Abstract
Objectives. We examined the mutual effects of smoking bans and taxes on smoking among a longitudinal cohort of young adults.
Methods. We combined a repository of US tobacco policies at the state and local level with the nationally representative geocoded National Longitudinal Survey of Youth 1997 (2004–2011) from ages 19 to 31 years and Census data, to examine the impact of tobacco policies on any current and daily pack smoking. The analytic sample amounts to 19 668 observations among 4341 individuals within 487 cities.
Results. For current smoking, we found significant effects for comprehensive smoking bans, but not excise taxes. We also found an interaction effect, with bans being most effective in locales with no or low taxes. For daily pack smoking, we found significant effects for taxes, but limited support for bans.
Conclusions. Social smoking among young adults is primarily inhibited by smoking bans, but excise taxes only deter such smoking in the absence of a ban. Heavy smokers are primarily deterred by taxes. Although both policies have an impact on young adult smoking behaviors, their dual presence does not intensify each policy’s efficacy.
The denormalization of tobacco use in Western nations has led to declines in both smoking and its public acceptability.1 Even with overall reductions in smoking, tobacco use remains the leading cause of preventable illness and death in the United States,2 making assessment of the efficacy of particular policies on actual smoking behavior an imperative. Tobacco-control policies have been described as intensifying the process of denormalization of smoking among young people.3 The focus on young people is much deserved, as those who begin smoking at younger ages are at higher risk for smoking, particularly heavy smoking, as adults.4,5 The identification of policies that affect smoking behavior among young people can have long-term implications for public health as those individuals age into later life.
Estimates suggest that tobacco-control policies have likely had an impact on tobacco consumption in the aggregate.6 A wide array of research has suggested that excise taxes and clean air policies are efficacious tobacco-control policy tools, but these studies have come with several limitations that prohibit linking policy with actual individual-level behavior. For clean air policies, studies have inferred the effects of such prohibitions through cohort effects,7 have relied on cross-sectional data,8–10 have not considered city-level policy,9–13 or have used data within a single locality.14,15 Studies have also found robust effects of excise taxes on tobacco use.10,12,13,16–29 We note, however, that most studies of excise taxes used either aggregate time-series or repeated cross-sectional data, and often at the state or national level. Thus, for both bans and taxes, the literature has yet to link policy contexts at the local level to a longitudinal data set of the same individuals over time as well as account for potential interactive effects of these policies. Even studies using the same data sets used herein have not considered the interaction between smoking bans and excise taxes.12
The local level is critically important, yet often is overlooked in studies of both clean air policies and excise taxes. Cities led the way in enacting smoking bans in the United States, such that the diffusion of clean air regulations began at the local level and spread vertically up to the state in an unusual example of “bottom-up federalism.”30 Chahine et al. suggested that
contextual covariates play a larger role more locally, for example at the level of towns or neighborhoods. This may especially be the case for indoor smoking restrictions, which are highly variable within states.9(p757)
They later suggested that future research should consider contextual variables at the local level to “fully characterize social determinants of smoking variability across populations and places.”9(p758) Furthermore, although prohibited in some states, cities in several states may levy taxes on tobacco products in addition to those imposed by the state, creating similar variability on the issue of taxation. Thus, without accounting for the city level, the policies to which an individual is subjected may be mischaracterized.
In our study, we overcame the limitations of past studies by, first, combining a repository of all tobacco ordinances in the United States with a nationally representative annual survey of a single cohort of youths, allowing us to directly link a multilevel policy context to individual-level behavior over time in a manner not possible through aggregate or repeated cross-sectional data. Second, we considered the critical but underexplored policy context of the city level. Third, no studies have considered the independent and interactive effects of taxes and bans simultaneously. This is important as interaction analyses may lead to the identification of potential synergistic effects of tobacco policies. Thus, we used multilevel statistical modeling to identify the impact of these 2 important tobacco-control policies on smoking behaviors over time in a nationally representative sample of US youths.
METHODS
The individual-level data came from the National Longitudinal Survey of Youth 1997 (NLSY97). The NLSY97 has a large, nationally representative, geocoded sample (n = 8984) designed to track the transition of youths into adulthood, with an oversample of Black and Latino youths. Adolescents aged from 12 to 16 years were randomly sampled in 1997 and have been surveyed annually. The retention rate was nearly 83% in 2011. The restricted-access, geocoded NLSY97 identifies the respondents’ core-based statistical area (CBSA; i.e., metropolitan or micropolitan area), county, and state. We analyzed a subset of respondents whose city of residence could be identified by combining CBSA and county information with a variable assessing whether the respondent lived in a principal city within the metro area. Thus, our analyses focused on those living in the largest principal city of a CBSA, given the importance of the local level within a broader multilevel policy context. We also restricted analyses to waves 2004 and later (ages 19–31 years), as this was the first year in which CBSA data were available. This subset amounts to 19 668 observations among 4341 individuals within 487 cities. We note that respondents only contributed in years in which they lived in these cities; that is, respondents moved in and out of the defined subset. Among the subset of individuals that contributed at least once, 33.6% lived in such a city within a CBSA in all years with valid data, and 59.6% lived in such a city in at least half of all years with valid data.
