Abstract
Background
Little is known about attitudes toward and experiences with opioid maintenance therapy (OMT) among people who inject drugs in Malaysia, a country where people who inject drugs comprise 1.3% of the adult population.
Methods
In 2010, 460 people who inject drugs in Greater Kuala Lumpur, Malaysia were surveyed to evaluate attitudes toward and experience with OMT and treatment readiness. Attitudes towards OMT with both methadone and buprenorphine were assessed using an opinions scale. Multivariable linear regression was used to assess correlates of treatment readiness, measured with the 19-item Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES).
Results
All 460 participants used opioids and nearly all (99.1%) met criteria for opioid dependence. Few had had previous experience with methadone (9.3%) or buprenorphine (12.6%) maintenance therapy, yet many had used methadone (55.2%) or buprenorphine (51.7%) outside of treatment settings. Fifteen percent had injected buprenorphine in the past month, and of the few that were currently receiving buprenorphine maintenance therapy, almost all were injecting it. The majority of subjects exhibited a moderate level of treatment readiness and a preference for methadone over buprenorphine. Those with low treatment readiness scores were more likely to have previous experience with compulsory drug detention centers (p<0.01), needle/syringe exchange programs (p<0.005), or be of Indian ethnicity (p<0.001). Past use of methadone (p<0.01), older age (p<0.001), stress symptom severity (p<0.001), and sharing of needles or syringes (p<0.05) were associated with higher treatment readiness scores.
Conclusion
There are suboptimal levels of OMT experience among people who inject drugs that may be improved by addressing factors that influence patient attitudes. Those individuals with moderate treatment readiness may be targeted by brief motivational and cognitive interventions in primary care, prisons or OMT clinics aimed at improving entry into and retention in treatment.
Keywords: Opioids, methadone, buprenorphine, opioid substitution therapy, SOCRATES, treatment readiness
1. INTRODUCTION
1.1. Opioid dependence and treatment in Malaysia
Globally, people who inject drugs (PWID) experience elevated morbidity and mortality, primarily related to opioid use (L. Degenhardt, et al., 2013b). Opioids contribute to profound health and economic consequences for both individuals and society (F.L. Altice, Kamarulzaman, Soriano, Schechter, & Friedland, 2010; Mathers, et al., 2010). In Malaysia, where opioids are the most commonly injected substances, 1.3% of adults are PWID, or about 170,000 individuals, which is among the highest rates of injection drug use globally (Bachireddy, et al., 2011; Louisa Degenhardt, et al., 2008; Fu, Bazazi, Altice, Mohamed, & Kamarulzaman, 2012; Mathers, et al., 2008). Among PWID in Malaysia, HIV prevalence is estimated at 15.9–19.0% (Ngadiman, 2014; Bazazi, 2014). Unlike the remainder of Southeast Asia where HIV-related mortality has decreased, HIV-related mortality has increased in Malaysia (Joint United Nations Programme on HIV/AIDS (UNAIDS), 2014), primarily related to inadequate access to harm reduction and antiretroviral therapy (ART) for PWID (L. Degenhardt, et al., 2013a). Until recently, the primary approach to address addiction in Malaysia was detention in prisons or compulsory drug detention centers (CDDCs), where evidence-based treatment for opioid dependence is not available (Fu, et al., 2012; Reid, Kamarulzaman, & Sran, 2007).
The high relapse rates following detention in CDDCs and other non-evidence-based approaches and a high HIV prevalence among PWID led the Malaysian government in 2005 to introduce evidence-based HIV prevention strategies that included both needle/syringe exchange programs (NSEPs) and opioid maintenance therapy (OMT) (Mesquita, et al., 2008; Reid, et al., 2007). Buprenorphine maintenance therapy (BMT) was introduced in 2006; however, this was followed by problems with diversion and misuse via injection, leading to its withdrawal from the market and replacement with co-formulated buprenorphine/naloxone in 2007 (R. D. Bruce, et al., 2008b; R. D. Bruce, Govindasamy, Sylla, Kamarulzaman, & Altice, 2009; Vicknasingam, Mazlan, Schottenfeld, & Chawarski, 2010). Methadone maintenance therapy (MMT) was introduced in 2006 (Noordin, Merican, Rahman, Lee, & Ramly, 2008; Razali, 2008), with a three-phase MMT expansion to addiction specialty clinics, primary care settings and then prisons (Sharifa Ezat, Noor Azimah, Rushidi, Raminder, & Ruhani, 2009; Wickersham, Marcus, Kamarulzaman, Zahari, & Altice, 2013a). Despite global recognition of the effectiveness of OMT for treating opioid dependence and preventing transmission of blood-borne infections, access to OMT in low- and middle-income countries like Malaysia is limited, and barriers to implementation persist (L. Degenhardt, et al., 2013a; Wolfe, Carrieri, & Shepard, 2010).
1.2. Opioid maintenance therapy for treatment of opioid dependence
Treatment of opioid dependence with MMT or BMT is an evidence-based practice that reduces opioid use, criminal behavior, HIV risk behaviors and consequently HIV transmission (Richard P Mattick, Breen, Kimber, & Davoli, 2009; R. P. Mattick, Kimber, Breen, & Davoli, 2008). For HIV-infected patients, OMT also contributes to improved HIV treatment outcomes, from diagnosis to linkage and retention in antiretroviral therapy (F. L. Altice, et al., 2011; F.L. Altice, et al., 2010; Binford, Kahana, & Altice, 2012; Thompson, et al., 2012; Kamarulzaman, 2015). BMT has similar efficacy as MMT, although retention is improved by using higher doses of methadone (Amato, et al., 2005; R. P. Mattick, et al., 2008). Methadone, however, has also been documented to have more adverse side effects and pharmacokinetic drug interactions (Chou, et al., 2014; Saber-Tehrani, Bruce, & Altice, 2011; Weimer & Chou, 2014), especially with antiretroviral therapy (F.L. Altice, et al., 2010; R. D. Bruce, Moody, Altice, Gourevitch, & Friedland, 2013; Saber-Tehrani, et al., 2011).
1.3. The importance of attitudes of people who inject drugs toward opioid maintenance therapy
Factors beyond the individual can limit OMT utilization; however, as access to OMT increases, individual attitudes and stigma toward OMT become more relevant barriers to treatment entry and retention (Wolfe, et al., 2010; Jin, et al., 2014). Although both MMT and BMT are effective, patients often have strong preferences for a particular medication (Kelly, et al., 2012; R. P. Schwartz, et al., 2008a; Zule & Desmond, 1998). A study of attitudes toward OMT can identify barriers to entry and retention in treatment that could be targeted by future interventions. Additionally, characterizing treatment readiness and motivation to change drug use behaviors is important because motivation is associated with increased treatment retention and lower relapse rates (Brocato & Wagner, 2008; Demmel, Beck, Richter, & Reker, 2004).
