Abstract
Context
Mental health services are typically subject to higher cost sharing than other health services. In 2008, the US Congress enacted legislation requiring parity in insurance coverage for mental health services in group health plans and Medicare Part B.
Objective
To determine the relationship between mental health insurance parity and the use of timely follow-up care after a psychiatric hospitalization.
Design, Setting, and Population
We reviewed cost-sharing requirements for outpatient mental health and general medical services for 302 Medicare health plans from 2001 to 2006. Among 43 892 enrollees in 173 health plans who were hospitalized for a mental illness, we determined the relation between parity in cost sharing and receipt of timely outpatient mental health care after discharge using cross-sectional analyses of all Medicare plans and longitudinal analyses of 10 plans that discontinued parity compared with 10 matched control plans that maintained parity.
Main Outcome Measures
Outpatient mental health visits within 7 and 30 days following a discharge for a psychiatric hospitalization.
Results
More than three-quarters of Medicare plans, representing 79% of Medicare enrollees, required greater cost sharing for mental health care compared with primary or specialty care. The adjusted rate of follow-up within 30 days after a psychiatric hospitalization was 10.9 percentage points greater (95% confidence interval [CI], 4.6-17.3; P<.001) in plans with equivalent cost sharing for mental health and primary care compared with plans with mental health cost sharing greater than primary and specialty care cost sharing. The association of parity with follow-up care was increased for enrollees from areas of low income and less education. Rates of follow-up visits within 30 days decreased by 7.7 percentage points (95% CI, −12.9 to −2.4; P= .004) in plans that discontinued parity and increased by 7.5 percentage points (95% CI, 2.0-12.9; P=.008) among control plans that maintained parity (adjusted difference in difference, 14.2 percentage points; 95% CI, 4.5-23.9; P=.007).
Conclusion
Medicare enrollees in health plans with insurance parity for mental health and primary care have markedly higher use of clinically appropriate mental health services following a psychiatric hospitalization.
Health insurers in the United States have historically treated mental illness as distinct from all other medical illnesses by imposing higher out-of-pocket costs and instituting special restrictions for the use of mental health services.1,2 The pursuit of equivalent benefits for mental health and general medical conditions has been among the most vigorously debated health policy issues over the past several decades.3-6
Advocates for parity argue that restricted mental health coverage unfairly discriminates against individuals with mental illness. Higher cost sharing and limited benefits can expose individuals with mental illness to catastrophic levels of health care spending, thereby negating a primary purpose of health insurance.7 Differential treatment of mental health benefits reinforces a stigma that mental illness is less deserving of generous coverage than other illnesses.8 Finally, because less than half of individuals with mental illness receive care for their condition, parity in insurance coverage could improve the use of effective treatment.9
The movement to ensure insurance parity for mental health conditions gained considerable momentum in 2008. On July 15, 2008, the US Congress enacted a Medicare law that reduced coinsurance in the Medicare program for outpatient mental health services from 50% to 20%, which is equivalent to the Medicare Part B coinsurance rate for other medical and surgical services, to be phased in over 5 years starting in 2010.10 On October 3, 2008, the US Congress and President Bush approved the Emergency Economic Stabilization Act of 2008. This law, which provided authority for the federal government to purchase as much as $700 billion of distressed financial assets, also required insurance parity in cost sharing and visit restrictions for mental health and medical services among group health plans covering more than 50 employees beginning in 2010.11
Few studies have assessed the effect of parity on the access and quality of mental health care. Implementation of mental health insurance parity in the Federal Employees' Health Benefits program in 2001 did not increase mental health spending but was associated with a modest improvement in the quality of acute-phase depression care.12,13 States that enacted parity laws experienced little change in the use of mental health services or perceived access to care.14-17
In this study, we assessed insurance benefits for mental health and general medical services for all Medicare health plans from 2001 to 2006. We investigated the relation between parity in outpatient cost sharing and adherence to 2 Health Plan Employer Data and Information Set (HEDIS) quality indicators, assessing whether enrollees visited a mental health practitioner within 7 and 30 days following a hospitalization for mental illness. Timely outpatient mental health care following a psychiatric hospitalization is associated with fewer readmissions, more effective transitions to community-based services, and improved mental health outcomes.18-24 For more than 10 years, these indicators of mental health care quality have been used to assess clinical performance for all Medicare health plans as well as most commercial and Medicaid managed care plans in the United States.25
Methods
Data Sources and Study Population
We obtained Medicare HEDIS data from 2001 to 2006 containing 37 446 029 observations for individuals in Medicare managed care from the Centers for Medicare & Medicaid Services (CMS). Information about data collection, measure specifications, and CMS-sponsored audits have been published previously.26,27 Brown University's Human Research Protections Office and the CMS Privacy Board approved the study protocol and waived the need for patient consent.
We matched observations in the HEDIS data set to the Medicare enrollment file to determine enrollees' demographic characteristics. We obtained monthly information on health plan benefits from 2001 to 2006 from CMS and linked these data to the study sample. This information included each plan's required co-payment or coinsurance for a primary care, specialty care, or mental health outpatient visit. Co-payments refer to fixed out-of-pocket fees required to obtain medical services. Coinsurance is a cost-sharing arrangement requiring enrollees to pay a percentage of the total cost of the visit. To obtain information on health plan characteristics, we linked the data to the Inter-study Competitive Edge Database.28 For 27 health plans that could not be matched to this database, we ascertained these characteristics by contacting the plans directly. Zip code–level data on income and education were obtained from the 2000 US Census. We excluded 8% of observations that could not be linked to the Medicare enrollment file, health plan benefits data, or data from the Interstudy Competitive Edge Database, yielding 34 478 237 enrollees from 302 health plans. We used this sample for analyses of national trends in co-payments and enrollment in plans with and without parity in insurance coverage (Figure 1).