Each year, respondents who indicated that they had ever smoked an entire cigarette were asked the number of days they had smoked during the 30 days before the interview, and the number of cigarettes they had smoked each day on those 30 days. We created 2 outcome variables based upon these self-reports: one indicating any cigarette use during the past 30 days (pooled mean = 34.5%) and a second variable for heavy use for those who reported smoking at least a pack per day (pooled mean = 4.9%).
In all models, we included a considerable battery of control variables at both the individual level and the city level. Because age is central to patterns of substance use among young adults, we chose age as our time metric,31 including a quadratic term as this fit the data better than any other polynomial for age. We also included age in 1997 in the models to control for cohort effects.
We included several other individual-level risk factors for tobacco use in the models. Regarding family, we included time-varying indicator variables for whether the respondent lived with a parent, was married, and had children.32–34 We also accounted for recent moves via a dummy variable for a past-year move across at least 1 county. For work-related risk factors, we included time-varying categorical variables for job status and job schedule.35 To assess peer-related influences, we included the percentage of peers who smoked in 1997, the only year it was measured.36 For academic performance, we included a dummy variable for receiving “mostly A’s” in high school.37 To control for the respondent’s mental health,38 the data set included a 5-item scale for depression asking whether the respondent in the past month had been a very nervous person, felt calm and peaceful, felt downhearted and blue, had been a happy person, and had felt so down in the dumps that nothing could cheer him or her up, of which we used the 2004 baseline measure (α = 0.77). To account for intergenerational health influences,39–44 we included parents’ self-reported health from 1997.
We included several measures for socioeconomic status (SES). We measured SES of household of origin by respondent-reported parents’ education level.45–47 We assessed the respondent’s SES by a time-varying measure that combined school enrollment status and degree attainment.32,37,47,48 Finally, we included controls for race/ethnicity,49,50 US nativity, and gender.51 Table A, available as a supplement to the online version of this article at http://www.ajph.org, shows the descriptive statistics for all predictors and outcomes.
City-level policy data came from the Americans for Nonsmokers’ Rights Foundation (ANRF) tobacco policy database. The ANRF collected a complete national repository of tobacco-related ordinances and regulations within the country by date. The main predictor variables were (1) whether the respondent lived in a city with a comprehensive smoking ban, defined as policies mandating that workplaces, bars, and restaurants are 100% smoke-free with no indoor exceptions (pooled mean = 35.8%); and (2) the total excise taxes in that locale (pooled mean = $1.26; SD = 1.05). From the ANRF repository, we created a location–year data set at the state and city level for each data year using the effective date for the policies. Because the state policies are not independent of city policy (i.e., a state ban automatically implies a city ban and, therefore, the dummy variables must match), we recoded cities in states with bans to reflect this status.
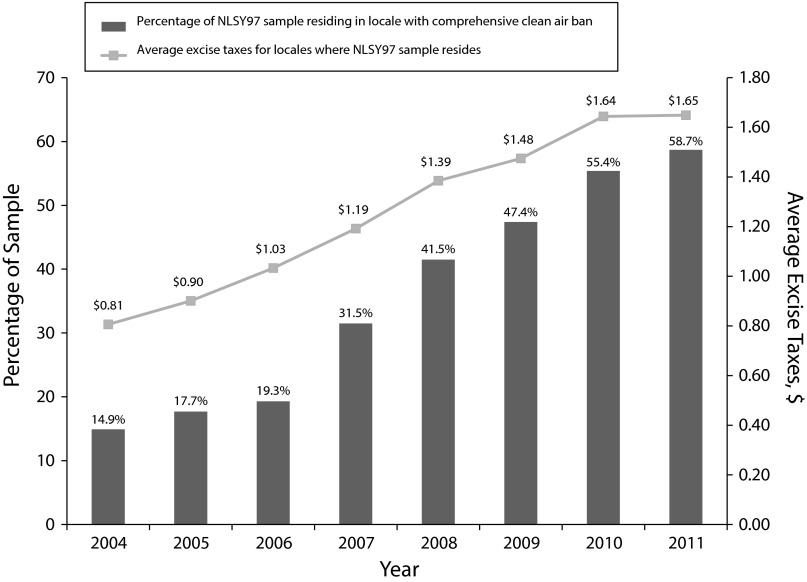
Similarly, total excise taxes reflect the per-pack sum of state taxes, from the Centers for Disease Control and Prevention, and city taxes, from ANRF. Thus, all policy information is statistically at the city level, but accounts for both state and local policies. We used Federal Information Processing Standard codes to link the geocoded NLSY97 to ANRF data at the city level, allowing us to determine the tobacco policy context within which respondents were located. Figure 1 displays both smoking bans and tax amounts by year for our respondents. There was a rapid increase over the observation period in both measures. The percentage living in a city with a comprehensive ban increased from 14.9% to 58.7% from 2004 to 2011, and average taxes increased from $0.81 to $1.65.
