Abstract
Severe dementia is a life-limiting condition; hip fractures are more common in patients who have dementia. This study outlines the case of a 92-year-old female with severe dementia who sustained a hip fracture. Despite having a terminal diagnosis (severe dementia and hip fracture) and poor premorbid quality of life, she had a life-prolonging surgery. The report outlines issues around treatment options in such circumstances, informed consent and substitute decision-making. The authors propose a ‘goals of care’ approach to manage patients in whom the best treatment is unclear, during their attendance to the emergency department. It is suggested that utilization of such a model may help with substitute decision-making and true informed consent.
A 92-year-old woman with dementia presented to the emergency department in pain with a right comminuted pertrochanteric femoral fracture after a fall. She had lived in a nursing home with severe cognitive impairment (mini-mental state examination score of 7/30), double incontinence and deteriorating mobility (increasingly wheelchair-dependent). Her other significant past medical history included insulin-dependent type 2 diabetes mellitus, chronic renal failure (baseline creatinine 100 µmol/l) and poorly controlled hypertension. Her next of kin was her son, who lived in Hong Kong. There were no documented advance care directives or medical powers of attorney recognized by her nursing home.
She had sustained a non-ST-segment elevation myocardial infarction (NSTEMI) in association with the fall (Fig. 1). As a result and given other significant comorbidities, initial anaesthetic review deemed that she had an unstable cardiac risk, with high possibility of intraoperative mortality. The anaesthetic recommendation was for a delay of 24–72 h in operative fixation, in order to allow monitoring and optimization of cardiac status. A palliative care review controlled her pain, via a continuous subcutaneous infusion of fentanyl. Over the next 2 days, she had a transthoracic echocardiogram (which revealed normal left ventricular size and function), an orthogeriatric and further anaesthetic review. She was subsequently deemed fit for surgery, but remained a ‘very high risk for anaesthesia’. The option of continuing non-operative management was not discussed and her son consented for the insertion of a dynamic hip screw. The patient's postoperative recovery was complicated by anaemia and aspiration pneumonia, both of which were successfully treated. Her perioperative symptoms of delirium and pain received ongoing palliative management, facilitating a good recovery by Day 5 of her admission.
Figure 1:
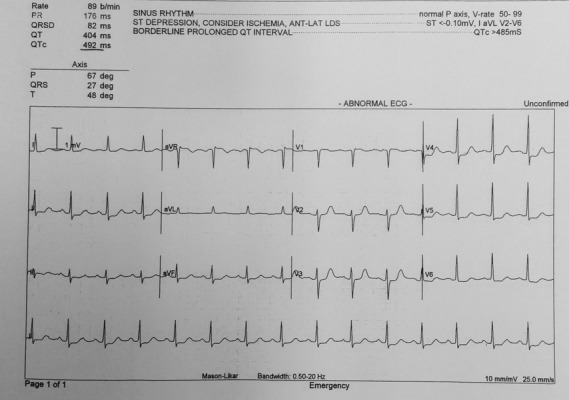
ECG at the time of admission. Note ST depression most prominent in leads V4–6 and II. Initial troponin T 25 ng/l, rising to 214 ng/l on Day 5 (reference range <13 ng/l).
The operative intervention was successful from an analgesic viewpoint. However, she was now bedbound and inappropriate for rehabilitation. She was therefore discharged back to her nursing home, a week after admission. In discussion with her son, he reflected on his decision—aware of his mother's poor premorbid quality of life and her life-prolonging treatment. It was clear that he was struggling with this outcome, but the complexity of his decision was recognized and supported by the palliative care team.
The nurse manager at the facility reported progressive disability, with prominent confusion and agitation subsequent to her return. She remained in the nursing home for 4 months, until her death from complications of her dementia.
DISCUSSION
The World Health Organization describes dementia as a ‘syndrome, usually of a chronic or progressive nature, caused by a variety of brain illnesses that affect memory, thinking, behaviour and ability to perform everyday activities’ [1]. It is estimated that the number of cases of dementia worldwide will more than triple by 2050 [2].
How we manage dementia is important in an ageing population, where prevalence rates increase with age. Hip fractures are more common in the elderly and especially in women, due to osteoporosis [3]. Importantly, recent meta-analyses confirm previous findings that patients with dementia also have a higher risk of hip fractures [4]. Furthermore, following a fracture, patients with dementia are at a higher risk of mortality than those without dementia [5].
How will we manage the growing number of dementia patients with hip fractures? The clinical management will most likely involve a substitute decision maker (SDM), by virtue of the patient's lack of capacity before, during or after an acute deterioration. SDMs often make difficult decisions regarding many aspects of care, but informed choices are important to support and guide this process.
In our case, the timing of the intervention and ensuring the patient was clinically stable was paramount. Mortality benefits of early intervention have previously been demonstrated by a systematic review of the literature in 2008. A delay beyond 48 h after admission was found to increase the odds of 30-day all-cause mortality by 41% and of 1-year all-cause mortality by 32% [6]. Early surgical intervention is therefore beneficial, but is it the only analgesic option for a patient with severe dementia? It is important to note that informed consent should include all appropriate management options, including conservative management [7].
