Abstract
Previous studies have revealed that TRPV1 and TRPA1 function downstream of many itch receptors, where they mediate inward current to trigger action potentials in primary afferents. Although other TRP channels, such as TRPV4, are expressed in primary afferents, whether or not they play an analogous role in itch was previously unknown. Now, Akiyama et al. provide evidence that TRPV4 is a key mediator of serotonin-induced itch. This finding is important because it uncovers an unanticipated role for TRPV4 in itch, thereby identifying a novel therapeutic target.
Clinical Relevance of Itch
Chronic itch, which is defined as itch lasting more than 6 weeks, is a prevalent problem that occurs in ~10% of the population (Mollanazar et al., 2015). Chronic itch conditions negatively affect quality of life, and yet there are no therapies that are both efficacious and selective for itch. The lack of effective treatment is partly attributable to a poor understanding of the mechanisms that underlie it. Although antihistamines are frequently prescribed as a treatment for itch, they are typically ineffective because most types of chronic itch are not histamine-mediated (Mollanazar et al., 2015). Unfortunately, while there are numerous mediators that can cause itch, the factors that are responsible in most circumstances of chronic itch are largely unknown. One candidate mediator is serotonin (5-hydroxytryptamine, 5-HT). Human psychophysical studies have shown that application of serotonin into the skin causes itch (Weisshaar et al., 2004). In rodents, serotonin is a key component of mast cells, and it is a potent mediator of itch. However, until recently, the mechanisms through which serotonin causes itch have remained uncertain.
TRPs as downstream mediators of itch (pruritogens)
Many pruritogens bind to metabotropic receptors on primary sensory neurons; however, these receptors must be coupled to ionotropic channels via intracellular signaling pathways in order to allow sufficient current influx to generate action potentials. Several groups have shown that the cation channels TRPV1 and TRPA1 are coupled to different pruritogen receptors and that they are critical for different forms of itch transmission (Ross, 2011). More specifically, TRPV1 is required for histaminergic itch, whereas TRPA1 is required for several types of non-histaminergic itch, such as that induced by chloroquine, BAM8-22, IL-31, endothelin-1, thymic stromal lymphopoietin, and bile acids. Until recently, whether serotonin receptors were likewise coupled to TRPs remained unknown.
Mechanisms of serotonin-induced itch
Understanding serotonin-mediated itch has been complicated by the fact that there are numerous serotonin receptors that are expressed on primary afferents, as well as on immune mediators that could be involved in itch. It was previously hypothesized that the primary pathway through which serotonin causes itch is via stimulation of histamine release from mast cells. However, contrary to this idea, antihistamines failed to reduce serotonin-induced itch sensation in humans (Hosogi et al., 2006). Thus, the mechanisms of serotonin-induced itch remained unknown.
A role for 5-HT7 and TRPA1 in serotonin-mediated itch
A recent study has demonstrated that one way in which serotonin induces itch is via direct activation of 5-HT7 (encoded by HTR7), which is expressed on subsets of primary sensory afferents (Morita et al., 2015). In this study, mice lacking either HTR7 or TRPA1 showed substantially reduced scratching behavior in response to an intradermal injection of a 5-HT7-selective agonist. Furthermore, HTR7 and TRPA1 knockout mice scratched considerably less in a model of atopic dermatitis. However, it seemed likely that this was only part of the serotonin-itch story, because the 5-HT2-selective agonist, α-methyl-5HT, is a potent pruritogen in mice. As reported in this issue of JID, the study by Carstens and colleagues (2015) provides further insight into the molecular players involved in serotonin-evoked itch by defining a TRPV4-dependent pathway that is likely to be downstream of 5-HT2-mediated itch.
An unexpected role for TRPV4 in serotonin-mediated itch
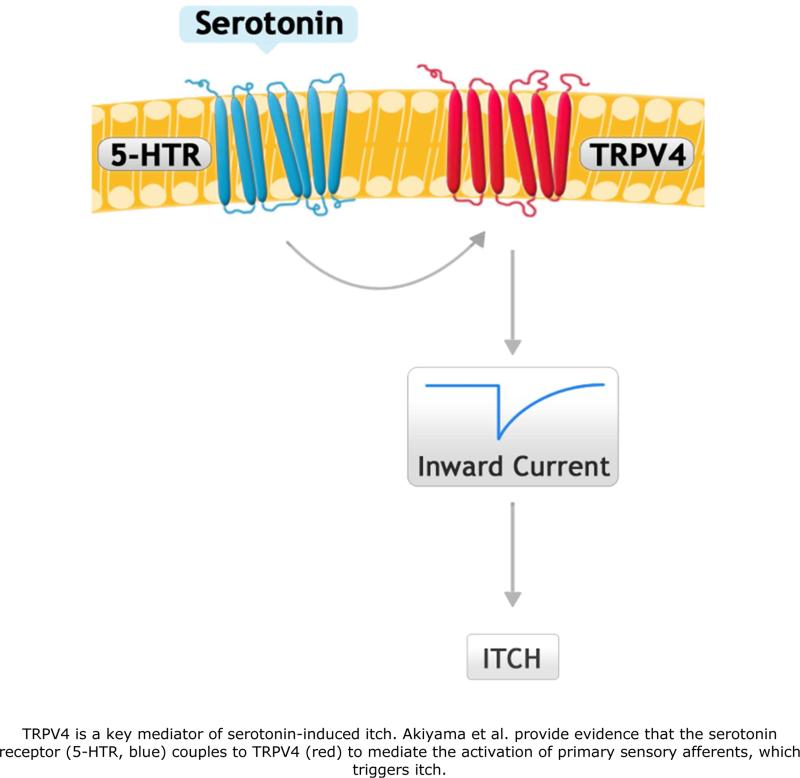
The original goal of this study was to investigate a possible role for TRPV4 in itch. TRPV4 is upregulated in the skin of individuals with certain itch conditions (Moore et al., 2013; Yang et al., 2015), suggesting that it may be involved in itch in humans. Interestingly, TRPV4 knockout mice displayed a significant reduction in scratching behavior in response to serotonin, but not to histamine, chloroquine, or SLIGRL (Akiyama et al., 2015). A TRPV4 antagonist also reduced substantially the amount of serotonin-evoked scratching, supporting the idea that TRPV4 is critical to serotonin signaling in normal mice. Importantly, the authors showed that the change in response to serotonin in the TRPV4 knockout mice was specifically a decrease in serotonin-evoked itch behaviors, and not a change in serotonin-evoked pain behaviors. This study demonstrates that TRPV4 is a key downstream component of serotonin-evoked itch (Figure 1).
