Abstract
Background
Steam inhalation has long been considered a beneficial home remedy to treat children with viral respiratory tract infections, but there is no evidence to suggest a benefit and children are at risk of serious burn injuries.
Aim
To determine the demographics, mechanism, management, and costs of steam inhalation therapy scalds to a regional burns centre in the UK, and to ascertain whether this practice is recommended by primary care providers.
Design and setting
A retrospective study of all patients admitted to a regional burns centre in Swansea, Wales, with steam inhalation therapy scalds.
Method
Patients who attended the burns centre for steam inhalation therapy scalds between January 2010 and February 2015 were identified using the burns database and data on patient demographics, treatment, and costs incurred were recorded. In addition, an electronic survey was e-mailed to 150 local GPs to determine whether they recommended steam inhalation therapy to patients.
Results
Sixteen children attended the burns centre with steam inhalation scalds. The average age attending was 7.4 years (range 1–15 years) and, on average, three children per year were admitted. The most common indication was for the common cold (n = 9). The average size of the burns was 3.1% (range: 0.25–17.0%) of total body area. One child was managed surgically; the remainder were treated with dressings, although one patient required a stay in a high-dependency unit. The total cost of treatment for all patients was £37 133. All in all, 17 out of 21 GPs surveyed recommended steam inhalation to their patients; eight out of 19 GPs recommended it for children aged <5 years.
Conclusion
Steam inhalation incurs a significant cost to patients and the healthcare system. Its practice continues to be recommended by GPs but children, due to their limited motor skills, curiosity, and poor awareness of danger, are at significant risk of burn injuries and this dangerous practice should no longer be recommended.
Keywords: burns, inhalation, paediatrics, scald, steam
INTRODUCTION
Traditionally, steam inhalation has been used to treat common respiratory infections; its use is believed to alleviate symptoms of blocked nasal passages. The administration methods include direct inhalation from boiling water placed in a bowl (often mixed with menthol or eucalyptus) or the use of a commercially available vaporiser, within which water is heated in a reservoir and then emitted into a room or directly into the nasal mucosa.
NHS Choices recommends ‘inhaling steam from a bowl of hot (but not boiling) water’ to relieve nasal congestion.1 Despite evidence suggesting no consistent benefits of steam inhalation, it remains a widely practised home remedy.2,3 Scalds remain the most common form of burn injury in the paediatric population and scalds secondary to steam inhalation therapy have been widely reported in the literature.3–6 Studies highlighting the dangers of steam inhalation date back to 1969 and have been published worldwide.7
This study reports on a case series of burn injuries sustained as a result of therapeutic steam inhalation and treated at a regional burns centre in Swansea, Wales. The aim of the study was to review the mechanism, management, and cost of steam inhalation therapy burns, along with the demographics of patients attending with such burns. In addition, a survey of local GPs was undertaken to evaluate their perspectives on steam inhalation and to ascertain whether this was a practice they recommended to patients. No previous GP surveys relating to steam inhalation therapy were identified in the literature.
METHOD
The study was conducted at the Welsh Centre for Burns and Plastic Surgery, based at Morriston Hospital in Swansea, Wales. A retrospective analysis of patients aged ≤16 years was conducted for the period between January 2010 and February 2015. Patients admitted or treated following steam inhalation injuries were identified from the burns database. Those attending with steam inhalation scalds were coded as such and so could be identified retrospectively.
The patients’ clinical notes, discharge summary, and database entries were accessed to record the clinical data. Data were recorded on a Microsoft Excel sheet and included:
patient demographics, including ethnicity;
date of admission and discharge;
mechanism and total body surface area (TBSA) of burn injury;
anatomical area of burn injury;
first aid given;
treatment given;
dressings used;
inpatient stay; and
outpatient follow-up.
