Abstract
Background
There is an increasing focus on optimizing healthcare quality and reducing costs. The care of children undergoing heart surgery requires significant investment of resources, and it remains unclear how costs of care relate to quality. We evaluated this relationship across a multi-center cohort.
Methods
Clinical data from The Society of Thoracic Surgeons Database were merged with cost data from the Pediatric Health Information Systems Database for children undergoing heart surgery (2006–2010). Hospital-level costs were modeled using Bayesian hierarchical methods adjusting for case-mix, and hospitals were categorized into cost tertiles. The primary quality metric evaluated was in-hospital mortality.
Results
Overall, 27 hospitals (30,670 patients) were included. Median adjusted cost/case was $82,360 and varied 5-fold across hospitals, while median adjusted mortality was 3.4% and ranged from 2.4%–5.0% across hospitals. Overall, hospitals in the lowest cost tertile had significantly lower adjusted mortality rates compared with the middle and high cost tertiles (2.5% vs. 3.8% and 3.5% respectively, both p<0.001). When assessed at the individual hospital level, most (75%) but not all hospitals in the lowest cost tertile were also in the lowest mortality tertile. Similar relationships were seen across the spectrum of surgical complexity. Lower cost hospitals also had shorter length of stay and trends toward fewer major complications.
Conclusions
Lowest cost hospitals generally deliver the highest quality care for children undergoing heart surgery, although there is some variation in this relationship. This information is important in the design of initiatives aiming to optimize healthcare value in this population.
Introduction
In this era of rising healthcare expenditures, there is increased emphasis on both optimizing quality of care and reducing costs, or providing high “value” care. Recent healthcare reforms provide incentives to encourage improvements in both of these domains, leading to heightened efforts to better understand the relationship between quality and cost across multiple medical and surgical specialties (1).
The care of children with heart disease is known to account for substantial resource utilization, and recent analyses have demonstrated that there is significant variation in cost of care for children undergoing heart surgery across US children’s hospitals (2–4). However, detailed information regarding the relationship between measures of hospital quality and cost in this population is lacking, and it is unclear whether it is possible to deliver high quality care at a relatively low cost (in relation to other centers providing this type of care). A previous study suggested that this may not be possible, and that low cost hospitals may deliver lower quality care (5). Understanding these relationships is critical in the appropriate design of policies aiming to optimize value in this population and others. For example, it would not be advisable to provide incentives to low cost centers if these low costs were achieved at the expense of poor clinical outcomes.
The purpose of the present study was to evaluate hospital-level relationships between measures of quality and cost for children undergoing heart surgery, using a unique dataset of merged clinical information and resource utilization data across a large multi-center cohort.
Material and Methods
Data Source
Merged information from the Society of Thoracic Surgeons Congenital Heart Surgery (STS-CHS) Database and Pediatric Health Information Systems (PHIS) Database was used for this analysis. As described previously, linking these datasets capitalizes on the strengths of both datasets, including the detailed clinical information in the STS-CHS Database and resource utilization information in the PHIS Database (6). The STS-CHS Database is the largest existing pediatric heart surgery registry, and collects detailed peri-operative data on all children undergoing heart surgery at >100 North American centers. Data quality is evaluated through intrinsic data verification (e.g. identification and correction of missing/out of range values and inconsistencies across fields), and random site audits at 10% of participating institutions annually. The PHIS Database is a large administrative database that collects resource utilization information from >40 US children’s hospitals. Systematic monitoring in the PHIS Database includes coding consensus meetings, consistency reviews, and quarterly data quality reports (6). This study was not considered human subjects research by the Duke University and University of Michigan Institutional Review Boards in accordance with the Common Rule (45 CFR 46.102(f)).
Study Population
As previously described and verified, STS-CHS and PHIS data were linked at the patient level for children 0–18 years undergoing congenital heart surgery using the method of indirect identifiers (6,7). For the purposes of this study, hospitals participating in both the STS-CHS and PHIS Databases from 2006–2010 were eligible for inclusion (n=33 hospitals). To optimize data quality, hospitals with >15% missing data for any of the study outcomes or patient characteristics (described below) were excluded (n=6 hospitals). From the remaining 27 hospitals, patients undergoing any cardiovascular operation (with or without cardiopulmonary bypass) classified in any of the Society of Thoracic Surgeons-European Association for Cardiothoracic Surgery (STAT) Categories were included (n=30,885 patients) (8). Patients (0.7%) with missing data for study outcomes were excluded.