1.4. Rationale for the study
Negative attitudes and inaccurate beliefs about OMT have been documented among HIV-infected PWID in a Malaysian prison in 2007 (Bachireddy, et al., 2011). No study in Malaysia has documented attitudes towards OMT among a more representative sample of community-recruited PWID, including those without HIV infection, and no study has evaluated treatment experiences of active PWID who are not necessarily treatment seeking. Here we use data from a sample of 460 community-recruited active PWID from Greater Kuala Lumpur to provide the first estimates in this population of access to, attitudes toward, and experience with OMT as well as evaluate treatment readiness and its correlates in this population.
2. METHODS
2.1. Study procedures
In 2010, 460 PWID were recruited to participate in a structured survey with HIV testing at three locations in Greater Kuala Lumpur. Eligibility criteria were: age ≥18 years; self-reported drug injection in the prior 30 days, confirmed by physical examination of injection sites and demonstration of knowledge of drug preparation methods; residing in Greater Kuala Lumpur; willingness to undergo rapid HIV testing and urine toxicology screening; and ability to communicate in Bahasa Malaysia or English. Respondent-driven sampling (RDS) was used to recruit participants (Heckathorn, 1997). Interviews were conducted at three private MMT clinics. Two initial participants (“seeds”) were selected with the help of outreach workers from the area surrounding each of the interview sites. Each participant received three coupons to recruit eligible peers. Participants were remunerated with RM50 (~16 USD) for participation and RM25 (~8 USD) for each eligible peer they recruited. This study was approved by the institutional review boards at the University of Malaya Medical Centre and Yale University.
2.2. Measures
Sections relevant to this analysis from the 60-minute interviewer-administered survey include demographics, general medical history, drug use behaviors, opioid dependence, and experience with the criminal justice system. Standardized measures were used to assess methadone and buprenorphine use, treatment history, and medication administration practices. Additionally, attitudes towards both MMT and BMT, and motivations, attitudes and barriers towards entering OMT were examined.
Income and education were dichotomized at the urban monthly poverty line (RM800) and graduation from high school (Form 5/SPM), respectively. Both marital status and stable housing (not homeless or in a temporary living situation) were treated as binary variables. Participants reported both buprenorphine and buprenorphine/naloxone use, but unless otherwise noted, we use the term buprenorphine to refer to either formulation. Opioid dependence in the past 12 months was evaluated using the Mini-International Neuropsychiatric Interview (Sheehan, et al., 1998). The 21-item Depression, Anxiety and Stress Scale (DASS-21), validated in the Malaysian context (Musa, Fadzil, & Zain, 2007), was used to measure the severity of symptoms for depression, anxiety, and stress (Lovibond & Lovibond, 1995; Shire, 2011).
We differentiated engagement in OMT (daily use of buprenorphine or methadone prescribed by a medical provider to treat opioid dependence) from intermittent use of methadone or buprenorphine. For both MMT and BMT, we assessed treatment experiences and perceived barriers to access. We also examined individual beliefs about the effects of buprenorphine and methadone.
We used the 19-item Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) to assess participants’ readiness for treatment. The SOCRATES has been validated among PWID (Gossop, Stewart, & Marsden, 2007; William R. Miller & Tonigan, 1996; William R Miller, Yahne, & Tonigan, 2003), and it has been adapted for use in the Malaysian context (Fauziah, et al., 2010). The SOCRATES is composed of 3 subscales: Recognition, Ambivalence, and Taking Steps. Previously-established cutoffs were used for these subscales (CASAA, 1995; William R. Miller & Tonigan, 1996).
Questions evaluating attitudes towards OMT were adapted from a 28-item Likert-style survey assessing attitudes towards both methadone and buprenorphine (Robert P Schwartz, et al., 2008b). We selected 11 identical items each for both methadone and buprenorphine. A t-test was used to evaluate the difference between attitudes toward methadone and buprenorphine.
2.3. Statistical methods for evaluating correlates of treatment readiness
Linear regression was used to evaluate independent correlates of treatment readiness, operationalized with the SOCRATES score. Variables were selected for inclusion in a preliminary model if they were significantly associated with the outcome in bivariate testing (p<0.05) or if they were of known clinical significance (e.g. use of alcohol in the past 6 months, and previous utilization of non-evidence-based treatment) regardless of the strength of their association. Variables were included in the final model, shown in Table 2, only if they were significantly associated with the outcome in the preliminary model. Variables included in the preliminary but not the final model included income, alcohol use, experience with hospital-based medication-assisted detoxification, detoxification without medication at a religious center, or involvement in Narcotics Anonymous (NA), previous experience with buprenorphine therapy, and total years of injection drug use. The Akaike information criterion (AIC), which penalizes model complexity, confirmed that the more parsimonious model had a better fit.
Given recognized concerns about the precision and accuracy of existing RDS estimators (Gile & Handcock, 2010; Goel & Salganik, 2010), we chose not to present RDS-adjusted population estimates or regressions weighted by individual network size.
3. RESULTS
3.1. Participant characteristics
Participant characteristics are summarized in Table 1. Our sample consists of 460 active PWID who were primarily male (96.3% male), ethnically Malay (90.4%), and in their late 30s (Mean: 38.8, SD: 9.2). All 460 participants used opioids and nearly all (99.1%) met criteria for opioid-dependence. Less than half of participants (47.1%) had completed high school, over a quarter (26.7%) were married, most (83.3%) had stable housing, and a sixth (15.9%) were HIV-infected.
Table 1.
Participant characteristics and drug use history
| Entire Sample (N=460) | |
|---|---|
|
| |
| Variable | N (%) |
|
| |
| Demographic | |
|
| |
| Male | 443 (96.3%) |
| Age, mean ± SD | 38.8 ± 9.2 |
| High school graduate | 217 (47.1%) |
| Single | 337 (73.3%) |
| Stable housing | 383 (83.3%) |
| At or above poverty | 356 (77.4%) |
| Malay | 416 (90.4%) |
| Indian | 31 (6.7%) |
| Chinese | 12 (2.6%) |
|
| |
| Age of first drug injection | |
|
| |
| Mean ± SD | 15.0 ± 9.2 |
|
| |
| Past drug usea | |
|
| |
| Opioid-dependent | 456 (99.1%) |
| Heroin | 437 (95.0%) |
| Methadone | 200 (43.5%) |
| Methamphetamines | 198 (43.0%) |
| Benzodiazepines | 197 (42.8%) |
| Buprenorphine | 129 (28.0%) |
| Poly-substance use | 338 (73.5%) |
|
| |
| Medical History+ | |
|
| |
| Withdrawal | 436 (94.8%) |
| Hospitalization | 52 (11.3%) |
| HIV positive | 73 (15.9%) |
|
| |
| Non-OMT Treatment Historya | |
|
| |
| Compulsory drug detention center | 283 (61.5%) |
| Religious detoxification | 201 (43.6%) |
| Narcotics Anonymous | 36 (7.8%) |
| Hospital detoxification | 35 (7.6%) |
| Therapeutic community (Pengasih) | 24 (5.2%) |
|
| |
| Previous OMT Historyb | |
|
| |
| Buprenorphine | 58 (12.6%) |
| Methadone | 43 (9.3%) |
Assessed in the prior 6 months.
