Abstract
PURPOSE
Quadriceps activation failure is considered to contribute to the weakness that lingers following anterior cruciate ligament (ACL) reconstruction. Importantly, the impact of pre-operative quadriceps activation on post-operative quadriceps function is unknown. Understanding this relationship is clinically important; as the counteractive approach clinicians should employ pre-operatively to mitigate post-operative quadriceps weakness is unclear. Accordingly, the primary purpose of this study was to investigate the relationship between pre-operative quadriceps activation and post-operative quadriceps strength and activation.
METHODS
Fifty-four individuals post-ACL injury reported for testing on two occasions: prior-to-surgery and post-surgery once they returned to activity. Quadriceps activation was assessed using the burst superimposition technique and quantified using the central activation ratio. Quadriceps strength was assessed using isometric contractions that were performed at 90° of knee flexion. Multiple linear regressions were utilized to detect the relationships between pre-operative activation and strength and post-operative activation and strength.
RESULTS
Pre-operative activation was not associated with post-operative strength (R2=0.064, P=0.186). Pre-operative quadriceps activation and strength were associated with post-operative activation (R2=0.383, P≤0.001) and strength (R2=0.465, P≤0.001), respectively.
CONCLUSIONS
Individuals with better pre-operative quadriceps activation demonstrated greater post-operative activation. Similarly, individuals with better pre-operative strength demonstrated better post-operative strength. Pre-operative quadriceps activation was not a predictor of post-operative strength. From a clinical perspective, our work indicates that clinicians should utilize therapies targeting both quadriceps activation and strength prior to ACL-reconstruction in order to maximize these factors post-ACL reconstruction, as pre-operative activation and strength are related to post-operative activation and strength, respectively at return-to-activity.
Keywords: central activation ratio, ACL, arthrogenic inhibition, muscle inhibition, muscle
INTRODUCTION
The restoration of quadriceps strength following anterior cruciate ligament (ACL) reconstruction is an essential component of rehabilitation. Although clinicians and researchers continue to make strides towards improving ACL rehabilitation protocols, patients often return to activity with diminished quadriceps strength [27]. Lingering quadriceps weakness is linked to reduced physical function [31,20] and quality of life [22], is thought to increase the risk of re-injury [31,28], and contributes to the development and progression of post-traumatic osteoarthritis [36]. Given that the failure to restore quadriceps strength has deleterious consequences to the knee, it is critical to develop rehabilitative approaches capable of maximizing quadriceps strength deficits following ACL reconstruction.
Quadriceps activation failure (QAF), the inability to completely contract the quadriceps muscle due to altered neural signaling [13,9], has been identified as a mechanism contributing to the lingering strength deficits following ACL reconstruction [25]. The changes in neural signaling associated with QAF reduce alpha motoneuron recruitment and/or firing rate, allowing only portions of the quadriceps to be volitionally utilized during exercise [13]. Clinically, rehabilitation professionals see QAF manifest as quadriceps weakness [9]. Although QAF is believed to be a natural response designed to protect the knee joint from further damage [13], persistent QAF impedes the inability to achieve complete muscle activation during strength training and creates a barrier to successful rehabilitation [14,30].
Prior investigations have found a link between pre- and post-operative quadriceps strength and function, demonstrating greater strength and function pre-operatively leads to better outcomes post-operatively [7,32,5,21]. Given that quadriceps strength, is in part dependent on volitional muscle activation [34], it seems plausible that better pre-operative quadriceps activation may also contribute to better quadriceps function at a time when individuals return to activity following ACL reconstruction. Understanding the relationship between pre-and post-operative quadriceps activation and strength is clinically important, as the counteractive approach clinicians should employ pre-operatively to mitigate post-operative quadriceps weakness is unclear and no investigation has systematically evaluated this relationship. As such, examining the impact of pre-operative quadriceps activation on post-operative quadriceps function will help to identify if restoring quadriceps activation should be a focus of pre-operative rehabilitation. Simply put, this investigation is needed, as it can help to justify if clinicians should focus on delivering pre-operative therapies that aim to remove or reverse QAF.