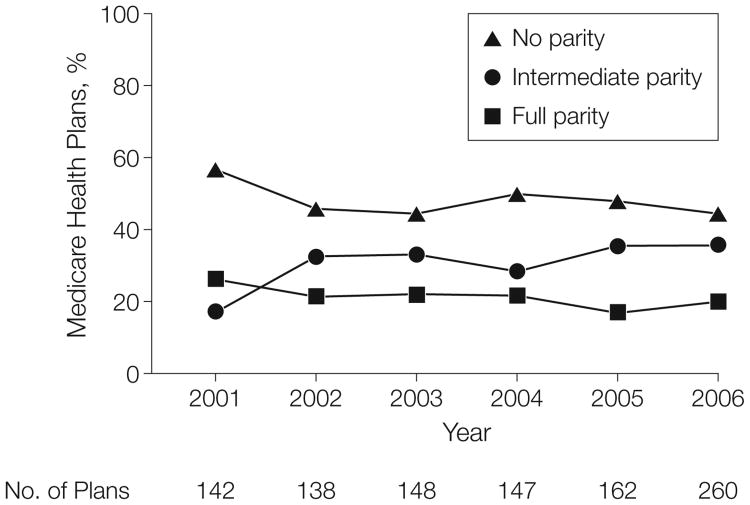
Figure 1. Parity for Outpatient Mental and Physical Health Services in Medicare Health Plans, 2001-2006.
Levels of parity are defined in the “Variables” section of the “Methods.”
For analyses of the association of parity on rates of follow-up visits after a psychiatric hospitalization, we limited the sample to observations from 2002 to 2006 that were assessed for 2 HEDIS indicators assessing follow-up care after a psychiatric hospitalization among plans with at least 2 years of participation in Medicare (n=53 647). Less than 2% of observations from staff or group model health plans had unequal cost sharing for mental health services compared with general medical services; therefore, we excluded observations from these plans (n=5569). Staff and group model plans had significantly better performance on the 2 HEDIS measures than all other plans but we were unable to assess whether this improved performance was mediated by the presence of parity or the model type of the plan. Our main analytic sample, therefore, included 48 078 observations representing 43 892 individuals in 173 health plans. The median number of observations per enrollee was 1 and the maximum was 4.
Variables
The main dependent variables were whether an enrollee who was hospitalized for a mental illness received follow-up care with a mental health practitioner within 7 or 30 days after discharge. Visits made within 7 days following discharge were included in analyses measuring visits within 30 days. Only enrollees who were continuously enrolled in the health plan from the date of discharge to 30 days after the discharge were eligible for these measures.
The primary independent variable was whether the enrollee's health plan had equivalent cost sharing for mental health, primary care, and specialist outpatient visits. We classified plans in 3 groups depending on whether the health plan's mental health cost sharing was (1) less than or equal to primary care cost sharing (full parity); (2) greater than primary care cost sharing but less than or equal to specialist cost sharing (intermediate parity); or (3) greater than both primary care and specialist cost sharing (no parity). Health plan cost sharing was defined by the plan's benefit policy in January of the measurement year. For 9% of plans with multiple insurance products with varying levels of parity, we classified parity status on the basis of the plan's median co-payment for outpatient services.
Individual-level covariates included age, sex, race, proportions of individuals aged 65 years or older in an individual's zip code with reported income less than the federal poverty level, proportions of individuals aged 65 years or older in an individual's zip code who reported attending college, and year of measurement. Race was derived from the Medicare enrollment file. Plan-level covariates included US Census region, average yearly Medicare enrollment, plan age, tax status, and the plan's co-payments for primary care and specialist visits.
Statistical Analysis
We assessed annual trends in co-payments for mental health, primary care, and specialist outpatient visits and the proportion of enrollees in each of the 3 parity categories. We measured unadjusted adherence rates to the HEDIS measures by health plan parity status as well as by the absolute level of mental health cost sharing. To determine the adjusted association of health plan parity with rates of follow-up after hospitalization, we constructed linear regression models with generalized estimating equations that adjusted for sociodemographic and health plan characteristics, measurement year, clustering of observations within plans, and repeated measurement among enrollees. We assessed whether the adjusted estimates of parity varied by income, education, and race by assessing 2-way interactions of these variables with health plan parity.
This main analytic sample contained 4348 observations in plans with full parity and 24 220 in plans with no parity. Therefore, the study had greater than 99% power to detect a 5 percentage-point difference in follow-up rates for plans with full parity compared with rates for plans with no parity, with α of .05. Using the method described by Kerry and Bland29 to account for the effect of clustering of observations, the study had 80% power to detect a 5 percentage-point difference between full-parity and no-parity plans with a design effect of as much as 5.
