Abstract
The goal of our study was to estimate the prevalence of osteoporosis and low bone mass based on bone mineral density (BMD) at the femoral neck and the lumbar spine in adults 50 years and older in the United States (US). We applied prevalence estimates of osteoporosis or low bone mass at the femoral neck or lumbar spine (adjusted by age, sex, and race/ethnicity to the 2010 Census) for the non-institutionalized population age 50 years and older from the National Health and Nutrition Examination Survey 2005–2010 to 2010 US Census population counts to determine the total number of older US residents with osteoporosis and low bone mass. There were over 99 million adults 50 years and older in the US in 2010. Based on an overall 10.3% prevalence of osteoporosis, we estimated that in 2010 10.2 million older adults had osteoporosis. The overall low bone mass prevalence was 43.9%, from which we estimated that 43.4 million older adults had low bone mass. We estimated that 7.7 million non-Hispanic White, 0.5 million non-Hispanic Black, and 0.6 million Mexican American adults had osteoporosis and another 33.8, 2.9, and 2.0 million had low bone mass, respectively. When combined, osteoporosis and low bone mass at the femoral neck or lumbar spine affected an estimated 53.6 million older US adults in 2010. Although most of the individuals with osteoporosis or low bone mass were non-Hispanic White women, a substantial number of men and women from other racial/ethnic groups also had osteoporotic BMD or low bone mass.
Keywords: Osteoporosis, Low bone mass, Prevalence, NHANES
Introduction
In 2002, the National Osteoporosis Foundation (NOF) reported the current and future projected number of adults 50 years and older with osteoporosis and low bone mass (previously called osteopenia) in the United States (US) (1). The estimates were based upon bone mineral density (BMD) at the femoral neck measured in the population-based data from the National Health and Nutrition Examination Survey (NHANES) – III (1988–1994). The report indicated that approximately 10 million US adults 50 years of age and older had osteoporosis and an additional 33 million had low bone mass (1). These estimates were based on femoral neck bone mineral density (BMD) only because this was the only skeletal site for which nationally representative BMD data were available from NHANES.
Since that time, multiple US and international organizations have developed new clinical treatment guidelines that may be used for determining the overall prevalence of osteoporosis. For example, the NOF recommends that clinicians consider BMD at both the femoral neck and the lumbar spine to define osteoporosis or low bone mass (2). Other groups such as the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis and the World Health Organization have recommended that population estimates of osteoporosis and low bone mass be based only on the femoral neck (3, 4). Adding to this variability, the International Society for Clinical Densitometry (ISCD) states that femoral neck, lumbar spine, and total hip BMD can be used to diagnose osteoporosis and low bone mass (5).
Starting in 2005, BMD was measured at both the proximal femur and the lumbar spine in NHANES, providing us the opportunity to conduct a comprehensive updated US evaluation of osteoporosis and low bone mass based on bone mass at more than one site. In this report, we estimate the recent and future number of adults 50 years of age and older with osteoporosis and low bone mass in US based on the femoral neck and lumbar spine. We conducted sensitivity analyses to calculate the number with osteoporosis and low bone mass at the femoral neck only in light of the alternative recommendations noted above and to facilitate comparison with results from the 2002 NOF report. We also examined the impact of including the total femur region of interest on prevalence estimates in light of the recommendation from ISCD.
Methods
Estimating Osteoporosis and Low Bone Mass Prevalence in NHANES
The prevalence of osteoporosis and low bone mass in the non-institutionalized US population age 50 years and older was calculated using lumbar spine and femoral neck BMD data collected in NHANES 2005–2010. The NHANES is conducted by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention, to assess the health and nutritional status of a representative sample of the non-institutionalized, civilian US population. BMD of the anterior-posterior lumbar spine and proximal femur was measured with Hologic QDR 4500A fan-beam dual energy X-ray absorptiometry (DXA) densitometers (Hologic, Inc., Bedford, Massachusetts) in specially equipped mobile examination centers. Details of the NHANES BMD examination protocol have been published else where (6–9).
Osteoporosis and low bone mass were defined in the present study using the WHO criteria (10). Specifically, osteoporosis was defined as a T-score ≤ −2.5 at either the femoral neck or the lumbar spine. Among those without osteoporosis, low bone mass was defined as those with T-scores between −1.0 and −2.5 at either skeletal site. As recommended by the WHO (11), the reference group for calculation of the scores at the femoral neck for both men and women, consisted of 20–29 non-Hispanic White females from NHANES III (12). As there is no internationally recommended reference group for the lumbar spine, the reference group for calculation of these scores at the lumbar spine consisted of 30-year old White females from the DXA manufacturer reference database (13). These reference groups were used to calculate T-scores for all race/ethnic groups and for both sexes.
