially in deep cavities with close proximity to the pulp. Further in vitro cell toxicity experiments with adhesive components and in vivo tissue toxicity studies with adhesives would therefore be beneficial. Since ethanol had a comparable effect on TEGDMA toxicity [41], these experiments should also include other, currently used adhesive solvents.
Although this study suggests that the DMSO in low concentrations could be applied on dentinal surface without causing significant damage to odontoblasts layer, additional studies are necessary to elucidate the possible effects of this potential adhesive solvent together with adhesives on dental pulp and its efficacy on preserving resin-dentin bond stability in periods of time beyond 12 months [23].
5. CONCLUSION
Within the limitations of the present study, the direct contact of odontoblast-like cells with low concentrations of DMSO did not evoke any substantial cytopathic effect.
HIGHLIGHTS.
Approaches to improve the hybrid layer and bond strength have been developed.
5% DMSO is able to inactivate human gelatinases MMP-2 and MMP-9.
Evaluation the possible toxic effect of DMSO against the pulp tissue.
Low concentrations of DMSO did not evoke any substantial cytopathic effect.
Acknowledgments
The present research was financially supported by the Brazilian Research Agencies São Paulo Research Foundation (FAPESP, 2012/08866-4) and National Counsel of Technological and Scientific Development (CNPq, grants 305204/2010-6 and 301291/2010-1 to JH, PI and grant 312768/2014-7 to MRC, PI), by the National Institute of Dental and Craniofacial Research (R01 DE015306 to DHP, PI) and the Academy of Finland.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pashley DH, Tay FR, Breschi L, Tjäderhane L, Carvalho RM, Carrilho M, et al. State of the art etch-and-rinse adhesives. Dent Mater. 2011;27:1–16. doi: 10.1016/j.dental.2010.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Munck J, Mine A, Poitevin A, Van Ende A, Cardoso MV, Van Landuyt KL, et al. Meta-analytical review of parameters involved in dentin bonding. J Dent Res. 2012;91:351–7. doi: 10.1177/0022034511431251. [DOI] [PubMed] [Google Scholar]
- 3.Spencer P, Wang Y, Katz JL. Identification of collagen encapsulation at the dentin/adhesive interface. J Adhes Dent. 2004;6:91–5. [PubMed] [Google Scholar]
- 4.Pashley DH, Tay FR, Yiu C, Hashimoto M, Breschi L, Carvalho RM, et al. Collagen degradation by host-derived enzymes during aging. J Dent Res. 2004;83:216–21. doi: 10.1177/154405910408300306. [DOI] [PubMed] [Google Scholar]
- 5.Hebling J, Pashley DH, Tjäderhane L, Tay FR. Chlorhexidine arrests subclinical degradation of dentin hybrid layers in vivo. J Dent Res. 2005;84:741–6. doi: 10.1177/154405910508400811. [DOI] [PubMed] [Google Scholar]
- 6.Carrilho MRO, Carvalho RM, de Goes MF, di Hipólito V, Geraldeli S, Tay FR, Pashley DH, Tjäderhane L. Chlorhexidine preserves dentin bond in vitro. J Dent Res. 2007;86:90–4. doi: 10.1177/154405910708600115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carrilho MRO, Geraldeli S, Tay F, de Goes MF, Carvalho RM, Tjäderhane L, Reis AF, Hebling J, Mazzoni A, Breschi L, Pashley D. In vivo preservation of the hybrid layer by chlorhexidine. J Dent Res. 2007;86:529–33. doi: 10.1177/154405910708600608. [DOI] [PubMed] [Google Scholar]
- 8.Reis AF, Carrilho MR, Ghaname E, Pereira PN, Giannini M, Nikaido T, et al. Effects of water-storage on the physical and ultramorphological features of adhesives and primer/adhesive mixtures. Dent Mater. 2010;29:697–705. doi: 10.4012/dmj.2009-091. [DOI] [PubMed] [Google Scholar]
- 9.Tersariol IL, Geraldeli S, Minciotti CL, Nascimento FD, Pääkkönen V, Martins MT, Carrilho MR, Pashley DH, Tay FR, Salo T, Tjäderhane L. Cysteine cathepsins in human dentin-pulp complex. J Endod. 2010;36:475–81. doi: 10.1016/j.joen.2009.12.034. [DOI] [PubMed] [Google Scholar]
