Abstract
Background
Characterizing geographic access depends on a broad range of methods available to researchers and the healthcare context to which the method is applied. Globally, travel time is one frequently used measure of geographic access with known limitations associated with data availability. Specifically, due to lack of available utilization data, many travel time studies assume that patients use the closest facility. To examine this assumption, an example using mammography screening data, which is considered a geographically abundant health care service in the United States, is explored. This work makes an important methodological contribution to measuring access—which is a critical component of health care planning and equity almost everywhere.
Method
We analyzed one mammogram from each of 646,553 women participating in the US based Breast Cancer Surveillance Consortium for years 2005–2012. We geocoded each record to street level address data in order to calculate travel time to the closest and to the actually used mammography facility. Travel time between the closest and the actual facility used was explored by woman-level and facility characteristics.
Results
Only 35 % of women in the study population used their closest facility, but nearly three-quarters of women not using their closest facility used a facility within 5 min of the closest facility. Individuals that by-passed the closest facility tended to live in an urban core, within higher income neighborhoods, or in areas where the average travel times to work was longer. Those living in small towns or isolated rural areas had longer closer and actual median drive times.
Conclusion
Since the majority of US women accessed a facility within a few minutes of their closest facility this suggests that distance to the closest facility may serve as an adequate proxy for utilization studies of geographically abundant services like mammography in areas where the transportation networks are well established.
Background
Appropriately assessing the influence that geographic access has on utilization of services is a critical component of health care planning and equity almost everywhere [1–4]. The ability to adequately measure the influence that geographic access has on health care service utilization depends on a broad range of methods available to researchers and the healthcare context for which the method is applied [5–11]. Globally popular methods for characterizing geographic access include the two step floating catchment area (2SFCA), areal interpolation methods such as kernel density estimation (KDE), and travel time studies [6, 7]. Notably, comparative analyses of these methods demonstrates that there is no conclusive, standard approach to characterizing geographic access in the context of healthcare; and because of this lack of standard it is difficult to determine the true magnitude of potential effect that geographic access has on utilization or healthcare services regardless of the geographic locale of study [6, 7, 12].
Since travel time is identified as a frequently used measure of geographic access to health care services, we will examine one of the fundamental assumptions associated with this particular geographic access method citing mammography in the United States as an example [13–30]. Typically, travel time is calculated as a driving time either based on geocoded residential addresses or, more commonly, using the distance from a representative residential location (e.g. polygon-based calculated centroids such as census block/block group/tract and/or ZIP code centroid in the United States) to the facility. Many travel time studies assume that individuals access health care services at the facility closest to the location where they reside [9, 12–15, 20, 21, 23, 24, 31, 32]. Thus, reported travel times have represented minimum travel times that may differ from actual travel times based on health care service utilization data.
Further, differences in potential versus actual travel time may vary by population subgroup characteristics in the United States. For example, rural patients may be more likely to use the facility that is closest because of fewer available service options or may be influenced by non-geographic factors such as seasonal weather burdens [22]. To our knowledge, prior studies have not tested the assumption that patients use the closest facility or whether this assumption differs for some population subgroups. This work addresses a fundamental methodological question in spatial epidemiology and health services research: concordance of proximity versus utilization-based measures of health care access, and whether population characteristics modify concordance.
We focus on mammography in the United States which is a relatively geographically abundant health care service. Prior US based work has measured geographic access to breast imaging facilities in terms of travel time to the closest facility [7, 14, 15, 19, 21, 24, 33]. However, these studies did not examine utilization data and thus were not able to fully characterize individuals’ travel patterns. Research suggests that, despite the abundance of mammography facilities, there are sub-populations for whom utilization is lower than recommended [23, 24, 27, 34, 35]. Increased travel burden may contribute to lower utilization rates in these sub-populations, but this hypothesis is difficult to assess when measures of geographic access are typically based solely on proximity to closest services [14, 18, 33, 36] rather than the services actually used.
We compare travel times between the closest and actual mammography facility attended for women within five registries of the Breast Cancer Surveillance Consortium (BCSC) [37] to establish the magnitude of differences between the two. By linking mammography registry data with patient and population characteristics from US Census data, we are able to quantify and compare closest versus actual geographic access for population subgroups, including stratifying patients by age, race, rural residence, and income. We also examine individual facility characteristics in order to determine if there may be health system factors associated with women more willing to travel further in order to obtain services.
Methods
Study population
Our study population includes all women aged 30–90 years who received a mammography exam at a facility participating in the BCSC between 2004 and 2010. In order to avoid over-estimating travel times, only one mammogram was included per woman. If there were multiple exams per woman, we randomly selected one. The BCSC is a National Cancer Institute (NCI)-funded network of mammography registries across the United States. We used registry data from New Hampshire, North Carolina, San Francisco, Vermont, and New Mexico. Each registry, as well as the Statistical Coordinating Center (SCC) that processed the pooled data, has received institutional review board (IRB) approval for either active or passive consenting processes or a waiver of consent to enroll participants, link data, and perform analytic studies. All procedures are Health Insurance Portability and Accountability Act (HIPAA) compliant and all registries and the SCC have received a Federal Certificate of Confidentiality and other protection for the identities of women, physicians, and facilities involved in this research.