There were 13 health plans that discontinued full parity between December 2002 and January 2006 by increasing mental health cost sharing. We matched 10 of these plans to 10 control plans with continuous Medicare participation from 2002 to 2005 that maintained full parity. Each plan was randomly matched to 1 control plan stratifying by US Census region and tax status. We matched identical years of measurement for each case and control plan. Among plans that discontinued parity, the mean increase in mental health co-payments was $12. Three plans that discontinued full parity were excluded because we could not identify control plans with identical census region and tax status that retained full parity. They included 2 western for-profit plans and 1 midwestern for-profit plan. In these 3 excluded plans, the rate of follow-up visits 7 days after a hospitalization for mental illness was 57.9% in the year prior to discontinuing full parity and 38.8% in the year after discontinuing full parity.
We calculated the change in posthospitalization follow-up rates from the year before to the year after a plan discontinued full parity to the longitudinal change in rates of follow-up for corresponding years within control plans. We further adjusted for age, sex, race, income, education, clustering within plans, and repeated measurements of enrollees using generalized estimating equations. We determined if our results were sensitive to the inclusion of more than 1 year of data before a plan discontinued parity. We also performed an analysis of posthospitalization follow-up rates using a sample of enrollees who were continuously enrolled in their respective plans. All analyses were performed using SAS statistical software version 9.1 (Cary, North Carolina) and reported with 2-tailed P values or 95% confidence intervals (CIs).
Results
Mental Health Parity in Medicare Managed Care Plans
Medicare plans without parity outnumbered intermediate- and full-parity plans for each year of the study (Figure 1). Across all years of the study, 47% of the enrollee observations (16 224 431) were from Medicare plans with no parity, 32% were from plans with intermediate parity (11 058 364), and 21% were from plans with full parity (7 195 442).
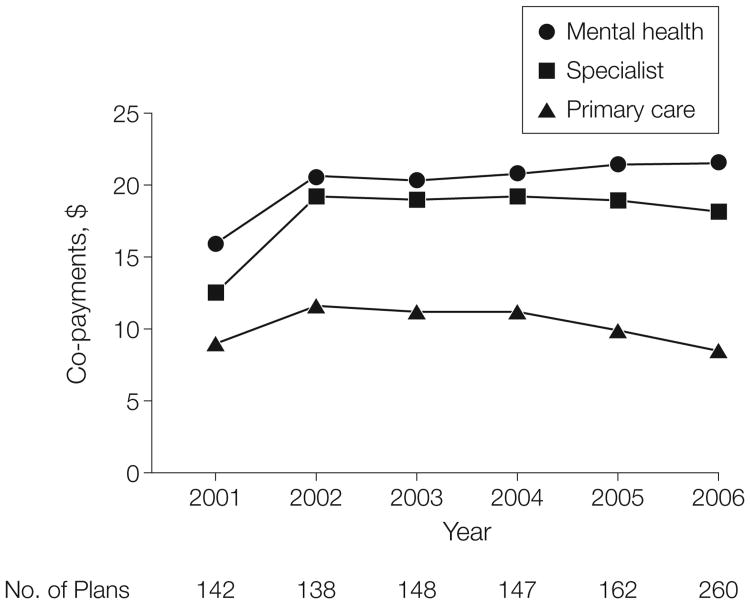
Mean co-payments for mental health outpatient services were greater than co-payments for either primary care or specialty outpatient services (Figure 2). From 2001 to 2006, the mean co-payment for a mental health outpatient visit was $20.36 (interquartile range [IQR], $12.50-$27.50), compared with $10.04 for a primary care visit (IQR, $5.00-$15.00), and $18.06 for visits to specialist physicians (IQR, $10-$25). Of the 997 plan-years in the study, 14% (139) required coinsurance for a mental health visit for at least 1 of the plan's insurance products. By contrast, the prevalence of coinsurance for a primary care or specialist visit among these plans was 2% (20). Among plans that required coinsurance, the mean coinsurance for a mental health visit was 38% (range, 10%-50%) and the mean coinsurance for both primary care and specialty visits was 19% (range, 10%-20%). Mean mental health co-payments were $9.32 (IQR, $0-$15) and $23.90 (IQR, $20-$30) in full- and no-parity plans, respectively.
Figure 2. Cost Sharing for Outpatient Mental and Physical Health Services in Medicare Health Plans, 2001-2006.
Data are shown for mental health, specialist, and primary care outpatient visits.
Insurance Parity and Rates of Follow-up Visits
Enrollees who were hospitalized for a mental illness were demographically similar regardless of the parity status of their plan (Table 1). Enrollees in full-parity plans were more likely to be in smaller plans in the West with fewer years of operation and not-for-profit tax status.
Table 1. Sociodemographic and Health Plan Characteristics of Enrollees, by Mental Health Parity Status of the Health Plana.