Data Collection
Data collected from the STS-CHS Database included demographics (age, weight, gender, race), standard STS-defined pre-operative risk factors, non-cardiac/genetic abnormalities, presence of prematurity, history of previous cardiothoracic surgery, and operative data including STAT category (9). Data on outcome/quality metrics included in-hospital mortality, post-operative length of stay (LOS), and the occurrence of any of the major post-operative complications collected and defined in the STS-CHS Database (renal failure requiring dialysis, neurologic deficit persisting at discharge, arrhythmia requiring permanent pacemaker, mechanical circulatory support, phrenic nerve injury/paralyzed diaphragm, and unplanned re-operation/re-intervention) (10).
Resource utilization information collected from the PHIS Database included payer type (government, private, and other) and total hospital charges. As previously described, costs were estimated using hospital and department specific cost-to-charge ratios, adjusted for regional differences using the Centers for Medicare and Medicaid Services price and wage index, and indexed to 2010 dollars (4). Of note, professional fees are not included in most administrative datasets, including the PHIS database, and thus could not be included in this analysis.
Analysis
Study population characteristics were described using standard summary statistics. Negative binomial Bayesian hierarchical models were used to calculate adjusted costs/case on a hospital level. Log link functions were used to account for the skewed cost distribution. This methodology also accounts for increased variability in estimates from centers with smaller sample size and shrinks estimates from smaller centers toward the population average to provide more stable estimates (11). All models included a center-level random intercept and adjusted for important patient characteristics/differences in case mix that may impact resource utilization and outcomes across sites including age, weight, gender, race, prematurity, the presence of any non-cardiac/genetic abnormality or STS-defined pre-operative risk factor, previous cardiothoracic surgery, payer type, year of surgery, and operation type using the STAT methodology (8).
In order to evaluate the relationship between hospital cost and quality, hospitals were categorized into low, middle, and high cost tertiles based on their adjusted cost estimates described above, and measures of quality across the cost tertiles were evaluated. In-hospital mortality was the primary quality metric evaluated, as it is currently the most widely used metric in the field. Post-operative LOS and major complication rates were also evaluated as additional quality metrics in secondary analysis. Both of these metrics are also commonly used as measures of quality of care by various organizations (10,12). In order to calculate adjusted mortality rates across the hospital cost tertiles, marginal logistic regression models using the method of generalized estimating equations (GEE) were fitted, including an indicator for hospital cost tertile and the patient characteristics described above. The observed-to-expected method was used to calculate the adjusted mortality rates. Similar methods were used to evaluate adjusted rates of major complications across the hospital cost tertiles. Odds ratios and 95% confidence intervals in middle and high vs. low cost hospitals were also calculated. For the evaluation of adjusted post-operative LOS, negative binomial GEE models with log link were fitted, including an indicator for hospital cost tertile, and the patient characteristics described above. Adjusted ratios of length of stay and 95% confidence intervals in the middle and high vs. low cost hospitals were also calculated. Analyses were performed overall as well as stratified by STAT categories 1–3 (“low” risk operations) and STAT 4–5 (“high” risk operations). R version 3.0.1 (R Foundation for Statistical Computing), OpenBUGS version 3.2.2 (OpenBUGS Foundation), and SAS software version 9.3 (SAS Institute) were used for the analysis. A p-value <0.05 was considered statistically significant.
Results
Study population characteristics
Overall, 27 hospitals (30,670 patients) were included (Table 1). Hospitals were diverse geographically (37% Midwest, 33% South, 19% West, 11% Northeast), and included a wide range of surgical volume (median 360 cases/year, range 109–910 cases/year). Compared with the overall cohort of hospitals participating in the STS-CHS Database during the study period (n=108), the 27 hospitals included in the present study had a higher average surgical volume (360 vs. 175 cases/year) and included a higher proportion of centers in the Midwest (37% vs. 22%).
Table 1.