Osteoporosis and low bone mass prevalence estimates were determined for the total sample and by sex, race/ethnicity, and age decade. All prevalence estimates were adjusted to the age, sex, and race/ethnic distribution of the US population at the time of the 2010 Census using direct standardization except where noted. These adjustments were necessary in order to obtain counts that summed up as expected across all relevant categories. This was not always the case when crude prevalence estimates were used. For example, the sum of the age-specific counts for men 50 years of age and older and age-specific counts for women 50 year of age and older did not equal the sum of age-specific counts for both sexes 50 years of age and older when based on crude prevalence estimates. This appeared to be due in part to differential missing data by age, sex and race/ethnicity that occurred in the NHANES BMD sample, in part because the age distribution of the population has changed slightly between 2005–2008 and 2010, and in part because the 2010 Census counts included institutionalized persons, whereas NHANES 2005–2010 was based on the non-institutionalized population. Specifically, the proportion of the 2010 population age 50 years and older falling into 32 age decade, sex, and race/ethnic subgroups was calculated and the resulting proportions were used as standard weights in the analyses.
The age categories used were: 50–59, 60–69, 70–79, and 80+ years, and the race/ethnic categories were non-Hispanic White, non-Hispanic Black, Mexican American, and other races. Estimates by race/ethnicity are presented separately for non-Hispanic Whites, non-Hispanic Blacks, and Mexican Americans because NHANES 2005–2010 provides reliable estimates for these three groups (14). Although estimates are not presented separately for those identified as other racial/ethnic groups, they were included in the estimates for the total population.
The NHANES data were analyzed with PC-SAS (Version 9.2, SAS Institute, Cary, NC) and SUDAAN (Version 10.0, Research Triangle Institute, NC). All analyses used sample weights and took into account the complex design of the survey when calculating standard errors. All procedures in NHANES 2005–2010 were approved by the NCHS Research Ethics Review Board, and written informed consent was obtained from all subjects.
Estimating the Number of Adults With Osteoporosis and Low Bone Mass in 2010
We used the 2010 Census data for the total population (non-institutionalized and institutionalized) from www.census.gov to obtain the total number of adults 50 years and older residing in the US and by state. To determine the overall number of men and women with osteoporosis and low bone mass, we multiplied the age, sex, and race/ethnic-adjusted prevalence estimates for the total non-institutionalized population from NHANES 2005–2010 by the corresponding Census counts for the overall population for the entire nation and by individual state. Similarly we multiplied the adjusted age, sex and race/ethnic-specific NHANES prevalence estimates to the corresponding Census counts for each demographic subgroup. We also applied the NHANES 2005–2010 adjusted prevalence estimates to the projected population counts from the Census for 2020 and 2030 (15) to estimate the future clinical burden of osteoporosis and low bone mass. State based estimates of osteoporosis and low bone mass by gender, age, and race/ethnicity are presented in the supplemental materials.
Sensitivity Analyses
To address previously mentioned definitions of osteoporosis and low bone mass by other international groups, we conducted two sensitivity analyses. For the first, we estimated the crude prevalence and corresponding counts of osteoporosis and low bone mass based only on femoral neck in NHANES 2005–2010, in order to be able to compare them with the estimates based on crude prevalence estimates published by NOF in 2002 (1). For the second sensitivity analysis, we evaluated how the addition of the total hip as a site affected the overall age, sex, and race/ethnic-adjusted prevalence and number of people with osteoporosis and low bone mass.
Our secondary analysis of NHANES and Census data was reviewed by the University of Alabama at Birmingham’s Institutional Review Board, and was deemed non-Human Subjects research.
Results
Table 1 shows the estimated 2010 US Census population estimates, the NHANES 2005–2010 adjusted prevalence of osteoporosis and low bone mass among non-institutionalized adults age 50 years and older, and the corresponding estimated number of persons with osteoporosis and low bone mass for the total population in 2010 as well as by age, sex, and race/ethnicity. Based on the overall adjusted prevalence estimates from NHANES, we determined that 10.2 million adults had osteoporosis and 43.4 million had low bone mass in 2010 (Table 1). More women than men had both osteoporosis and low bone mass. An estimated 8.2 million women and 2.0 million men had osteoporosis and an additional 27.3 million women and 16.1 million men had low bone mass.
Table 1.
Estimates of the Number of US Residents with Osteoporosis and Low Bone Mass at Either the Femoral Neck or Lumbar Spine in 2010.