Patient and facility characteristics
At the time of examination, women receiving mammography at a BCSC facility self-report basic demographic information including age, ethnicity/race and highest level of education. For women in the BCSC with multiple mammography exams, we randomly selected one exam per woman. We linked individual self-report demographic data to community-level characteristics that were obtained through address-based linkage to 2010 US Census data from the ESRI Business Analyst application [38]. Community-level demographic information included rural–urban status, diversity index score [a measure of the population diversity of a given geographic area that ranges from 0 (low diversity) to 1 (high diversity)] [39], median household income level, median travel time to work, and mean dollars spent on public transportation per year. The lowest level of geography available, either census block group, tract or ZIP code level, for each variable is indicated in Table 1.
Table 1.
Sample characteristics of BCSC mammograms by woman, facility, and census-level characteristics
| Geographic level of variable | N | % | N missing | |
|---|---|---|---|---|
| Total population | 646,553 | |||
| Woman-level characteristics | ||||
| Age | Woman level | 0 | ||
| 30–40 | 35,483 | 5.5 | ||
| 40–49 | 194,760 | 30.1 | ||
| 50–59 | 181,832 | 28.1 | ||
| 60–69 | 126,106 | 19.5 | ||
| 70–79 | 75,192 | 11.6 | ||
| 80+ | 33,180 | 5.1 | ||
| Race/ethnicity | Woman level | 119,624 | ||
| White, non-Hispanic | 372,016 | 70.6 | ||
| Black, non-Hispanic | 38,949 | 7.4 | ||
| Hispanic | 27,315 | 5.2 | ||
| Asian | 75,278 | 14.3 | ||
| Native American | 3040 | 0.6 | ||
| Other | 10,331 | 2 | ||
| Education | Woman level | 242,322 | ||
| Less than high school | 37,773 | 9.3 | ||
| High school | 83,888 | 20.8 | ||
| Some college | 100,696 | 24.9 | ||
| College or post-college graduate | 181,874 | 45 | ||
| Census-levelb characteristics | ||||
| Rurality | Censusb: 2006 zip code | 238 | ||
| Urban core | 452,224 | 70 | ||
| Suburban areas | 41,888 | 6.5 | ||
| Large town areas | 93,165 | 14.4 | ||
| Small town and isolated rural | 59,038 | 9.1 | ||
| Median household income | Censusb: Block group | 503 | ||
| <45K | 144,480 | 22.4 | ||
| 45–59,999K | 139,912 | 21.7 | ||
| 60–84,999K | 198,303 | 30.7 | ||
| 85K+ | 163,355 | 25.3 | ||
| Diversity index | Censusb: Tract | 503 | ||
| 0–25 | 148,217 | 22.9 | ||
| 26–50 | 158,971 | 24.6 | ||
| 51–75 | 243,632 | 37.7 | ||
| 76–100 | 95,230 | 14.7 | ||
| Average spent on public transportation | Censusb: Block group | 503 | ||
| <100$ | 364,469 | 56.4 | ||
| >100$ | 281,581 | 43.6 | ||
| Median travel time to work | Censusb: Block group | 3 | ||
| <15 min | 51,038 | 7.9 | ||
| 15–30 min | 473,988 | 73.3 | ||
| >30 min | 121,524 | 18.8 | ||
| Actual facilitya characteristics | ||||
| Academic status | Facility levela | 172,334 | ||
| Academic | 65,966 | 13.9 | ||
| Non-academic | 408,253 | 86.1 | ||
| Practice type | Facility levela | 172,334 | ||
| Multispecialty | 126,331 | 26.6 | ||
| General radiology | 330,449 | 69.7 | ||
| Breast imaging only | 13,370 | 2.8 | ||
| Non-radiology | 4069 | 0.9 |
aFacility where the exam took place
bCensus-level variable for woman’s place of residence
In 2012, registries provided data on characteristics of each BCSC participating mammography facility. This analysis provided results from 105 of the BCSC affiliated locations. These data included academic affiliation (academic, non-academic) and practice type (multi-specialty breast center, radiology, breast imaging only, and non-radiology). A “multi-specialty breast center” refers to a practice with additional specialties beyond radiology (e.g., cancer center with breast imagers, breast surgeons, and breast oncologists); “general radiology” practice images other body parts in addition to the breasts; “breast imaging only” is a radiology practice only imaging the breasts; and “non-radiology” is a facility without radiologists that offers screening mammography services on-site (e.g., an obstetrician-gynecologist clinic).
Closest and actual travel times
To calculate travel time, we obtained residential and individual mammography facility addresses and geocoded them to the street level. Approximately 10 % of patient addresses could not be geocoded at the street address level and were excluded from the analysis. Since some facilities in a woman’s area may not participate in the BCSC, each registry provided a catchment area to search for additional locations that provide mammography. To delineate a catchment area, each registry provided a list of zip codes that are considered part of the facility catchment area. Those zip codes were then used to look up facilities listed in the Food and Drug Administration (FDA) mammography database [40] that do not participate in the BCSC. The BCSC versus non-BCSC counts for each registry are listed here: in NC, we had 236 BCSC facilities and 5 non-BCSC facilities, NH we have 47 BCSC and 11 non-BCSC facilities, San Francisco we have 25 BCSC facilities and 98 non-BCSC facilities, NM has 27 BCSC facilities and 30 non-BCSC facilities, and VT has 16 BCSC facilities and 1 non-BCSC facility. This is a total of 321 BCSC facilities and 145 non-BCSC facilities for our study population. For each registry, we used ArcGIS v. 10.1 (Environmental Systems Research Institute, Redlands, CA), and the Streetmap N.A. network datasest, to calculate the shortest travel time between each woman’s address and facility location pair, with 180 min as the upper limit. We exclude patients outside of the 180 min, or if their residential address was outside of the designated facility catchment area, to reduce computational challenges. We chose a 180 min cut off since we assume it is unlikely a woman would drive more than 3 h for a mammography screening. Outside of catchment area excludes N = 9810 women; outside the 180 min service area excludes an additional 6485 women. Differential drive time was calculated as the difference between drive time to the closest facility and the facility actually used. A differential drive time of 0 indicates that the exam took place at the closest facility; differences greater than 0 indicate that the woman did not use the closest facility for the exam.