| Characteristic | No Parity (n = 24 220) | Intermediate Parity (n = 19510) | Full Parity (n = 4348) |
|---|---|---|---|
| Enrollees | |||
| Age, mean (SD), y | 65 (15) | 65 (15) | 67 (14) |
|
| |||
| Female, % | 60 | 59 | 61 |
|
| |||
| Race, %b | |||
| White | 81 | 85 | 86 |
|
| |||
| Black | 13 | 11 | 9 |
|
| |||
| Other | 6 | 5 | 5 |
|
| |||
| Below poverty level, %c | 11 | 10 | 10 |
|
| |||
| Attended college, %d | 33 | 32 | 35 |
|
| |||
| Plans | |||
| Region, % | |||
| Northeast | 30 | 34 | 29 |
|
| |||
| South | 31 | 37 | 18 |
|
| |||
| Midwest | 12 | 13 | 19 |
|
| |||
| West | 27 | 16 | 35 |
|
| |||
| No. of Medicare enrollees in plan, % | |||
| 0-24 999 | 15 | 18 | 30 |
|
| |||
| 25000-49 999 | 45 | 36 | 63 |
|
| |||
| ≥50000 | 40 | 47 | 7 |
|
| |||
| Age of plan, y, % | |||
| <10 | 12 | 15 | 20 |
|
| |||
| 10-24.9 | 73 | 49 | 50 |
|
| |||
| ≥25 | 14 | 36 | 29 |
|
| |||
| Tax status, % | |||
| Not-for-profit | 25 | 17 | 64 |
|
| |||
| For-profit | 75 | 83 | 36 |
Percentages may not total 100 because of rounding. Parity was defined based on whether the health plan's mental health cost sharing was: (1) less than or equal to primary care cost sharing (full parity); (2) greater than primary care cost sharing but less than or equal to specialist cost sharing (intermediate parity); or (3) greater than both primary care and specialty cost sharing (no parity).
Race was derived from the Medicare enrollment file.
This category denotes the mean percentage of individuals living in the enrollee's zip code area who were aged 65 years or older and reported income less than the federal poverty level.
This category denotes the mean percentage of individuals living in the enrollee's zip code area who were aged 65 years or older and who reported attending college.
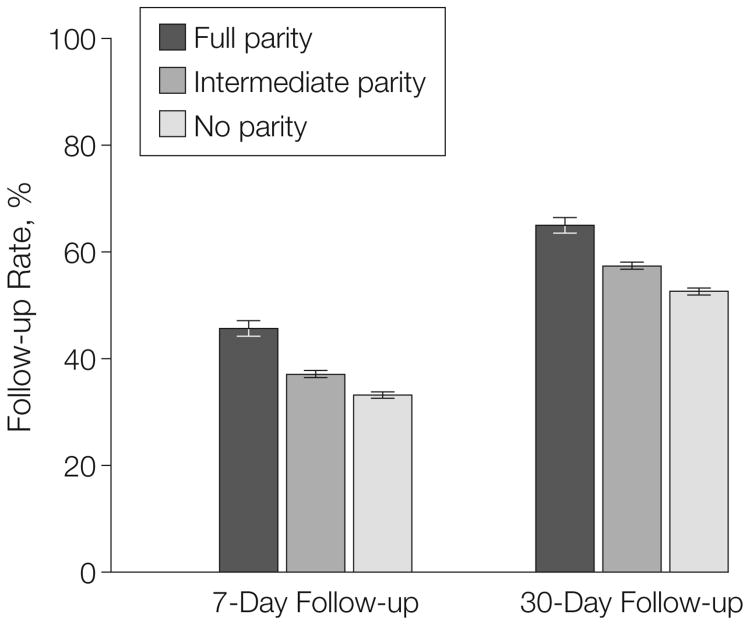
Individuals in full-parity plans were more likely to visit a mental health practitioner within 7 and 30 days after a hospitalization compared with enrollees in Medicare plans with intermediate or no parity (Figure 3). We observed a similar relationship between the absolute level of mental health cost sharing and rates of follow-up after discharge. For example, rates of 7-day follow-up in health plans with mental health co-payments of $15 or less were 37.5% (95% CI, 36.8%-38.3% [n=16 039]), compared with follow-up rates of 29.6% (95% CI, 28.5%-30.8% [n=5872]) among health plans with co-payments of more than $30.
Figure 3. Rates of 7-Day and 30-Day Follow-up After Hospitalization for a Mental Illness by Health Plan Parity Status.
Error bars indicate 95% confidence intervals. Levels of parity are defined in the “Variables” section of the “Methods.”
In analyses adjusting for individual and health plan characteristics, rates of follow-up within 7 and 30 days after a psychiatric hospitalization were greater in plans with equivalent cost sharing for mental health and primary care vs plans with mental health cost sharing greater than primary and specialty care cost sharing (Table 2). The association of parity with follow-up visit rates was greater than any of the individual or health plan–level covariates in our model.
Table 2. Adjusted Effect of Mental Health Parity Status on Follow-up Visits After Hospitalization for Mental Illness.
| Mental Health Parity Statusa | |||||
|---|---|---|---|---|---|
|
|
|||||
| Intermediate Parity (n = 19510) | Full Parity (n = 4348) | ||||
|
|
|
||||
| Measure | No Parity (n = 24220) | Rate (95% CI) | P Value | Rate (95% CI) | P Value |
| Follow-up in 7 days | Reference | 3.0 (−0.5 to 6.5) | .10 | 10.5 (3.8 to 17.1) | .002 |
|
| |||||
| Follow-up in 30 days | Reference | 4.0 (0.2 to 7.8) | .04 | 10.9 (4.6 to 17.3) | <.001 |
Abbreviation: CI, confidence interval.
Estimates reflect adjusted percentage point differences in follow-up rates compared with rates in plans with no parity (the reference group). Estimates have been adjusted for sociodemographic and health plan characteristics, year of measurement, clustering of observations within health plans, and repeated measurements of enrollees. Levels of parity are defined in the “Variables” section of the “Methods” and in the first footnote to Table 1.