- 10.Tjäderhane L, Nascimento FD, Breschi L, Mazzoni A, Tersariol ILS, Geraldeli S, Tezvergil-Mutluay A, Carrilho MR, Carvalho RM, Tay FR, Pashley DH. Optimizing dentin bond durability: Control of collagen degradation by matrix metalloproteinases and cysteine cathepsins. Dent Mater. 2013;29:116–35. doi: 10.1016/j.dental.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vidal CM, Tjäderhane L, Scaffa PM, Tersariol IL, Pashley D, Nader HB, Nascimento FD, Carrilho MR. Abundance of MMPs and cysteine cathepsins in caries-affected dentin. J Dent Res. 2014;93:269–74. doi: 10.1177/0022034513516979. [DOI] [PubMed] [Google Scholar]
- 12.Tjäderhane L, Nascimento FD, Breschi L, Mazzoni A, Tersariol ILS, Geraldeli S, Tezvergil-Mutluay A, Carrilho MR, Carvalho RM, Tay FR, Pashley DH. Strategies to prevent hydrolytic degradation of the hybrid layer – a review. Dent Mater. 2013;29:999–1011. doi: 10.1016/j.dental.2013.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gendron R, Grenier D, Sorsa T, Mayrand D. Inhibition of the activities of matrix metalloproteinases 2, 8, and 9 by chlorhexidine. Clin Diagn Lab Immunol. 1999;6:437–9. doi: 10.1128/cdli.6.3.437-439.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scaffa PMC, Vidal CMP, Barros N, Gesteira TF, Carmona AK, Breschi L, Pashley DH, Tjäderhane L, Tersariol ILS, Nascimento FD, Carrilho MR. Chlorhexidine inhibits the activity of dental cysteine cathepsins. J Dent Res. 2012;91:420–5. doi: 10.1177/0022034511435329. [DOI] [PubMed] [Google Scholar]
- 15.Komori PC, Pashley DH, Tjäderhane L, Breschi L, Mazzoni A, de Goes MF, Wang L, Carrilho MR. Effect of 2% chlorhexidine digluconate on the bond strength to normal versus caries-affected dentin. Oper Dent. 2009;34:157–65. doi: 10.2341/08-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breschi L, Mazzoni A, Nato F, Carrilho M, Visintini E, Tjäderhane L, Ruggeri A, Jr, Tay FR, Dorigo Ede S, Pashley DH. Chlorhexidine stabilizes the adhesive interface: a 2-year in vitro study. Dent Mater. 2010;26:320–5. doi: 10.1016/j.dental.2009.11.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brackett MG, Tay FR, Brackett WW, Dip A, Dipp FA, Mai S, Pashley DH. In vivo chlorhexidine stabilization of an acetone-based dentin adhesives. Oper Dent. 2009;34:381–5. doi: 10.2341/08-103. [DOI] [PubMed] [Google Scholar]
- 18.Brackett WW, Tay FR, Brackett MG, Dib A, Sword RJ, Pashley DH. The effect of chlorhexidine on dentin hybrid layers in vivo. Oper Dent. 2007;32:107–11. doi: 10.2341/06-55. [DOI] [PubMed] [Google Scholar]
- 19.Ricci HA, Sanabe ME, de Souza Costa CA, Pashley DH, Hebling J. Chlorhexidine increases the longevity of in vivo resin-dentin bonds. Eur J Oral Sci. 2010;118:411–6. doi: 10.1111/j.1600-0722.2010.00754.x. Erratum in: Eur J Oral Sci 2010;118:535. [DOI] [PubMed] [Google Scholar]
- 20.Stanislawczuk R, Reis A, Loguercio AD. A 2-year in vitro evaluation of a chlorhexidine containing acid on the durability of resin-dentin interfaces. J Dent. 2011;39:40–47. doi: 10.1016/j.jdent.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Carrilho MR, Carvalho RM, Sousa EN, Nicolau J, Brsechi L, Mazzoni A, Tjäderhane L, Tay FR, Agee KA, Pashley DH. Substantivity of chlorhexidine to human dentin. Dent Mater. 2010;26:779–85. doi: 10.1016/j.dental.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim J, Uchiyama T, Carrilho M, Agee KA, Mazzoni A, Breschi L, Carvalho RM, Tjäderhane L, Tezvergil-Mutluay A, Tay FR, Pashley DH. Chlorhexidine binding to mineralized versus demineralized dentin. Dent Mater. 2010;26:771–8. doi: 10.1016/j.dental.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tjäderhane L, Mehtälä P, Scaffa P, Vidal C, Pääkkönen V, Breschi L, Hebling J, Tay FR, Nascimento FD, Pashley DH, Carrilho MR. The effect of dimethyl sulfoxide (DMSO) on dentin bonding. Dent Mater. 2013;29:1055–62. doi: 10.1016/j.dental.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 24.Marren K. Dimethyl sulfoxide: an effective penetration enhancer for topical administration of NSAIDs. Phys Sportsmed. 2011;39:75–82. doi: 10.3810/psm.2011.09.1923. [DOI] [PubMed] [Google Scholar]
- 25.Vishnyakov A, Lyubartsev AP, Laaksonen A. Molecular dynamics simulations of dimethyl sulfoxide and dimethyl sulfoxide-water mixture. J Phys Chemi A. 2001;105:1702–10. [Google Scholar]
