Abstract
Foramen of Winslow hernia is a rare surgical entity with very few reported cases in literature. Preoperative diagnosis used to be difficult but with emerging computed tomography technology, diagnosing this internal abdominal hernia has become easier.
We present an unusual case report of foramen of Winslow hernia in a 77-year-old patient who presented with severe abdominal pain. The patient underwent laparoscopic repair of the hernia and recovered well postoperatively.
This presentation of symptoms in a 77-year-old male is unusual and laparoscopic management of foramen of Winslow hernia presents an interesting and challenging management scenario.
Keywords: foramen of Winslow hernia, epiploic foramen, epiploic hernia, hernia into lesser sac, internal abdominal hernia
First described in 1834 by Blandin,1 Foramen of Winslow hernia is a distinct clinical entity with very few reported cases in literature. This is a type of internal hernia usually formed from protrusion of a viscous through a peritoneal or mesenteric defect within the abdominal cavity.2 This defect could either be a preexisting anatomical structure or an acquired defect.2 It is a rare cause of bowel obstruction and typically presents with abdominal symptoms. Treatment usually involves emergent surgery with reduction of hernia and fixation of cecum with closure of the hernia defect.1 We present a case of foramen of Winslow hernia that was diagnosed preoperatively on computed tomography (CT) and was successfully repaired laparoscopically.
Case Presentation
Our patient is a 77-year-old male who presented to the emergency room after experiencing some severe crampy and diffuse abdominal pain. His pain started 5 hours ago before arrival and on presentation, he was in excruciating pain. The patient denied any other complaints such as nausea, vomiting or diarrhea. He denied any shortness of breath, chest pain, radiation of pain or any history of recent trauma. He denied any symptoms of bloating and stated that he had a regular bowel movement earlier in the day and had been doing well until this episode of pain. His past medical history was significant for a history of hypertension and a prostatectomy done 10 years ago.
On presentation, he was afebrile and hemodynamically stable with a blood pressure of 135/86 mm Hg and a heart rate of 97 beats per minute. On physical examination, he had mild tenderness in the epigastric region. The patient had no evidence of abdominal distension or any evidence of generalized peritonitis. His blood work was only remarkable for a high white blood cell count of 16,400.
He underwent a CT scan with oral and intravenous contrast to look for the cause of his pain. The preliminary read by the radiologist did not suggest any underlying pathology and by the time the CT scan was performed, the patient's pain had improved on its own without the use of any pain relieving medicines. He felt much better and with resolved symptoms and a preliminary normal radiographic finding, the emergency room physician discharged the patient home. The CT scan was reviewed again by the radiologist who saw a mobile cecum located in the lesser sac between the stomach and pancreas with mesenteric swirling raising a concern for foramen of Winslow hernia with bowel ischemia. With this new finding, the patient was appropriately called back to return to the emergency room.
On his return, a surgical consultant was called to look in to this clinical entity and suggest management options in the scenario of resolved abdominal pain. On examination by the surgery team, patient reported no symptoms and had no abdominal tenderness or distension. With the knowledge of presence of foramen of Winslow hernia on the CT scan and with complete resolution of symptoms, it was decided to observe the patient with serial abdominal exams, and repeat the CT scan to see if the hernia was still present.
The CT scan was repeated after couple of hours and it showed a persistent foramen of Winslow hernia with mesenteric swirling with no evidence of bowel obstruction or ischemia (Figs. 1 and 2). With a persistent hernia, the patient was taken to the operating room and a diagnostic laparoscopy was performed with an infraumbilical 11 mm port, one right lateral 5 mm port and one left lateral 5 mm port. Diagnostic laparoscopy confirmed the presence of hernia with the cecum and terminal ileum seen to be herniating in to the lesser sac through the foramen of Winslow with distension of the cecum consistent with a partial obstruction at the hernia orifice.
Fig. 1.