FIGURE 1—
Average Excise Tax and Percentage Subject to Comprehensive Clean Air Ban for US National Longitudinal Survey of Youth 1997 (NLSY97) Respondents by Year (2004–2011)
Several city-level measures from Census data are included as controls.52 Census data came from the 2000 and 2010 decennial censuses, with linear interpolation for in-between years and official estimates used for 2011. To include both population size and density, we created a categorical measure of population, and density was considered continuous (logged because of skewness). We included the percentage of female-headed households as a useful proxy for other economic measures such as poverty and income.53 To measure ties to the community, we used the percentage of owner-occupied housing. Finally, we included the percentage of non-Hispanic Whites and percentage of minors to account for community racial/ethnic and age composition, respectively.
Because of the various levels of analysis and a binary outcome, we used multilevel logistic regression models, also known as mixed-effects models, to estimate the effects of clean air policies and excise taxes on young adult smoking. Although respondents can move across cities and thus the structure is more akin to a cross-classified model, the loss in precision of the estimation of the variance components from using the typical multilevel structure is slight relative to the great computational advantage.54(p117) Among years spent within the subset located in the largest city within a CBSA, 15.3% were located among 2 cities, 2.3% among 3, and 0.4% among 4, such that the cross-classification of individual and city is of little consequence. Still, for robustness, we checked models for those who did and did not move and found similar results, and also included a fixed effect in all models to adjust for the average effect of moving across geographic units since the last survey.
In our analysis that used a typical hierarchical structure, then, observations were nested within individuals, who were nested within cities. Our 3-level model thus included random intercepts for both the individual level (level 2) and the city level (level 3). These models adjusted for the person- and city-level averages through a variance parameter that defines a normal distribution for each of those averages. At the lowest level of observation (level 1), the predictors represent time-varying measures for both the city and the individual. At the individual level, we have the time-invariant characteristics of the respondent. Because we did not include static city characteristics, the random intercept was the only term at level 3. All models used the XTMELOGIT procedure in Stata 14.0 (StataCorp LP, College Station, TX), with the MARGINS postestimation command used to estimate predicted values.
RESULTS
Table 1 shows the coefficients from our models for our policy variables of interest (see Table B, available as a supplement to the online version of this article at http://www.ajph.org, for the full table with all control variables). According to model 1 for the outcome of current smoking, even controlling for a robust set of covariates and excise taxes, there was a significant effect of comprehensive smoking bans. Those residing in cities with bans were 21.1% less likely to currently smoke. By comparison, there was no significant effect from taxes.
TABLE 1—
Multilevel Logistic Regression of Smoking Outcomes: US National Longitudinal Survey of Youth 1997 (2004–2011)
| Any Tobacco Use in Past 30 d, |
≥1 Pack Daily in Past 30 d, |
|||
| Variable | Model 1 | Model 2 | Model 3 | Model 4 |
| Comprehensive smoking ban | ||||
| Coefficient (SE) | −0.22* (0.10) | −0.51** (0.17) | −0.28 (0.17) | −0.57* (0.28) |
| OR (95% CI) | 0.70 (0.65, 0.98) | 0.60 (0.43, 0.84) | 0.755 (0.54, 1.06) | 0.56 (0.33, 0.97) |
| Excise taxes | ||||
| Coefficient (SE) | −0.04 (0.06) | −0.22* (0.10) | −0.20* (0.10) | −0.36* (0.16) |
| OR (95% CI) | 0.96 (0.86, 1.08) | 0.80 (0.66, 0.98) | 0.82 (0.68, 0.999) | 0.70 (0.51, 0.95) |
| Ban × taxes | ||||
| Coefficient (SE) | . . . | 0.22* (0.11) | . . . | 0.23 (0.17) |
| OR (95% CI) | . . . | 1.25 (1.02, 1.53) | . . . | 1.26 (0.90, 1.77) |
| Level 2 variance | 3.83 (0.09) | 3.84 (0.09) | 3.30 (0.15) | 3.30 (0.15) |
| Level 3 variance | 0.67 (0.13) | 0.67 (0.13) | 0.28 (0.26) | 0.23 (0.32) |
| Log likelihood | −8095.67 | −8093.45 | −2599.16 | −2598.27 |
Note. CI = confidence interval; OR = odds ratio. The displayed variance components account for the differences in averages on the outcomes across individuals (level 2) and cities (level 3). All models contain time-invariant controls for gender, race/ethnicity, US nativity, age cohort, parents’ education, parent self-reported health, baseline depression, high-school grades, and peer smoking in 1997; time-varying respondent controls for age, living with a parent, education, recent move between counties, employment status, job schedule, marital status, and parent status; and time-varying city control for population, population density, owner-occupied housing, percentage minors, female-headed households, and percentage non-Hispanic Whites.