Thus, in order to direct care and improve rehabilitative techniques, the primary purpose of this investigation was to examine if pre-operative quadriceps activation was related to the level of post-operative activation and strength at a time when individuals were returned-to-activity following ACL reconstruction. Our primary hypothesis was that pre-operative quadriceps activation would be positiviely related to post-operative quadriceps strength and activation, wherein individuals with greater levels of quadriceps activation prior to surgery would return to sport with greater levels of quadriceps activation and strength. Furthermore, consistent with the current literature, we anticipated that strength prior to ACL reconstruction would be positively related to post-operative quadriceps strength. To help provide baseline context of the relationship between QAF and quadriceps strength at the pre- and post-operative time points, we included the contralateral, non-injured limb in this analysis. Though there are inherent issues with utilizing the contralateral limb as control post-ACL injury, as potential contralateral quadriceps strength deficits have been reported [11], using the contralateral limb as a control is a commonly employed and a clinically acceptable technique [19,23,33,3].
MATERIALS AND METHODS
Fifty-four individuals scheduled for ACL reconstruction with a bone-patellar-tendon-bone graft were invited to participate in this study (Table 1). Potential participants were excluded if they: had a previous history of surgery to either knee, suffered a previous ACL injury, or had a known heart condition. Pregnant females were also excluded. Surgical reports were obtained to report any concomitant meniscal damage that required surgical intervention (Table 1). Informed consent was obtained from all subjects and approved by the University’s Institutional Review Board prior to testing.
Table 1.
Participant Demographics (mean±SD)
| Participants | Sex | Age (yrs) | Height (m) | Mass (kg) | Time to Test (months) | Meniscal Surgery | Self-reported Function | ||
|---|---|---|---|---|---|---|---|---|---|
| Pre-operative: Post-injury | Post-operative: Post-surgery | Pre-operative | Post-operative | ||||||
| N=54 | Female=31 | 19.9±5.1 | 1.70±0.3 | 75.9±16.5 | 2.23±2.1 | 7.24±1.1 | ACL-only=33 | Tegner=3.0 (median)±1.3 | Tegner=6.0 (median)±1.9 |
| Male=23 | (range:14–38) | (range:0.5–10.4) | (range:5.2–11.7) | Repair=14 | (range:0–6) | (range:2–10) | |||
| Meniscectomy=7 | IKDC=57.6±15.6* | IKDC=80.4±11.1* | |||||||
| (range:11.5–87.4) | (range:50.6–98.9) | ||||||||
Abbreviations: IKDC, International Knee Documentation Committee Form
P≤0.001 as compared to pre-operative
The details of the post-operative rehabilitation protocol can be found in Appendix 1. All participants completed standard post-operative rehabilitation at one orthopedic outpatient clinic. The rehabilitation protocol consisted of two to three physical therapy appointments per week beginning during the first post-operative week and concluding approximately seven months-post surgery. The program emphasized full knee extension range of motion immediately and knee flexion as tolerated, progression of functional exercises, quadriceps re-education and muscle strengthening. Variation between rehabilitation protocols existed based on concomitant meniscal surgery, age and individual’s response to treatment.
Overview of Testing Scheme
All participants were tested on two separate occasions: post-ACL injury but prior to ACL-reconstruction, and post-ACL reconstruction once patients had been cleared by their orthopedic surgeon to return back to activity (i.e. competitive sport, recreational sport, or activities of daily living, Table 1). To be cleared for activity all participants were required to complete a basic three-week agility program and a leg press test (Appendix 2). If a patient was unable to successfully pass the leg press test, or did not complete the agility program, their clearance for participation was delayed until both of these criteria were met. No other objective return-to-activity criterion is used at this clinic. At each testing session, measurements of QAF and quadriceps strength were assessed in both the ACL injured/reconstructed limb and the contralateral limb. In addition to these measures of quadriceps function, participant’s self-reported function was quantified at the pre- and post-operative time point using the Tegner [1] and International Knee Documentation Committee Form (IKDC)[12] (Table 1). The Tegner and IKDC forms are two widely used questionnaires among researchers and clinicians that are capable of measuring patient reported outcomes of knee function with good reliability and validity (IKDC, r=0.47–0.66, ICC=0.92–0.95[15]; Tegner, r=0.46[1], ICC=0.90–0.97[35]).
Quadriceps Strength and QAF Measurement
To assess quadriceps strength, patients were positioned with their hips flexed to 90°, their back supported, and their testing leg and torso securely strapped into an isokinetic dynamometer (Biodex System 3, Biodex Medical Systems, Shirley, NY, USA). At each testing session, participants were asked to perform maximal voluntary isometric contractions (MVICs) with the testing knee flexed to 90°. There was no limit to the number of MVIC trials a participant could perform, but contractions were ceased when an improvement in torque was no longer evident. This procedure helped to ensure that each participant’s MVIC was achieved and has been used by others [26]. The maximal knee extension torque produced across trials was normalized to body weight and used for statistical analysis. Participants were allowed sufficient rest time between contractions and measures to ensure an accurate assessment of torque.