Statistical analysis
We summarized the actual, closest and differential drive times by sub-groups defined by patient and facility characteristics using univariate summary statistics [median and interquartile range (IQR)]. Additionally, we calculated the proportion of women using the closest facility including cumulative distribution functions for closest, actual, and differential drive time, accounting for censoring of actual drive times at 180 min. The probability of differential drive time being less than 5, 10, 30 and 60 min for different covariate levels were derived from the cumulative distribution functions. These univariate summary measures enable us to describe whether the difference between travel times to the closest and actual facility differs across population sub-groups. All statistical analyses were conducted in R 3.1.2 [41].
Results
Patient- and facility-level characteristics
The 646,553 eligible mammography exams in our study sample are described in Table 1. Overall, the largest proportion of women in the sample population were within the screening ages of 40–49 (30.1 %), 50–59 (28.1 %) and 60–69 (19.5 %). 70.6 % of the women were non-Hispanic white, and the largest proportion of the sample population reported at least college or post-graduate degrees (45 %). Most exams took place at non-academic facilities (86.1 %) and general radiology practices (69.7 %).
Area-level characteristics
Census characteristics reveal that the sample population lived in predominantly ‘Urban Core’ (70 %) areas. The median household income was relatively high in this sample population. For example, 30.7 % of the Census block groups reported a median household income of ‘60–84K’ and 25.3 % reported an income of ‘85K or higher’. More than half of the sample lived in areas in which residents spent less than $100 a year on public transportation (56.4 %). Moreover, nearly three quarters of study participants lived in Census block groups where the median travel time to work was ‘15–30 min’ and 18.8 % % lived in areas having a median travel time to work ‘greater than 30 min’.
Travel time summary
The travel times to the closest and actual facilities visited are summarized in Table 2. Figure 1 shows the cumulative distribution of closest, actual, and differential travel time overall and stratified by population characteristics. The median travel time to the closest facility was 5 min (IQR [3,10]), and to the actual facility was 9 min (IQR [5,17]). Rural/urban status revealed notable differences in travel time to closest and actual facilities. Those living in the urban core had a median travel time to the closest facility of 4 min (IQR [2,7]), while those living in small towns or isolated rural areas had a median travel time of 14 min to the closest facility (IQR [6,25]) and an actual travel time of 23 min (IQR [9,41]).
Table 2.
Summary of closest, actual, and differential travel times in sample of BCSC mammograms by woman, facility, and census-level characteristics
| Geographic level of variable | Travel time-median and IQR | Cumulative distribution of differential travel time (proportion) | |||||
|---|---|---|---|---|---|---|---|
| Closest facility | Actual facility | (actual = closest) 0 m | <5 m | <10 m | <30 m | ||
| All | 5 (3,10) | 9 (5,17) | 0.35 | 0.73 | 0.84 | 0.96 | |
| Woman-level characteristics | |||||||
| Age | Woman level | ||||||
| 30–40 | 6 (3,11) | 11 (6,19) | 0.29 | 0.68 | 0.79 | 0.94 | |
| 40–49 | 5 (3,10) | 10 (6,18) | 0.33 | 0.7 | 0.82 | 0.96 | |
| 50–59 | 6 (3,11) | 10 (6,18) | 0.34 | 0.72 | 0.83 | 0.95 | |
| 60–69 | 5 (3,11) | 9 (5,17) | 0.37 | 0.74 | 0.84 | 0.95 | |