| Total Population, N | OP Prevalencea % (SE) | OP, N (95% CI)b | LBM Prevalencea % (SE) | LBM, N (95% CI) b | |
|---|---|---|---|---|---|
| Both Sexes | |||||
| Total Population | 99,048,838 | 10.3 (0.37) | 10.2 (9.4,10.9) | 43.9 (0.72) | 43.4 (42.0,44.8) |
| Age | |||||
| 50–59 | 41,962,930 | 5.1 (0.60) | 2.2 (1.7,2.6) | 40.2 (1.12) | 16.9 (16.0,17.8) |
| 60–69 | 29,253,187 | 8.0 (0.87) | 2.3 (1.8,2.8) | 43.6 (1.18) | 12.8 (12.1,13.4) |
| 70–79 | 16,595,961 | 16.4 (0.94) | 2.7 (2.4,3.0) | 47.3 (1.41) | 7.9 (7.4,8.3) |
| 80+ | 11,236,760 | 26.2 (1.59) | 2.9 (2.6,3.4) | 52.9 (2.22) | 5.9 (5.5,6.4) |
| Race/Ethnicityc | |||||
| NH-White | 75,272,609 | 10.2 (0.47) | 7.7 (7.0,8.4) | 44.9 (0.89) | 33.8 (32.5,35.1) |
| NH-Black | 9,830,977 | 4.9 (0.65) | 0.5 (0.4,0.6) | 29.7 (1.51) | 2.9 (2.6,3.2) |
| Mexican American | 4,595,535 | 13.4 (1.10) | 0.6 (0.5,0.7) | 43.2 (1.41) | 2.0 (1.9,2.1) |
|
| |||||
| Women | |||||
| Total Population | 53,151,456 | 15.4 (0.63) | 8.2 (7.5,8.9) | 51.4 (0.93) | 27.3 (26.3,28.3) |
| Age | |||||
| 50–59 | 21,506,008 | 6.8 (0.83) | 1.5 (1.1,1.8) | 49.3 (1.69) | 10.6 (9.9,11.3) |
| 60–69 | 15,323,140 | 12.3 (1.44) | 1.9 (1.5,2.3) | 53.4 (1.54) | 8.2 (7.7,8.6) |
| 70–79 | 9,169,601 | 25.7 (1.56) | 2.4 (2.1,2.6) | 51.8 (1.70) | 4.7 (4.4,5.1) |
| 80+ | 7,152,707 | 34.9 (2.44) | 2.5 (2.2,2.8) | 52.7 (3.07) | 3.8 (3.3,4.2) |
| typoRace/Ethnicityc | |||||
| NH-White | 40,089,289 | 15.8 (0.81) | 6.3 (5.7,7.0) | 52.6 (1.17) | 21.1 (20.2,22.0) |
| NH-Black | 5,534,149 | 7.7 (1.10) | 0.4 (0.3,0.5) | 36.2 (2.03) | 2.0 (1.8,2.2) |
| Mexican American | 2,371,091 | 20.4 (1.70) | 0.5 (0.4,0.6) | 47.8 (2.33) | 1.1 (1.0,1.2) |
|
| |||||
| Men | |||||
| Total Population | 45,897,382 | 4.3 (0.40) | 2.0 (1.6,2.3) | 35.2 (0.93) | 16.1 (15.3,17.0) |
| Age | |||||
| 50–59 | 20,456,922 | 3.4 (0.68) | 0.7 (0.4,1.0) | 30.7 (1.78) | 6.3 (5.6,7.0) |
| 60–69 | 13,930,047 | 3.3 (0.73) | 0.5 (0.3,0.7) | 32.9 (1.82) | 4.6 (4.1,5.1) |
| 70–79 | 7,426,360 | 5.0 (0.78) | 0.4 (0.3,0.5) | 41.8 (2.51) | 3.1 (2.7,3.5) |
| 80+ | 4,084,053 | 10.9 (1.7) | 0.4 (0.3,0.6) | 53.1 (2.82) | 2.2 (1.9,2.4) |
| Race/Ethnicityc | |||||
| NH-White | 35,183,320 | 3.9 (0.39) | 1.4 (1.1,1.6) | 36.0 (1.13) | 12.7 (11.9,13.4) |
| NH-Black | 4,296,828 | 1.3* (0.40) | 0.1 (0.02,0.1) | 21.3 (1.75) | 0.9 (0.8,1.1) |
| Mexican American | 2,224,444 | 5.9 (1.08) | 0.1 (0.1,0.2) | 38.3 (2.55) | 0.9 (0.7,1.0) |
Prevalence from NHANES 2005–2010 has been adjusted to the age, sex, and race/ethnic distribution of the US population at the time of the 2010 Census using the direct method.
Count expressed in millions; 95% CI=95% confidence limits
Other races not shown separately
may be statistically unreliable, standard error/percent is 31–39% or sample size is < 30
OP = osteoporosis; LBM= low bone mass; NH= non-Hispanic
Age and race/ethnic patterns in the counts of people with osteoporosis or low bone mass did not always coincide with age or race-ethnic patterns in the prevalence estimates in Table 1. This is due to the fact that the count is a function of both the prevalence and the population distribution by age or race/ethnicity. In men, for example, the prevalence of osteoporosis was higher in men 80+ (10.9%) compared to men 50–59 years of age (3.4%); however, due to the decrease in male population counts by age, the estimated number of men with osteoporosis was lower by age: 0.7 million in the 50–59 group and 0.4 million in the 80+ group. Another example is the much smaller number of Mexican Americans with osteoporosis (0.6 million) than non-Hispanic whites (7.5 million) with osteoporosis, due to the much smaller proportion of adults age 50 years and older who are Mexican American.