The association between insurance parity and follow-up visits was magnified for individuals from areas of lower income and education. For example, individuals in the lowest quartile of area-level income had an adjusted 7-day follow-up rate that was 14.7 percentage points lower (95% CI, 7.2-22.3) in plans with no parity vs plans with full parity. For individuals in the lowest quartile of area-level education, the 30-day follow-up rate was 18.3 percentage points lower (95% CI, 10.3-26.2) in plans with no parity vs plans with full parity. The interaction of race and parity was not statistically significant.
Results of Difference-in-Differences
Analyses Rates of outpatient follow-up decreased in 10 plans that discontinued parity and increased in 10 control plans that maintained full parity (Table 3). Among 8 plans with 2 years of data before discontinuing parity, rates of follow-up in 7 days were 49.8% (95% CI, 45.7%-53.9% [n=555]) 2 years before discontinuing parity, 47.0% (95% CI, 43.0%-50.9% [n=584]) in the year prior, and 37.9% (95% CI, 34.0%-41.8% []n=561) in the year after discontinuing parity. We observed similar trends for rates of 30-day follow-up. In a sensitivity analysis restricted to individuals continuously enrolled in their Medicare plan, the rates of follow-up in 7 days decreased by 6.9 percentage points in plans that discontinued parity and increased by 1.8 percentage points in control plans that maintained parity (difference-indifference, 8.7 percentage points; 95% CI, −4.0 to 21.4).
Table 3. Change in Rates of Follow-up After a Hospitalization for Mental Illness in Medicare Plans That Discontinued Full Parity (n = 10) vs Medicare Plans That Maintained Full Parity (n = 10).
| Rate of Follow-up Visits, No. (%)a | Change | Between-Group Differenceb | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Measure | Type of plan | Year Before Change | Year After Change | Percentage Points (95% CI) | P Value | Unadjusted, Percentage Points (95% CI) | P Value | Adjusted, Percentage Points (95% CI)c | P Value |
| Follow-up in 7 d | Discontinued full parity | 650 (46.9) | 615 (35.7) | −11.2 (−16.4 to −5.8) | <.001 | 20.2 (12.1 to 28.2) | <.001 | 19.0 (6.6 to 31.3) | .003 |
|
|
|||||||||
| Maintained full parity | 544 (45.8) | 456 (54.8) | 9.0 (3.0 to 15.0) | .004 | |||||
|
| |||||||||
| Follow-up in 30 d | Discontinued full parity | 650 (64.8) | 615 (57.1) | −7.7 (−12.9 to −2.4) | .004 | 15.1 (7.4 to 22.8) | <.001 | 14.2 (4.5 to 23.9) | .007 |
|
|
|||||||||
| Maintained full parity | 544 (68.5) | 456 (76.0) | 7.5 (2.0 to 12.9) | .008 | |||||
Abbreviation: CI, confidence interval.
Refers to the denominator of total observations in each category.
Difference between plans that discontinued full parity and plans that maintained full parity.
Adjusted for sociodemographic and health plan characteristics, clustering by plan, and repeated measurements of enrollees.
Comment
We investigated the relationship between parity in cost sharing for mental health services and clinical performance on 2 widely used mental health quality indicators. Our results strongly suggest that beneficiaries enrolled in Medicare plans in which mental health cost sharing is greater than cost sharing for other health services are less likely to receive outpatient follow-up care within 7 and 30 days after hospitalization for a mental illness. The association of parity with receipt of appropriate follow-up care was consistent in both cross-sectional analyses of all Medicare plans and longitudinal analyses of 10 plans that dropped parity compared with control plans that maintained parity.
We previously reported an 8 percentage point–lower rate of biennial breast cancer screening in health plans with mammography co-payments averaging $20 compared with screening rates in health plans with first-dollar coverage.30 In this study of mental health insurance parity, co-payments that were $14 greater in plans without parity compared with full-parity plans were associated with an 11 percentage point–lower rate of follow-up after a psychiatric hospitalization. The association of parity with follow-up visit rates was increased by a factor of 1.4 for enrollees in the lowest quartiles of zip code–level income and 1.7 for enrollees in the lowest quartile of zip code–level education. Our study is therefore broadly consistent with results from the Rand Health Insurance Experiment, which found that mental health services are more sensitive to cost sharing than other medical services and that the effect of cost sharing is increased in vulnerable subgroups.31-33
Our findings differed from the more modest effects observed in other studies of parity and the quality of mental health care. Two studies of the Federal Employees' Health Benefits program found that implementation of behavioral health parity resulted in a slight increase in the number of mental health visits and use of medication therapy following a diagnosis of major depression.12,13 However, a large proportion of depression care occurs in primary care settings.34,35 Reductions in cost sharing for mental health visits may not affect visit frequency or antidepressant prescriptions for individuals who receive depression care exclusively from generalists.
Studies of the effect of state parity laws find little effect on the use of mental health services among individuals with mental illness.15,16 However, state parity laws do not apply to the majority of US residents who receive coverage through self-insured plans or the federal Medicare program.36 Moreover, such laws are heterogeneous. For example, some state parity laws apply to only 1 specific mental illness or may not address cost sharing for outpatient services.14,37 In contrast to these studies, our analysis assessed health plan benefit policies to determine parity in insurance coverage and quality indicators that specifically measured whether critical postacute visits to mental health practitioner occurred.
The overall rate of follow-up after a psychiatric hospitalization was disturbingly low, even for plans with full parity, suggesting that parity alone is insufficient to raise the quality of mental health care to acceptable levels.6 For example, a referral to a mental health practitioner and the availability of mental health appointments strongly predict receipt of appropriate aftercare services.21 Both of these factors are largely unrelated to insurance parity.