| 70–79 | 5 (2,9) | 8 (4,15) | 0.40 | 0.79 | 0.88 | 0.96 | |
| 80+ | 4 (2,8) | 7 (4,12) | 0.44 | 0.83 | 0.91 | 0.98 | |
| Race/ethnicity | Woman level | ||||||
| White, non-Hispanic | 6 (3,12) | 10 (6,19) | 0.39 | 0.74 | 0.83 | 0.95 | |
| Black, non-Hispanic | 5 (3,10) | 10 (6,21) | 0.31 | 0.68 | 0.78 | 0.92 | |
| Hispanic | 6 (3,10) | 9 (6,14) | 0.36 | 0.76 | 0.89 | 0.97 | |
| Asian | 3 (2,5) | 8 (4,11) | 0.16 | 0.66 | 0.86 | 0.98 | |
| Native American | 5 (3,10) | 10 (6,16) | 0.28 | 0.73 | 0.87 | 0.96 | |
| Other | 4 (2,8) | 8 (4,16) | 0.32 | 0.72 | 0.84 | 0.97 | |
| Education | Woman level | ||||||
| Less than high school | 4 (2,7) | 8 (4,12) | 0.37 | 0.77 | 0.90 | 0.97 | |
| High school | 6 (3,13) | 10 (5,19) | 0.43 | 0.75 | 0.85 | 0.95 | |
| Some college | 5 (3,10) | 9 (5,18) | 0.37 | 0.72 | 0.82 | 0.95 | |
| College or post-college graduate | 4 (2,9) | 9 (5,16) | 0.31 | 0.71 | 0.83 | 0.96 | |
| Census-levelb characteristics | |||||||
| Rurality | Censusb: 2006 zip code | ||||||
| Urban core | 4 (2,7) | 8 (5,13) | 0.29 | 0.75 | 0.87 | 0.98 | |
| Suburban areas | 18 (12,24) | 23 (15,32) | 0.43 | 0.69 | 0.79 | 0.96 | |
| Large town areas | 9 (4,16) | 14 (6,27) | 0.47 | 0.72 | 0.77 | 0.9 | |
| Small town and isolated rural | 14 (6,25) | 23 (9,41) | 0.57 | 0.65 | 0.7 | 0.86 | |
| Median household income | Censusb: Block group | ||||||
| <45K | 6 (3,14) | 10 (5,25) | 0.43 | 0.73 | 0.8 | 0.92 | |
| 45–59,999K | 8 (3,14) | 12 (6,23) | 0.38 | 0.72 | 0.81 | 0.94 | |
| 60–84,999K | 5 (3,9) | 9 (6,15) | 0.34 | 0.74 | 0.88 | 0.98 | |
| 85K+ | 4 (2,7) | 8 (5,14) | 0.28 | 0.72 | 0.85 | 0.98 | |
| Diversity index | Censusb: Tract | ||||||
| 0–25 | 11 (5,18) | 14 (7,24) | 0.53 | 0.76 | 0.83 | 0.95 | |
| 26–50 | 6 (2,10) | 9 (5,17) | 0.35 | 0.74 | 0.82 | 0.95 | |
| 51–75 | 4 (2,7) | 8 (5,14) | 0.27 | 0.72 | 0.85 | 0.96 | |
| 76–100 | 4 (2,8) | 9 (5,14) | 0.28 | 0.69 | 0.83 | 0.97 | |
| Average spent on public transportation | Censusb: Block group | ||||||
| <100$ | 8 (4,14) | 12 (7,22) | 0.38 | 0.72 | 0.82 | 0.93 | |
| >100$ | 3 (2,6) | 7 (4,12) | 0.31 | 0.75 | 0.86 | 0.98 | |
| Median travel time to work | Censusb: Block group | ||||||
| <15 min | 4 (2,6) | 6 (3,15) | 0.54 | 0.78 | 0.8 | 0.88 | |
| 15–30 min | 6 (3,11) | 10 (6,17) | 0.36 | 0.74 | 0.84 | 0.96 | |
| >30 min | 5 (3,9) | 9 (6,19) | 0.22 | 0.69 | 0.85 | 0.98 | |
| Actual facilitya characteristics | |||||||
| Academic status | Facility levela | ||||||
| Academic | 4 (2,9) | 9 (5,17) | 0.31 | 0.69 | 0.83 | 0.95 | |
| Non-academic | 4 (2,8) | 9 (5,14) | 0.33 | 0.75 | 0.87 | 0.98 | |
| Practice type | Facility levela | ||||||
| Multispecialty | 3 (2,6) | 8 (4,14) | 0.22 | 0.68 | 0.83 | 0.98 | |
| General radiology | 5 (2,9) | 9 (5,15) | 0.38 | 0.77 | 0.88 | 0.97 | |
| Breast imaging only | 7 (4,11) | 10 (7,16) | 0.22 | 0.72 | 0.87 | 0.96 | |
| Non-radiology | 8 (4,14) | 12 (7,21) | 0.42 | 0.73 | 0.85 | 0.98 | |
aFacility where the exam took place
bCensus-level variable for woman’s place of residence
Fig. 1.
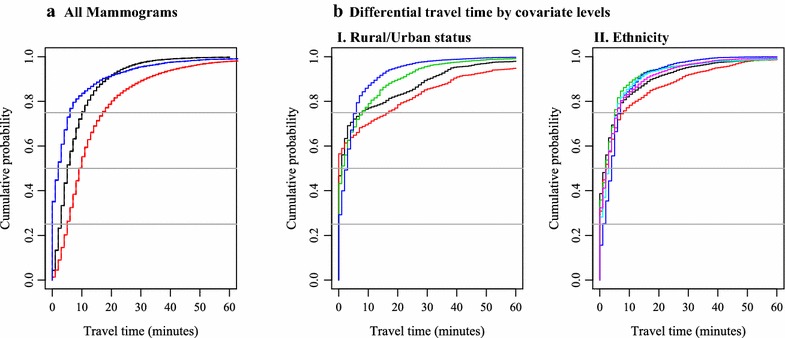
a Cumulative distribution functions of actual, closest, and differential drive time. b Cumulative distribution functions of differential drive times by covariates. I Rural/urban status. II Ethnicity. a
 Closest.
Closest.  Actual.
Actual.  Differential. bI
Differential. bI
 Large rural town.
Large rural town.  Small town/isolated rural.
Small town/isolated rural.  Sub-urban.
Sub-urban.  Urban core. bII
Urban core. bII
 White, non-Hispanic.
White, non-Hispanic.  Black, non-Hispanic.
Black, non-Hispanic.  Hispanic.
Hispanic.  Asian.
Asian.  Native American.