There are sparse data on the non-operative management of hip fractures in medically unfit patients. The 2010 National Hip Fracture Database (NHFD) report outlines that only 3% of patients sustaining a hip fracture are managed non-operatively. The report also advocates palliative management (end-of-life pathway) of patients who present in such poor health that surgery offers no benefit [8]. The authors did not define what constituted ‘such poor health’. McNamara and Sharma examined the question of surgery or palliation for patients with advanced malignancy and a hip fracture. In this study, 53% were bedbound for the majority of the day and overall 48% of fractures were non-malignant. The main reason for non-operative intervention was an anticipated rapid deterioration or death, consistent with the latter stages of dementia. Importantly, the authors found that conservative treatment did not compromise pain control [9].
How can we better guide acute care, given the likelihood of many more similar cases to the one above? We propose that general practitioners (GPs) could use a ‘goals of care’ (GOC) approach with dementia patients, as well as other nursing home patients. The three-phase GOC model describes the medical status of the patient as curative/restorative phase (‘beating it’), palliative phase (‘living with disease, anticipating death’) or terminal phase (‘dying very soon’) [10]. The prognoses associated with these three categories as defined by Thomas et al. [10] are indefinite, months to years and days to weeks, respectively. The stratification of GOC can additionally facilitate a discussion of the limitations of medical treatment, as seen in the acute hospital system. On admission, our patient would have been assessed as dying very soon (likely days to weeks prognosis), given her hip fracture, acute NSTEMI and advanced dementia. This assessment could have been shared with her son to help inform his decision. Thomas et al. [10] are clear that determining GOC requires ‘high-quality clinical assessment and good communication skills’. GPs responsible for patient care in nursing homes are ideally placed to formulate GOC discussions, placing them and the patient/SDM as the key decision makers. Cardona-Morrell and Hillman [11] recently proposed a screening tool (CriSTAL) for the identification of the dying patient. Such tools may help determine the limits of medical treatment and the preferred venue of care for patients in both community and acute settings.
Despite the clinical scenario, our patient survived the operation and lived another 4 months. The change in her quality of life remains debatable, but this case highlights a growing issue. As ever in medicine, we need to first consider if we should intervene. Once that decision is made, how we should proceed is even more important. Our care should respect the people we meet, their beliefs and the relationships upon which their lives are bound.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
The relevant institution does not require ethics approval. The manuscript conforms to standards currently applied in Australia.
CONSENT
Consent is provided in the format used by the Medical Journal of Australia. The patient's next of kin has read the final document and indicated as such on the provided consent form. In addition, the manuscript has been completely anonymized.
GUARANTOR
E.W. is a guarantor of the study.
REFERENCES
- 1.World Health Organization (WHO). 10 Facts on Dementia. March 2015 . http://www.who.int/features/factfiles/dementia/en/ (26 June 2015, date last accessed). [Google Scholar]
- 2.Alzheimer's Disease International. Dementia Statistics. http://www.alz.co.uk/research/statistics (26 June 2015, date last accessed). [Google Scholar]
- 3.National Health Service Choices. Hip Fracture. July 2014. http://www.nhs.uk/conditions/hip-fracture/Pages/introduction.aspx (26 June 2015, date last accessed). [Google Scholar]
- 4.Melton LJ III, Beard CM, Kokmen E, Atkinson EJ, O'Fallon WM. Fracture risk in patients with Alzheimer's disease. J Am Geriatr Soc 1994;42:614–19. [DOI] [PubMed] [Google Scholar]
- 5.Laditka JN, Laditka SB, Cornman CB. Evaluating hospital care for individuals with Alzheimer's disease using inpatient quality indicators. Am J Alzheimers Dis Other Demen 2005;20:27–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth 2008;55:146–54. [DOI] [PubMed] [Google Scholar]
- 7.Fleeter TB. Informed Consent: More Than Just a Signature. American Academy of Orthopaedic Surgeons; http://www.aaos.org/news/aaosnow/jan10/managing4.asp (11 August 2015, date last accessed). [Google Scholar]
- 8.National Hip Fracture Database 2010. British Geriatric Society. http://www.nhfd.co.uk/20/hipfractureR.nsf/vwcontent/2010ReportDownload/$File/NHFD2010Report.pdf?openelement (28 January 2016, date last accessed).
- 9.McNamara P, Sharma K. Surgery or palliation for hip fractures in patients with advanced malignancy? Age Ageing 1997;26:471–74. [DOI] [PubMed] [Google Scholar]
- 10.Thomas RL, Zubair MY, Hayes B, Ashby MA. Goals of care: a clinical framework for limitation of medical treatment. Med J Aust 2014;201:452–55. [DOI] [PubMed] [Google Scholar]
- 11.Cardona-Morrell M, Hillman K. Development of a tool for defining and identifying the dying patient in hospital: Criteria for Screening and Triaging to Appropriate aLternative care (CriSTAL). BMJ Support Palliat Care 2015;5:78–90. [DOI] [PMC free article] [PubMed] [Google Scholar]