Performance on the measures in this study was substantially lower than performance on HEDIS process of care indicators assessing diabetes, cardiovascular, and cancer screening care.26 Furthermore, many aspects of mental health care remain unmeasured. For example, of the 179 quality indicators included in the National Healthcare Quality Report, only 4 are related to mental illness.38,39 In order to improve the quality of mental health, further valid quality indicators are urgently needed.
Because in indemnity insurance the demand for mental health care is particularly sensitive to cost sharing, insurers have had concerns that generous coverage may induce patients to overuse mental health services of questionable benefit. However, recent studies in managed care settings have observed little impact of expanded benefits on mental health services use or spending.12,40 Our study further suggests that patients with severe mental illness are likely to forgo valuable services in response to even modest co-payments. Reductions in cost sharing for outpatient mental health services could improve the use of clinically appropriate follow-up care after a psychiatric hospitalization, thereby averting costly rehospitalizations among high-risk patients.19,20
The US Congress enacted legislation to equalize cost sharing for mental and physical health services in group health plans and the Medicare Part B program.11,12 Our findings suggest 3 important policy questions regarding such parity. First, does equal cost sharing refer to equivalent co-payments or coinsurance? Because mental health services are frequently reimbursed at a lower level than other physician services or are delivered in less expensive formats such as with social workers or group visits, equivalent co-payments for mental and other medical services may still represent higher coinsurance for mental health services.41,42
Second, does equivalence in cost sharing refer to equal cost sharing for mental health compared with primary care or specialty care? In contrast to physician specialty care that requires a single consultation or infrequent repeat visits, individuals with severe mental illness generally require more intensive and frequent visits.43 Therefore, mental health co-payments could quickly become prohibitive, even if they were equivalent to co-payments for other specialist care. Our study suggests that equivalent cost sharing for mental health and primary care would likely have a greater effect on use of appropriate mental health care.
Third, should insurance parity be extended to other populations? Parity legislation enacted in 2008 did not require insurance parity in group health plans with 50 or fewer employees, individual insurance policies, Medicare Part A (which retains a lifetime limit of 190 covered inpatient days in psychiatric hospitals), or the Medicare managed care program (the focus of this study). Our study suggests that policy makers consider additional efforts to extend mental health parity to these groups.
Our study has several important limitations. We cannot exclude the possibility that the higher performance rates in full-parity plans could be explained by such plans enrolling individuals with a higher tendency to use outpatient mental health services. However, this selection effect is unlikely to explain our findings for 3 reasons. First, the sample was restricted to individuals with prior use of inpatient mental health care. Second, we observed few differences in the demographic characteristics of age, sex, race, and area-level income and education. Third, plans that discontinued full parity experienced a decline in follow-up rates compared with plans that maintained full parity, and this trend was observed in analyses restricted to individuals who were continuously enrolled in their plan.
Our data did not include information on other mechanisms that plans may use to reduce use of mental health services. For example, plans with limited numbers of contracted mental health practitioners or more stringent prior authorization policies may reduce use of outpatient mental health care irrespective of the plan's parity status.44,45 We were unable to determine whether the higher proportion of follow-up visits in full-parity plans was associated with lower rates of rehospitalization. We lacked information on beneficiaries' psychiatric diagnoses and were therefore unable to determine whether the effect of insurance parity differed by the type of mental illness. We were unable to determine which enrollees in our sample may have been eligible for Medicaid coverage of their co-payments. Finally, our study was limited to Medicare managed care plans and may not be generalizable to other settings.
Most Medicare health plans, like most commercial health plans, have unequal coverage for mental health services compared with other medical services. Enrollees in plans without parity in cost sharing are less likely to receive timely outpatient care following a hospitalization for mental illness. While prior studies have shown that adoption of mental health parity does not increase mental health spending, parity legislation that equalizes cost sharing for mental health and primary care may increase the use of clinically appropriate mental health services.
Acknowledgments
Funding/Support: This study was supported by a Health Policy Scholars Award to Dr Trivedi from the Pfizer Foundation. Dr Swaminathan was supported by a postdoctoral training grant (T32 HS000011) from the Agency for Healthcare Research and Quality, of which Dr Mor is principal investigator.
Role of the Sponsor: The funder played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Additional Contributions: We are grateful to John Ayanian, MD, MPP (Brigham and Women's Hospital and Harvard Medical School, Boston, Massachusetts), for thoughtful comments on a previous version of this article. We also thank Kim Elmo, BA, Judy Giles, and Michael McCann, BS, of the Centers for Medicare & Medicaid Services for assistance with data acquisition; and the Research Data Assistance Center of the University of Minnesota for advice in obtaining Medicare data. Those acknowledged did not receive compensation for their contributions.
Footnotes
Author Contributions: Dr Trivedi had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Trivedi, Mor.
Acquisition of data: Trivedi.
Analysis and interpretation of data: Trivedi, Swaminathan, Mor.
Drafting of the manuscript: Trivedi.
Critical revision of the manuscript for important intellectual content: Swaminathan, Mor.
Statistical analysis: Trivedi, Swaminathan, Mor.
Obtained funding: Trivedi.
Study supervision: Trivedi, Mor.
Financial Disclosures: None reported.
Contributor Information
Amal N. Trivedi, Department of Community Health, Warren Alpert Medical School at Brown University, Providence, Rhode Island; Research Enhancement Award Program, Providence VA Medical Center, Providence, Rhode Island.