When the adjusted prevalence estimates of osteoporosis and low bone mass from NHANES 2005–2010 were applied to the 2020 and 2030 Census population projections, we estimated that the number of adults 50 years and older with osteoporosis or low bone mass at either the femoral neck or lumbar spine will increase by 10.4 million (19%) from 2010 to 2020 and by 17.2 million (32%) from 2010 to 2030 (Figure 1). We observed similar percentage increases in the number of individuals with osteoporosis alone between 2010, 2020, and 2030.
Figure 1. Projections of Osteoporosis and Low Bone Mass at the Femoral Neck or Lumbar Spine (number in millions).
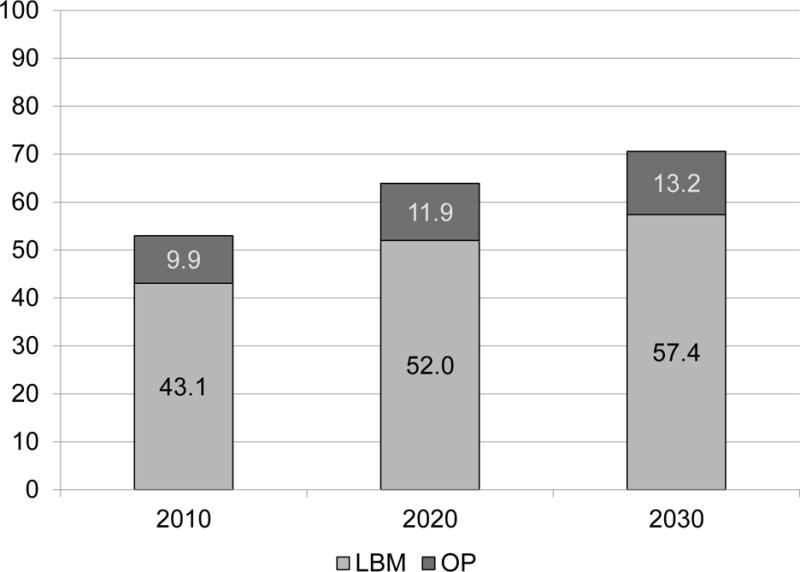
LBM = low bone mass; OP = osteoporosis
Sensitivity Analyses
For the first sensitivity analysis using unadjusted prevalence estimates for femoral neck measurements alone from NHANES 2005–2010, we estimated that in 2010, 4.0 and 25.6 million women and 0.7 and 13.4 million men had osteoporosis and low bone mass, respectively. The number of adults with osteoporosis and low bone mass was lower when using femoral neck alone compared to our main results with femoral neck and lumbar spine. When compared to results from the 2002 NOF report, which were based on unadjusted prevalence estimates for the femoral neck, there was an apparent decrease in the number of women and men 50 years and older with osteoporosis at the femoral neck [women: −3.7 million (−48%); men: −1.6 million (−70%)] between 2000 and 2010]. However, there was an increase in the number with low bone mass [women: +3.8 million (17%); men: +1.6 million (14%)]. When osteoporosis and low bone mass were considered together, no change was observed between the two reports (Table 2).
Table 2.
Absolute and Relative Difference in the Clinical Burden of Osteoporosis and Low Bone Mass at the Femoral Neck Only in 2002 and 2010
| Women*
|
Men*
|
|||||||
|---|---|---|---|---|---|---|---|---|
| 2002 | 2010 | Absolute Diff | % Diff | 2002 | 2010 | Absolute Diff | % Diff | |
| OP | 7.7 | 4.0 | −3.7 | −48.1 | 2.3 | 0.7 | −1.6 | −69.6 |
| LBM | 21.8 | 25.6 | 3.8 | 17.4 | 11.8 | 13.4 | 1.6 | 13.6 |
| OP + LBM | 29.6 | 29.5 | 0.0 | 0.0 | 14.1 | 14.1 | 0.0 | 0.0 |
Diff = difference; OP= osteoporosis; LBM = low bone mass
number in millions based on crude prevalence.
For the second sensitivity analysis, we determined the impact of including the total hip in the definition of osteoporosis and low bone mass. Including the total hip increased the adjusted prevalence of osteoporosis in 2010 among both sexes by 0.4 percentage units and the prevalence of low bone mass by 0.6 percentage units. This increased the number of adults with osteoporosis by 0.8 million and the number with low bone mass by 0.5 million. We observed overlapping confidence intervals between the prevalence estimates with the two sites (femoral neck and lumbar spine) and the prevalence estimates with the three sites, indicating no difference in the two prevalence estimates.
Discussion
We estimated that among adults age 50 years and older, 10.3% or 10.2 million had osteoporosis at the femoral neck or lumbar spine and 43.9% or 43.4 million had low bone mass at either skeletal site in 2010. When combined, the estimated number of adults with osteoporosis and low bone mass was 53.6 million, representing approximately 54% of the US adult population ages 50 years and older.