How this fits in
Children with viral respiratory tract infections are often treated using the home remedy of steam inhalation therapy. International studies have highlighted a lack of efficacy using this treatment and a high risk of burn injuries. This study highlights a British experience of steam inhalation burns including the management, costs, and GPs’ perspectives. The findings highlight the importance of prevention and raising awareness among healthcare providers so this dangerous practice is no longer recommended.
In addition, to determine the cost of the treatment, records maintained by the health board finance department were accessed. The financial costs of treatment were calculated using predetermined hospital standard tariffs — such as those for a single-day stay in a ward, single outpatient appointment, and number and type of operative procedures performed — and coded accordingly. Microsoft Excel and Access were used for analysis.
GPs were identified from two regional health board intranet address books. A total of 150 local GPs were e-mailed the survey, which comprised eight questions on their knowledge of, and advice regarding, steam inhalation therapy.
RESULTS
Demographics
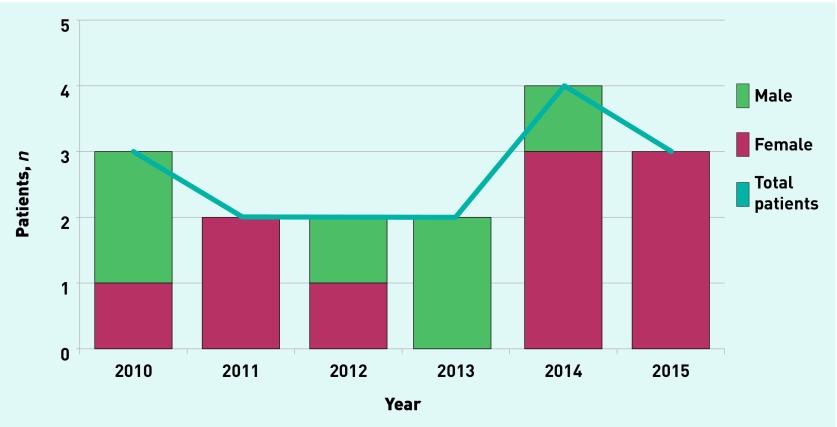
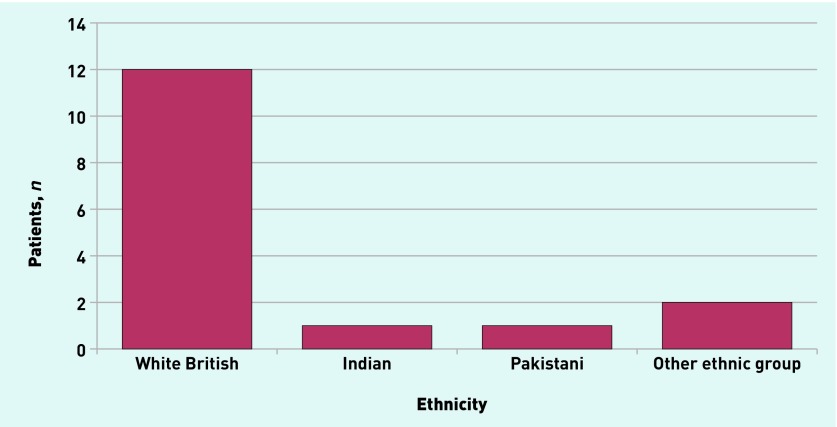
During the 5-year period, a total of 16 patients were treated at the centre with steam inhalation-related burn injuries: an average of three patients per year. Ten patients were female and six were male (Figure 1). The mean age was 7.43 years (range 1–15 years). Twelve of the patients were white British, with the remaining four being Indian, Pakistani, or from other ethnic groups (Figure 2).
Patients treated for steam inhalation-related burns at the Welsh Centre for Burns and Plastic Surgery, 2010–2015.
Figure 2.
Ethnicity of patients presenting with steam inhalation scalds.