Native American.  Other
Other
Summary of differential travel times
Overall, 65 % of exams did not occur at a woman’s closest facility (Table 2). Women who were older (44 % of women 80 and older), lived in non-urban areas (57 % of small town and isolated rural), and/or areas with low diversity (53 % of 0–25 diversity index) or lower median incomes (43 % of 45K or less) were more likely to use the closest facility. These exams were more likely to take place at a ‘general radiology’ (38 %) or ‘non-radiology’ (42 %) location.
In contrast, exams that were less likely to take place at the closest facility included those obtained at a “breast imaging only” (22 %) or “multispeciality” (22 %) facility and those for women who lived in census blocks in urban core areas (29 %), with higher population diversity indices (27 % of areas with 51–75 % diversity score), greater median yearly income (28 % for 85K or higher), and/or longer median travel times to work (22 % for a commute of 30 min or longer).
While approximately one-third of exams took place at the closest facility, most occurred at facilities that were within a few minutes’ drive of the closest facility. Figure 1 shows the cumulative distribution function for differential travel time. Overall, 73 % of exams took place at facilities at or within 5 min’ travel time of the closest facility. This percentage displayed relatively little variability across subgroups (all were in a range of ±10 % points).
Specific sub-groups for which comparatively more exams took place within 5 min of the closest facility included women >80 years old (83 %) and those living in a block group with a median travel time to work <15 min (78 %). Sub-groups for which a smaller proportion of exams had differential drive times ≤5 min included women who were Black or Asian (68 and 66 %, respectively), women living in an area with high population diversity (69 % of 76–100 % diversity score), women <40 years old (68 % of women ages 30–40), women living in a suburban area (69 %), and women living in areas where the median travel time to work was >30 min (69 %).
Figure 1b provides a more detailed view of the differences by rural/urban status and ethnicity. We selected these specific variables because they highlight most noticeable differences in differential drive times. Particularly, exams obtained in urban cores were less likely to take place at the closest facility but overall had relatively small differential drive times, compared with suburban and rural regions. The distribution of differential drive times is quite similar by ethnicity, although there is some indication that the distribution is slightly different among African American women.
Discussion
Our study provides an improved understanding of how accuracy in measuring geographic access is likely to matter in the broader context of healthcare utilization, regardless of study locale. Specifically, our study critically examines a common assumption associated with estimating geographic access—whether or not using the closest facility to evaluate geographic access is an adequate proxy for utilization data. Our analysis aimed to elucidate the differences that may exist between closest and actual facility attended both overall and for specific populations, and contexts. To our knowledge, this type of comparative analysis has not been applied to this common assumption before.
Our analysis was facilitated by having both the street level addresses of patients and mammography facilities as well as utilization data from the nationally representative BCSC sample of breast imaging facilities. Our study reveals that only 35 % of women undergoing mammography used the closest facility. Nevertheless, nearly 75 % of women undergoing mammography used a facility within 5 min of the closest facility. Population-level urban/rural status, income, and travel time to work appear to be more closely associated with the use of the closest facility. In general, these findings point to the fact that those living in more diverse urban areas and those traveling farther for work are less likely to use their closest facilities.
Our study suggests that appropriateness of using the common assumption that travel time to the closest facility to assess geographic access to healthcare service may depend on the abundance of the service. In an area where the service is geographically abundant, people may be less likely to use the closest facility; whereas in areas where the services are less uniformly available, including rural areas or areas that are far from places of employment, the assumption of closest facility utilization is more likely to be valid.
Nonetheless, analyses for which closest travel time is used as an approximation to determine the influence geographic access has on utilization may not be completely in error given that in the United States nearly three-fourths of women not utilizing the closest facility in this sample traveled to facilities within 5 min of the closest facility. This means that for geographically abundant services like mammography, even if they are not choosing their closest facility, the facility they are choosing is unlikely to be dramatically distant from their closest facility. However, in analyses where this approximation is used as a predictor, this will introduce measurement error which can lead to bias when estimating relationships between access to care and health outcomes [42].
It is also important to note that the interquartile ranges of the actual travel times were quite large in many sub-groups of our study population, even though the median values were relatively small (e.g., women younger than 40 had an actual median travel time of 10, but the IQR 6–18). For some, their round trip travel time may be substantially longer than the median for this study sample. Specifically, this analysis only reflects a one-way travel time, and to get a more accurate picture of the total travel burden we would need to obtain a round trip travel time. For this example, median round trip travel to a mammographic service was 20 min with an interquartile range of 12–36 min. This is important to consider when evaluating the differential travel times since the discrepancies between travel time to the closest and actual facilities would be larger in analyses that examined round trip travel times.
The results of this paper augment existing US based studies in which the influence of geographic access to healthcare, as measured by travel time, is not precisely understood [13, 15, 33]. Often this is due to limitations in available data that compel researchers to use the closest facility assumption in order to gain insight into health care utilization patterns [7, 14, 19, 21, 36]. Our study reveals that under certain conditions, the use of the closest facility to estimate geographic access to mammographic facilities may be appropriate. In the pooled data, we found that the closest facility assumption is most likely to hold for women living in rural communities and in populations that are older, have lower socio-economic status and are more racially and ethnically homogeneous.