Shailender Swaminathan, Department of Community Health, Warren Alpert Medical School at Brown University, Providence, Rhode Island.
Vincent Mor, Department of Community Health, Warren Alpert Medical School at Brown University, Providence, Rhode Island.
References
- 1.Hodgkin D, Horgan CM, Garnick DW, Merrick EL. Cost sharing for substance abuse and mental health services in managed care plans. Med Care Res Rev. 2003;60(1):101–116. doi: 10.1177/1077558702250248. [DOI] [PubMed] [Google Scholar]
- 2.Barry CL, Gabel JR, Frank RG, Hawkins S, Whitmore HH, Pickreign JD. Design of mental health benefits: still unequal after all these years. Health Aff (Millwood) 2003;22(5):127–137. doi: 10.1377/hlthaff.22.5.127. [DOI] [PubMed] [Google Scholar]
- 3.Glied SA, Frank RG. Shuffling toward parity—bringing mental health care under the umbrella. N Engl J Med. 2008;359(2):113–115. doi: 10.1056/NEJMp0804447. [DOI] [PubMed] [Google Scholar]
- 4.Frank RG, Glied SA. Better But Not Well: Mental Health Policy in the United States Since 1950. Baltimore, MD: Johns Hopkins University Press; 2006. [Google Scholar]
- 5.Mechanic D. Policy challenges in improving mental health services: some lessons from the past. Psychiatr Serv. 2003;54(9):1227–1232. doi: 10.1176/appi.ps.54.9.1227. [DOI] [PubMed] [Google Scholar]
- 6.Frank RG, Goldman HH, McGuire TG. Will parity in coverage result in better mental health care? N Engl J Med. 2001;345(23):1701–1704. doi: 10.1056/NEJM200112063452311. [DOI] [PubMed] [Google Scholar]
- 7.Zuvekas SH, Banthin JS, Selden TM. Mental health parity: what are the gaps in coverage? J Ment Health Policy Econ. 1998;1(3):135–146. doi: 10.1002/(sici)1099-176x(1998100)1:3<135::aid-mhp17>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 8.Frank RG, McGuire TG. Economics and Mental Health. Cambridge, MA: National Bureau of Economic Research; 1999. Working paper 7052. [Google Scholar]
- 9.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Govtrak Text of H.R. 6331: Medicare Improvements for Patients and Providers Act of 2008. [Accessed November 6, 2008]; http://www.govtrack.us/congress/billtext.xpd?bill=h110-6331.
- 11.Govtrak. Text of H.R. 1424: Emergency Economic Stabilization Act of 2008. [Accessed November 6, 2008]; http://www.govtrack.us/congress/billtext.xpd?bill=h110-1424.
- 12.Goldman HH, Frank RG, Burnam MA, et al. Behavioral health insurance parity for federal employees. N Engl J Med. 2006;354(13):1378–1386. doi: 10.1056/NEJMsa053737. [DOI] [PubMed] [Google Scholar]
- 13.Busch AB, Huskamp HA, Normand ST, Young AS, Goldman H, Frank RG. The impact of parity on major depression treatment quality in the Federal Employees' Health Benefits Program after parity implementation. Med Care. 2006;44(6):506–512. doi: 10.1097/01.mlr.0000215890.30756.b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pacula RL, Sturm R. Mental health parity legislation: much ado about nothing? Health Serv Res. 2000;35(1 pt 2):263–275. [PMC free article] [PubMed] [Google Scholar]
- 15.Sturm R. State parity legislation and changes in health insurance and perceived access to care among individuals with mental illness: 1996-1998. J Ment Health Policy Econ. 2000;3(4):209–213. doi: 10.1002/mhp.97. [DOI] [PubMed] [Google Scholar]
- 16.Bao Y, Sturm R. The effects of state mental health parity legislation on perceived quality of insurance coverage, perceived access to care, and use of mental health specialty care. Health Serv Res. 2004;39(5):1361–1377. doi: 10.1111/j.1475-6773.2004.00294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris KM, Carpenter C, Bao Y. The effects of state parity laws on the use of mental health care. Med Care. 2006;44(6):499–505. doi: 10.1097/01.mlr.0000215813.16211.00. [DOI] [PubMed] [Google Scholar]
- 18.Dorwart RA, Hoover CW. A national study of transitional hospital services in mental health. Am J Public Health. 1994;84(8):1229–1234. doi: 10.2105/ajph.84.8.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Solomon P, Gordon B, Davis JM. Reconceptualizing assumptions about community mental health. Hosp Community Psychiatry. 1986;37(7):708–712. doi: 10.1176/ps.37.7.708. [DOI] [PubMed] [Google Scholar]
- 20.Rosenfield S, Canton C, Nachumi G, Robbins E. Closing the gaps: the effectiveness of linking programs connecting chronic mental patients from the hospital to the community. J Appl Behav Sci. 1986;22(4):411–423. doi: 10.1177/002188638602200405. [DOI] [PubMed] [Google Scholar]
- 21.Klinkenberg WD, Calsyn RJ. Predictors of receipt of aftercare and recidivism among persons with severe mental illness: a review. Psychiatr Serv. 1996;47(5):487–496. doi: 10.1176/ps.47.5.487. [DOI] [PubMed] [Google Scholar]
- 22.Schoenbaum SC, Cookson D, Stelovich S. Post-discharge follow-up of psychiatric inpatients and re-admission in an HMO setting. Psychiatr Serv. 1995;46(9):943–945. doi: 10.1176/ps.46.9.943. [DOI] [PubMed] [Google Scholar]
- 23.Winston A, Pardes H, Papernik DS, Breslin L. Aftercare of psychiatric patients and its relation to re-hospitalization. Hosp Community Psychiatry. 1977;28(2):118–121. doi: 10.1176/ps.28.2.118. [DOI] [PubMed] [Google Scholar]
- 24.Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51(7):885–889. doi: 10.1176/appi.ps.51.7.885. [DOI] [PubMed] [Google Scholar]
- 25.Druss BG, Miller CL, Rosenheck RA, Shih SC, Bost JE. Mental health care quality under managed care in the United States: a view from the Health Plan Employer Data and Information Set (HEDIS) Am J Psychiatry. 2002;159(5):860–862. doi: 10.1176/appi.ajp.159.5.860. [DOI] [PubMed] [Google Scholar]
- 26.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005;353(7):692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- 27.Health Care Financing Administration. Medicare HEDIS 3.0/1998 Data Audit Report. [Accessed July 18, 2008];Quality of Care National Projects. http://permanent.access.gpo.gov/websites/www.hcfa.gov/quality/3i2.htm.