Assessed for lifetime
3.2. Drug use
Nearly all participants (98.7%) had ever used heroin, and over half (61.1% for each) had ever used methamphetamine or benzodiazepines. Within the past 6 months, 95% had used heroin. Methamphetamine (42.8%), and benzodiazepine (40%) use was high in the past 6 months as well; 73.5% of the sample reported using more than one substance in the same day in the previous 30 days.
3.3. Alternative approaches to substance dependence
Aside from OMT, 40% of participants had experience with some alternative approach to opioid dependence. Most (61.5%) had been at least once to a compulsory drug detention center, historically the government’s primary response to substance dependence. Almost half (43.8%) had participated in a detoxification without medication assistance with a religious healer, 7.8% had participated in Narcotics Anonymous, 7.6% had experienced hospital detoxification, and 5.2% had undergone treatment in Pengasih (a therapeutic community and abstinence-oriented residential program). In the past six months, only 5.5% of participations had participated in any of these approaches.
3.4. Intermittent and regular use of methadone and buprenorphine
Overall, only 18.7% of our sample had had any previous experience with OMT. While 55.2% had taken methadone intermittently at some point and 43.5% had used methadone in the past 6 months, only 9.3% had ever received MMT as a treatment for drug dependence from a licensed clinic. Of those who had received MMT (n=43), about half (53.5%) were currently receiving MMT. Of those who had never participated in MMT (n=417), the most frequently cited reason was a lack of interest (35.7%), followed by prohibitive costs (6.3%) and mistreatment by staff (12.1%).
Similar to methadone, the slight majority (51.7%) had ever taken buprenorphine. Twenty eight percent had taken buprenorphine in the past 6 months, and 15% had injected it in the previous 30 days; however, only 12.6% had ever enrolled in BMT. Of those who had enrolled (n=58), 36% had received BMT in the last 6 months and 30% were currently receiving BMT. For the 39.1% who had never been enrolled in BMT, lack of interest was the most commonly-cited reason (35.6%).
Of the 36% who had received BMT in the past 6 months, most (81%) had injected the buprenorphine prescribed to them from the clinic and only one person had consistently taken buprenorphine sublingually. Out of those who had ever used buprenorphine in the past 30 days (n=53), the majority (74.6%) received it directly from a doctor, 50.7% reported splitting buprenorphine tablets with others, and 63.4% reported pooling their money with others to purchase buprenorphine.
3.5. Characterization of attitudes towards opioid maintenance therapy
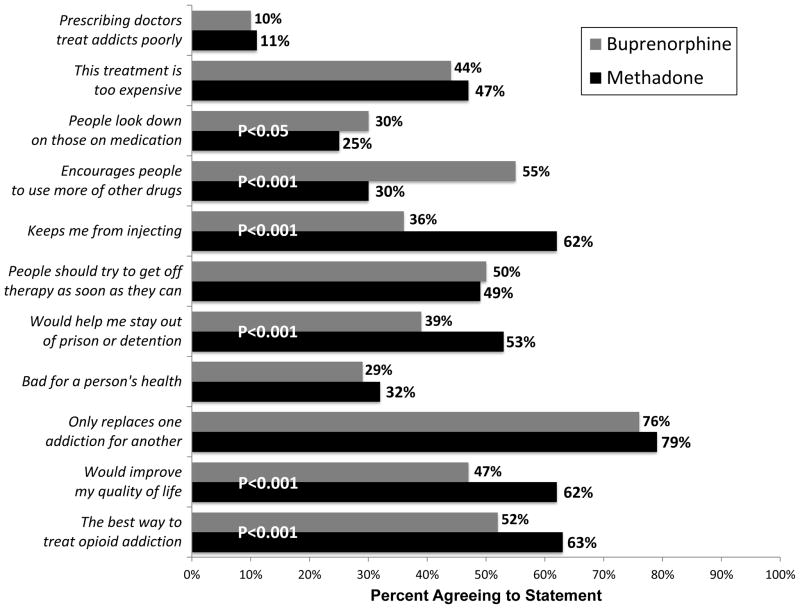
Most participants had favorable attitudes toward OMT with methadone or buprenorphine, although attitudes toward methadone were significantly more favorable. When asked about the best way to treat opioid addiction, 63.3% of participants agreed that methadone was the best option, while only 51.5% agreed that buprenorphine was best when asked the same question. As shown in Figure 1, attitudes towards methadone were more favorable for a number of other questions. Additionally, most participants disagreed with the statement that methadone (67.8%) or buprenorphine (66.7%) providers treated clients poorly. Over half (54.6%) of participants, however, believed that buprenorphine encouraged people to use more of other drugs, and over three-quarters of participants felt that OMT with methadone (78.7%) or buprenorphine (75.5%) was problematic because they were “replacing one addiction for another.” A full description of these attitudes is shown in Figure 1.
Figure 1.
“Attitudes Towards Methadone vs. Buprenorphine”
A comparison of attitudes towards buprenorphine and methadone. Overall, participants demonstrated more positive attitudes towards methadone.
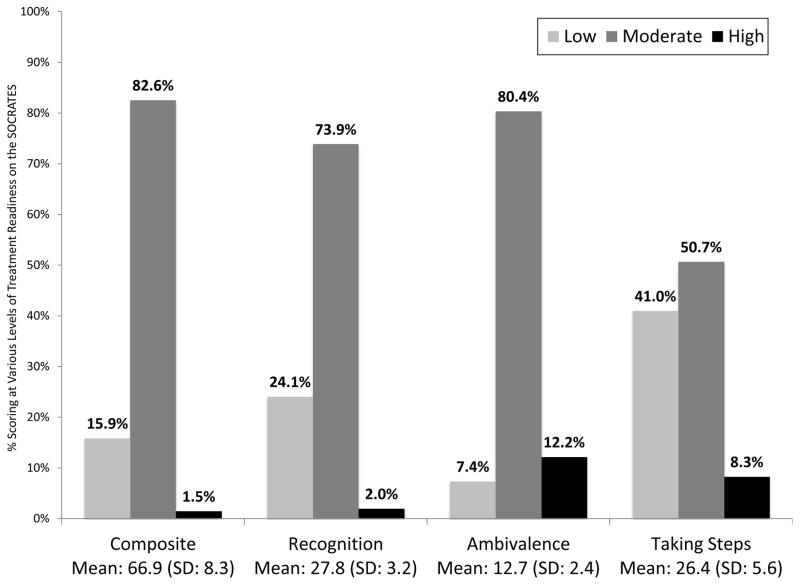
3.6. Evaluating treatment readiness using the SOCRATES
Overall, the majority of the subjects (82.6%) demonstrated moderate treatment readiness. For the Recognition subscale, 2.0% had a high score and 24.1% had a low score. For the Ambivalence subscale, 12.2% had a high score and 7.4% had a low score. For the Taking Steps subscale, 8.3% had a high score and 41.0% had a low score. Complete data for SOCRATES total and subscale scores are shown in Figure 2.