A more precise model of utilization facilitates insight into the role that travel time plays in choice of health care facility, particularly for breast cancer screening in the context of the United States. In our study, it appears that with a relatively geographically abundant health service such as mammography, geographic access is generally longer for certain rural sub-populations. For example, for almost all of those in an urban core, a facility can be reached in <30 min; whereas, in a small town and isolated rural areas, that number climbs to >60 min. It appears that urban residents, more so than their rural counterparts, may be able to exercise “choice” in facilities due to the relative abundance of mammographic services within a small geographic area.
The translation of these results to international settings outside of the United States are broadly applicable to geographic locales that maintain similar geographic features to our example in relation to (1) the availability of abundant health care services (such as our case with mammography), (2) with well-established transportation networks.
It is especially important to note that the apparent rural access burden in the United States may be tempered by the fact that individuals who work further away from their residences may actually have geographic access patterns that align with their regular daily routines. For instance, the potential burden would be lessened if a woman can access the service at a location near her place of employment. This general observation could also apply to women outside the United States that travel reasonably far distances to work and want to obtain care close to her place of employment to minimize the daily travel burden.
Limitations of our analysis include the assumption that all registry patients have personal access to a vehicle. This assumption persists in most travel time analyses [7, 15, 19–23, 31, 33, 35, 36] that have indicated that urban travel times are relatively small, but assume that individuals are driving a single passenger vehicle when they are likely walking or taking public transportation to their destination. Future studies should accommodate urban multi-modal transportation networks. A study by Peipins et al. [23], which included a multi-modal network for Atlanta, further illustrates the need for national multi-modal networks to include both public and private transportation. The need for a multi-modal transportation network is of particular relevance to the international community for which multi-modal transportation networks are relatively more broadly accepted as a means of travel than the United States which is commonly associated with single passenger travel. Additionally, while the BCSC sample data are considered representative of the US population, this analysis does not include Hawaii and Alaska which have larger proportions of rural populations and different modes of transportation including water or air transportation, both resulting in different patterns of access and utilization compared to other sub-populations [27]. Moreover, the highest proportion of women represented in this study coincides with the time that most women begin screening (age 40–49), and within this study population, the data reflect a large proportion of women who are highly educated with a high income (two variables that tend to coincide with one another). Additionally, for median household income, rurality, population diversity index, dollars spent on public transportation and median travel time to work, we used population-level data from the US Census as individual-level data were not available, which may lead to ecological fallacy. Finally, this study is descriptive in nature and focuses on univariate relationships. Indeed, many of the demographic factors investigated are likely correlated with geographic location/rurality.
Two strengths of this paper are the availability of utilization data, and improved accuracy of using geocoded street level addresses for both women’s residences and breast imaging facility locations to calculate travel times. To our knowledge, no other health services research study has been able to achieve this level of detail in travel time analysis to examine utilization patterns either in the United States or globally. Additional strengths of the study are the large sample size, as well as the rich information about characteristics of women, facilities, and the environment.
As a final point, this study does not examine clinical factors that might alter the relationship between proximity and utilization. For instance, for women with a cancer diagnosis, proximity may be an essential consideration due to frequency of visits or intensity of subsequent treatment regimens. This could change the relationship between patient and facility characteristics and differential drive time. This remains an opportunity to expand on the current understanding of the underlying factors that affect mammography utilization.
Conclusion
Unlike previous travel time studies, this analysis is able to examine geographic access patterns using both patient level and breast imaging facility level street addresses and then compare the common closest facility assumption against actual utilization patterns. We found that a large proportion of our US based sample that didn’t use the closest facility, roughly three-quarters, accessed care at a facility within 5 min of their closest facility, suggesting that use of the closest facility may not introduce substantial error for studies of geographically abundant services in areas where the transportation network is well established. Therefore, the use of the closest facility as a proxy to summarize geographic access appears to be appropriate for certain population sub-groups. Where populations are by-passing the closest facility, it appears that individuals tend to live in an urban core, or may have greater income, or include areas where the travel time to work might be longer. Additional research is needed to investigate whether similar relationships hold in the context of other health care services outside of the United States, particularly those that are not as geographically dense or where populations access healthcare facilities by other transportation means such as walking, riding a bike or by public transit.
Authors’ contributions
All authors have read and approved the manuscript, and each author has participated sufficiently in, and stands by, the validity of this work. JA, MA, MPH designed the study, directed its implementation, drafted the manuscript, and gave final approval for the submission. JML, Ph.D. prepared the analytic files, assisted with the manuscript draft and reviewed the final content for submission. RAH, Ph.D., assisted with the design and analysis as well as assisted with the manuscript draft and reviewed the final content for submission. CIL MD, MSHS, provided analysis, assisted with the manuscript draft and review the final content for submission JSH, MD provided analysis, assisted with the manuscript draft and review the final content for submission. XS, Ph.D., provided analysis and reviewed the manuscript. HAC, MS prepared analytic files, assisted with the manuscript draft and review the final content for submission. LH, Ph.D. provided analysis, assisted with the manuscript draft and reviewed the final content for submission. DH, Ph.D. provided analysis, assisted with the manuscript draft and review the final content for submission. ANAT, ScD, provided manuscript review. TO, MS, Ph.D., designed the study, oversaw the implementation and reviewed the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We thank the participating women, mammography facilities, and radiologists for the data they have provided for this study. A list of the BCSC investigators and procedures for requesting BCSC data for research purposes are provided at: http://breastscreening.cancer.gov/. The collection of cancer and vital status data used in this study was supported in part by several state public health departments and cancer registries throughout the US. For a full description of these sources, please see: http://breastscreening.cancer.gov/work/acknowledgement.html. Data collection for this work was supported by the National Cancer Institute-funded Breast Cancer Surveillance Consortium (HHSN261201100031C). Additional support for this work has been funded by the BCSC P01 project (P01CA154292). We thank the Norris Cotton Cancer Center’s GeoSpatial Resource: http://cancer.dartmouth.edu/res/geospatial.html.