Similar to previous studies, we found that the prevalence of osteoporosis increased with age, and differed by gender, race and ethnicity (16). The pattern of estimated counts of people with osteoporosis by these demographic characteristics did not always match the pattern of prevalence estimates because the subgroups with the highest prevalence made up a smaller proportion of the total population than subgroups with lower prevalence estimates. For example, the prevalence of osteoporosis was three times higher in men over age 80 than in men age 50–59. However, the number of men with osteoporosis was 41% lower because there are far fewer men over age 80 in the population.
Non-Hispanic Blacks had the lowest prevalence of osteoporosis and low bone mass at either of these two skeletal sites of the three race/ethnic groups compared in our analyses, a result that is consistent with previous results from NHANES (12, 17), as well as other cohort based studies (18). Compared to the other two groups, Mexican Americans had a higher prevalence of osteoporosis in the present study, a finding that has been made previously when age-adjusted prevalence estimates of osteoporosis were examined (16). Differences in prevalence between Mexican Americans and non-Hispanic Whites depend on the skeletal site being considered. Past studies have found a similar or lower prevalence of osteoporosis among Mexican Americans than non-Hispanic Whites at the femoral neck (12, 17), but higher prevalence estimates in Mexican Americans at other skeletal sites such as the spine (16).
The WHO Osteoporosis Working Group and other international osteoporosis organizations have stated that the femoral neck is the only site that should be used in the estimation of osteoporosis prevalence at a population level (3, 4). However, an objective of the present study was to estimate the number of people with osteoporosis and low bone mass as defined by the clinical guidelines from the NOF, which are based on bone status at either the femoral neck or lumbar spine. The rationale for inclusion of lumbar spine BMD testing in the NOF guidelines was to help clinicians identify patients with spinal osteoporosis who warrant consideration for treatment to prevent vertebral fracture. Vertebral fractures are the most common osteoporotic fractures (19), with significant morbidity and increased mortality (20–26), and are a “gateway” to other more serious and more expensive fractures, like the hip (22, 23, 27–32).
Although there is justification for the inclusion of lumbar spine when assessing osteoporosis and low bone mass, we performed secondary analyses to estimate osteoporosis and low bone mass for the femoral neck only to permit comparison with the estimates published by NOF in 2002 (1). When compared to estimates based on either femoral neck or lumbar spine, the use of only femoral neck measurements reduced the number of people in 2010 with osteoporosis by 54% and reduced the number of people with low bone mass by 10%. The differences in these reductions are potentially attributed to bone composition of the lumbar spine, which is predominantly trabecular bone and more prone to the thinning and microarchitectural changes associated with osteoporosis than regions of the hip that are richer in cortical bone.
When compared to the results from the 2002 NOF prevalence report, we found a large decrease in the number of men and women with osteoporosis in 2010, but an increase in the number of people with low bone mass, resulting in no change in the number of people with osteoporosis and low bone mass combined. These changes probably reflect the increase in femoral neck BMD values that has been observed between the two NHANES datasets that were used in these reports (NHANES III 1988–1994 and NHANES 2005–2010) (33). Reasons for these changes have been explored previously (17, 38). Specifically, Looker et. al (38) explored the potential contribution of between-survey changes in 14 bone-related determinants (BMI, height, weight history smoking, health status, dietary calcium, sodium, caffeine, alcohol intake, milk intake, personal and maternal fracture history, use of bone-enhancing and bone-reducing drugs) as well as use of different DXA systems (single-beam versus fan-beam) to the higher BMD values observed in NHANES 2005–2008. Femoral neck BMD differences between the two surveys varied by age, sex, and race/ethnicity, and the differences in several population subgroups fell in the range that could be attributed to use of different DXA systems. However, femoral neck BMD in older non-Hispanic White women remained significantly higher in 2005–2008 even after adjusting for adjusting for DXA methodology or for the bone determinants that had changed in a manner that could lead to higher BMD (increased body size, greater use of osteoporosis treatments other than estrogen, higher calcium consumption, less smoking, and lower caffeine consumption). Thus, the reason for the change in femoral neck BMD between these surveys has not been conclusively identified for all population subgroups (38).
Our second sensitivity analyses examined the effect of considering BMD at the total hip in addition to femoral neck and lumbar spine when estimating osteoporosis and low bone mass prevalence in 2010. This analysis was done because the ISCD includes the use of this site as well as the femoral neck for the diagnosis of osteoporosis and low bone mass (5). Including the total hip in the definition of osteoporosis and low bone mass resulted in small, statistically insignificant increases in the estimates of the prevalence and number with osteoporosis and low bone mass. Thus, the addition of the total hip in the definitions does not appear to significantly increase the prevalence of osteoporosis or low bone mass found in our main analysis. This is not surprising, given that femoral neck T-scores were lower than total hip T-scores in 86% of adults age 50 years and older in NHANES 2005–2010. Whether this would be the case when DXA instruments from manufacturers other than Hologic are used is not clear, since the femur regions of interest vary between DXA manufacturers (34).