Figure. TRPV4 is a key mediator of serotonin-induced itch.
Akiyama et al. provide evidence that the serotonin receptor (5-HTR, blue) couples to TRPV4 (red) to mediate the activation of primary sensory afferents, which triggers itch.
In order to link serotonin to TRPV4 and the activation of sensory neurons, the authors visualized calcium responses to serotonin in dorsal root ganglion neurons. They found that ~90% of sensory neurons that respond to serotonin also expressed TRPV4. Serotonin-mediated activation was dependent on TRPV4, as a TRPV4 antagonist reduced significantly the calcium response to the application of serotonin. In support of this finding, the authors demonstrated that the proportion of neurons that responded to serotonin was reduced significantly in TRPV4 knockout mice. Interestingly, the proportion of neurons responding to other types of pruritogens did not change in mice lacking TRPV4, indicating that TRPV4 plays an important and specific role in responses to serotonin in primary sensory neurons. To identify the receptor through which serotonin acts, Akiyama et al. (2015) used subtype specific antagonists for 5-HT1 and 5-HT2. The 5-HT2 antagonist, but not the 5-HT1 antagonist, reduced serotonin-evoked scratching. This finding raises the possibility that 5-HT2, acting via TRPV4, is key mediator of serotonin-evoked itch. Thus, there appear to be at least two distinct pathways through which serotonin mediates itch: a TRPA1-dependant pathway that mediates 5-HT7-mediated itch, as well as a TRPV4-dependent pathway that likely mediates 5-HT2-mediated itch. What remains to be tested is whether these receptors are expressed on distinct or overlapping populations of primary sensory afferents.
ACKNOWLEDGEMENTS
This research was supported by NIH grants R01 AR063772 and R21 AR064445 to S.E.R and R37 AA10422 to G.E.H. L.M.S. and M.S.K. are supported by a T32 NS 73548-3.
Footnotes
TRPV4 is a key mediator of serotonin-induced itch, thereby identifying a novel therapeutic target.
Conflict of Interest
The authors state no conflict of interest.
References
- Akiyama T, Ivanov M, Nagamine M, et al. Involvement of TRPV4 in serotonin-evoked scratching. J Invest Dermatol. 2015 doi: 10.1038/JID.2015.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosogi M, Schmelz M, Miyachi Y, et al. Bradykinin is a potent pruritogen in atopic dermatitis: a switch from pain to itch. Pain. 2006;126:16–23. doi: 10.1016/j.pain.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Mollanazar NK, Smith PK, Yosipovitch G. Mediators of Chronic Pruritus in Atopic Dermatitis: Getting the Itch Out? Clin Rev Allergy Immunol. 2015 doi: 10.1007/s12016-015-8488-5. [DOI] [PubMed] [Google Scholar]
- Moore C, Cevikbas F, Pasolli HA, et al. UVB radiation generates sunburn pain and affects skin by activating epidermal TRPV4 ion channels and triggering endothelin-1 signaling. Proc Natl Acad Sci U S A. 2013;110:E3225–34. doi: 10.1073/pnas.1312933110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morita T, McClain SP, Batia LM, et al. HTR7 Mediates Serotonergic Acute and Chronic Itch. Neuron. 2015;87:124–38. doi: 10.1016/j.neuron.2015.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross SE. Pain and itch: insights into the neural circuits of aversive somatosensation in health and disease. Curr Opin Neurobiol. 2011;21:880–7. doi: 10.1016/j.conb.2011.10.012. [DOI] [PubMed] [Google Scholar]
- Weisshaar E, Dunker N, Rohl FW, et al. Antipruritic effects of two different 5-HT3 receptor antagonists and an antihistamine in haemodialysis patients. Exp Dermatol. 2004;13:298–304. doi: 10.1111/j.0906-6705.2004.00184.x. [DOI] [PubMed] [Google Scholar]
- Yang YS, Cho SI, Choi MG, et al. Increased expression of three types of transient receptor potential channels (TRPA1, TRPV4 and TRPV3) in burn scars with post-burn pruritus. Acta Derm Venereol. 2015;95:20–4. doi: 10.2340/00015555-1858. [DOI] [PubMed] [Google Scholar]