Competing interests
The authors declare that they have no competing interests.
Contributor Information
Jennifer Alford-Teaster, Email: jennifer.a.alford-teaster@dartmouth.edu.
Jane M. Lange, Email: lange.j@ghc.org
Rebecca A. Hubbard, Email: rhubb@mail.med.upenn.edu
Christoph I. Lee, Email: stophlee@uw.edu
Jennifer S. Haas, Email: jhaas@partners.org
Xun Shi, Email: Xun.Shi@dartmouth.edu.
Heather A. Carlos, Email: Heather.A.Carlos@dartmouth.edu
Louise Henderson, Email: louise_henderson@med.unc.edu.
Deirdre Hill, Email: dahill@salud.unm.edu.
Anna N. A. Tosteson, Email: Anna.N.A.Tosteson@dartmouth.edu
Tracy Onega, Email: Tracy.L.Onega@dartmouth.edu.
References
- 1.Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136:161–171. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- 2.Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19(2):69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- 3.Apparicio P, Abdelmajid M, Riva M, Shearmur R. Comparing alternative approaches to measuring the geographical accessibility of urban health services: distance types and aggregation-error issues. Int J Health Geogr. 2008;7:7. doi: 10.1186/1476-072X-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schuurman N, Fiedler RS, Grzybowski SC, Grund D. Defining rational hospital catchments for non-urban areas based on travel-time. Int J Health Geogr. 2006;5:43. doi: 10.1186/1476-072X-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jin C, Cheng J, Lu Y, Huang Z, Cao F. Spatial inequity in access to healthcare facilities at a county level in a developing country: a case study of Deqing County, Zhejiang, China. Int J Equity Health. 2015;14(1):67. doi: 10.1186/s12939-015-0195-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang DH, Goerge R, Mullner R. Comparing GIS-based methods of measuring spatial accessibility to health services. J Med Syst. 2006;30(1):23–32. doi: 10.1007/s10916-006-7400-5. [DOI] [PubMed] [Google Scholar]
- 7.Lian M, Struthers J, Schootman M. Comparing GIS-based measures in access to mammography and their validity in predicting neighborhood risk of late-stage breast cancer. PLoS One. 2012;7(8):e43000. doi: 10.1371/journal.pone.0043000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahman S, Price JH, Dignan M, Rahman S, Lindquist PS, Jordan TR. Access to mammography facilities and detection of breast cancer by screening mammography: a GIS approach. Int J Cancer Prev. 2009;2(6):403–413. [PMC free article] [PubMed] [Google Scholar]
- 9.Nesbitt RC, Gabrysch S, Laub A, et al. Methods to measure potential spatial access to delivery care in low- and middle-income countries: a case study in rural Ghana. Int J Health Geogr. 2014;13:25. doi: 10.1186/1476-072X-13-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Delamater PL, Messina JP, Shortridge AM, Grady SC. Measuring geographic access to health care: raster and network-based methods. Int J Health Geogr. 2012;11(1):15. doi: 10.1186/1476-072X-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salze P, Banos A, Oppert JM, et al. Estimating spatial accessibility to facilities on the regional scale: an extended commuting-based interaction potential model. Int J Health Geogr. 2011;10:2. doi: 10.1186/1476-072X-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan-Gates JA, Ersek JL, Eberth JM, Adams SA, Pruitt SL. Geographic access to mammography and its relationship to breast cancer screening and stage at diagnosis: a systematic review. Women’s Health Issues. 2015;25(5):482–493. doi: 10.1016/j.whi.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boscoe FP, Johnson CJ, Henry KA, et al. Geographic proximity to treatment for early stage breast cancer and likelihood of mastectomy. Breast (Edinburgh, Scotland) 2011;20(4):324–328. doi: 10.1016/j.breast.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Celaya MO, Berke EM, Onega TL, et al. Breast cancer stage at diagnosis and geographic access to mammography screening (New Hampshire, 1998–2004) Rural Remote Health. 2010;10(2):1361. [PMC free article] [PubMed] [Google Scholar]
- 15.Elkin EB, Ishill NM, Snow JG, et al. Geographic access and the use of screening mammography. Med Care. 2010;48(4):349–356. doi: 10.1097/MLR.0b013e3181ca3ecb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gomez D, Haas B, Doumouras AG, et al. A population-based analysis of the discrepancy between potential and realized access to trauma center care. Ann Surg. 2013;257(1):160–165. doi: 10.1097/SLA.0b013e31827b9649. [DOI] [PubMed] [Google Scholar]
- 17.Loh CPA, Cobb SC, Johnson CK. Potential and actual accessibility to hospital and hospital services in Northeast Florida. Southeast Geogr. 2009;49(2):171–184. doi: 10.1353/sgo.0.0043. [DOI] [Google Scholar]
- 18.Luo W, Whippo T. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place. 2012;18(4):789–795. doi: 10.1016/j.healthplace.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 19.Onega T, Cook A, Kirlin B, et al. The influence of travel time on breast cancer characteristics, receipt of primary therapy, and surveillance mammography. Breast Cancer Res Treat. 2011;129(1):269–275. doi: 10.1007/s10549-011-1549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D. Geographic access to cancer care in the U.S. Cancer. 2008;112(4):909–918. doi: 10.1002/cncr.23229. [DOI] [PubMed] [Google Scholar]