To quantify quadriceps activation the superimposed burst technique was utilized [17], wherein the peak torque recorded from the MVIC trials was inputted into a custom written program (LabVIEW version 8.5, National Instruments, Austin, TX, USA) set to deliver a supramaximal electrical stimulus (100 pulses/sec, 600μsec pulse duration, 10 pulse train, 130 V) to the quadriceps muscle once the maximal knee extension torque had been reached and then subsequently dropped by one Nm [26]. The electrical stimulus was delivered through two self-adhesive stimulating electrodes (Dura-Stick II [7 × 13cm] Chattanooga Group, Hixson, TN, USA) applied over the vastus lateralis muscle proximally and the vastus medialis distally using a Grass S88 Dual Output Square Pulse Stimulator (S88, Grass Technologies, West Warick, RI, USA) with an SIU8T Transformer Stimulus Isolation Unit (SIU8T, Grass Technologies, West Warick, RI, USA) attached. Volitional activation of the quadriceps was quantified using the central activation ratio (CAR) formula (Equation 1) wherein, the subject’s peak torque generated immediately prior to the delivery of the stimulus was divided by the peak torque generated as a result of the electrical stimulus and multiplied by 100. A CAR of 100 was used to represent complete quadriceps activation [16]. CAR values that were ≥ 90 were considered to be ‘normal’ and/or representative of a healthy CAR value [17] [29]. The maximal CAR value (i.e. trial that displayed the least amount of QAF) that was collected was used for statistical analysis.
| Equation 1 |
This investigation was approved by the University of Michigan IRBMED (Approval # HUM00016184). Prior to testing, all participants provided written informed consent.
Statistical Analysis
Sample size was estimated using an a priori power analysis based on previous work examining the ability of pre-operative quadriceps strength to predict post-operative quadriceps strength [24]. In order to detect associations with a α-level of 0.05 and the 1-β 0.80, it was determined that 37 participants would be needed for this investigation.
Multiple linear regressions in both the ACL and contralateral limb were utilized to examine the relationships between 1) pre-operative activation and post-operative isometric strength, 2) pre-operative activation and post-operative activation and 3) pre- and post-operative isometric strength. All linear regression models met the assumptions of linearity, normality, independence and homogeneity of variance. Due to inclusion of participants with concomitant meniscus injury and subsequent repair, meniscal surgery was entered as a covariate in each of the regression models to detect if additional surgical procedures had an affect on these relationships. To measure the recovery of quadriceps strength in the ACL limb, the quadriceps index (Equation 2)[19] was utilized to quantify isometric strength deficits at the pre-and post-operative time point in the ACL limb as compared to the contralateral limb. Paired t-tests were then utilized to detect the difference between pre-and post-operative quadriceps activation, strength in the ACL limb, contralateral limb as well as the quadriceps index. Additionally, paired t-tests were utilized to detect differences in patient self-reported function at the pre- and post-operative time points. The α-level was set a priori at P≤0.05. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software version 21.0 (IBM Corp., Armonk, NY, USA).
| Equation 2 |
RESULTS
Pre-operative Quadriceps Activation and Post-operative Quadriceps Strength
Pre-operative quadriceps activation was not related to post-operative quadriceps strength in the ACL limb (R2=0.064, P=n.s [bQAF=0.230, PQAF=n.s., bMeniscus=0.110, PMeniscus=n.s.] Figure 1A). Pre-operative quadriceps activation was positively related to post-operative isometric strength in the contralateral limb (R2=0.134, P=0.026 [bQAF=0.324, PQAF=0.016, bMeniscus=0.175, PMeniscus=n.s.] Figure 1B).
Figure 1.
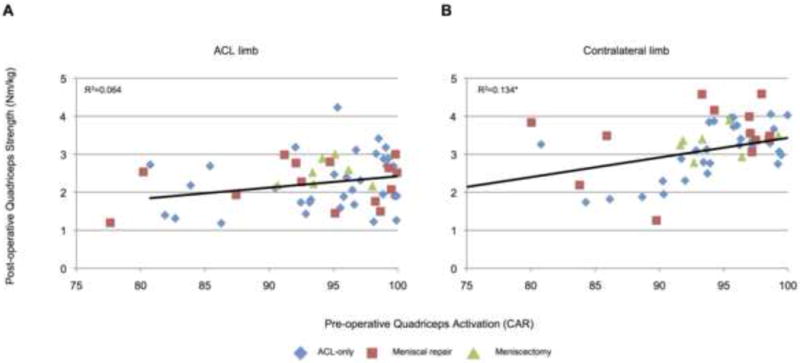
Pre-operative quadriceps activation plotted against post-operative quadriceps strength. Pre-operative quadriceps activation was positively related to post-operative quadriceps strength in the contralateral (B, *P=0.026), but not ACL limb (A, P=0.064).