Study population characteristics
| Adjusted Hospital Cost Tertile | |||||
|---|---|---|---|---|---|
| Overall (n=30,670; 27 hospitals) |
Low (n=10,491; 9 hospitals) |
Middle (n=11,419, 9 hospitals) |
High (n=8760; 9 hospitals) |
p-value | |
| Patient Characteristics | |||||
| Age at surgery, years* | 0.6 (0.1–3.5) | 0.6 (0.1–3.2) | 0.6 (0.1–3.6) | 0.6 (0.1–4.0) | <0.001 |
| Neonates | 6,687 (21.8%) | 2,397 (22.8%) | 2,435 (21.3%) | 1,855 (21.2%) | <0.01 |
| Weight at surgery, kg | 6.7 (2.9–14.4) | 6.6 (3.8–13.5) | 6.6 (3.9–14.6) | 6.8 (3.9–15.2) | <0.0001 |
| Any previous CT surgery | 9,264 (30.2%) | 3,179 (30.3%) | 3,375 (29.6%) | 2,710 (30.9%) | 0.44 |
| Any non-cardiac/genetic anomaly | 8,718 (28.4%) | 3,079 (29.3%) | 3,165 (27.7%) | 2,474 (28.2%) | 0.08 |
| Any STS pre-op risk factor | 7,585 (24.7%) | 2,811 (26.8%) | 2,733 (23.9%) | 2,041 (23.3%) | <0.0001 |
| STAT Category 4–5 (vs. 1–3) | 7,566 (24.7%) | 2,784 (26.5%) | 2,785 (24.4%) | 1,997 (22.8%) | <0.0001 |
| Hospital Characteristics | |||||
| Surgical Volume (cases/yr) | 360 (286–420) | 411 (351–580) | 355 (333–406) | 359 (249–383) | 0.08 |
Data are presented as n (%) and median (interquartile range)
For age at surgery (years), 10% trimmed means as an additional measure of central tendency across groups are: low: 1.6, middle: 1.8, high: 2.0.
In the included 27 hospitals, median adjusted cost/case at the hospital level was $82,360 and varied 5-fold across hospitals. The median adjusted mortality rate was 3.4% and ranged from 2.4% – 5.0% across hospitals.
Patient and center characteristics across hospital cost tertiles
Hospitals were categorized into tertiles based on adjusted costs. Median adjusted cost/case was $53,410 in the low cost tertile, $82,360 in the middle cost tertile, and $154,410 in the high cost tertile. Patient and center characteristics across the adjusted hospital cost tertiles are displayed in Table 1. Hospitals in the low cost tertile tended to be have a higher surgical volume (median annual surgical volume of 411 cases/year vs. 355 cases/year in the middle cost tertile, and 359 cases/year in the high cost tertile, p=0.08). The low cost hospitals appeared to treat a similar to slightly higher complexity patient population. For example 26.5% of patients at low cost centers were in STAT category 4–5 vs. 24.4% in the middle cost tertile and 22.8% in the high cost tertile (p<0.0001). Low cost hospitals also treated a slightly higher proportion of neonates and those with STS-defined pre-operative risk factors (Table 1).