- 26.Yeh AT, Nelson JS, Tromberg BJ. Reversible dissociation of collagen in tissues. Journal of Investigative Dermatology. 2003;121:1332–5. doi: 10.1046/j.1523-1747.2003.12634.x. [DOI] [PubMed] [Google Scholar]
- 27.Zimmerley M, McClure RA, Choi B, Potma EO. Following dimethyl sulfoxide skin optical clearing dynamics with quantitative nonlinear multimodal microscopy. Applied Optics. 2009;48:D79–87. doi: 10.1364/ao.48.000d79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Basso FG, Pansani TN, Turrioni AP, Bagnato VS, Hebling J, de Souza Costa CA. In vitro wound healing improvement by low-level laser therapy application in cultured gingival fibroblasts. Int J Dent. 2012:719452. doi: 10.1155/2012/719452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basso FG, Turrioni AP, Hebling J, de Souza Costa CA. Effects of zoledronic acid on odontoblast-like cells. Arch Oral Biol. 2013;58:467–73. doi: 10.1016/j.archoralbio.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 30.Yu J, He H, Tang C, Zhang G, Li Y, Wang R, Shi J, Jin Y. Differentiation potential of STRO-1+ dental pulp stem cells changes during cell passaging. BMC Cell Biology. 2010;11:32–8. doi: 10.1186/1471-2121-11-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pal R, Mamidi MK, Das AK, Bhonde R. Diverse effects of dimethyl sufoxide (DMSO) on the differentiation potential of human embryonic stem cells. Arch Toxicol. 2012;86:651–61. doi: 10.1007/s00204-011-0782-2. [DOI] [PubMed] [Google Scholar]
- 32.Adler S, Pellizzer C, Paparella M, Hartung T, Bremer S. The effects of solvents on embryonic stem cell differentiation. Toxicol in vitro. 2006;20:265–71. doi: 10.1016/j.tiv.2005.06.043. [DOI] [PubMed] [Google Scholar]
- 33.Fiore M, Degrassi F. Dimethyl sulfoxide restores contact inhibition-induced growth arrest and inhibits cell density-dependent apoptosis in hamster cells. Exp Cell Res. 1999;251:102–10. doi: 10.1006/excr.1999.4542. [DOI] [PubMed] [Google Scholar]
- 34.Marthyn P, Beuscart A, Coll J, Moreau-Gachelin F, Righi M. DMSO reduces CSF-1 receptor levels and causes apoptosis in v-myc immortalized mouse macrophages. Exp Cell Res. 1998;243:94–100. doi: 10.1006/excr.1998.4149. [DOI] [PubMed] [Google Scholar]
- 35.Trubiani O, Pieri C, Rapino M, Di Primio R. The c-myc gene regulates the polyamine pathway in DMSO-induced apoptosis. Cell Prolif. 1999;32:119–29. doi: 10.1046/j.1365-2184.1999.32230119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Galvão J, Davis B, Tilley M, Normando E, Duchen MR, Cordeiro MF. Unexpected low-dose toxicity of the universal solvent DMSO. FASEB J. 2014;28:1317–30. doi: 10.1096/fj.13-235440. [DOI] [PubMed] [Google Scholar]
- 37.Cheung WMW, Ng WW, Kung AWC. Dimethyl sufoxide as an inducer of differentiation in preosteoblast MC3T3-E1 cells. FEBS Lett. 2006;580:121–6. doi: 10.1016/j.febslet.2005.11.062. [DOI] [PubMed] [Google Scholar]
- 38.Akkök Ca, Liseth K, Herviq T, Ryningen A, Bruserud Ø, Ersvaer E. Use of different DMSO concentrations for cryopreservation of autologous peripheral blood stem cell grafts does not have any major impact on levels of leukocyte- and platelet-derived soluble mediators. Cytotherapy. 2009;11:749–60. doi: 10.3109/14653240902980443. [DOI] [PubMed] [Google Scholar]
- 39.Santos NC, Figueira-Coelho J, Martins-Silva J, Sladanha C. Multidisciplinary utilization of dimethylsulfoxide: pharmacological, cellular and molecular aspects. Biochem Pharmacol. 2003;65:1035–41. doi: 10.1016/s0006-2952(03)00002-9. [DOI] [PubMed] [Google Scholar]
- 40.Geurtsen W, Lehmann F, Spahl W, Leyhausen G. Cytotoxicity of 35 dental resin composite monomers/additives in permanent 3T3 and three human primary fibroblast cultures. J Biomed Mater Res. 1998;41:474–480. doi: 10.1002/(sici)1097-4636(19980905)41:3<474::aid-jbm18>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 41.Nocca G, DÁnto V, Rivieccio V, Schweikl H, Amato M, Rengo S, Lupi A, Spagnuolo G. Effects of ethanol and dimethyl sulfoxide on solubility and cytotoxicity of the resin monomer triethylene glycol dimethacrylate. J Biomed Mater Res Part B. 2012;100B:1500–6. doi: 10.1002/jbm.b.32718. [DOI] [PubMed] [Google Scholar]


