Introduction
Eccrine syringofibroadenoma (ESFA) is a rare neoplasm that usually presents as a solitary, often large, hyperkeratotic nodular lesion with predilection for the extremities. Histologically, there are thin anastomosing epithelial cords and strands forming a lattice and connected to the undersurface of the epidermis. Ducts are presented within the tumor. Between the strands, there is a rich fibrovascular stroma.
Eccrine syringofibroadenoma is typically a rare benign neoplasm. Eccrine syringofibroadenoma (ESFA) is of acrosyringeal or eccrine dermal duct differentiation. Histologically, there are multiple anastomosing cords of benign epithelial cells surrounded by a loose fibrovascular stroma. The epithelial cords demonstrate ductal differentiation. Occasional luminal eccrine ducts are noted within the anastomosing cords.
The authors describe two cases with different subtypes of ESFA, a solitary ESFA and a reactive ESFA with squamous cell carcinoma.
Case report
Patient 1
A 77-year-old Thai male patient presented with asymptomatic erythematous plaques on both soles for a year. The lesions had slowly extended from the middle of his soles to heels and medial part of the feet (Figure 1A). He denied history of previous trauma. The patient had valvular heart disease and coronary artery disease. He had undergone valve and coronary bypass surgery 10 years ago. He is currently on oral warfarin treatment.
Figure 1A.

The lesions slowly extended from the middle of the soles to the heels and medial part of the feet. [Copyright: ©2016 Temnithikul et al.]
Physical examination revealed bilateral, well-defined, firm, cobblestone-like, erythematous plaques on both soles with keratoderma.
Histological examination was obtained. The histopathology showed thin reticular strands of proliferating cells connected to the epidermis and extending into the dermis, anastomosing irregularly. Small eccrine ducts could be seen within the cords. The area between the strands was filled with richly vascular fibrous stroma. Perivascular infiltration with lymphocytes, plasma cells and mast cells were noted (Figure 1B and 1C).
Figure 1B.

Histopathologic findings. [Copyright: ©2016 Temnithikul et al.]
Figure 1C.
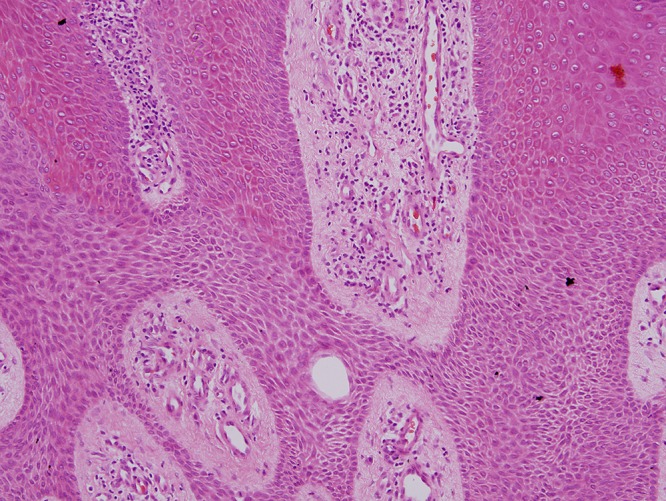
Histopathologic findings. [Copyright: ©2016 Temnithikul et al.]
Immunohistochemical staining was done. Positive staining was observed for epithelial membrane antigen (EMA) and carcinoembryonic antigen (CEA).
Patient 2
A 52-year-old Thai female patient presented with asymptomatic erythematous exophytic masses on the dorsum of her left foot (Figure 2A). She had gradually developed asymptomatic erythematous exophytic masses on her left foot for several years. A surgical excision was performed on the lesions one year ago. Histopathological diagnosis revealed squamous cell carcinoma. This patient had developed dome-shaped reddish exophytic masses on top of the surgical scar after surgery 6 months ago. She denied history of trauma and never had previous keloidal scars.
Figure 2A.