Quality-cost relationship
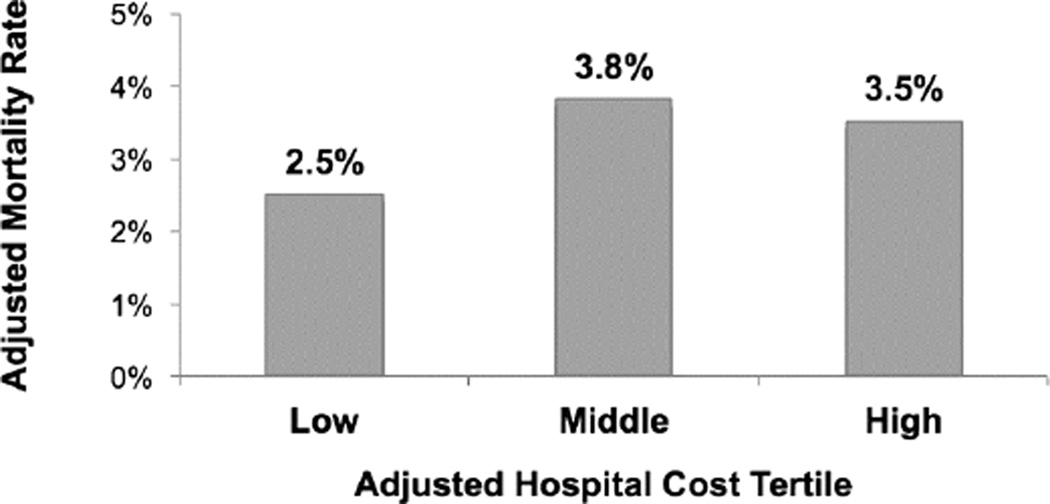
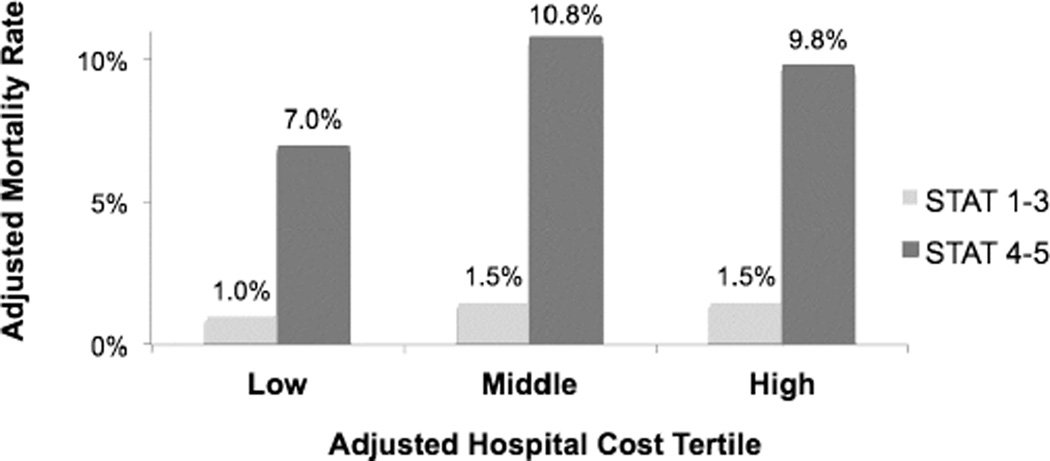
As displayed in Figure 1A, hospitals in the lowest adjusted cost tertile had significantly lower adjusted mortality rates compared with the middle and high cost tertiles (2.5% vs. 3.8% and 3.5% respectively, both p<0.001). In stratified analysis, a similar relationship was seen within both STAT categories 1–3 and 4–5 (Figure 1B).
Figure 1.
a. Mortality across hospital cost tertiles
p<0.001 for low vs. middle and low vs. high cost tertiles p=0.46 for middle vs. high cost tertile
B. Stratified by STAT category
p<0.03 for low vs. middle and low vs. high cost tertiles for both groups p=0.84 (STAT 1–3), and p=0.44 (STAT 4–5) for middle vs. high cost tertile
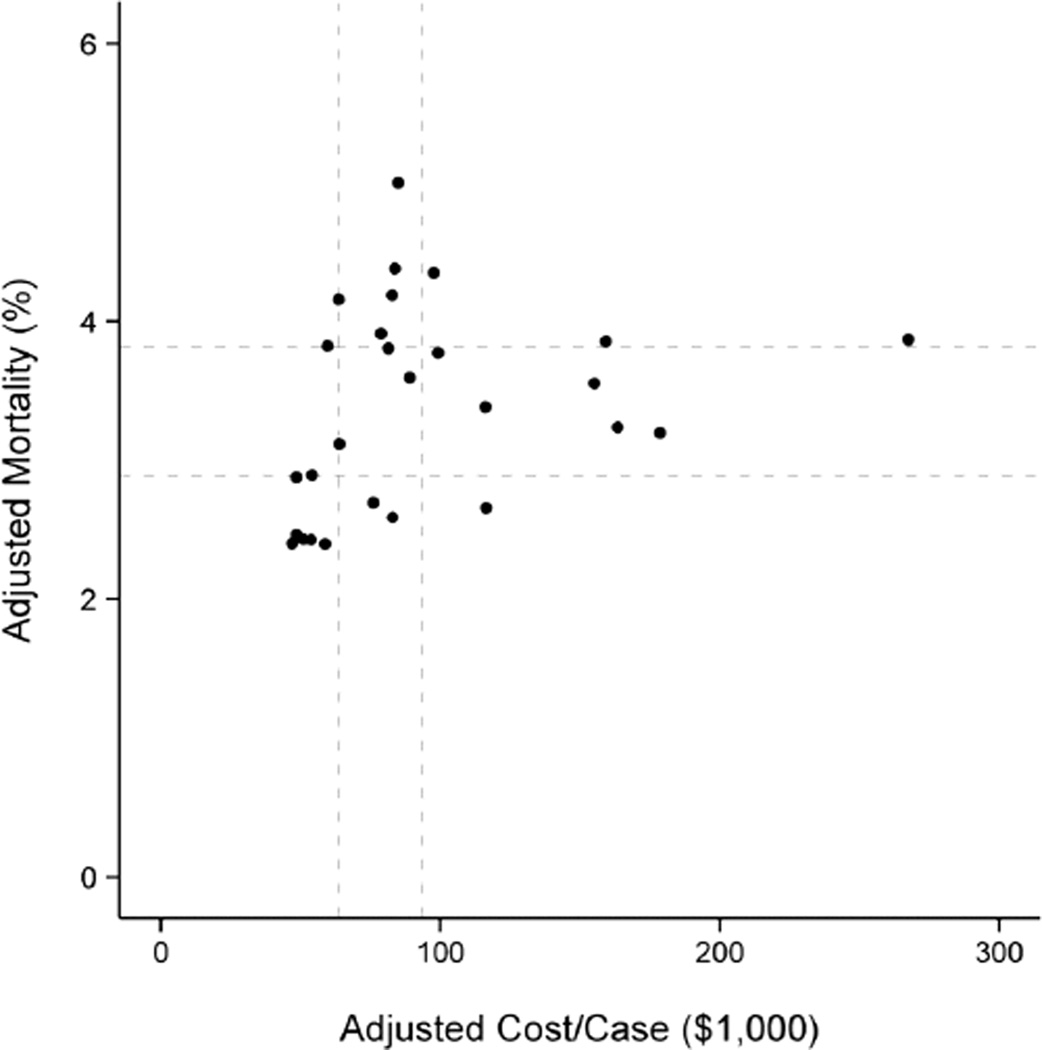
These general associations were also examined at the individual hospital level, and there was some variability across hospitals (Figure 2). For example, most (75%), but not all hospitals in the lowest adjusted cost tertile were also in the lowest adjusted mortality tertile.
Figure 2. Adjusted mortality and costs across individual hospitals.
Each dot represents one of the 27 hospitals in the cohort. Dotted lines indicate tertile cutoffs for adjusted costs and adjusted mortality. Spearman correlation = 0.5 (p=0.01).
In secondary analysis, post-operative LOS and major complications were evaluated across adjusted hospital cost tertiles. Hospitals in the lowest adjusted cost tertile had significantly shorter post-operative LOS (11.9 days vs. 13.7 days in the middle cost tertile and 15.2 days in the high cost tertile, both p<0.05; Table 2). These relationships were similar within both STAT categories 1–3 and 4–5 (Table 2). Evaluation of major complications showed a trend toward fewer complications at low cost hospitals, most prominent within STAT categories 4–5; however these differences were not statistically significant (Table 2).
Table 2.