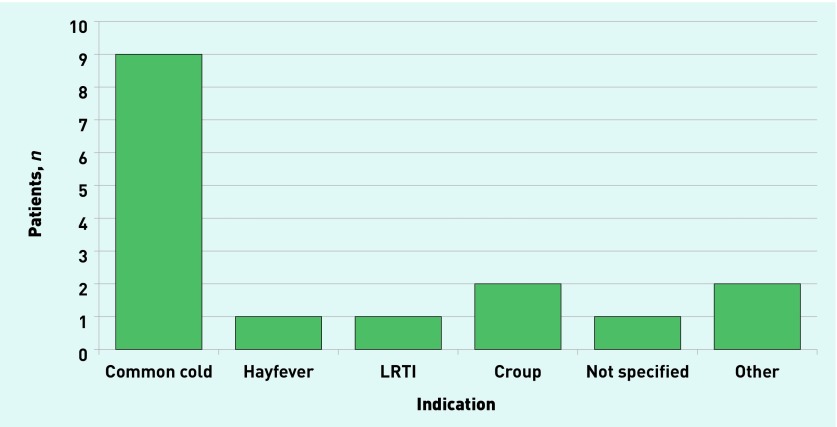
The annual trend of steam inhalation scalds did not change substantially over the study period. There has been a slight increase over the last 2 years, although, due to the low overall numbers, no inferences can be made regarding this. The indications for using steam inhalation were:
common cold (n = 9);
croup (n = 2);
lower respiratory tract infections (n = 1);
hayfever (n = 1);
other (n = 2); and
unspecified (n = 1) (Figure 3).
Figure 3.
Indications for administration of steam inhalation therapy. LRTI = lower respiratory tract infection
First aid was administered by parents to 13 patients, using cold water or soaks. In one patient, toothpaste was used for first aid; two patients did not receive any first aid.
Burns and treatment
Table 1 summarises the demographics, mechanism, indication, and anatomical area affected in each of the 16 steam inhalation burns cases managed at the unit.
Table 1.
Demographics, indication of steam inhalation, mechanism, and anatomical area of burn injury
| Year | Age, years | Sex | Indication | Mechanism | Anatomical area |
|---|---|---|---|---|---|
| 2010 | 10 | Female | LRTI | Boiling water | Left hand, left thigh |
| 2010 | 4 | Male | Croup | Facial steamer + boiling water | Left thigh |
| 2010 | 4 | Male | Croup | Boiling water | Left forearm and left elbow |
| 2011 | 13 | Female | Not specified | Boiling water | Both legs, groin |
| 2011 | 10 | Female | Hayfever | Boiling water | Both thighs, perineum |
| 2012 | 1 | Female | Coryza | Boiling water + Vicks® VapoRub | Left thigh, buttock |
| 2012 | 2 | Male | Cold | Boiling water | Right thigh |
| 2013 | 15 | Male | Cold | Boiling water | Both thighs, penis, scrotum, abdomen, both hands |
| 2013 | 13 | Male | Cold | Boiling water + Olbas® Oil | Abdomen, genitalia |
| 2014 | 2 | Female | Cold | Steam inhaler + boiling water | Medial left thigh, right middle and ring finger |
| 2014 | 15 | Female | Cold | Boiling water | Both lower legs, both feet |
| 2014 | 6 | Female | Cold | Boiling water | Right buttock |
| 2014 | 14 | Male | Cold and headache | Boiling water + lemon juice | Left dorsum foot |
| 2015 | 1 | Female | Cold | Boiling water + Olbas Oil | Left hand (palm) |
| 2015 | 2 | Female | Temperature and cough | Boiling water | Face, right chest, right leg, left arm |
| 2015 | 7 | Female | Cold | Boiling water + mint | Both thighs, buttocks, left leg, abdomen |
LRTI = lower respiratory tract infection.
The mean TBSA involved was 3.1% (range 0.25–17.0%). Fourteen patients had only partial-thickness burns and the remaining two had mixed-depth burns. Of the two patients with mixed-depth burns, one had 0.15% and the other 1% full-thickness burns.