- 21.Onega T, Hubbard R, Hill D, et al. Geographic access to breast imaging for US women. J Am Coll Radiol. 2014;11(9):874–882. doi: 10.1016/j.jacr.2014.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Onitilo AA, Liang H, Stankowski RV, et al. Geographical and seasonal barriers to mammography services and breast cancer stage at diagnosis. Rural Remote Health. 2014;14(3):2738. [PubMed] [Google Scholar]
- 23.Peipins LA, Graham S, Young R, et al. Time and distance barriers to mammography facilities in the Atlanta metropolitan area. J Community Health. 2011;36(4):675–683. doi: 10.1007/s10900-011-9359-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peipins LA, Miller J, Richards TB, et al. Characteristics of US counties with no mammography capacity. J Community Health. 2012;37(6):1239–1248. doi: 10.1007/s10900-012-9562-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shi X, Alford-Teaster J, Onega T, Wang D. Spatial access and local demand for major cancer care facilities in the United States. Ann Assoc Am Geogr. 2012;102(5):1125–1134. doi: 10.1080/00045608.2012.657498. [DOI] [Google Scholar]
- 26.Tarlov E, Zenk SN, Campbell RT, Warnecke RB, Block R. Characteristics of mammography facility locations and stage of breast cancer at diagnosis in Chicago. J Urban Health. 2009;86(2):196–213. doi: 10.1007/s11524-008-9320-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Towne SD, Jr, Smith ML, Ory MG. Geographic variations in access and utilization of cancer screening services: examining disparities among American Indian and Alaska Native Elders. Int J Health Geogr. 2014;13:18. doi: 10.1186/1476-072X-13-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wasserman M, Meersman S, Rakowski W, Clark MA. Distance and mammogram utilization among unmarried middle-aged and older women. New York, NY: Population Association of America; 2007. [Google Scholar]
- 29.Gunderson CC, Nugent EK, McMeekin DS, Moore KN. Distance traveled for treatment of cervical cancer: who travels the farthest, and does it impact outcome? Int J Gynecol Cancer. 2013;23(6):1099–1103. doi: 10.1097/IGC.0b013e3182989464. [DOI] [PubMed] [Google Scholar]
- 30.Jones AP, Haynes R, Sauerzapf V, Crawford SM, Zhao H, Forman D. Travel times to health care and survival from cancers in Northern England. Eur J Cancer. 2008;44(2):269–274. doi: 10.1016/j.ejca.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 31.Berke EM, Shi X. Computing travel time when the exact address is unknown: a comparison of point and polygon ZIP code approximation methods. Int J Health Geogr. 2009;8:23. doi: 10.1186/1476-072X-8-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huerta Munoz U, Kallestal C. Geographical accessibility and spatial coverage modeling of the primary health care network in the Western Province of Rwanda. Int J Health Geogr. 2012;11:40. doi: 10.1186/1476-072X-11-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang B, Dignan M, Han D, Johnson O. Does distance matter? Distance to mammography facilities and stage at diagnosis of breast cancer in Kentucky. J Rural Health. 2009;25(4):366–371. doi: 10.1111/j.1748-0361.2009.00245.x. [DOI] [PubMed] [Google Scholar]
- 34.Goldman LE, Walker R, Hubbard R, Kerlikowske K. Timeliness of abnormal screening and diagnostic mammography follow-up at facilities serving vulnerable women. Med Care. 2013;51(4):307–314. doi: 10.1097/MLR.0b013e318280f04c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kempe KL, Larson RS, Shetterley S, Wilkinson A. Breast cancer screening in an insured population: whom are we missing? Perm J. 2013;17(1):38–44. doi: 10.7812/TPP/12-068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Henry KA, Boscoe FP, Johnson CJ, Goldberg DW, Sherman R, Cockburn M. Breast cancer stage at diagnosis: is travel time important? J Community Health. 2011;36(6):933–942. doi: 10.1007/s10900-011-9392-4. [DOI] [PubMed] [Google Scholar]
- 37.NCI. Breast Cancer Surveillance Consortium (BCSC). 2014. http://breastscreening.cancer.gov/. Accessed 3 Nov 2014.
- 38.ESRI. Business analyst. 2014. http://www.esri.com/software/businessanalyst. Accessed 5 Nov 14.
- 39.ESRI. Demographic, consumer and business data metholodolgy statements. 2010/2014. 2015. http://www.esri.com/data/esri_data/methodology-statements. Accessed 28 Jan 2015.
- 40.FDA. Mammography facilities. 2014. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfMQSA/mqsa.cfm. Accessed 28 Nov 2012, 29 Nov 2012, 10 Jan 2013, 16 Jan 2013, 18 March 2013, 2012–2013.
- 41.Team RC. R: a language and environment for statistical computing. 2014. http://www.R-project.org/.
- 42.De Klerk NH, English DR, Armstrong BK. A review of the effects of random measurement error on relative risk estimates in epidemiological studies. Int J Epidemiol. 1989;18(3):705–712. doi: 10.1093/ije/18.3.705. [DOI] [PubMed] [Google Scholar]