Pre-and Post-operative Quadriceps Activation
Pre-operative quadriceps activation was positively associated with post-operative activation in the ACL (R2=0.383, P≤0.001 [bQAF=0.612, PQAF≤0.001, bMeniscus=0.102, PMeniscus=n.s.] Figure 2A) and contralateral limbs (R2=0.202, P≡0.003 [bQAF=0.444, PQAF≡0.001, bMeniscus=−0.056, PMeniscus=n.s.] Figure 2B). Further, it was found that participants demonstrated greater QAF (smaller CARs) in the ACL limb after reconstruction compared to the pre-operative time point (t53=5.283, P≤0.001, Table 2). No difference in quadriceps activation was found in the contralateral limb between time points (t53=0.446, P=n.s., Table 2).
Figure 2.
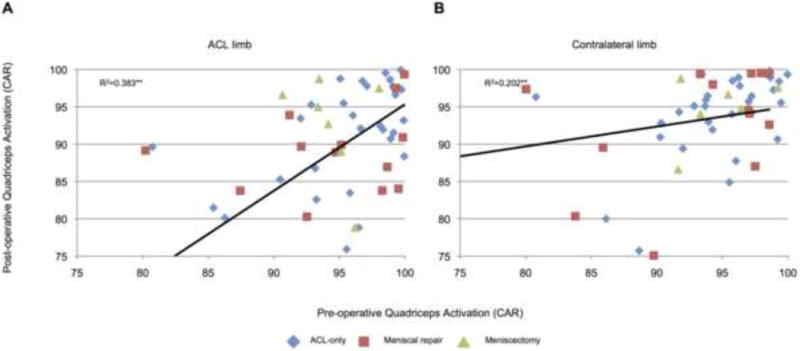
Pre-operative quadriceps activation plotted against post-operative quadriceps activation. Pre-operative quadriceps activation was positively related to post-operative quadriceps activation in the ACL (A, P≤0.001,) and contralateral limb (B, P≤0.001).
Table 2.
Quadriceps Activation, Strength and Index (mean±SD)
| Measure | ACL limb | Contralateral limb | – | ||
|---|---|---|---|---|---|
| Activation (CAR) | Strength (Nm/kg) | Activation (CAR) | Strength (Nm/kg) | Quadriceps Index | |
| Pre-operative | 94.0±5.8 | 2.5±0.7 | 93.2±6.5 | 3.1±0.7 | 83.8±14.8 |
| Post-operative | 88.8±9.1** | 2.2±0.6* | 92.7±7.3 | 3.2±5.8 | 72.2±18.5** |
Abbreviations: CAR; central activation ratio
P=0.001 as compared to pre-operative
P≤0.001 as compared to pre-operative
Pre-and Post-operative Quadriceps Strength
Quadriceps isometric strength prior to ACL reconstruction was positively related to post-operative strength in the ACL (R2=0.465, P≤0.001 [bStrength=0.661, PStrength≤0.001, bMeniscus=0.147, PMeniscus=n.s.] Figure 3A) and contralateral limb (R2=0.650, P≤0.001 [bStrength=0.781, PStrength≤0.001, bMeniscus=0.123, PMeniscus=n.s.] Figure 3B). It was also found that participants demonstrated significantly less quadriceps isometric strength (t53=3.422, P=0.001) and a lower quadriceps index (t53=4.091, P≤0.001, Table 2) at the post-operative time point as compared to pre-operative time point. No difference in quadriceps strength was found in the contralateral limb between time points (t53=−1.478, P=n.s., Table 2).
Figure 3.
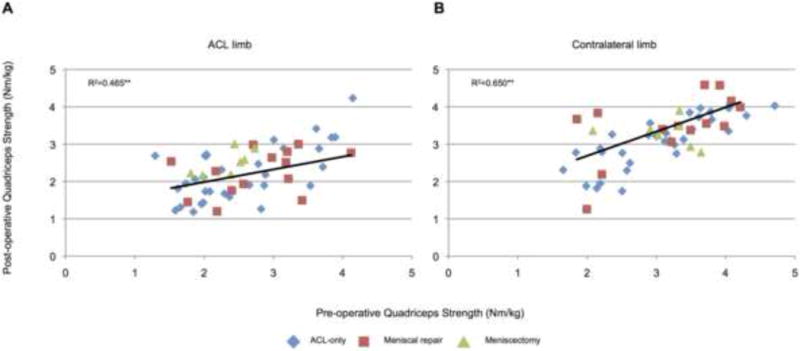
Pre-operative quadriceps strength plotted against post-operative quadriceps strength. Pre-operative quadriceps strength was positively related to post-operative quadriceps strength in the ACL (A, P≤0.001,) and contralateral limb (B, P≤0.001).