Anatomically, two-thirds of the burns were sustained over the thighs (n = 11), followed by groin/genitals and legs (n = 4 for each area). Thigh/leg burns were the commonest burns in both the 0–5 years (n = 5/7) and >5 years (n = 6/9) age groups. Groin/genitalia burns were the next most common burns occurring in the >5 year age group. Potential mechanisms of the burns are:
spillage of hot water from a bowl placed on a child’s lap; or
the child accidentally kicking or dropping the bowl, or falling into it.
Table 2 highlights the management, affected TBSA, burn depth, dressing type, and time to heal in each case. Only one patient, who had mixed-thickness burns (4.5% TBSA) to the left thigh and buttock, required debridement and skin grafting in theatre. The remaining patients were managed conservatively. One patient, with a superficial partial-thickness scald (17% TBSA) to the thighs, buttocks, and legs, required urinary catheterisation, fluid resuscitation, and several days’ stay on the burns high-dependency unit.
Table 2.
Characteristics and management of burn injuries
| Year | Management | TBSA, % | Deep dermal/full-thickness burn, % | Dressing | Heal time, days |
|---|---|---|---|---|---|
| 2010 | Conservative | 0.5 | 0 | Mepilex Ag | 4 |
| 2010 | Conservative | 2 | 0 | Mepilex Ag | 7 |
| 2010 | Conservative | 1 | 0 | Mepilex Ag | 7 |
| 2011 | Conservative | 6 | 0.15 | Mepilex Ag + Flamazine | 10 |
| 2011 | Conservative | 2.5 | 0 | Mepilex Ag + Flamazine | NS |
| 2012 | Theatre: debridement and sheet graft to left thigh | 4.5 | 1 | Flamazine | 50 |
| 2012 | Conservative | 0.5 | 0 | Mepilex Lite | 25 |
| 2013 | Conservative | 7.5 | 0 | Mepilex Lite | 60 |
| 2013 | Conservative | 0.25 | 0 | Mepilex Lite | NS |
| 2014 | Conservative | 0.25 | 0 | Mepilex Ag | 14 |
| 2014 | Conservative | 0.5 | 0 | Mepilex Ag | 11 |
| 2014 | Conservative | 1 | 0 | Mepilex Lite | 13 |
| 2014 | Conservative | 1 | 0 | Mepilex Ag | 9 |
| 2015 | Conservative | 1.5 | 0 | Mepilex Ag + Bactigras | 11 |
| 2015 | Conservative | 4 | 0 | Mepilex Ag | 55 |
| 2015 | Conservative | 17 | 0 | Mepilex Ag | 45 |
NS = not specified. TBSA = total body surface area.
Predominantly, Mepilex® Ag (Mölnlycke Health Care) and Mepilex Lite (Mölnlycke Health Care) were used to dress burns. In two patients, Flamazine™ (Smith & Nephew) was used before switching to silver-based dressings, and Bactigras™ (Smith & Nephew) was used in one patient.
In 14 patients, the average healing time for burn injuries was 22.92 days; this included the patient who required a trip to theatre, although complete healing was not documented for two patients (Table 2). None of these 14 patients had any permanent scarring except for the patient that underwent skin grafting.
Hospital stay and cost
Ten of the 16 patients required hospital admission. The average hospital stay was 2.7 days (range: 1–14 days) and the average cost of treatment £3094 (range: £75–£17 242). The cost of treatment was not available for four patients. The highest cost of treatment was £17 242; this was for a 7.5% TBSA partial-thickness burn, which was managed conservatively. The total cost of treatment for all patients was £37 133. The costs reported exclude the cost of treating these injuries in the emergency department.
Survey
Of the 150 GPs who were e-mailed the survey, 21 (14.0%) responded. Results, which are outlined in Table 3, revealed that the majority (n = 17, 81.0%) had advised patients to use steam inhalation at some point in their career. It is a concern that eight out of 19 GPs recommended steam inhalation therapy to children aged 0–5 years. Only a small proportion of GPs were aware of evidence relating to the use of steam inhalation and none was aware of the 2013 Cochrane review.8 Five out of 21 GPs reported the potential risk of scalds using steam inhalation.