Erythematous exophytic masses on dorsum of the left foot. [Copyright: ©2016 Temnithikul et al.]
Physical examination revealed multiple well-defined firm dome-shaped exophytic erythematous masses on top of the surgical scar on the dorsum of her left foot.
Histological examination from the lesion was obtained and showed proliferation of atypical squamous cells extending to the superficial dermis. There was also aggregation of anastomosing slender elongated cords and strands of cuboidal cells embedded in fibrovascular stroma with a diagnosis of recurrent squamous cell carcinoma with eccrine syringofibroadenoma at the periphery of the specimen (Figure 2B and C).
Figure 2B.

Histopathologic findings. [Copyright: ©2016 Temnithikul et al.]
Figure 2C.

Histopathologic findings. [Copyright: ©2016 Temnithikul et al.]
Immunohistochemical staining was done. Positive staining was observed for epithelial membrane antigen (EMA) and carcinoembryonic antigen (CEA).
Discussion
Eccrine syringofibroadenoma (ESFA) (synonym: syringofibroadenoma, eccrine syringofibroadenomatous hyperplasia [1], acrosyringeal adenomatosis [2]) is a rare benign adnexal tumor arising most often on the extremities of elderly individuals with characteristic histopathology. The tumor consists of anastomosing cords of cuboidal epithelial cells surrounded by a fibrovascular stroma containing plasma cells and ductal structures [3]. Although the exact site of origin of ESFA remains controversial, it is believed to be derived from the acrosyringium or eccrine dermal duct. ESFA stains positively with epithelial membrane antigen (EMA) and carcinoembryonic antigen (CEA). Cytokeratin studies have been inconsistent [4]. Human papillomavirus 10 (HPV-10) may also play a role in the development of eccrine syringofibroadenomas. Cases of ESFA have been divided into five distinct subtypes due to clinical manifestations: solitary lesions, multiple lesions associated with an ectodermal dysplasia, lesions with no additional cutaneous pathology, nevoid lesions, and reactive lesions:
Solitary ESFA is typically a nonhereditary solitary nodule or verrucous mass normally found on the lower extremities of the middle-aged and elderly.
Multiple ESFA without associated cutaneous finding (eccrine syringofibroadenomatosis) are nonfamilial palmoplantar lesions without significant associated cutaneous finding.
Multiple ESFA with hidrotic ectodermal dysplasia (HED) presents in two different variants, Schöpf-Schulz-Passarge syndrome and Clouston’s syndrome. Schöpf-Schulz-Passarge syndrome (SSPS) is a rare autosomal dominant ectodermal dysplasia, characterized by hypodontia, hypotrichosis, nail dystrophy, palmoplantar keratoderma, and periocular and eyelid margin apocrine hidrocystoma. Clouston’s syndrome is autosomal dominant ectodermal dysplasia, characterized by dystrophic nails and sparse hair. HPV-10 has been detected in the lesions occurring in Clouston’s syndrome [5].
Nevoid ESFA (nonfamilial unilateral linear ESFA) is a rare genetic mosaicism, producing diffuse plantar hyperkeratosis. It may be the result of a somatic mutation in the early embryonic stage.
Reactive ESFA associated with inflammatory or neoplastic dermatosis is often in an acral location. This reactive change has been seen next to burn scar ulcer, erosive palmoplantar lichen planus [6], hidrotic ectodermal dysplasia, bullous pemphigoid [1], diabetes mellitus with polyneuropathy and chronic ulcer, inflammatory psoriasis or persistent local infection, lymphedema (elephantiasis), nevus sebaceous and squamous cell carcinoma. The pathogenesis may be associated with a specific type of eccrine duct remodeling or repair.