The main strength of our study is the use of prevalence estimates of osteoporosis and low bone mass from nationally representative data collected in NHANES, which were applied to US Census population data to estimate the recent and future number of older individuals with both osteoporosis and low bone mass. Although nationally based, the study has some limitations. The study focused on estimates of osteoporosis as defined by BMD. However, fragility fracture constitutes the primary clinical burden associated with osteoporosis and low bone mass, and individuals who have sustained a fragility fracture, particularly hip or spine, without having osteoporosis T-score thresholds, would clinically be considered as having osteoporosis and would warrant treatment (2). The burden of fragility fracture is considerable. For example, data from the Women’s Health Initiative showed that fracture incidence among non-Black women over a one year period was greater than the incidence of invasive breast cancer or cardiovascular disease events combined (35). It has been observed that many women sustaining a fracture fall within the low bone mass range (36). However, fractures were not included in the definition of osteoporosis used in the present study because the validity of the self-reported fracture data available in NHANES was uncertain for non-hip skeletal sites. As a result, our estimates of osteoporosis may be an underestimate of the true clinical burden of osteoporosis in the US population. Likewise, we may be underestimating the number of people who warrant treatment, as clinical decisions regarding treatment include consideration of other risk factors. For example, based on cost effectiveness considerations, treatment thresholds have been proposed using FRAX scores in the NOF treatment guidelines (2).
Other limitations include application of the NHANES prevalence estimates for the non-institutionalized US population to the 2010 Census estimates of the total US population, which includes institutionalized individuals. The impact of our assumption that the prevalence estimates for the non-institutionalized population apply to the total population, including institutionalized persons, is not clear. Studies in North America have shown that the prevalence of osteoporosis in nursing homes, one example of an institutionalized population, range from 13 to 51% (37–42). Use of the osteoporosis and low bone mass prevalence estimates from the non-institutionalized participants of NHANES could have led to an underestimate of the true prevalence in the total population. However, the magnitude of this bias may be modest given that the institutionalized population is a small proportion of the overall 50 years and older population in the US (43).
Although all races and ethnic groups were included in the estimates for the total population, we were not able to estimate the specific prevalence of osteoporosis and low bone mass in Asians or Hispanic groups other than Mexican Americans, as NHANES 2005–2010 can provide estimates by race or ethnicity only for non-Hispanic Whites, non-Hispanic Blacks and Mexican Americans (14). Although Mexican Americans make up 54% of the Hispanic population, the prevalence of osteoporosis and related fractures varies by Hispanic origin (44). Our estimates for Mexican Americans may not apply to other Hispanic groups.
Estimates of the future prevalence of osteoporosis and low bone mass were based on the assumption that prevalence estimates from 2005–2010 reflect the future prevalence of osteoporosis and low bone mass. However, the crude prevalence of low femoral neck osteoporosis and low bone mass appear to have declined in the US in the past two decades (38). If the prevalence of osteoporosis and low bone mass continues to decline, our projections of the number of people with osteoporosis will be overestimated. Finally, we also assumed that the national estimates of osteoporosis and low bone mass reflected the prevalence of osteoporosis and low bone mass in individual states when calculating the estimated number of affected persons by state shown in the supplemental tables.
Conclusion
Osteoporosis and low bone mass combined affected approximately 53.6 million (54%) older US adults in 2010. The estimated number varied by sex and race/ethnicity, with women and non-Hispanic Whites having the largest counts. The patterns of osteoporosis and low bone mass counts by age also varied between men and women. The large number of individuals with osteoporosis and low bone mass underscores the continued importance of addressing bone health in the older population in order to reduce the clinical burden caused by fragility fracture.