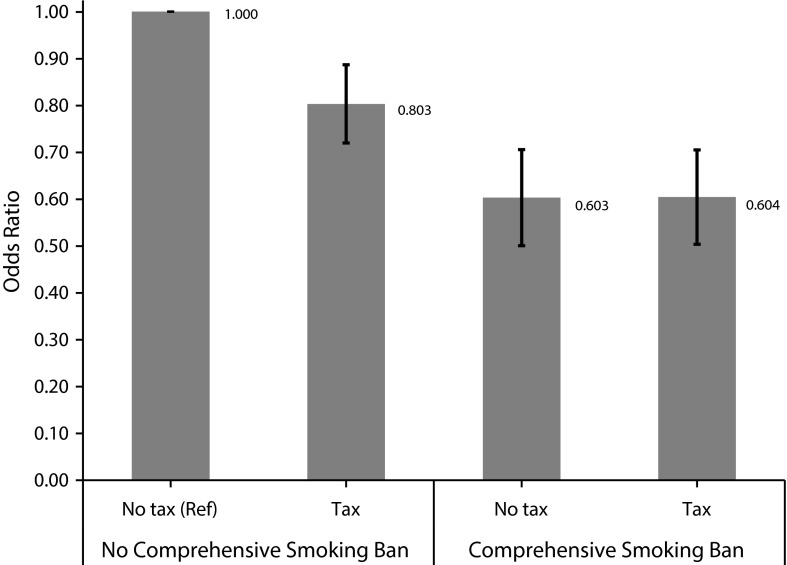
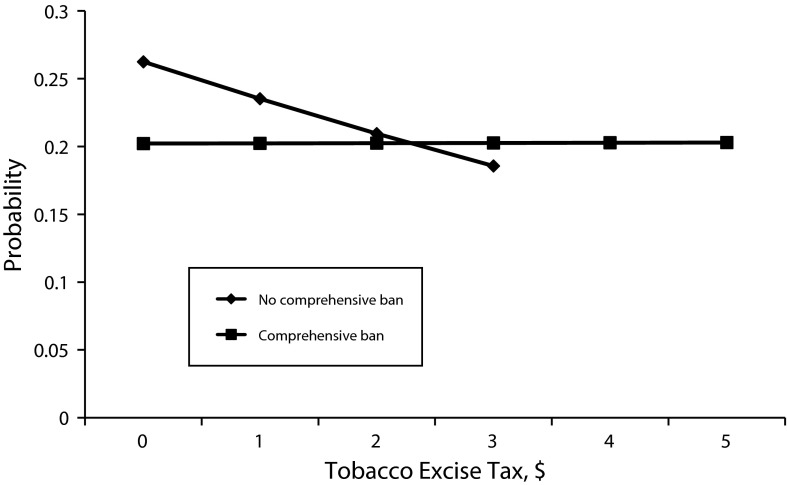
Turning to model 2, however, we found a significant interaction effect of the 2 tobacco policies, with the odds ratios for the interaction displayed in Figure 2. The main effect for excise taxes represents the slope for cities with no smoking ban. In such cities, an increase of $1 in taxes resulted in a 19.7% lower odds of individual-level current smoking ([1–0.803]*100% = −19.7%). The coefficient for bans now represents the effect when taxes are zero. In the absence of a tax, then, the odds of currently smoking were 39.7% lower when a smoking ban was in effect. By the definition of an interaction effect, the sum of the excise tax main effect (–0.220) and the interaction effect (0.222) represents the slope for taxes in cities with a comprehensive smoking ban, which is virtually zero (–0.220 + 0.222 = 0.002). In other words, taxes were of little consequence in cities with smoking bans, as reflected in the equal odds ratios for locations with comprehensive smoking bans in Figure 2. Figure 2, however, only displays the differences for a $1 increase in taxes. To understand the effect across the distribution of excise taxes, we display the predicted probability of current smoking by taxes and the presence of a ban in Figure 3. As reflected in the zero slope noted previously, the tax effect in cities with bans was negligible. Relative to the line for cities without bans, the largest effect of bans occurred in cities with no to low excise taxes. The effect of the ban became smaller as taxes increased, such that the effect of a ban became negligible relative to a city without a ban when taxes were just over $2 per pack. We note that the shorter length of the line for locales with no bans reflects the fact that the maximum excise taxes in such places was $3.40, compared with $5.85 for locales with a ban.
FIGURE 2—
Odds Ratios for Interaction Between City Comprehensive Smoking Ban and Tobacco Excise Lax on Any Tobacco Use in Past 30 Days: US National Longitudinal Survey of Youth 1997 (2004–2011)
Note. Tax effect represents the difference for a $1 increase. The reference group is no tax, no comprehensive smoking ban. The error bars represent the 95% confidence interval for the odds ratio.