Post-operative LOS and major complications across hospital cost tertiles
| LOS | Major Complications | |||||
|---|---|---|---|---|---|---|
| Overall | ||||||
| Adjusted Hospital Cost Tertile |
Adjusted ratio (95% CI) |
Adjusted estimate (days) |
P-value | Adjusted OR (95% CI) |
Adjusted estimate (%) |
P-value |
| Low | Reference | 11.9 | Reference | 7.6% | ||
| Middle | 1.13 (1.004, 1.75) | 13.7 | 0.04 | 1.22 (0.86, 1.53) | 9.3% | 0.19 |
| High | 1.22 (1.11, 1.69) | 15.2 | 0.0001 | 1.18 (0.90, 1.61) | 8.8% | 0.19 |
| STAT 1–3 | ||||||
| Low | Reference | 9.1 | Reference | 5.1% | ||
| Middle | 1.14 (1.00, 1.74) | 10.5 | 0.05 | 1.14 (0.71, 1.58) | 5.8% | 0.48 |
| High | 1.20 (1.09, 1.70) | 11.4 | <0.001 | 1.10 (0.76, 1.66) | 5.6% | 0.52 |
| STAT 4–5 | ||||||
| Low | Reference | 22.0 | Reference | 15.1% | ||
| Middle | 1.14 (1.02, 1.76) | 25.5 | 0.02 | 1.32 (0.96, 1.45) | 20.1% | 0.08 |
| High | 1.27 (1.16, 1.64) | 30.2 | <0.0001 | 1.26 (0.94, 1.51) | 18.9% | 0.10 |
For LOS, data are presented as adjusted estimates and adjusted ratios of LOS (length of stay) across cost tertiles; for major complications, data are presented as adjusted rates and adjusted OR (odds ratios) of major complications across cost tertiles.
Comment
This multi-center analysis demonstrates that lowest cost hospitals generally delivered the highest quality care for children undergoing heart surgery with regard to in-hospital mortality. At the individual hospital level, this relationship was somewhat variable and was not uniformly consistent across every institution. Our general findings regarding the quality-cost relationship were present across the spectrum of surgical complexity and lower cost hospitals also had shorter LOS and trends toward fewer major complications.
Efforts to optimize both quality and cost have received much attention due to rising healthcare expenditures and several recent national healthcare initiatives. However, the relationship between quality and cost is not well understood. Many studies in the adult surgical literature suggest that high quality care is associated with lower costs (13–15). For example, high quality care may be associated with shorter LOS, and fewer complications and readmissions, which translate into lower costs (14,15). On the other hand, it may be that achieving the best overall outcomes requires significant investment of resources. Some studies suggest that higher quality care can actually lead to higher costs, for example through longer LOS and higher readmission rates, which may be costly but avert worse outcomes, including death (16,17).
In the congenital heart surgery population, a previous study evaluating the quality-cost relationship utilized a large administrative database, the Kid’s Inpatient Database (KID), and included 35,446 children undergoing heart surgery in 2003, 2006, and 2009 (5). Interestingly, contrary to the findings of the present study, this study found that children treated at higher cost hospitals had significantly lower in-hospital mortality (higher quality). However, several characteristics of administrative data and related methodology can make these results difficult to interpret. First, the sampling strategy used in the KID Database includes 80% of hospitalized children, however it is not clear how this pertains to patients with congenital heart disease in terms of the proportion or type of lesions included across hospitals. In addition, due to limitations of the ICD-9 system used in administrative datasets, it is known that there can be inaccuracies in case ascertainment (capture and coding of all relevant cases across hospitals) which can have a significant impact on outcomes assessment (18–20). However, likely most important in this case are issues related to risk adjustment. While the data captured in administrative datasets do allow for some degree of adjustment for differences in important patient characteristics and baseline comorbidities across hospitals, other important data are not captured (e.g. weight at surgery). In addition, the methodology used in administrative data also may not distinguish between comorbidities present at admission versus complications that occur later during the admission. Because of this, a high quality hospital with a low complication rate may instead be characterized as treating a low “severity of illness” patient population with few baseline comorbidities. (21,22). In adjusted analyses, this can falsely worsen reported outcomes at high quality centers and vise versa.
The methodology in the present study takes advantage of a unique dataset that leverages the detailed clinical information captured in the STS-CHS Database for case ascertainment and case-mix adjustment, and the important resource utilization information captured in the PHIS Database. Our results demonstrate that the lowest cost hospitals generally delivered the highest quality care, as measured by the metrics evaluated in this study. However, it is also important to note that this relationship was not completely consistent across hospitals and that not all of the lowest cost institutions were also categorized in the group with the highest quality care. In addition, this study demonstrates that the lowest cost hospitals tended to be higher volume centers. This finding is consistent with previous analyses that have evaluated volume-cost and volume-outcome relationships in much greater detail and have demonstrated associations between higher volume, lower costs, and better outcomes, primarily for high complexity patients (4,23)
These results have several important implications. First, our findings suggest that policies and initiatives aiming to improve quality may also hold the potential for reducing cost, resulting in higher value care. These may include multi-center quality improvement initiatives, policies geared toward centralizing care at regional centers of excellence, or proposed federal reforms as a part of the Affordable Care Act tying reimbursements to meeting certain quality standards (24). Further study of the characteristics of high quality, low cost hospitals will be particularly important in informing such initiatives aiming to improve value across institutions.