- 28.The InterStudy Competitive Edge 12.1. St Paul, MN: InterStudy Publications; 2001. [Google Scholar]
- 29.Kerry SM, Bland JM. Sample size in cluster randomisation. BMJ. 1998;316(7130):549. doi: 10.1136/bmj.316.7130.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N Engl J Med. 2008;358(4):375–383. doi: 10.1056/NEJMsa070929. [DOI] [PubMed] [Google Scholar]
- 31.Keeler EB, Manning WG, Wells KB. The demand for episodes of mental health services. J Health Econ. 1988;7(4):369–392. doi: 10.1016/0167-6296(88)90021-5. [DOI] [PubMed] [Google Scholar]
- 32.Lurie N, Kamberg CJ, Brook RH, Keeler EB, New-house JP. How free care improved vision in the health insurance experiment. Am J Public Health. 1989;79(5):640–642. doi: 10.2105/ajph.79.5.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keeler EB, Brook RH, Goldberg GA, Kamberg CJ, Newhouse JP. How free care reduced hypertension in the health insurance experiment. JAMA. 1985;254(14):1926–1931. [PubMed] [Google Scholar]
- 34.Harman JS, Crystal S, Walkup J, Olfson M. Trends in elderly patients' office visits for the treatment of depression according to physician specialty: 1985–1999. J Behav Health Serv Res. 2003;30(3):332–341. doi: 10.1007/BF02287321. [DOI] [PubMed] [Google Scholar]
- 35.Pincus HA, Tanielian TL, Marcus SC, et al. Prescribing trends in psychotropic medications: primary care, psychiatry, and other medical specialties. JAMA. 1998;279(7):526–531. doi: 10.1001/jama.279.7.526. [DOI] [PubMed] [Google Scholar]
- 36.Buchmueller TC, Cooper PF, Jacobson M, Zuvekas SH. Parity for whom? exemptions and the extent of state mental health parity legislation. Health Aff (Millwood) 2007;26(4):w483–w487. doi: 10.1377/hlthaff.26.4.w483. [DOI] [PubMed] [Google Scholar]
- 37.Sturm R, Pacula RL. State mental health parity laws: cause or consequence of differences in use? Health Aff (Millwood) 1999;18(5):182–192. doi: 10.1377/hlthaff.18.5.182. [DOI] [PubMed] [Google Scholar]
- 38.Agency for Healthcare Research and Quality. 2004 National Healthcare Quality Report. Rockville, MD: Agency for Healthcare Research and Quality; 2004. [Google Scholar]
- 39.Patel KK, Butler B, Wells KB. What is necessary to transform the quality of mental health care? Health Aff. 2006;25(3):681–693. doi: 10.1377/hlthaff.25.3.681. [DOI] [PubMed] [Google Scholar]
- 40.Sturm R. How expensive is unlimited mental health care coverage under managed care? JAMA. 1997;278(18):1533–1537. [PubMed] [Google Scholar]
- 41.Wells KB, Manning WG. Preliminary results of a controlled trial of the effect of a prepaid group practice on the outpatient use of mental health services. J Hum Resour. 1986;21(3):293–320. [Google Scholar]
- 42.Mechanic D, Schlesinger M, McAlpine DD. Management of mental health and substance abuse services: state of the art and early results. Milbank Q. 1995;73(1):19–55. [PubMed] [Google Scholar]
- 43.Mechanic D. Mental health services in the context of health insurance reform. Milbank Q. 1993;71(3):349–364. [PubMed] [Google Scholar]
- 44.Regier DA, Bufka LF, Whitaker T, et al. Parity and the use of out-of-network mental health benefits in the FEHB program. Health Aff (Millwood) 2008;27(1):w70–w83. doi: 10.1377/hlthaff.27.1.w70. [DOI] [PubMed] [Google Scholar]
- 45.Committee on Aging of the Group for the Advancement of Psychiatry. Medicare managed mental health care: a looming crisis. Psychiatr Serv. 2005;56(7):795–797. doi: 10.1176/appi.ps.56.7.795. [DOI] [PubMed] [Google Scholar]