FIGURE 3—
Interaction Between City Comprehensive Smoking Ban and Tobacco Excise Tax: US National Longitudinal Survey of Youth 1997 (2004–2011)
Note. The length of the line for locales with no comprehensive smoking bans is shorter to avoid extrapolation resulting from the lower maximum for taxes in such places ($3.40), compared with locales with bans ($5.85). For interaction, P = .035.
The results for smoking a pack daily are shown in model 3. Without the interaction, we found the opposite effect in comparison with any current smoking: excise taxes significantly reduced the odds of daily pack smoking, whereas smoking bans did not. A $1 increase in taxes was associated with 17.9% lower odds of daily pack smoking. Model 4 shows that the interactive effect was nonsignificant, although the significant main effects were still informative, yet should be interpreted with caution. When taxes were zero, we again found a significant effect of smoking bans, such that those in cities with bans were 43.6% less likely to smoke a pack daily. Similarly, there was a significant reduction in daily pack smoking as taxes increased in cities with no bans (by 30.0% per $1), although the interaction term tells us that this slope was not significantly different in cities with smoking bans. We note that we also interacted the policy terms by time to determine if these effects varied across the period of observation; these terms were nonsignificant.
DISCUSSION
These findings provide further evidence for the efficacy of comprehensive clean air policies and excise taxes as tobacco-control tools. Yet, we found that their influence is dependent upon the form of smoking under consideration. Our results indicate that any smoking in the past 30 days among young adults is inhibited by comprehensive smoking bans. The outcome of any current smoking includes a large pool of young adults who smoke, but do not smoke at a daily pack level. This indicates that smoking bans may be most effective in deterring social-smoking young adults, which may be an important point of early intervention. Given the interaction, comprehensive clean air policies are most pertinent as a tobacco-control strategy in locations with low excise taxes. Excise taxes only deter such social smoking in the absence of a ban, and the impact eventually converges with that of smoking bans at high-enough tax rates. This finding does not imply that bans are ineffective in high-tax environments, but simply that the addition of higher excise taxes does not further deter young adult social smoking.
By contrast, heavy smokers are primarily deterred by economic costs incurred through higher excise taxes. We also found limited support for the influence of bans on heavy smoking in places with no taxes, though, given the nonsignificant interaction term, we interpret this finding with caution. Importantly, these policy effects were robust to the inclusion of a considerable battery of control variables at both the individual and city levels.
Although both policies had an impact on young adult smoking behaviors, their dual presence did not intensify each policy’s efficacy. In other words, smoking bans and high excise taxes together do not appear to have an additional effect beyond that of each policy in the absence of the other. This finding reiterates that either tobacco-control policy can have some impact, as exemplified by the highest levels of smoking occurring in cities with low taxes and no smoking bans. Importantly, there are multiple policy pathways to reducing young people’s smoking, with variation depending on the outcome measure, giving policymakers several effective options for tobacco control. Furthermore, even though the effect of bans and taxes on young adult smoking may converge at high-enough tax levels, studies have found other health benefits to passing comprehensive clean air policies, often related to reductions in secondhand smoke intake,55–57 and excise taxes, such as reductions in prenatal exposure.58 Yet, the uneven geographic distribution of these laws may reinforce health disparities as these policies are more likely to be passed in locations with higher per-capita incomes, higher education, and lower percentage of non-Hispanic Blacks after accounting for urbanity.59,60 If one considers that clean air policies both directly inhibit smoking and foster the denormalization of tobacco use, policymakers should work to ensure a fair distribution of such tobacco controls to promote the health of all.
We are careful to note limitations within our study. First, we only included young adults whose city we could identify. The subset of analyzed respondents was similar on almost all individual-level variables as the sample as a whole, with 2 exceptions. In light of our focus on cities, it was not surprising that Blacks were somewhat overrepresented (34% in subset vs 27% in whole sample) and Whites were underrepresented (40% vs 50%) relative to the entire sample. The subset was also more likely to work. We were careful to limit our generalizability to young people living in such locales. Furthermore, CBSAs were first measured in 2004, such that we examined those aged 19 to 31 years. Although we restricted the data to those aged 19 years and older, we do not view this restriction as negative as that constitutes an age when young adults begin to frequent establishments such as bars and nightclubs with the most between-city variation in clean air policy, and can legally purchase tobacco products. In addition, members of the longitudinal cohort self-reported smoking behaviors, which may be subject to recall and social desirability biases, as is common in behavioral research.
This article has taken an important next step in the analysis of excise taxes and comprehensive clean air policies as a means of tobacco control among young adults. The strengths include directly linking policy and individual behavior over time, examining the important city-level policy context, and modeling the potential interactive impact of both policies. In sum, we found comprehensive smoking bans and excise taxes to be important forms of tobacco control for young people, but there appear to be no synergistic effects in locations with both policies. Furthermore, each policy has an impact on a different form of tobacco use.