In addition, the variability in the cost-quality relationship found in our study and inconsistencies across institutions, suggest that information on both quality and cost are important. Policies and incentives geared toward improving value likely cannot be designed or accurately informed based on knowing just one side of the equation. Further efforts are needed to provide hospitals and other stakeholders with accurate and integrated information regarding both quality and costs of care, so that they may benchmark their performance and track changes over time. Merged information from clinical and administrative sources, such as the datasets used in this study, may have the best potential to provide such information.
Limitations
This study involved a subset of US children’s hospitals performing congenital heart surgery. While the included hospitals had a geographic distribution mirroring that of the larger cohort of all US congenital heart centers, and included a wide range of center volume, further evaluation is necessary to assess whether the relationships identified in our study are similar across a broader sample of hospitals (25). Our assessment was also limited to in-hospital outcomes and costs, and further evaluation of longer-term outcomes and resource utilization is also necessary. Finally, our results should be interpreted as hospital-level associations rather than cause and effect. Further study is needed to understand the mechanisms underlying differences in quality and cost across hospitals, and to evaluate both patient and hospital-level interventions to improve quality and assess relationships with cost.
Conclusions
This multi-center analysis demonstrates that low cost hospitals generally delivered the highest quality care for children undergoing heart surgery. Our results also demonstrated some degree of variability in the quality-cost relationship suggesting both the opportunity for improvement, and that knowledge of both sides of the equation is important in the design of initiatives aiming to incentivize and reward high value care. Further efforts are necessary to study the impact of such initiatives, to evaluate longer-term quality and cost, and to better provide integrated and accurate quality-cost feedback to hospitals and other stakeholders so that performance may be benchmarked and assessed over time.
Acknowledgments
Funding source
Supported in part by the National Heart, Lung, and Blood Institute (K08HL103631 and R01HL122261, PI: Pasquali).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 2.Keren R, Luan X, Localio R, et al. Prioritization of comparative effectiveness research topics in hospital pediatrics. Arch Pediatr Adolesc Med. 2012;166:1155–1164. doi: 10.1001/archpediatrics.2012.1266. [DOI] [PubMed] [Google Scholar]
- 3.Robbins JM, Bird TM, Tilford JM, et al. Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects-United States, 2003. MMWR. 2007;56:25–29. [PubMed] [Google Scholar]
- 4.Pasquali SK, Jacobs ML, He X, et al. Variation in congenital heart surgery costs across hospitals. Pediatrics. 2014;133:e553–e560. doi: 10.1542/peds.2013-2870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Romley JA, Chen AY, Goldman DP, Williams R. Hospital costs and inpatient mortality among children undergoing surgery for congenital heart disease. Health Services Research. 2014;49:588–608. doi: 10.1111/1475-6773.12120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pasquali SK, Jacobs JP, Shook GJ, et al. Linking clinical registry data with administrative data using indirect identifiers: Implementation and validation in the congenital heart surgery population. Am Heart J. 2010;160:1099–1104. doi: 10.1016/j.ahj.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pasquali SK, Li JS, He X, et al. Perioperative methylprednisolone and outcome in neonates undergoing heart surgery. Pediatrics. 2012;129:e385–e391. doi: 10.1542/peds.2011-2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Brien SM, Clarke DR, Jacobs JP, et al. An empirically based tool for analyzing mortality associated with congenital heart surgery. J Thorac Cardiovasc Surg. 2009;138:1139–1153. doi: 10.1016/j.jtcvs.2009.03.071. [DOI] [PubMed] [Google Scholar]