Self-reported Function
Self-reported function was found to be significantly greater post-ACL reconstruction at a time when individuals were returned to activity than prior to surgery (Tegner: t53=−10.689, P≤0.001; IKDC: t53=−9.744, P≤0.001; Table 1).
DISCUSSION
The primary purpose of this investigation was to examine the relationship between pre-operative quadriceps QAF and post-operative quadriceps activation and strength following ACL reconstruction. Investigating the relationship between quadriceps activation and strength could help to advance pre-operative rehabilitation protocols by identifying modifiable factors of quadriceps function that can be treated prior to surgery that improve post-operative outcomes. The most important finding of this present study was that greater pre-operative quadriceps activation and strength are moderately [4], and positively, related to greater post-operative quadriceps activation and strength in both the affected and unaffected limbs. Quadriceps activation in the ACL limb prior to surgery was not related to post-operative strength. Simply put, individuals with greater quadriceps activation and strength prior to surgery demonstrated greater levels of quadriceps function at return-to-activity, which clinically indicates that treatments that can reduce pre-operative quadriceps dysfunction should be employed to improve post-operative outcomes.
Relationship between Pre-operative Quadriceps Activation and Post-operative Quadriceps Strength
Pre-operative quadriceps activation was positively related to post-operative strength in the contralateral (Figure 1B), but not the ACL limb (Figure 1A). This result in the contralateral limb was expected given that volitional muscle activation has been found to be related to strength in healthy individuals [34], and examining this result across time points should not change this relationship. This finding in the ACL reconstructed limb was unexpected, as previous research has established that quadriceps activation is related to strength in ACL deficient individuals [38,3,23]. As such, we had anticipated that greater levels of pre-operative quadriceps activation would be positively associated with post-operative strength in both the ACL and contralateral limb. It is possible that the failure to establish a relationship in the ACL limb between pre-operative activation and post-operative strength resulted from a change in mediators of QAF from the pre-operative to post-operative time point. The current literature indicates that several triggers of QAF, such as pain, effusion, or altered afferent input from the damaged ACL, are likely present and contribute in combination to strength deficits following ACL injury and reconstruction [9,30,25]. Moreover, the central mechanisms that may mediate QAF such as descending cortical inhibition, pre-synaptic inhibition, Ib inhibition, and/or recurrent inhibition may have also varied between the two time points. Hence, it is possible that pre-operative QAF may be triggered and mediated by different factors than post-operative QAF, which may have affected strength differently at each time point and limited the potential relationship between pre-operative QAF and post-operative isometric strength. Further complicating this relationship is the trauma induced by surgical reconstruction of the ligament as well as concomitant injury / subsequent repair, which may increase the magnitude of QAF from the pre- to post-operative time point [7]. Given that our participants demonstrated significantly more QAF post-operatively compared to pre-operative (Table 2), our data supports this theory that surgery may induce a higher level of QAF. Unfortunately, though our measure of QAF (superimposed burst) was able to detect a change in volitional muscle activation due to a reduction in motor unit recruitment and/or firing rate [16], the SIB measure does not specifically identify the mechanisms of QAF at work in the ACL injured/reconstructed limb. Furthermore, because the CAR is measured during maximal muscle contractions, this approach only estimates activation under complete maximal effort, although it is widely accepted and commonly employed post-reconstruction [17,9]. Given that 100% of muscle activation has not been found to be physiologically possible [8], supplementing this measure with a variety of neural tests that can assess varying degrees of volitional effort (rest, sub maximal and maximal) that may be more related to functions of daily activity seems to be justified. To accomplish this, and provide more comprehensive neural testing, investigators may choose to use measurement techniques such as the Hoffmann reflex, V-wave, interpolated twitch, and/or transcranial magnetic stimulation. Ultimately it is important to note that quadriceps activation and strength can be affected by a variety of factors, and at this point in time, it is unknown what triggers and mechanism(s) contribute to QAF in ACL deficient and reconstruction patients.