Figure 2.
“Treatment Readiness Using the SOCRATES Scale”
SOCRATES composite scores overall and for the 3 subscales of the survey tool. Most participants were found to be in the moderate category, with an exception being the “Taking Steps” subscale.]
In multiple linear regression, variables significantly and positively associated with treatment readiness included use of methadone in the past 6 months (β=2.4; 95% Confidence Interval [CI]: 0.8, 4.0), whether the subject had shared a syringe or needle in the past month (β=1.7; CI: 0.1, 3.4), age (β=0.2; CI: 0.1, 0.4), and stress symptom severity score on the DASS-21 (β=0.3; CI: 0.1, 0.5). Indian ethnicity (β=−6.2; CI: −9.0, −3.3), previous detention within a CDDC (β=−2.3; CI: −4.0, −0.6), and participation in a NSEP (β=−2.7; CI: −4.2, −1.1) were negatively correlated with treatment readiness. Estimated coefficients and confidence intervals for all explanatory variables in the final model are shown in Table 2.
Table 2.
Correlates of Treatment Readiness from Multivariable Linear Regression
| Coefficient Estimates | ||
|---|---|---|
|
| ||
| Explanatory Variablea | B̂ | 95% CI |
|
| ||
| Characteristics | ||
|
| ||
| Age | 0.2 | 0.1 – 0.4 |
| High school graduate | 0.9 | −0.5 – 2.3 |
| Married | 1.6 | −0.3 – 3.6 |
| Stable housing | 0.5 | −1.5 – 2.4 |
| At or above poverty | −1.1 | 2.8 – 0.6 |
| HIV infection | −0.8 | −2.8 – 1.2 |
| Indian ethnicityb | −6.2 | −9.0 – −3.3 |
| Chinese ethnicityb | −2.5 | −7.0 – 1.9 |
| Ever hospitalized | −1.3 | −3.9 – 0.9 |
| Ever incarcerated | 0.3 | −1.8 – 2.4 |
| Unprotected sexc | −0.7 | −2.6 – 1.1 |
|
| ||
| Past drug used | ||
|
| ||
| Years of injection drug use | −0.1 | −0.2 – 0.1 |
| Heroin | −2.3 | −5.4 – 1.6 |
| Methadone | 2.4 | 0.8 – 4.0 |
| Suboxone | 0.2 | −2.2 – 2.3 |
| Subutex | 2.1 | −0.9 – 5.1 |
| Benzodiazepines | 0.2 | −1.5 – 1.8 |
| Methamphetamine | 0.2 | −1.4 – 1.6 |
|
| ||
| Non-OMT Treatment Historyd | ||
|
| ||
| Compulsory drug detention center | −2.3 | −4.0 – −0.6 |
| Religious detoxification | 1.3 | −3.8 – 6.6 |
| Narcotics Anonymous | 2.7 | −1.3 – 6.7 |
| Hospital detoxification | 4.7 | −5.3 – 9.7 |
|
| ||
| OMT Treatment Historye | ||
|
| ||
| Methadone | 2.6 | −1.8 – 7.4 |
| Buprenorphine | −0.6 | −2.5 – 1.9 |
|
| ||
| Injection practices | ||
|
| ||
| Needle exchange used | −2.7 | −4.2 – −1.1 |
| Needle or syringe sharingc | 1.7 | 0.1 – 3.4 |
|
| ||
| DASS-21 | ||
|
| ||
| Depression | −0.1 | −0.2 – 0.1 |
| Anxiety | 0.1 | −0.1 – 0.3 |
| Stress | 0.3 | 0.1 – 0.5 |
Significant (p<0.05) explanatory variables are presented in bold
Ethnicity is as compared to Malay ethnicity
Assessed in the past 30 days
Assessed in the prior 6 months
Assessed as lifetime
4. DISCUSSION
This study is the first in Malaysia to document attitudes of active PWID toward both MMT and BMT and, to our knowledge, is the first in Asia to evaluate correlates of treatment readiness among PWID. We find that a high proportion of PWID had ever used methadone (55.2%) or buprenorphine (51.7%), primarily in non-treatment settings, while comparatively few had ever been prescribed methadone (9.3%) or buprenorphine (24.3%) within OMT settings. For those who had never been in treatment, approximately a third of the sample (35.7%) cited a lack of interest as a reason for not entering treatment (35.7%), followed by prohibitive costs (6.3%) and mistreatment by staff (12.1%). We also found that the majority of subjects demonstrated a low (15.9%) or moderate (82.6%) treatment readiness.
This study confirms recently-described barriers to accessing OMT in Malaysia and other key countries where PWID contribute greatly to the HIV epidemic (L. Degenhardt, et al., 2013a). Expanding access to OMT has been challenging in many low- and middle-income countries (Carrieri, et al., 2006; Wickersham, et al., 2013a). Our finding that 18.7% of subjects had previous experience with OMT is markedly lower than a 2008 WHO study of access to OMT in low- and middle-income countries where previous OMT enrollment was 37%, ranging from 4% in Ukraine to 60% in Thailand (Lawrinson, et al., 2008). Despite recent efforts to scale up OMT in Malaysia, treatment capacity remains low compared to the number of PWID (Mazlan, et al., 2006; Sylla, Bruce, Kamarulzaman, & Altice, 2007; Wickersham, et al., 2013a).
The only previous study to examine attitudes toward OMT in Malaysia was conducted in 2007 among 102 HIV-infected Malaysian prisoners and found that while 51% believed that OMT would be helpful, only 33% believed they needed OMT to prevent relapse after prison release (Bachireddy, et al., 2011). This is a dramatic difference from the 70–90% of incarcerated prisoners that actually do experience a relapse after release (McLellan, Lewis, O’Brien, & Kleber, 2000; Reid, et al., 2007), which indicates a need for education of PWID about treatment. In our study, only 36% believed that BMT could help prevent relapse, although this figure was higher at 62% for MMT.
We found that participants generally preferred methadone over buprenorphine. Strong preferences for different forms of OMT previously have been documented outside of Malaysia (Kelly, et al., 2012; R. P. Schwartz, et al., 2008a). Whereas methadone was introduced in a controlled fashion, first in specialized addiction centers in 2007, buprenorphine was introduced in less controlled settings in primary care clinics in 2006 (Gill & Habil, 2007; Wickersham, et al., 2013a). Buprenorphine was initially available without naloxone, and its injection has been commonplace since its introduction (R Douglas Bruce, et al., 2008a; R. D. Bruce, et al., 2008b; R. D. Bruce, et al., 2009; Vicknasingam, et al., 2010). Because injection of buprenorphine has been commonplace and examples of its proper use are less common than methadone, participants may not perceive buprenorphine to be as efficacious.