Supplementary Material
Acknowledgments
This work was funded by a contract between University of Alabama at Birmingham and The National Osteoporosis Foundation.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Role of Authors:
NCW: Study design, data acquisition, data analysis, manuscript preparation
ACL: Study concept, data acquisition, data analysis, manuscript preparation
KGS: Study design, manuscript review
JRC: Manuscript review
ESD: Manuscript review
SR: Study concept, manuscript review
BDH: Study concept, study design, manuscript review
References
- 1.America’s Bone Health: The State of Osteoporosis and Low Bone Mass in Our Nation. Washington, DC: National Osteoporsis Foundation; 2002. [Google Scholar]
- 2.Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, DC: National Osteoporosis Foundation; 2013. [Google Scholar]
- 3.WHO Scientific Group on the Assessment of Osteoporosis at Primary Health Care Level. Brussels: World Health Organization; 2004. [Google Scholar]
- 4.Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster JY, Borgstrom F, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2008;19(4):399–428. doi: 10.1007/s00198-008-0560-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.2013 ISCD Official Positions - Adult. International Society for Clinical Densitometry; 2013. [Google Scholar]
- 6.Cogswell ME, Looker AC, Pfeiffer CM, Cook JD, Lacher DA, Beard JL, et al. Assessment of iron deficiency in US preschool children and nonpregnant females of childbearing age: National Health and Nutrition Examination Survey 2003–2006. American Journal of Clinical Nutrition. 2009;89(5):1334–42. doi: 10.3945/ajcn.2008.27151. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention NCfHS. National health and Nutrition Examination Survey Body Composition Procedure Manual. US Department of Health and Human Services, Centers for Disease Control and Prevention; 2006. [cited 2011 May 5]. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/BC.pdf. [Google Scholar]
- 8.Centers for Disease Control and Prevention NCfHS. National Health and Nutrition Examination Survey Dual-energy X-ray Absorptimetry (DXA) Procedure Manual Hyattsville. MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. [cited 2011 May 5]. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_dexa.pdf. [Google Scholar]
- 9.Wahner HW, Looker A, Dunn WL, Walters LC, Hauser MF, Novak C. Quality control of bone densitometry in a national health survey (NHANES III) using three mobile examination centers. J Bone Miner Res. 1994;9(6):951–60. doi: 10.1002/jbmr.5650090621. [DOI] [PubMed] [Google Scholar]
- 10.Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ, 3rd, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008;42(3):467–75. doi: 10.1016/j.bone.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Geneva, Switzerland: World Health Organization; 2004. [PubMed] [Google Scholar]
- 12.Looker AC, Orwoll ES, Johnston CC, Jr, Lindsay RL, Wahner HW, Dunn WL, et al. Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res. 1997;12(11):1761–8. doi: 10.1359/jbmr.1997.12.11.1761. [DOI] [PubMed] [Google Scholar]
- 13.Kelly T. Bone mineral density reference databases for American men and women. J Bone Miner Res. 1990;5(Suppl1):S249. [Google Scholar]
- 14.Johnson CLP-RR, Ogden CL, Carroll MD, Kruszan-Moran D, Dohrmann SM, Curtin LR. National Health and Nutrition Examination Survey: Analytic guidelines, 1999–2010. Hyattsville MD: National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- 15.U.S. Census Bureau PD, editor. Projections of the Population by Age and Sex for the United States: 2015 to 2060 (NP2012-T12) 2012. Table 12. [Google Scholar]
- 16.Looker A, Borrud LG, Dawson-Hughes B, Shepherd JA, Wright N. Osteoporosis or low bone mass at the femur neck or lumbar spine in older adults: United States, 2005–2008. NCHS Data Brief. 2012 Apr;(93):1–8. [PubMed] [Google Scholar]
- 17.Looker AC, Melton LJ, 3rd, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005–2006 compared with NHANES III. J Bone Miner Res. 2010;25(1):64–71. doi: 10.1359/jbmr.090706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger ML, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005;20(2):185–94. doi: 10.1359/JBMR.041007. [DOI] [PubMed] [Google Scholar]
- 19.Ensrud KE. Epidemiology of Fracture Risk With Advancing Age. J Gerontol A Biol Sci Med Sci. 2013 doi: 10.1093/gerona/glt092. [DOI] [PubMed] [Google Scholar]
- 20.Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–21. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 21.Ensrud KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, et al. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc. 2000;48(3):241–9. doi: 10.1111/j.1532-5415.2000.tb02641.x. [DOI] [PubMed] [Google Scholar]
- 22.Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O. Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 2003;14(1):61–8. doi: 10.1007/s00198-002-1316-9. [DOI] [PubMed] [Google Scholar]
- 23.Ismail AA, Cockerill W, Cooper C, Finn JD, Abendroth K, Parisi G, et al. Prevalent vertebral deformity predicts incident hip though not distal forearm fracture: results from the European Prospective Osteoporosis Study. Osteoporos Int. 2001;12(2):85–90. doi: 10.1007/s001980170138. [DOI] [PubMed] [Google Scholar]