Table 3.
GPs’ (n = 21) knowledge of, and advice about, steam inhalation
| Question | Responders, % |
|---|---|
| Have you ever advised a patient to use steam inhalation? | |
| Yes | 81 |
| No | 19 |
|
| |
| At what age would you advise the use of steam inhalation?a | |
| 0–2 years | 42 |
| >2–5 years | 42 |
| >5–10 years | 47 |
| >10–15 years | 47 |
| Adults (≥16) | 90 |
|
| |
| How would you advise a patient to apply the steam inhalation?a | |
| Towel over head | 47 |
| Directly to face | 0 |
| Sit in steamy room | 53 |
|
| |
| How would you advise preparation of the water for the steam?a | |
| Using kettle | 53 |
| Using hob | 0 |
| Other | 47 |
| Steamy bathroom | 26 |
|
| |
| Are you aware of any evidence supporting the use of steam inhalation?b | |
| Yes | 10 |
| Topic in British Medical Journal | 5 |
| Anecdotal | 5 |
| No | 90 |
|
| |
| Are there any contraindications for the use of steam inhalation? | |
| Yes | 43 |
| Risk of scalding | 24 |
| Poor dexterity | 5 |
| Facial skin eczema | 5 |
| No | 57 |
|
| |
| Are there any particular additional agents that you advise for use during steam inhalation? | |
| Yes | 57 |
| Olbas® Oil | 38 |
| Vicks® VapoRub | 19 |
| Menthol | 24 |
| No | 43 |
|
| |
| What are the indications for advising steam inhalation? | |
| Upper respiratory tract infection | 24 |
| Lower respiratory tract infection | 0 |
| Sinusitis | 43 |
| Other | 33 |
| Bronchiolitis | 5 |
| Croup | 5 |
n = 19.
n = 20.
DISCUSSION
Summary
This study confirms that, despite the considerable risk of paediatric scalds with steam inhalation, as highlighted in previous articles,5–7,9–11 this practice continues to be advocated in primary care. Physicians may recommend it in light of favourable anecdotal experiences rather than a solid evidence base, even though burns often lead to significant adverse effects, such as psychological distress.
Steam for therapy can be delivered by commercially made vaporisers or by using a bowl of hot water and using a towel to contain the steam or vapours.6 In this study, patients mostly used bowls with hot water at home; only two patients used a steam inhaler.
In the majority of cases, first aid was given appropriately, possibly reducing the severity of the injury, although one parent applied toothpaste as a form of first aid. The authors did not find any evidence or any recommendation for using toothpaste as first aid in a burn injury and it is believed it can potentially cause harm by possibly contributing to further tissue destruction.12
The mechanism of hot water spillage from a bowl on a child’s lap, or a child kicking or falling into a bowl of hot water, explains the most common anatomical sites affected: the thigh/leg and the groin/genitalia. Older children may more commonly burn their groin/genitalia as they balance hot water on their laps. Younger children (<5 years) were less likely to scald this site. The mean age affected in the current study was 7 years. This contrasts with the average age of 1 year, in the study by Wallis and colleagues on an Australian patient group,6 where young children were more commonly burned on commercial vaporiser devices. The majority of patients in the current study were managed conservatively with dressings (15/16) and one patient was managed surgically. Costs were mainly incurred because of the multiple attendances for dressing changes and the days of inpatient stay in hospital. On average, children were admitted for 2.7 days.
Strengths and limitations
This study utilised costing for standard tariffs to estimate as closely as possible the costs associated with steam inhalation burns. However, the exact economic costs incurred could not be calculated due to missing data.
Although the authors aimed to collect comprehensive data on patients with steam inhalation therapy scalds and used the burns database to identify as many of these patients as possible, some may have not been identified in the database and would have, therefore, been omitted from the study. In addition, a number of patients with scalds may have not attended this regional burns unit; these individuals may have been treated at home, managed by their GP, or attended their local hospital only.