Our data also showed evidence of buprenorphine misuse. In our sample, 15% had injected buprenorphine in the past month, and of the few that were currently on BMT, almost all were injecting rather than taking it sublingually. Previous research suggests that people inject buprenorphine because they cannot afford to take it sublingually (R. D. Bruce, et al., 2008b; R. D. Bruce, et al., 2009; Vicknasingam, et al., 2010). While MMT is available in both private and government facilities, buprenorphine is only available in the private sector. Buprenorphine also has higher bioavailability when injected, so patients are able to maintain themselves on a lower, more affordable, dosage if buprenorphine is injected. Although few participants cited cost as a barrier to accessing BMT, this might be because most are purchasing low, subtherapeutic doses. The widespread misuse of buprenorphine, driven by economic motivations, may be responsible for more negative attitudes toward buprenorphine than methadone.
Systemic factors influencing how OMT is prescribed may affect willingness to engage in treatment and shape potential interventions to increase treatment engagement. As of 2013, referral into OMT was set as a performance indicator for NSEPs; however, NSEPs in Malaysia have reported low referrals into OMT programs (Ngadiman, 2014). In the private sector, OMT providers both prescribe and dispense OMT, creating a conflict of interest that may adversely influence the way OMT is prescribed. Methadone and buprenorphine are typically priced by the milligram rather than a fixed price for daily treatment (irrespective of dose). Thus, there is an incentive for prescribers to sell OMT medications to patients at whatever dosage and frequency patients can afford to purchase them, which can result in suboptimal dosing and sporadic, “informal” use of these medications. Patients’ experience with low-dose, intermittent treatment may adversely affect their perceptions of the efficacy of these medications to treat opioid dependence. To optimize treatment outcomes, systemic changes are needed in the way OMT medications are dispensed to align prescriber financial incentives with patient health outcomes, including substance abuse treatment and HIV prevention outcomes.
The finding that NSEP participation was associated with lower readiness for treatment may represent baseline differences between clients who do and do not utilize NSEPs. NSEP outreach workers target PWID with riskier behaviors and a higher demand for injection equipment, and it has been documented elsewhere that these higher-risk individuals are more likely to enroll in and be retained in NSEP (Fisher, Reynolds, & Harbke, 2002; Hagan, et al., 2000; Hahn, Vranizan, & Moss, 1997). These individuals may also be less ready for drug treatment, which is reflected in our data here.
The majority of our sample (82.6%) was moderately ready for treatment. Brief motivational interventions have been successfully deployed in clinical and community outreach (e.g., NSEP) settings to increase patients’ readiness for treatment (Booth, Kwiatkowski, Iguchi, Pinto, & John, 1998; Kidorf, et al., 2005; Strathdee, et al., 2006). Brief cognitive interventions, while originally tested on individuals with alcohol use disorders (Maisto, et al., 2001; Rollnick, Heather, Gold, & Hall, 1992; Wilk, Jensen, & Havighurst, 1997), have been efficacious in increasing treatment entry for cocaine, heroin and amphetamine users (Baker, Boggs, & Lewin, 2001; Bernstein, et al., 2005; Saunders, Wilkinson, & Phillips, 1995). These sessions consist of a single, structured encounter targeting cessation of drug use conducted by a healthcare professional in a primary care setting. In our study, many subjects interface with OMT providers to purchase methadone or buprenorphine for intermittent use. Therefore, it may be possible to provide interventions through OMT clinics or community outreach settings that already have contact with patients in order to promote engagement in OMT.
Related to this brief interventional practice is the finding of Brocado et al. that motivation to change, particularly recognition of a drug problem, is positively related to the strength of the therapeutic alliance between health care provider and patient (Brocato & Wagner, 2008). Our study showed that a majority of our participants demonstrated a positive attitude towards providers. In addition to systemic changes in OMT medication dispensation, educating providers about evidence-based practices for OMT will be instrumental in encouraging users to enter treatment. The therapeutic alliance is thus important for the effectiveness of brief interventions and represents another potential target area for improving OMT.
This study was conducted in 2010. By 2011, MMT had been expanded in the prison system (Singh, Chawarski, Schottenfeld, & Vicknasingam, 2013; Wickersham, et al., 2013a; Wickersham, Zahari, Azar, Kamarulzaman, & Altice, 2013b). By 2013, OMT had expanded to approximately 380 general medical practice offices that treated approximately 10,000 patients. In addition, 27,756 patients were actively enrolled in 333 general medical practice offices and government-run MMT centers (Singh, et al., 2013). Expansion of methadone in the time since this study was conducted may have led to a higher proportion of PWID now having accessed structured MMT.
Beginning July 2011, in addition to the community-based (MMT) program provided by the Ministry of Health and private practitioners, the National Anti-Drug Agency (NADA-AADK) underwent a transformation that saw a shift away from compulsory detention by converting the CDDCs into Cure & Care Centers which provide voluntary comprehensive client centered treatment and support services including MMT (Ghani et. al., 2015; L. Degenhardt, et al., 2013a). There are currently 59 Cure and Care centers operated under National Anti-Drug Agency (NADA-AADK) which are client-friendly (Ghani, et al., 2014; Ngadiman, 2014). Furthermore, AADK has plans to convert 18 of the 28 CDDCs into voluntary treatment centers by 2015 (Kaur, 2013). To date, NADA-AADK reports that more than 36,000 PWID have accessed these services, with a total of 6500 people currently receiving MMT (Kaur, 2013). Nonetheless, there are an estimated 170,000 PWID, mostly who use opioids (Ngadiman, 2014), indicating that coverage is low and many individuals are not enrolled in treatment.
Our findings are most applicable to the Malaysian setting. Although the SOCRATES scale has been validated in PWID in Malaysia, the cutoffs determining whether someone has “high”, “moderate” or “low” levels of treatment readiness may not be valid in this setting, making it possible that a higher number of subjects were treatment-ready than we find. Even if these cutoffs were slightly different, however, readiness for treatment would still be extraordinarily low in this sample of PWID. Also, the SOCRATES measures general treatment readiness, which we interpret solely in the context of OMT, the primary evidence-based treatment for opioid dependence. Finally, it is important to acknowledge that there are a number of external barriers, apart from attitudes, that prevent PWID from obtaining and being retained in OMT. One such complication is the fact that 42.8% and 40% use methamphetamine and benzodiazepines, respectively, suggesting that OMT alone may not be sufficient and would likely be most effective in combination with behavioral interventions. Stimulant and benzodiazepine abuse and dependence negatively influence OMT outcomes, but the treatments for these substances are more complex (Brands, et al., 2008; Kamal, et al., 2007). Drug use stigma and social factors affecting readiness for treatment are also worthy of future study, as are structural barriers such as the cost and accessibility of treatment. Notwithstanding these limitations, we have been able to document experiences with and attitudes toward OMT as well as correlates of treatment readiness in a community-based sample of PWID in Malaysia.