- 24.Jalava T, Sarna S, Pylkkanen L, Mawer B, Kanis JA, Selby P, et al. Association between vertebral fracture and increased mortality in osteoporotic patients. J Bone Miner Res. 2003;18(7):1254–60. doi: 10.1359/jbmr.2003.18.7.1254. [DOI] [PubMed] [Google Scholar]
- 25.Kado DM, Duong T, Stone KL, Ensrud KE, Nevitt MC, Greendale GA, et al. Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int. 2003;14(7):589–94. doi: 10.1007/s00198-003-1412-5. [DOI] [PubMed] [Google Scholar]
- 26.Trone DW, Kritz-Silverstein D, von Muhlen DG, Wingard DL, Barrett-Connor E. Is radiographic vertebral fracture a risk factor for mortality? Am J Epidemiol. 2007;166(10):1191–7. doi: 10.1093/aje/kwm206. [DOI] [PubMed] [Google Scholar]
- 27.Black DM, Arden NK, Palermo L, Pearson J, Cummings SR. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999;14(5):821–8. doi: 10.1359/jbmr.1999.14.5.821. [DOI] [PubMed] [Google Scholar]
- 28.Delmas PD, Genant HK, Crans GG, Stock JL, Wong M, Siris E, et al. Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone. 2003;33(4):522–32. doi: 10.1016/s8756-3282(03)00241-2. [DOI] [PubMed] [Google Scholar]
- 29.Hodsman AB, Leslie WD, Tsang JF, Gamble GD. 10-year probability of recurrent fractures following wrist and other osteoporotic fractures in a large clinical cohort: an analysis from the Manitoba Bone Density Program. Arch Intern Med. 2008;168(20):2261–7. doi: 10.1001/archinte.168.20.2261. [DOI] [PubMed] [Google Scholar]
- 30.Roux C, Fechtenbaum J, Kolta S, Briot K, Girard M. Mild prevalent and incident vertebral fractures are risk factors for new fractures. Osteoporos Int. 2007;18(12):1617–24. doi: 10.1007/s00198-007-0413-1. [DOI] [PubMed] [Google Scholar]
- 31.Schousboe JT, Fink HA, Lui LY, Taylor BC, Ensrud KE. Association between prior non-spine non-hip fractures or prevalent radiographic vertebral deformities known to be at least 10 years old and incident hip fracture. J Bone Miner Res. 2006;21(10):1557–64. doi: 10.1359/jbmr.060711. [DOI] [PubMed] [Google Scholar]
- 32.Buckens C, de Jong P, Mali W, Verhaar H, van der Graaf Y, Verkooijen H. Prevalent vertebral fractures on chest CT: Higher risk for future hip fracture. J Bone Miner Res. 2013 doi: 10.1002/jbmr.2028. [DOI] [PubMed] [Google Scholar]
- 33.Looker AC, Melton LJ, 3rd, Borrud LG, Shepherd JA. Changes in femur neck bone density in US adults between 1988–1994 and 2005–2008: demographic patterns and possible determinants. Osteoporos Int. 2012;23(2):771–80. doi: 10.1007/s00198-011-1623-0. [DOI] [PubMed] [Google Scholar]
- 34.Fan B, Lu Y, Genant H, Fuerst T, Shepherd J. Does standardized BMD still remove differences between Hologic and GE-Lunar state-of-the-art DXA systems? Osteoporos Int. 2010;21(7):1227–36. doi: 10.1007/s00198-009-1062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cauley JA, Wampler NS, Barnhart JM, Wu L, Allison M, Chen Z, et al. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19(12):1717–23. doi: 10.1007/s00198-008-0634-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hillier TA, Cauley JA, Rizzo JH, Pedula KL, Ensrud KE, Bauer DC, et al. WHO absolute fracture risk models (FRAX): do clinical risk factors improve fracture prediction in older women without osteoporosis? J Bone Miner Res. 2011;26(8):1774–82. doi: 10.1002/jbmr.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chandler JM, Zimmerman SI, Girman CJ, Martin AR, Hawkes W, Hebel JR, et al. Low bone mineral density and risk of fracture in white female nursing home residents. JAMA. 2000;284(8):972–7. doi: 10.1001/jama.284.8.972. [DOI] [PubMed] [Google Scholar]
- 38.Elliott ME, Binkley NC, Carnes M, Zimmerman DR, Petersen K, Knapp K, et al. Fracture risks for women in long-term care: high prevalence of calcaneal osteoporosis and hypovitaminosis D. Pharmacotherapy. 2003;23(6):702–10. doi: 10.1592/phco.23.6.702.32182. [DOI] [PubMed] [Google Scholar]
- 39.Elliott ME, Drinka PJ, Krause P, Binkley NC, Mahoney JE. Osteoporosis assessment strategies for male nursing home residents. Maturitas. 2004;48(3):225–33. doi: 10.1016/j.maturitas.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 40.Giangregorio LM, Jantzi M, Papaioannou A, Hirdes J, Maxwell CJ, Poss JW. Osteoporosis management among residents living in long-term care. Osteoporos Int. 2009;20(9):1471–8. doi: 10.1007/s00198-009-0837-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Swislocki A, Green JA, Heinrich G, Barnett CA, Meadows ID, Harmon EB, et al. Prevalence of osteoporosis in men in a VA rehabilitation center. Am J Manag Care. 2010;16(6):427–33. [PubMed] [Google Scholar]
- 42.Toofanny N, Maddens ME, Voytas J, Kowalski D. Low bone mass and postfall fracture risk among elderly nursing home men. J Am Med Dir Assoc. 2004;5(6):367–70. doi: 10.1097/01.JAM.0000141951.73974.F9. [DOI] [PubMed] [Google Scholar]
- 43.Characteristics of the Group Quarters Population by Group Quarters Type - 2010 American Community Survey 1-Year Estimates (S2601B) Washington, DC: U.S. Census Bureau; 2010. [Google Scholar]
- 44.Lauderdale DS, Jacobsen SJ, Furner SE, Levy PS, Brody JA, Goldberg J. Hip fracture incidence among elderly Hispanics. Am J Public Health. 1998;88(8):1245–7. doi: 10.2105/ajph.88.8.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