- 9.STS Database Full Specifications. [Accessed 12/9/2014]; Available at: http://www.sts.org/sites/default/files/documents/CongenitalDataSpecsV3_22.pdf. [Google Scholar]
- 10.Jacobs JP, Jacobs ML, Austin EH, et al. Quality Measures for Congenital and Pediatric Cardiac Surgery. World J Pediatr Congenit Heart Surg. 2012;3:32–47. doi: 10.1177/2150135111426732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dimick JB, Staiger DO, Birkmeyer JD. Ranking hospitals on surgical mortality: The importance of reliability adjustment. Health Serv Res. 2010;45(6 Pt 1):1614–1629. doi: 10.1111/j.1475-6773.2010.01158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs JP, Jacobs ML, Mavroudis C, et al. Durham, NC: The Society of Thoracic Surgeons and Duke Clinical Research Institute, Duke University Medical Center; Executive Summary: STS Congenital Heart Surgery Database–Twenty-first Harvest–(July 1, 2010–June 30, 2014) [Google Scholar]
- 13.Glance LG, Dick AW, Osler TM, Meredith W, Mukamel DB. The association between cost and quality in trauma: Is greater spending associated with higher-quality care? Ann Surg. 2010;252:217–222. doi: 10.1097/SLA.0b013e3181e623f6. [DOI] [PubMed] [Google Scholar]
- 14.Birkmeyer JD, Gust G, Dimick JB, Birkmeyer NJ, Skinner JS. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg. 2012;255:1–5. doi: 10.1097/SLA.0b013e3182402c17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA., Jr Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531–537. doi: 10.1016/j.jamcollsurg.2004.05.276. [DOI] [PubMed] [Google Scholar]
- 16.Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med. 2010;363:297–298. doi: 10.1056/NEJMc1001882. [DOI] [PubMed] [Google Scholar]
- 17.Ong MK, Mangione CM, Romano PS, et al. Looking forward, looking back: assessing variations in hospital resource use and outcomes for elderly patients with heart failure. Circ Cardiovasc Qual Outcomes. 2009;2:548–557. doi: 10.1161/CIRCOUTCOMES.108.825612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pasquali SK, Peterson ED, Jacobs JP, et al. Differential case ascertainment in clinical registry vs. administrative data and impact on outcomes assessment in pediatric heart surgery. Ann Thorac Surg. 2013;95:197–203. doi: 10.1016/j.athoracsur.2012.08.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jantzen DW, He X, Jacobs JP, et al. The impact of differential case ascertainment in clinical registry versus administrative data on assessment of resource utilization in pediatric heart surgery. World Journal for Pediatric and Congenital Heart Surgery. 2014;5:398–405. doi: 10.1177/2150135114534274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pasquali SK, He X, Jacobs JP, et al. Measuring hospital performance in congenital heart surgery: A comparison of administrative and clinical registry data. Ann Thorac Surg. 2015;99:932–938. doi: 10.1016/j.athoracsur.2014.10.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hughes JS, Averill FR, Goldfield NI, et al. Identifying potentially preventable complications using a present on admission indicator. Health Care Financing Reviews. 2006;27:63–81. [PMC free article] [PubMed] [Google Scholar]
- 22.Dalton JE, Glance LG, Mascha EJ, Ehrlinger J, Chamoun N, Sessler DI. Impact of present-on-admission indicators on risk-adjusted hospital mortality measurement. Anesthesiology. 2013;118:1298–1206. doi: 10.1097/ALN.0b013e31828e12b3. [DOI] [PubMed] [Google Scholar]
- 23.Welke KF, O’Brien SM, Peterson ED, Ungerleider RM, Jacobs ML, Jacobs JP. The complex relationship between pediatric cardiac surgical case volumes and mortality rates in a national clinical database. J Thorac Cardiovasc Surg. 2009;137(5):1133–1140. doi: 10.1016/j.jtcvs.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 24.Accountable care organizations (ACOs) and Pediatricians: Evaluation and Engagement. AAP news. 2011 Jan 1;32(1) [Google Scholar]
- 25.Jacobs ML, Daniel M, Mavroudis C, et al. Report of the 2010 Society of Thoracic Surgeons Congenital Heart Surgery Practice and Manpower Survey. Ann Thorac Surg. 2011;92:762–768. doi: 10.1016/j.athoracsur.2011.03.133. [DOI] [PubMed] [Google Scholar]