5. CONCLUSIONS
OMT is the most effective treatment for opioid dependence and is an important tool for primary and secondary HIV prevention. HIV prevention efforts among PWID have been limited by inadequate scale-up of OMT. By understanding the factors that contribute to patients’ unwillingness to enter or return to treatment, we can target areas of improvement and potentially improve the health of PWID in Malaysia. Interventions should target PWID who display moderate levels of treatment readiness to transition them to a higher state of treatment readiness. The preference for MMT over BMT, coupled with the evidence of buprenorphine misuse, indicates the need for education of both PWID and providers with respect to evidence-based OMT practices. Finally, addressing attitudinal factors and barriers to entering treatment will be essential in enrolling and retaining PWID in treatment.
Acknowledgments
This work was supported by the National Institutes for Drug Abuse for career development (K24 DA017072; FLA), research (NIDA R01 DA032106; FLA, AK), and training (T32GM07205, T32MH020031; ARB) grants as well as University Malaya’s High Impact Research Grant (E-000001-20001; A.K) and the Yale Downs Fellowship (ARB). OraSure Technologies, Inc. provided discounted rapid HIV tests. Funders had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
References
- Altice FL, Bruce RD, Lucas GM, Lum PJ, Korthuis PT, Flanigan TP, Cunningham CO, Sullivan LE, Vergara-Rodriguez P, Fiellin DA, Cajina A, Botsko M, Nandi V, Gourevitch MN, Finkelstein R Collaborative, B. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: results from a multisite study. J Acquir Immune Defic Syndr. 2011;56:S22–32. doi: 10.1097/QAI.0b013e318209751e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376:59–79. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abuse Treat. 2005;28:321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Bachireddy C, Bazazi AR, Kavasery R, Govindasamy S, Kamarulzaman A, Altice FL. Attitudes toward opioid substitution therapy and pre-incarceration HIV transmission behaviors among HIV-infected prisoners in Malaysia: implications for secondary prevention. Drug Alcohol Depend. 2011;116:151–157. doi: 10.1016/j.drugalcdep.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker A, Boggs TG, Lewin TJ. Randomized controlled trial of brief cognitive-behavioural interventions among regular users of amphetamine. Addiction. 2001;96:1279–1287. doi: 10.1046/j.1360-0443.2001.96912797.x. [DOI] [PubMed] [Google Scholar]
- Bazazi AR, Zelenev A, Fu JJ, Yee I, Kamarulzaman A, Altice FL. High prevalence of non-fatal overdose among people who inject drugs in Malaysia: Correlates of overdose and implications for overdose prevention from a cross-sectional study. International Journal of Drug Policy. 2014 doi: 10.1016/j.drugpo.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein J, Bernstein E, Tassiopoulos K, Heeren T, Levenson S, Hingson R. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug Alcohol Depend. 2005;77:49–59. doi: 10.1016/j.drugalcdep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Binford MC, Kahana SY, Altice FL. A systematic review of antiretroviral adherence interventions for HIV-infected people who use drugs. Curr HIV/AIDS Rep. 2012;9:287–312. doi: 10.1007/s11904-012-0134-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth RE, Kwiatkowski C, Iguchi MY, Pinto F, John D. Facilitating treatment entry among out-of-treatment injection drug users. Public Health Reports. 1998;113:116. [PMC free article] [PubMed] [Google Scholar]
- Brands B, Blake J, Marsh DC, Sproule B, Jeyapalan R, Li S. The impact of benzodiazepine use on methadone maintenance treatment outcomes. Journal of addictive diseases. 2008;27:37–48. doi: 10.1080/10550880802122620. [DOI] [PubMed] [Google Scholar]
- Brocato J, Wagner EF. Predictors of retention in an alternative-to-prison substance abuse treatment program. Criminal Justice and Behavior. 2008;35:99–119. [Google Scholar]
- Bruce RD, Govindasamy S, Sylla L, Haddad MS, Kamarulzaman A, Altice FL. Case series of buprenorphine injectors in Kuala Lumpur, Malaysia. Am J Drug Alcohol Abuse. 2008a;34:511–517. doi: 10.1080/00952990802122259. [DOI] [PubMed] [Google Scholar]
- Bruce RD, Govindasamy S, Sylla L, Haddad MS, Kamarulzaman A, Altice FL. Case series of buprenorphine injectors in Kuala Lumpur, Malaysia. Am J Drug Alcohol Abuse. 2008b;34:511–517. doi: 10.1080/00952990802122259. [DOI] [PubMed] [Google Scholar]
- Bruce RD, Govindasamy S, Sylla L, Kamarulzaman A, Altice FL. Lack of reduction in buprenorphine injection after introduction of co-formulated buprenorphine/naloxone to the Malaysian market. Am J Drug Alcohol Abuse. 2009;35:68–72. doi: 10.1080/00952990802585406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce RD, Moody DE, Altice FL, Gourevitch MN, Friedland GH. A review of pharmacological interactions between HIV or hepatitis C virus medications and opioid agonist therapy: implications and management for clinical practice. Expert Rev Clin Pharmacol. 2013;6:249–269. doi: 10.1586/ecp.13.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrieri MP, Amass L, Lucas GM, Vlahov D, Wodak A, Woody GE. Buprenorphine use: The international experience. Clinical Infectious Diseases. 2006;43:S197–215. doi: 10.1086/508184. [DOI] [PubMed] [Google Scholar]
- CASAA. Socrates Version 8. 2014 from http://casaa.unm.edu/inst/SOCRATESv8.pdf.