Relationship between Pre-operative Quadriceps Activation and Post-operative Quadriceps Activation
Previous investigations have found that patients with greater pre-operative quadriceps strength have greater strength post-operatively [5,7,32], but our work is the first to examine the relationship between pre- and post-operative activation. As quadriceps activation is an estimate of motorneuron pool excitability and is therefore thought to represent the proportion of the muscle that one is capable of voluntarily contracting, we had expected to find that having a greater portion of the muscle available prior to surgery would be beneficial for post-operative quadriceps activation (Figure 2). This result indicates that quadriceps activation prior to surgery is an important component of quadriceps function at return-to-activity, and in part, justifies clinical rationale as to why mitigating pre-operative QAF is important to post-operative outcomes. The difficulty with this finding is that our results seem to indicate that ACL surgery induces a greater level of QAF than ACL injury itself (Table 2). This finding raises the question of how effective pre-operative treatments can be if the greatest amount of QAF is induced post-surgery. This question remains unanswered and requires more research. Furthermore, although we know post-operative QAF impedes strength gains [14,13], it is unknown what impact QAF has on other clinically meaningful functional outcomes such as knee mechanics and performance based measures. Though previous investigators have shown that alterations in quadriceps electromyographic activity post-ACL reconstruction are related to functional activities such as gait [2], the link between QAF and function is less clear. Given this gap in the literature, future work should focus on the affect that post-operative quadriceps activation has on more functional outcomes (e.g. other than strength) to study to what extent alterations in volitional muscle activation affect clinically relevant measures of function.
Relationship between Pre-operative Quadriceps Strength and Post-operative Quadriceps Strength
Our results indicate that pre-operative quadriceps isometric strength was positively related to the recovery of post-operative strength (Figure 3A). This finding is in agreement with previous work by Eitzen et al. [7], Shelbourne and Johnson [32], and de Jong et al. [5]. These investigators utilized isokinetic strength measures at 60°/second [7,5] and 180°/second [32,5] and found that individuals with better pre-operative quadriceps strength demonstrated greater post-operative quadriceps strength [7,5,32], better performance during hoping tasks [7,5], and higher levels of self-reported function [7]. Thus, individuals with greater strength post-ACL injury, but prior to ACL-reconstruction, may not experience as much early post-operative muscle weakness and may be able to regain strength better in the ACL limb than those with less pre-operative strength.
Notably it was found that our patients had substantial strength deficits at the post-operative time point as compared to pre-operative (Table 2). The current literature recommends that individuals are returned to sport once side-to-side strength deficits (or quadriceps indices) are within ~10%[6] [37,31]. Though these recommendations may seem to be conservative in nature, recent work indicates that strength deficits greater than 10% are associated with alterations in knee mechanics during gait [6] as well as decreased performance during functional tasks [31]. Given that our participants have an average strength deficit of 28% at return to play, it seems reasonable to deduce that this strength imbalance is hazardous to future knee joint function and health. Equally important, this data indicates that the clinical leg press test utilized to clear participants for sport is not sensitive enough to detect clinically meaningful deficits in quadriceps strength. Taken together, these findings further emphasis the need for clinicians and researchers to continue to work to identify therapeutic approaches capable of minimizing post-operative strength deficits and to employ clinical tools such as isokinetic testing at return-to-play that are capable of objectively measuring strength.
Self-Reported Function
Self-reported function quantified via the Tegner and IKDC forms was found to be improved post-ACL reconstruction. This finding was not surprising, given that pre-operative levels of self-reported function are expected to be low. Though self-reported function improved after surgery, again it is important to note, that our subjects had IKDC scores that are below clinical recommendations of 90% (Table 2) [6]. Similar to our strength data, these results seem to indicate that individuals may have benefitted from a longer physical therapy regime, as they have not met clinical recommendations for return-to-sport.
Concomitant Meniscal Surgery
Due to the potential of concomitant injury and additional surgical procedures to cause alterations in quadriceps function, we included concomitant meniscal surgeries as a covariate in our analyses [14] and found that it did not influence our results (Figures 1,2 and 3).