The authors acknowledge that the overall response rate for the GP survey was poor and, as such, the findings may not be fully representative. E-mails were sent but the authors believe that, due to high workloads, GPs may not have had time to respond. However, although the GP survey had a small sample size and a low response rate it demonstrates that the current perspective of a number of GPs is to advocate this dangerous practice.
Figure 4.
Mixed-thickness burn to patient’s thigh resulting from administration of steam inhalation therapy.
Comparison with existing literature
Studies by various authors report a range of mean TBSA (5–11%) of burn injury following steam inhalation.5,6,9 Mean TBSA in this study was 3.1% and mostly consisted of partial-thickness burns; as such, the findings are fairly similar to those of other studies.
In the current study, the thigh/leg was the most common site scalded. This is similar to other studies identified in the literature.6,9
Wallis and colleagues investigated the mechanism of burn injuries and presented burns secondary to the spillage of boiling water and those sustained when the heat source was touched.6 In the current case series, the mechanism of the burn also involved spillage of hot water, because of the tendency to place the bowl in the patient’s lap or because the patient had accidentally kicked, dropped, or fallen into the bowl.
As in the study presented here, surgical intervention and skin grafting for steam inhalation burns have been reported in the literature: Murphy and colleagues reported surgical intervention and scarring in four out of seven children;10 in Wallis and colleagues’ study, two children out of 17 underwent skin grafting after burns sustained by spilling hot water and were hospitalised for a period of time thereafter,6 whereas Baartmans and colleagues reported skin grafting in six of 16 patients.9 In this current study, only one patient required debridement and split thickness skin grafting in theatre.
Baartmans and colleagues reported a mean hospital stay of 9.8 days,9 Wallis and colleagues 9.2 days,6 Ebrahim and colleagues 14.7 days,11 and Belmonte and colleagues14 days.5 The average hospital stay in the study presented here was 2.7 days. The location of the burns necessitating such action — often around sensitive areas such as the groin or genitals — makes them particularly challenging to treat, requires regular dressing changes, and makes toileting difficult; this was often the reason for admission.
The Cochrane review published in 2013 evaluated the use of commercial vaporisers, also known as rhinotherms, and highlighted no improvement in object measures, although symptomatic relief was reported in some studies.8 However, no comment was made on the potential risks of paediatric scalds, which are known to occur following the commonly used method of administering steam inhalation, using a bowl of boiling water. The current study highlighted that considerable harm may result following burns from steam inhalation therapy.
The cost of treatment of burn injuries is high.4 The average cost of treatment of steam inhalation therapy burns per patient in the study presented here was £3094. In a similar study by Baartmans and colleagues, the total cost of treatment of steam inhalation therapy burns was higher at £44 500. The difference in cost is primarily due to the higher number of patients who required surgical intervention and an intensive therapy unit (ITU) stay in the study by Baartmans and colleagues, compared with the study presented here, in which all but one patient were managed conservatively and none required an ITU stay.10 No other study was found that reported the cost of steam inhalation burn injuries.
Implications for practice
Steam inhalation is postulated to provide relief of respiratory congestion by loosening respiratory secretions,13 but there is a lack of evidence to support the improvement in objective outcome measures such as viral titres in nasal washings.2
The hazards and costs of steam inhalation to the UK have not previously been estimated. Significant costs, both emotional and economic, are incurred from steam inhalation burns. Rarely, children may develop life-threatening infections from staphylococcal toxic shock syndrome. Emotional costs include the patient’s or parent’s pain and anxiety. The economic costs to the hospital must also be considered, as well as the costs to society resulting from parents being absent from work.