- Chou R, Cruciani RA, Fiellin DA, Compton P, Farrar JT, Haigney MC, Inturrisi C, Knight JR, Otis-Green S, Marcus SM, Mehta D, Meyer MC, Portenoy R, Savage S, Strain E, Walsh S, Zeltzer L. Methadone safety: a clinical practice guideline from the American Pain Society and College on Problems of Drug Dependence, in collaboration with the Heart Rhythm Society. J Pain. 2014;15:321–337. doi: 10.1016/j.jpain.2014.01.494. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Larance B, Mathers B, Azim T, Kamarulzaman A, Mattick R, Panda S, Toufik A, Tyndall M, Wiessing L. A global review of availability, extra-medical use, injection and the association with HIV. Prepared on behalf of the Reference Group to the United Nations on HIV and Injecting Drug Use. Sydney: University of New South Wales; 2008. Benefits and risks of pharmaceutical opioids: Essential treatment and diverted medication. [Google Scholar]
- Degenhardt L, Mathers BM, Wirtz AL, Wolfe D, Kamarulzaman A, Carrieri MP, Strathdee SA, Malinowska-Sempruch K, Kazatchkine M, Beyrer C. What has been achieved in HIV prevention, treatment and care for people who inject drugs, 2010–2012? A review of the six highest burden countries. Int J Drug Policy. 2013a doi: 10.1016/j.drugpo.2013.08.004. Epub Ahead of Print 04 Sep 2013. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Hall WD, Freedman G, Burstein R, Johns N, Engell RE, Flaxman A, Murray CJ, Vos T. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet. 2013b doi: 10.1016/S0140-6736(13)61530-5. [DOI] [PubMed] [Google Scholar]
- Demmel R, Beck B, Richter D, Reker T. Readiness to change in a clinical sample of problem drinkers: Relation to alcohol use, self-efficacy, and treatment outcome. European addiction research. 2004;10:133–138. doi: 10.1159/000077702. [DOI] [PubMed] [Google Scholar]
- Fauziah I, Arifin Z, Wan Shahrazad W, Lukman Z, Roseliza Murni A, Zainah A, Siti Fatihah G. Measuring motivational readiness for change among drug addicts in Malaysia: A descriptive analysis. The Social Sciences. 2010;5:429–432. [Google Scholar]
- Fisher DG, Reynolds GL, Harbke CR. Selection effect of needle exchange in Anchorage, Alaska. J Urban Health. 2002;79:128–135. doi: 10.1093/jurban/79.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu JJ, Bazazi AR, Altice FL, Mohamed MN, Kamarulzaman A. Absence of antiretroviral therapy and other risk factors for morbidity and mortality in Malaysian compulsory drug detention and rehabilitation centers. PLoS ONE. 2012;7:e44249. doi: 10.1371/journal.pone.0044249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghani MA, Brown S-E, Khan F, Wickersham JA, Lim SH, Dhaliwal SK, Kamarulzaman A, Altice FL. An Exploratory Qualitative Assessment of Self-Reported Treatment Outcomes and Satisfaction Among Patients Accessing an Innovative Voluntary Drug Treatment Centre in Malaysia. International Journal of Drug Policy. 2014 doi: 10.1016/j.drugpo.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gile KJ, Handcock MS. Respondent-Driven Sampling: An Assessment of Current Methodology. Sociol Methodol. 2010;40:285–327. doi: 10.1111/j.1467-9531.2010.01223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill JS, Habil M. The first methadone programme in Malaysia: overcoming obstacles and achieving the impossible. Asean J Psychiatry. 2007;8:64–70. [Google Scholar]
- Goel S, Salganik MJ. Assessing respondent-driven sampling. Proc Natl Acad Sci U S A. 2010;107:6743–6747. doi: 10.1073/pnas.1000261107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Marsden J. Readiness for change and drug use outcomes after treatment. Addiction. 2007;102:301–308. doi: 10.1111/j.1360-0443.2006.01681.x. [DOI] [PubMed] [Google Scholar]
- Hagan H, McGough JP, Thiede H, Hopkins SG, Weiss NS, Alexander ER. Volunteer bias in nonrandomized evaluations of the efficacy of needle-exchange programs. J Urban Health. 2000;77:103–112. doi: 10.1007/BF02350966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn JA, Vranizan KM, Moss AR. Who uses needle exchange? A study of injection drug users in treatment in San Francisco, 1989–1990. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;15:157–164. doi: 10.1097/00042560-199706010-00010. [DOI] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Social problems. 1997:174–199. [Google Scholar]
- Jin H, Earnshaw VA, Wickersham JA, Kamarulzaman A, Desai MM, John J, Altice FL. An assessment of health-care students’ attitudes toward patients with or at high risk for HIV: implications for education and cultural competency. AIDS Care. 2014 doi: 10.1080/09540121.2014.894616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS) The Gap Report. Geneva, Switzerland: 2014. [Accessed on 24 August 2014]. at: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2014/unaids_gap_report_en.pdf) [Google Scholar]
- Kamal F, Flavin S, Campbell F, Behan C, Fagan J, Smyth R. Factors affecting the outcome of methadone maintenance treatment in opiate dependance. Irish medical journal. 2007;100:393–396. [PubMed] [Google Scholar]
- Kamarulzaman A, Altice FL. Challenges in managing HIV in people who use drugs. Current opinion in infectious diseases. 2015;28:10–16. doi: 10.1097/QCO.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur S. Evidence-Based Drug Policies for an Effective HIV Response: Malaysian Experience. 7th IAS Conference on HIV Pathogenesis, Treatment and Prevention; 2013. Abstract MOSS0104. [Google Scholar]
- Kelly SM, Brown BS, Katz EC, O’Grady KE, Mitchell SG, King S, Schwartz RP. A comparison of attitudes toward opioid agonist treatment among short-term buprenorphine patients. Am J Drug Alcohol Abuse. 2012;38:233–238. doi: 10.3109/00952990.2011.643983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidorf M, Disney E, King V, Kolodner K, Beilenson P, Brooner RK. Challenges in motivating treatment enrollment in community syringe exchange participants. Journal of Urban Health. 2005;82:456–467. doi: 10.1093/jurban/jti091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrinson P, Ali R, Buavirat A, Chiamwongpaet S, Dvoryak S, Habrat B, Jie S, Mardiati R, Mokri A, Moskalewicz J, Newcombe D, Poznyak V, Subata E, Uchtenhagen A, Utami DS, Vial R, Zhao C. Key findings from the WHO collaborative study on substitution therapy for opioid dependence and HIV/AIDS. Addiction. 2008;103:1484–1492. doi: 10.1111/j.1360-0443.2008.02249.x. [DOI] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour research and therapy. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Conigliaro J, McNeil M, Kraemer K, Conigliaro RL, Kelley ME. Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. Journal of Studies on Alcohol and Drugs. 2001;62:605. doi: 10.15288/jsa.2001.62.605. [DOI] [PubMed] [Google Scholar]
- Mathers BM, Degenhardt L, Ali H, Wiessing L, Hickman M, Mattick RP, Myers B, Ambekar A, Strathdee SA. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet. 2010;375:1014–1028. doi: 10.1016/S0140-6736(10)60232-2. [DOI] [PubMed] [Google Scholar]
- Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, Wodak A, Panda S, Tyndall M, Toufik A, Mattick RP Reference Group to the U. N. o. H. I. V., & Injecting Drug, U. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372:1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009:3. doi: 10.1002/14651858.CD002209. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Kimber J, Breen C, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2008:CD002207. doi: 10.1002/14651858.CD002207.pub3. [DOI] [PubMed] [Google Scholar]
- Mazlan M, Mazlan M, Schottenfeld RS, Mazlan M, Schottenfeld RS, Chawarski MC, Mazlan M, Schottenfeld RS, Chawarski MC. New challenges and opportunities in managing substance abuse in Malaysia. Drug and Alcohol Review. 2006;25:473–478. doi: 10.1080/09595230600883354. [DOI] [PubMed] [Google Scholar]
- McLellan A, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Mesquita F, Jacka D, Ricard D, Shaw G, Tieru H, Hu Y, Poundstone K, Salva M, Fujita M, Singh N. Accelerating harm reduction interventions to confront the HIV epidemic in the Western Pacific and Asia: the role of WHO (WPRO) Harm Reduct J. 2008;5:26. doi: 10.1186/1477-7517-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers’ motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10:81–89. [Google Scholar]
- Miller WR, Yahne CE, Tonigan JS. Motivational interviewing in drug abuse services: a randomized trial. Journal of consulting and clinical psychology. 2003;71:754. doi: 10.1037/0022-006x.71.4.754. [DOI] [PubMed] [Google Scholar]
- Mohamad N, Bakar N, Musa N, Talib N, Ismail R. Better retention of Malaysian opiate dependents treated with high dose methadone in methadone maintenance therapy. Harm Reduct J. 2010;7:30. doi: 10.1186/1477-7517-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musa R, Fadzil MA, Zain Z. Translation, validation and psychometric properties of Bahasa Malaysia version of the Depression Anxiety and Stress Scales (DASS) ASEAN Journal of Psychiatry. 2007;8:82–89. [Google Scholar]
- Ngadiman Sa, Anita S, Yuswan Fazidah. Malaysia 2014: Country Responses to HIV/AIDS. UNAIDS Global Progress Report 2014 [Google Scholar]
- Noordin NM, Merican MI, Rahman HA, Lee SS, Ramly R. Substitution treatment in Malaysia. Lancet. 2008;372:1149–1150. doi: 10.1016/S0140-6736(08)61479-8. [DOI] [PubMed] [Google Scholar]
- Razali SM. Drug substitution therapy: a new approach in preventing the spread of HIV/AIDS in Malaysia. Trop Doct. 2008;38:109–110. doi: 10.1258/td.2007.070001. [DOI] [PubMed] [Google Scholar]
- Reid G, Kamarulzaman A, Sran SK. Malaysia and harm reduction: The challenges and responses. International Journal of Drug Policy. 2007;18:136–140. doi: 10.1016/j.drugpo.2006.12.015. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’questionnaire for use in brief, opportunistic interventions among excessive drinkers. British journal of addiction. 1992;87:743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Saber-Tehrani AS, Bruce RD, Altice FL. Pharmacokinetic drug interactions and adverse consequences between psychotropic medications and pharmacotherapy for the treatment of opioid dependence. Am J Drug Alcohol Abuse. 2011;37:1–11. doi: 10.3109/00952990.2010.540279. [DOI] [PubMed] [Google Scholar]
- Saunders B, Wilkinson C, Phillips M. The impact of a brief motivational intervention with opiate users attending a methadone programme. Addiction. 1995;90:415–424. doi: 10.1046/j.1360-0443.1995.90341510.x. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Kelly SM, O’Grady KE, Mitchell SG, Peterson JA, Reisinger HS, Agar MH, Brown BS. Attitudes toward buprenorphine and methadone among opioid-dependent individuals. Am J Addict. 2008a;17:396–401. doi: 10.1080/10550490802268835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz RP, Kelly SM, O’Grady KE, Mitchell SG, Peterson JA, Reisinger HS, Agar MH, Brown BS. Attitudes toward buprenorphine and methadone among opioid-dependent individuals. The American Journal on Addictions. 2008b;17:396–401. doi: 10.1080/10550490802268835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifa Ezat WP, Noor Azimah H, Rushidi R, Raminder K, Ruhani I. Compliance towards methadone maintenance therapy and its associated factors in Selangor primary care centers and Kuala Lumpur hospital. Med J Malaysia. 2009;64:65–70. [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- Shire. A Guide to the Depression, Anxiety, and Stress Scale. from http://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0018/212904/DASS21_Summary_Final.pdf.
- Singh D, Chawarski MC, Schottenfeld R, Vicknasingam B. Substance abuse and the HIV situation in Malaysia. Journal of Food and Drug Analysis. 2013;21:S46–S51. doi: 10.1016/j.jfda.2013.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Ricketts EP, Huettner S, Cornelius L, Bishai D, Havens JR, Beilenson P, Rapp C, Lloyd JJ, Latkin CA. Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: Results from a community-based behavioral intervention trial. Drug Alcohol Depend. 2006;83:225–232. doi: 10.1016/j.drugalcdep.2005.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylla L, Bruce RD, Kamarulzaman A, Altice FL. Integration and co-location of HIV/AIDS, tuberculosis and drug treatment services. International Journal of Drug Policy. 2007;18:306–312. doi: 10.1016/j.drugpo.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson MA, Mugavero MJ, Amico KR, Cargill VA, Chang LW, Gross R, Orrell C, Altice FL, Bangsberg DR, Bartlett JG, Beckwith CG, Dowshen N, Gordon CM, Horn T, Kumar P, Scott JD, Stirratt MJ, Remien RH, Simoni JM, Nachega JB. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156:817–833. doi: 10.7326/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicknasingam B, Mazlan M, Schottenfeld RS, Chawarski MC. Injection of buprenorphine and buprenorphine/naloxone tablets in Malaysia. Drug Alcohol Depend. 2010;111:44–49. doi: 10.1016/j.drugalcdep.2010.03.014. [DOI] [PubMed] [Google Scholar]
- Weimer MB, Chou R. Research gaps on methadone harms and comparative harms: findings from a review of the evidence for an American Pain Society and College on Problems of Drug Dependence clinical practice guideline. J Pain. 2014;15:366–376. doi: 10.1016/j.jpain.2014.01.496. [DOI] [PubMed] [Google Scholar]
- Wickersham JA, Marcus R, Kamarulzaman A, Zahari MM, Altice FL. Implementing methadone maintenance treatment in prisons in Malaysia. Bull World Health Organ. 2013a;91:124–129. doi: 10.2471/BLT.12.109132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickersham JA, Zahari MM, Azar MM, Kamarulzaman A, Altice FL. Methadone dose at the time of release from prison significantly influences retention in treatment: Implications from a pilot study of HIV-infected prisoners transitioning to the community in Malaysia. Drug Alcohol Depend. 2013b;132:378–382. doi: 10.1016/j.drugalcdep.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. Journal of general internal medicine. 1997;12:274–283. doi: 10.1046/j.1525-1497.1997.012005274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet. 2010;376:355–366. doi: 10.1016/S0140-6736(10)60832-X. [DOI] [PubMed] [Google Scholar]
- Zule WA, Desmond DP. Attitudes toward methadone maintenance: implications for HIV prevention. Journal of Psychoactive Drugs. 1998;30:89–97. doi: 10.1080/02791072.1998.10399674. [DOI] [PubMed] [Google Scholar]