Recommendations for Future Work
Future work would benefit from examining pre-operative rehabilitation techniques/therapies that are capable of positively influencing post-operative quadriceps function. Though previous work has found that interventions incorporating quadriceps strength and perturbation training prior to ACL reconstruction can positively influence post-operative gait as well as quadriceps strength [10], limited information on the effectiveness of pre-operative therapies is available. Given the deleterious consequences of persistent quadriceps weakness [27] and the findings of this investigation as well as others [7,32,5], it seems continued investigation of pre-operative interventions that can target and successfully combat the factors of post-operative quadriceps dysfunction is needed. In addition to these pre-operative rehabilitation considerations, future work would also benefit from examining the role of muscle atrophy. Krishnan and Williams [18] have shown that quadriceps atrophy is a major contributor to weakness following ACL reconstruction and found that in individuals 2–15 years post-ACL reconstruction quadriceps atrophy is a more significant contributor than QAF to post-operative strength deficits. As such, analyzing factors such as alterations in muscle morphology, in addition to the neural and strength measures that were utilized in this investigation would provide a more comprehensive analysis of overall knee joint function post-injury and reconstruction. Furthermore, obtaining serial post-operative measures (e.g. once a month) and tracking post-operative rehabilitation schemes, would allow for a more in-depth analysis of how pre-operative factors affect the magnitude of recovery (or change) and how therapies can positively affect post-operative quadriceps function.
Conclusion
Individuals with better pre-operative quadriceps activation demonstrated greater post-operative activation. Likewise, individuals with better pre-operative strength demonstrated better post-operative strength. Pre-operative quadriceps activation was not a predictor of post-operative strength. Taken together, our work provides an initial first step towards clarifying the effect of pre-operative quadriceps function on post-operative outcomes, and clinically indicates that treatments that can improve quadriceps strength and activation prior to surgery should be employed to improve post-operative quadriceps function at return-to-activity.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under Award Number K08 AR05315201A2 to Dr. Palmieri-Smith. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would like to thank Ms. Meg Strickland BS for her assistance with data processing.
References
- 1.Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The Reliability, Validity, and Responsiveness of the Lysholm Score and Tegner Activity Scale for Anterior Cruciate Ligament Injuries of the Knee 25 Years Later. Am J Sports Med. 2009;37(5):890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 2.Bulgheroni P, Bulgheroni MV, Andrini L, Guffanti P, Giughello A. Gait patterns after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1997;5(1):14–21. doi: 10.1007/s001670050018. [DOI] [PubMed] [Google Scholar]
- 3.Chmielewski TL, Stackhouse S, Axe MJ, Snyder-Mackler L. A prospective analysis of incidence and severity of quadriceps inhibition in a consecutive sample of 100 patients with complete acute anterior cruciate ligament rupture. J Orthop Res. 2004;22(5):925–930. doi: 10.1016/j.orthres.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 4.Cohen J. Statistical Analysis for the Behavioral Sciences. Academic Press; New York: 1977. [Google Scholar]
- 5.de Jong SN, van Caspel DR, van Haeff MJ, Saris DBF. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23(1):21–28. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 6.Di Stasi S, Logerstedt D, Gardinier E, Snyder-Mackler L. Gait Patterns Differ Between ACL-Reconstructed Athletes Who Pass Return-To-Sport Criteria and Those Who Fail. Am J Sports Med. 2013;41(6):1310–1318. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eitzen I, Risberg MA, Holm I. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43(5):371–376. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 8.Gandevia SC, Allen GM, Butler JE, Taylor JL. Supraspinal factors in human muscle fatigue: evidence for suboptimal output from the motor cortex. J Physiol. 1996;490(Pt 2):529–536. doi: 10.1113/jphysiol.1996.sp021164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45(1):87–97. doi: 10.4085/1062-6050-45.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hartigan E, Axe MJ, Snyder-Mackler L. Perturbation training prior to ACL reconstruction improves gait asymmetries in non‚Äêcopers. J Orthop Res. 2009;27(6):724–729. doi: 10.1002/jor.20754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hiemstra LA, Webber S, MacDonald PB, Kriellaars DJ. Contralateral limb strength deficits after anterior cruciate ligament reconstruction using a hamstring tendon graft. Clin Biomech. 2007;22(5):543–550. doi: 10.1016/j.clinbiomech.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R, Cook C. Reliability and validity of the International Knee Documentation Committee (IKDC) subjective knee form. Joint Bone Spine. 2007;74(6):594–599. doi: 10.1016/j.jbspin.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 13.Hopkins JT, Ingersoll CD. Arthrogenic muscle inhibition: A limiting factor in joint rehabiliation. J Sport Rehab. 2000;9:135–159. [Google Scholar]