ACKNOWLEDGMENTS
This work was supported by the National Institute on Drug Abuse (grant R03DA034933; PI: Vuolo).
This research was conducted with restricted access to Bureau of Labor Statistics data. The authors would like to thank the staff at the American Nonsmokers’ Rights Foundation, particularly Maggie Hopkins and Laura Walpert. We also thank Emily Harris, Alexandra Marin, Jake Brosius, and Emily Ekl for research assistance.
Note. The views expressed here do not necessarily reflect the views of the Bureau of Labor Statistics, National Institute on Drug Abuse, or American Nonsmokers’ Rights Foundation.
HUMAN PARTICIPANT PROTECTION
The study was approved by the Purdue University institutional review board.
Footnotes
See also Galea and Vaughan, p. 201.
REFERENCES
- 1.Bayer R, Stuber J. Tobacco control, stigma, and public health: rethinking the relations. Am J Public Health. 2006;96(1):47–50. doi: 10.2105/AJPH.2005.071886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rockville, MD: US Department of Health and Human Services, Office of the Surgeon General; 2010. How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the Surgeon General. [PubMed] [Google Scholar]
- 3.Kelly BC. Smoke-free air policy: subcultural shifts and secondary health effects among NYC club-going youth. Sociol Health Illn. 2009;31(4):569–582. doi: 10.1111/j.1467-9566.2008.01150.x. [DOI] [PubMed] [Google Scholar]
- 4.Chassin L, Presson CC, Pitts SC et al. The natural history of cigarette smoking from adolescence to adulthood in a Midwestern community sample: multiple trajectories and their psychosocial correlates. Health Psychol. 2000;19(3):223–231. [PubMed] [Google Scholar]
- 5.Wills TA, Resko JA, Ainette MG et al. Smoking onset in adolescence: a person-centered analysis with time-varying predictors. Health Psychol. 2004;23(2):158–167. doi: 10.1037/0278-6133.23.2.158. [DOI] [PubMed] [Google Scholar]
- 6.Warner KE, Sexton DW, Gillespie BW et al. Impact of tobacco control on adult per capita cigarette consumption in the United States. Am J Public Health. 2014;104(1):83–89. doi: 10.2105/AJPH.2013.301591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boardman JD, Blalock CL, Pampel FC. Trends in the genetic influences on smoking. J Health Soc Behav. 2010;51(1):108–123. doi: 10.1177/0022146509361195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levy DT, Romano E, Mumford E. The relationship of smoking cessation to sociodemographic characteristics, smoking intensity, and tobacco control policies. Nicotine Tob Res. 2005;7(3):387–396. doi: 10.1080/14622200500125443. [DOI] [PubMed] [Google Scholar]
- 9.Chahine T, Subramanian SV, Levy JI. Sociodemographic and geographic variability in smoking in the US: a multilevel analysis of the 2006–2007 Current Population Survey, Tobacco Use Supplement. Soc Sci Med. 2011;73(5):752–758. doi: 10.1016/j.socscimed.2011.06.032. [DOI] [PubMed] [Google Scholar]
- 10.Vuolo M. Placing deviance in a legal and local context: a multilevel analysis of cigarette use in the European Union. Soc Forces. 2012;90:1377–1402. [Google Scholar]
- 11.Nagelhout GE, Mons U, Allwright S et al. Prevalence and predictors of smoking in “smoke-free” bars: findings from the International Tobacco Control (ITC) Europe Surveys. Soc Sci Med. 2011;72(10):1643–1651. doi: 10.1016/j.socscimed.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shang C. The effect of smoke-free air law in bars on smoking initiation and relapse among teenagers and young adults. Int J Environ Res Public Health. 2015;12(1):504–520. doi: 10.3390/ijerph120100504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farrelly MC, Loomis BR, Han B et al. A comprehensive examination of the influence of state tobacco control programs and policies on youth smoking. Am J Public Health. 2013;103(3):549–555. doi: 10.2105/AJPH.2012.300948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siegel M, Albers AB, Cheng DM et al. Effect of local restaurant smoking regulations on environmental tobacco smoke exposure among youths. Am J Public Health. 2004;94(2):321–325. doi: 10.2105/ajph.94.2.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kilgore EA, Mandel-Ricci J, Johns M et al. Making it harder to smoke and easier to quit: the effect of 10 years of tobacco control in New York City. Am J Public Health. 2014;104(6):e5–e8. doi: 10.2105/AJPH.2014.301940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanders A, Slade G. State cigarette excise tax, secondhand smoke exposure, and periodontitis in US nonsmokers. Am J Public Health. 2013;103(4):740–746. doi: 10.2105/AJPH.2011.300579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song AV, Dutra LM, Neilands TB et al. Association of smoke-free laws with lower percentages of new and current smokers among adolescents and young adults: an 11-year longitudinal study. JAMA Pediatr. 2015;169(9):e152285. doi: 10.1001/jamapediatrics.2015.2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jha P, Peto R. Global effects of smoking, of quitting, and of taxing tobacco. N Engl J Med. 2014;370(1):60–68. doi: 10.1056/NEJMra1308383. [DOI] [PubMed] [Google Scholar]