There is also a lack of awareness among primary care physicians of the potential risks of burns associated with steam inhalation therapy; NHS Choices recommends ‘inhaling steam from a bowl of hot (but not boiling) water’ despite the lack of evidence to suggest that this is beneficial. The results of the study presented here demonstrate that steam inhalation therapy continues to be advocated and administered, despite the risks of injury that are associated with it. As such, strategies to prevent steam inhalation burns occurring should be implemented by health professionals. These include:
not recommending the practice to parents;
advising parents of the dangers associated with it; and
informing parents of the lack of evidence demonstrating that it has any beneficial effects for patients.
As burns surgeons and paediatricians, the authors aim to promote awareness of both primary care professionals and the public to reduce the risk of therapeutic steam inhalation burns.
Acknowledgments
Sarah Al Himdani and Muhammad Umair Javed are joint first authors. The authors thank Alyson Huntley for her assistance in review of data extraction.
Funding
None.
Ethical approval
A formal ethical review was not required and appropriate letters of exemption were obtained from the Joint Study Review Committee (JSRC) (3 June 2015), Abertawe Bro Morgannwg University Health Board.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Patient consent
Patient consent for publication of the image has been obtained.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.NHS Choices Home remedies for common conditions. http://www.nhs.uk/Livewell/Pharmacy/Pages/home-remedies-for-common-conditions.aspx (accessed 1 Feb 2016).
- 2.Singh M. Heated, humidified air for the common cold. Cochrane Database Syst Rev. 2006;19(3):CD001728. doi: 10.1002/14651858.CD001728.pub3. [DOI] [PubMed] [Google Scholar]
- 3.Mathew JL. Steam inhalation in respiratory illnesses — full steam ahead or full stop? A systematic review of randomized controlled trial. Indian Pediatr. 2010;47(12):1047–1050. doi: 10.1007/s13312-010-0168-1. [DOI] [PubMed] [Google Scholar]
- 4.Koompirochana V, Javed MU, Eales M, Hemington Gorse S. Ten year epidemiology and cost analysis of paediatric burns undergoing fluid resuscitation and treatment at the Welsh Centre for Burns and Plastic Surgery. http://www.medbc.com/annals/review/vol_28/num_3b/text/vol28n3bp247.htm (accessed 1 Feb 2016).
- 5.Belmonte JA, Domínguez-Sampedro P, Pérez E, et al. [Severe burns related to steam inhalation therapy]. [In Spanish] An Pediatr (Barc) 2015;82(2):95–99. doi: 10.1016/j.anpedi.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Wallis BA, Turner J, Pearn J, Kimble RM. Scalds as a result of vapour inhalation therapy in children. Burns. 2008;34(4):560–564. doi: 10.1016/j.burns.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 7.Meuwly J. [Burns in children caused by steam air humidifier]. [In German] Helv Chir Acta. 1969;36(1):152–154. [PubMed] [Google Scholar]
- 8.Singh M, Singh M. Heated, humidified air for the common cold. Cochrane Database Syst Rev. 2013;6:CD001728. doi: 10.1002/14651858.CD001728.pub5. [DOI] [PubMed] [Google Scholar]
- 9.Baartmans M, Kerkhof E, Vloemans J, et al. Steam inhalation therapy: severe scalds as an adverse side effect. Br J Gen Pract. 2012 doi: 10.3399/bjgp12X652337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murphy SM, Murray D, Smith S, Orr DJ. Burns caused by steam inhalation for respiratory tract infections in children. BMJ. 2004;328(7442):757. doi: 10.1136/bmj.328.7442.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ebrahim MK, Bang RL, Lari AR. Scald accidents during water aerosol inhalation in infants. Burns. 1990;16(4):291–293. doi: 10.1016/0305-4179(90)90142-j. [DOI] [PubMed] [Google Scholar]
- 12.Skinner A, Peat B. Burns treatment for children and adults: a study of initial burns first aid and hospital care. NZ Med J. 2002;115(1163):U199. [PubMed] [Google Scholar]
- 13.Sanu A, Eccles R. The effects of a hot drink on nasal airflow and symptoms of common cold and flu. Rhinology. 2008;46(4):271–275. [PubMed] [Google Scholar]