- 14.Hurley MV, Jones DW, Newham DJ. Arthrogenic quadriceps inhibition and rehabilitation of patients with extensive traumatic knee injuries. Clin Sci (Colch) 1994;86(3):305–310. doi: 10.1042/cs0860305. [DOI] [PubMed] [Google Scholar]
- 15.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelbourne KD. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 16.Kent-Braun JA, Le Blanc R. Quantitation of central activation failure during maximal voluntary contractions in humans. Muscle Nerve. 1996;19(7):861–869. doi: 10.1002/(SICI)1097-4598(199607)19:7<861::AID-MUS8>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 17.Krishnan C, Williams GN. Quantification method affects estimates of voluntary quadriceps activation. Muscle & Nerve. 2010;41(6):868–874. doi: 10.1002/mus.21613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krishnan C, Williams GN. Factors explaining chronic knee extensor strength deficits after ACL reconstruction. J Orthop Res. 2011;29(5):633–640. doi: 10.1002/jor.21316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lephart SM, Kocher MS, Harner CD, Fu FH. Quadriceps strength and functional capacity after anterior cruciate ligament reconstruction. Patellar tendon autograft versus allograft. Am J Sports Med. 1993;21(5):738–743. doi: 10.1177/036354659302100519. [DOI] [PubMed] [Google Scholar]
- 20.Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech. 2002;17(1):56–63. doi: 10.1016/s0268-0033(01)00097-3. [DOI] [PubMed] [Google Scholar]
- 21.Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Pre-operative quadriceps strength predicts IKDC2000 scores 6 months after anterior cruciate ligament reconstruction. The Knee. 2013;(20):208–212. doi: 10.1016/j.knee.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 23.Lynch AD, Logerstedt DS, Axe MJ, Snyder-Mackler L. Quadriceps activation failure after anterior cruciate ligament rupture is not mediated by knee joint effusion. J Orthop Sports Phys Ther. 2012;42(6):502–510. doi: 10.2519/jospt.2012.3793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McHugh MP, Tyler TF, Browne MG, Gleim GW, Nicholas SJ. Electromyographic predictors of residual quadriceps muscle weakness after anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30(3):334–339. doi: 10.1177/03635465020300030601. [DOI] [PubMed] [Google Scholar]
- 25.Palmieri-Smith RM, Thomas AC. A Neuromuscular mechanism of posttraumatic osteoarthritis associated with ACL injury. Exerc Sport Sci Rev. 2009;37(3):147–153. doi: 10.1097/JES.0b013e3181aa6669. [DOI] [PubMed] [Google Scholar]
- 26.Palmieri-Smith RM, Thomas AC, Karvonen-Gutierrez C, Sowers MF. A clinical trial of neuromuscular electrical stimulation in improving quadriceps muscle strength and activation among women with mild and moderate osteoarthritis. Phys Ther. 2010;90(10):1441–1452. doi: 10.2522/ptj.20090330. [DOI] [PubMed] [Google Scholar]
- 27.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27(3):405–424. doi: 10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 28.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pietrosimone BG, Hertel J, Ingersoll CD, Hart JM, Saliba SA. Voluntary quadriceps activation deficits in patients with tibiofemoral osteoarthritis: a meta-analysis. PM&R. 2011;3(2):153–162. doi: 10.1016/j.pmrj.2010.07.485. [DOI] [PubMed] [Google Scholar]
- 30.Rice DA, McNair PJ. Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheu. 2010;40(3):250–266. doi: 10.1016/j.semarthrit.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 31.Schmitt LC, Paterno MV, Hewett TE. The Impact of Quadriceps Femoris Strength Asymmetry on Functional Performance at Return to Sport Following Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shelbourne KD, Johnson BC. Effects of patellar tendon width and preoperative quadriceps strength on strength return after anterior cruciate ligament reconstruction with ipsilateral bone-patellar tendon-bone autograft. Am J Sports Med. 2004;32(6):1474–1478. doi: 10.1177/0363546503262171. [DOI] [PubMed] [Google Scholar]
- 33.Snyder-Mackler L, Delitto A, Bailey SL, Stralka S. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1995;77(8):1167–1173. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Stackhouse SK, Dean JC, Lee SC, Binder-MacLeod SA. Measurement of central activation failure of the quadriceps femoris in healthy adults. Muscle Nerve. 2000;23(11):1706–1712. doi: 10.1002/1097-4598(200011)23:11<1706::aid-mus6>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 35.Tegner Y, Lysolm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 36.Tourville TW, Jarrell KM, Naud S, Slauterbeck JR, Johnson RJ, Beynnon BD. Relationship Between Isokinetic Strength and Tibiofemoral Joint Space Width Changes After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2014;42(2):302–311. doi: 10.1177/0363546513510672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR. Recent advances in the rehabilitation of anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2012;42(3):153–171. doi: 10.2519/jospt.2012.3741. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