- 19.Chaloupka FJ, Yurekli A, Fong JT. Tobacco taxes as a tobacco control strategy. Tob Control. 2012;21(2):172–180. doi: 10.1136/tobaccocontrol-2011-050417. [DOI] [PubMed] [Google Scholar]
- 20.Becker GS, Grossman M, Murphy KM. An empirical analysis of cigarette addiction. Am Econ Rev. 1994;84:396–418. [Google Scholar]
- 21.Farrelly MC, Bray JW, Pechacek T et al. Response by adults to increases in cigarette prices by sociodemographic characteristics. South Econ J. 2001;68:156–165. [Google Scholar]
- 22.Tauras JA. Public policy and smoking cessation among young adults in the United States. Health Policy. 2004;68(3):321–332. doi: 10.1016/j.healthpol.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Jiménez-Ruiz JA, Saenz de Miera B, Reynales-Shigematsu LM et al. The impact of taxation on tobacco consumption in Mexico. Tob Control. 2008;17(2):105–110. doi: 10.1136/tc.2007.021030. [DOI] [PubMed] [Google Scholar]
- 24.Townsend J, Roderick P, Cooper J. Cigarette smoking by socioeconomic group, sex, and age: effects of price, income and health publicity. BMJ. 1994;309(6959):923–927. doi: 10.1136/bmj.309.6959.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chaloupka FJ. Macro-social influences: the effects of prices and tobacco-control policies on the demand for tobacco products. Nicotine Tob Res. 1999;1(suppl 1):S105–S109. doi: 10.1080/14622299050011681. [DOI] [PubMed] [Google Scholar]
- 26.Gallet CA, List JA. Cigarette demand: a meta-analysis of elasticities. Health Econ. 2003;12(10):821–835. doi: 10.1002/hec.765. [DOI] [PubMed] [Google Scholar]
- 27.Blecher EH, van Walbeek CP. An international analysis of cigarette affordability. Tob Control. 2004;13(4):339–346. doi: 10.1136/tc.2003.006726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sung HY, Hu T, Ong M et al. A major state tobacco tax increase, the Master Settlement Agreement, and cigarette consumption: the California experience. Am J Public Health. 2005;95(6):1030–1035. doi: 10.2105/AJPH.2004.042697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Powell LM, Tauras JA, Ross H. The importance of peer effects, cigarette prices, and tobacco control policies for youth smoking behavior. J Health Econ. 2005;24(5):950–968. doi: 10.1016/j.jhealeco.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 30.Shipan CR, Volden C. Bottom-up federalism: the diffusion of antismoking policies from US cities to states. Am J Pol Sci. 2006;50:825–843. [Google Scholar]
- 31.Yang Y. Aging, cohorts, and methods. In: Binstock RH, George LK, editors. Handbook of Aging and the Social Sciences. 7th ed. New York, NY: Academic Press; 2010. pp. 17–30. [Google Scholar]
- 32.Bachman JG, Wadsworth KN, O’Malley PM . Smoking, Drinking, and Drug Use in Young Adulthood: The Impacts of New Freedoms and Responsibilities. Mahwah, NJ: Lawrence Erlbaum; 1997. [Google Scholar]
- 33.Fleming CB, White HR, Catalano RF. Romantic relationships and substance use in early adulthood: an examination of the influences of relationship type, partner substance use, and relationship quality. J Health Soc Behav. 2010;51(2):153–167. doi: 10.1177/0022146510368930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brown SL, Rinelli LN. Family structure, family processes, and adolescent smoking and drinking. J Res Adolesc. 2010;20(2):259–273. doi: 10.1111/j.1532-7795.2010.00636.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson MK. Further evidence on adolescent employment and substance use: differences by race and ethnicity. J Health Soc Behav. 2004;45(2):187–197. doi: 10.1177/002214650404500205. [DOI] [PubMed] [Google Scholar]
- 36.Alexander C, Piazza M, Mekos D et al. Peers, schools, and adolescent cigarette smoking. J Adolesc Health. 2001;29(1):22–30. doi: 10.1016/s1054-139x(01)00210-5. [DOI] [PubMed] [Google Scholar]
- 37.Schulenberg J, Bachman JG, O’Malley PM et al. High school educational success and subsequent substance use: a panel analysis following adolescents into young adulthood. J Health Soc Behav. 1994;35(1):45–62. [PubMed] [Google Scholar]
- 38.Swan GE, Javitz HS, Jack LM et al. Heterogeneity in 12-month outcome among female and male smokers. Addiction. 2004;99(2):237–250. doi: 10.1111/j.1360-0443.2003.00629.x. [DOI] [PubMed] [Google Scholar]
- 39.Serbin LA, Karp J. The intergenerational transfer of psychosocial risk: mediators of vulnerability and risk. Annu Rev Psychol. 2004;55:333–363. doi: 10.1146/annurev.psych.54.101601.145228. [DOI] [PubMed] [Google Scholar]