The co-existence of ESFA and squamous cell carcinoma has been reported [4,7]. It is unclear whether ESFA develops in response to squamous cell carcinoma or squamous cell carcinoma represents a malignant degeneration of ESFA. The incidence of squamous cell carcinoma arising in ESFA is unknown. The histologic picture of coexistence of ESFA and squamous cell carcinoma have appeared as squamous cell carcinoma with ductal differentiation impinged by benign ESFA and squamous cell carcinoma surrounded by ESFA. The malignant degeneration of ESFA has been termed as eccrine syringofibrocarcinoma (ESFAC) [7–9]. The mechanisms of underlying malignant transformation remain unclear. It is recommended that ESFA be completely excised to prevent malignant degeneration, although the risk of this occurrence is unknown. Recurrences and metastatic disease have not been reported. Excision appears to be the definitive treatment. Trauner et al reported a patient with ESFA successfully treated with a dual pulse width flashlamp pumped pulsed dye laser [10].
In conclusion, the authors show two rare cases of eccrine syringofibroadenoma (ESFA) with different clinical manifestations. Patient 1 was diagnosed with ESFA by histological findings. The immunohistochemical demonstration was consistent with ESFA. He had no associated findings or sign of ectodermal dysplasia and he was therefore classified as multiple EFSA without associated cutaneous findings. Patient 2 was classified as reactive ESFA and diagnosed as ESFA with squamous cell carcinoma by typical histological and immunohistological findings. Excision of the ESFA was the definitive treatment to prevent the malignant degeneration. Mohs surgery was done for squamous cell carcinoma. She has been evaluated with a complete skin examination every 6 months.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
All authors have contributed significantly to this publication.
References
- 1.Nomura K, Hashimoto I. Eccrine syringofibroadenoma in two patients with bullous pemphigoid. Dermatology. 1997;195:395–8. doi: 10.1159/000245997. [DOI] [PubMed] [Google Scholar]
- 2.Hara K, Mizuno E, Nitta Y, Ikeya T. Acrosyringeal adenomatosis (eccrine syringofibroadenoma of Mascaro). A case report and review of the literature. Am J Dermatopathol. 1992;14:328–39. doi: 10.1097/00000372-199208000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Starink TM. Eccrine syringofibroadenoma: Multiple lesion representing a new cutaneous marker of the Schöpf syndrome, and solitary nonhereditary tumors. J Am Acad Dermatol. 1997;36:569–76. doi: 10.1016/s0190-9622(97)70245-7. [DOI] [PubMed] [Google Scholar]
- 4.Schadt CR, Boyd AS. Eccrine syringofibroadenoma with coexistent squamous cell carcinoma. J Cutan Pathol. 2007;34:71–4. doi: 10.1111/j.1600-0560.2007.00740.x. [DOI] [PubMed] [Google Scholar]
- 5.Carlson JA, Rohwedder A, Daulat S, Schwartz J, Schaller J. Detection of human papillomavirus type 10 DNA in eccrine syringofibroadenomatosis occurring in Clouston’s syndrome. J Am Acad Dermatol. 1999;40:259–62. doi: 10.1016/s0190-9622(99)70201-x. [DOI] [PubMed] [Google Scholar]
- 6.French LE, Masgrau E, Chavaz P, Saurat JH. Eccrine syringofibroadenoma in a patient with erosive palmoplantar lichen planus. Dermatology. 1997;195:399–401. doi: 10.1159/000245998. [DOI] [PubMed] [Google Scholar]
- 7.Bjarke T, Ternesten-Bratel A, Hedblad M, Rausing A. Carcinoma and eccrine syringofibroadenoma: a report of five cases. J Cutan Pathol. 2003;30:382–92. doi: 10.1034/j.1600-0560.2003.00072.x. [DOI] [PubMed] [Google Scholar]
- 8.González-Serva A, Pró-Rísquez MA, Oliver M, Caruso MG. Syringofibrocarcinoma versus squamous cell carcinoma involving syringofibroadenoma: is there a malignant counterpart of Mascaro’s syringofibroadenoma? Am J Dermatopathol. 1997;19:58–65. doi: 10.1097/00000372-199702000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Katane M, Akiyama M, Ohnishi T, Watanabe S, Matsuo I. Carcinomatous transformation of eccrine syringofibroadenoma. J Cutan Pathol. 2003;30:211–4. doi: 10.1034/j.1600-0560.2003.00039.x. [DOI] [PubMed] [Google Scholar]
- 10.Trauner MA, Narurkar VA, Ruben BS. Eccrine syringofibroadenoma treated with a dual pulse width flashlamp pumped pulsed dye laser. Dermatol Surg. 1999;25:418–20. doi: 10.1046/j.1524-4725.1999.08278.x. [DOI] [PubMed] [Google Scholar]