- 40.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 41.Bygren LO. Intergenerational health responses to adverse and enriched environments. Annu Rev Public Health. 2013;34:49–60. doi: 10.1146/annurev-publhealth-031912-114419. [DOI] [PubMed] [Google Scholar]
- 42.Wakschlag LS, Pickett KE, Cook E et al. Maternal smoking during pregnancy and severe antisocial behavior in offspring: a review. Am J Public Health. 2002;92(6):966–974. doi: 10.2105/ajph.92.6.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kandel DB, Griesler PC, Hu MC. Intergenerational patterns of smoking and nicotine dependence among US adolescents. Am J Public Health. 2015;105(11):e63–e72. doi: 10.2105/AJPH.2015.302775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kennedy-Hendricks A, Schwartz H, Thornton RJ et al. Intergenerational social networks and health behaviors among children living in public housing. Am J Public Health. 2015;105(11):2291–2297. doi: 10.2105/AJPH.2015.302663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Friestad C, Pirkis J, Biehl M et al. Socioeconomic patterning of smoking, sedentary lifestyle, and overweight status among adolescents in Norway and the United States. J Adolesc Health. 2003;33(4):275–278. doi: 10.1016/s1054-139x(03)00214-3. [DOI] [PubMed] [Google Scholar]
- 46.Soteriades ES, DiFranza JR. Parents’ socioeconomic status, adolescents’ disposable income, and adolescents’ smoking status in Massachusetts. Am J Public Health. 2003;93(7):1155–1160. doi: 10.2105/ajph.93.7.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pampel FC, Mollborn S, Lawrence EM. Life course transitions in early adulthood and SES disparities in tobacco use. Soc Sci Res. 2014;43:45–59. doi: 10.1016/j.ssresearch.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Margolis R. Educational differences in healthy behavior changes and adherence among middle-aged Americans. J Health Soc Behav. 2013;54(3):353–368. doi: 10.1177/0022146513489312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johnson RA, Hoffmann JP. Adolescent cigarette smoking in US racial/ethnic subgroups: findings from the National Education Longitudinal Study. J Health Soc Behav. 2000;41(4):392–407. [PubMed] [Google Scholar]
- 50.Pampel FC. Racial convergence in cigarette use from adolescence to the mid-thirties. J Health Soc Behav. 2008;49(4):484–498. [PMC free article] [PubMed] [Google Scholar]
- 51.Pampel FC. Cigarette diffusion and sex differences in smoking. J Health Soc Behav. 2001;42(4):388–404. [PubMed] [Google Scholar]
- 52.Mathur C, Erickson DJ, Stigler MH et al. Individual and neighborhood socioeconomic status effects on adolescent smoking: a multilevel cohort-sequential latent growth analysis. Am J Public Health. 2013;103(3):543–548. doi: 10.2105/AJPH.2012.300830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.LeClere FB, Rogers RG, Peters K. Neighborhood social context and racial differences in women’s heart disease mortality. J Health Soc Behav. 1998;39(2):91–107. [PubMed] [Google Scholar]
- 54.Goldstein H. Multilevel Statistical Models, First Internet Edition. London, England: Institute of Education; 1999. [Google Scholar]
- 55.Pell JP, Haw S, Cobbe S et al. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med. 2008;359(5):482–491. doi: 10.1056/NEJMsa0706740. [DOI] [PubMed] [Google Scholar]
- 56.Menzies D, Nair A, Williamson PA et al. Respiratory symptoms, pulmonary function, and markers of inflammation among bar workers before and after a legislative ban on smoking in public places. JAMA. 2006;296(14):1742–1748. doi: 10.1001/jama.296.14.1742. [DOI] [PubMed] [Google Scholar]
- 57.Lin HC, Park J, Seo D. Comprehensive US statewide smoke-free indoor air legislation and secondhand smoke exposure, asthma prevalence, and related doctor visits: 2007–2011. Am J Public Health. 2015;105(8):1617–1622. doi: 10.2105/AJPH.2015.302596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hawkins SS, Baum CF. Impact of state cigarette taxes on disparities in maternal smoking during pregnancy. Am J Public Health. 2014;104(8):1464–1470. doi: 10.2105/AJPH.2014.301955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Huang J, King BA, Babb SD et al. Sociodemographic disparities in local smoke-free law coverage in 10 states. Am J Public Health. 2015;105(9):1806–1813. doi: 10.2105/AJPH.2015.302655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gonzalez M, Sanders-Jackson A, Song AV et al. Strong smoke-free law coverage in the United States by race/ethnicity: 2000–2009. Am J Public Health. 2013;103(5):e62–e66. doi: 10.2105/AJPH.2012.301045. [DOI] [PMC free article] [PubMed] [Google Scholar]