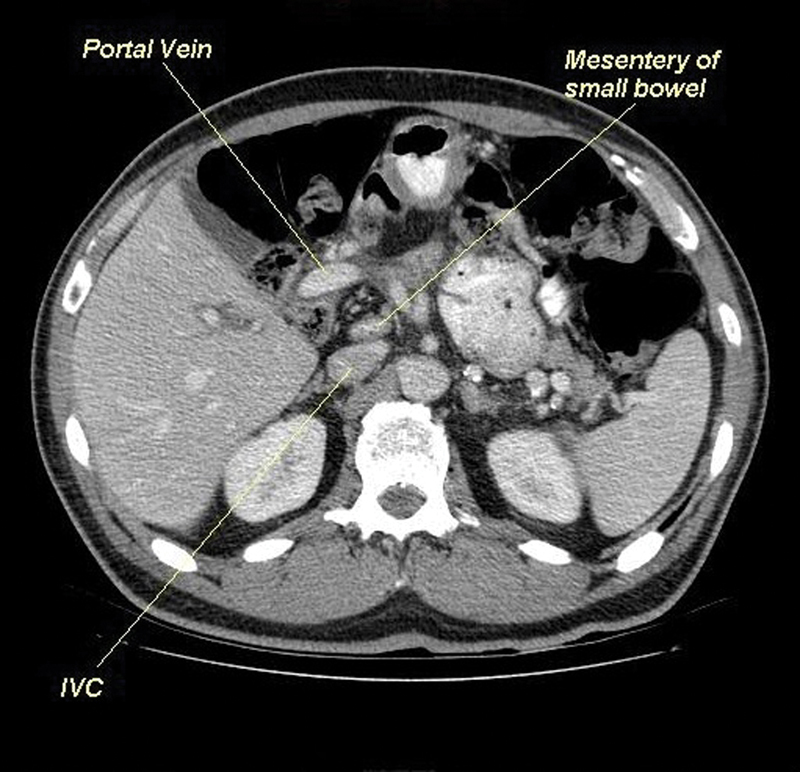
A CT scan showing loop of bowel between IVC and portal vein. CT, computed tomography; IVC, inferior vena cava.
Fig. 2.
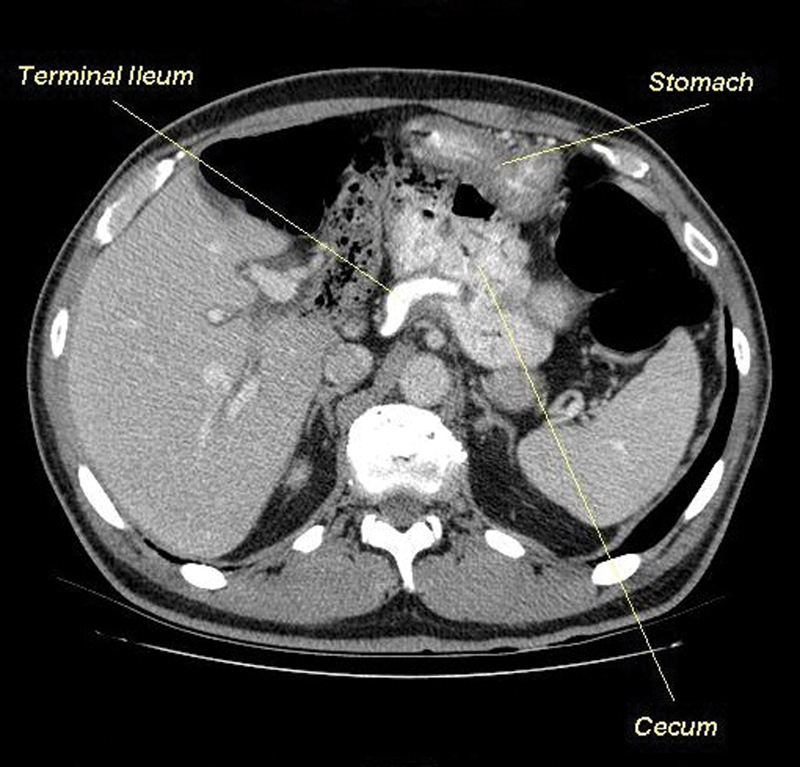
A CT scan showing terminal ileum and cecum within Foramen of Winslow. CT, computed tomography.
At this juncture, it was felt comfortable to proceed laparoscopically to fix the hernia, though with very few instances reported in the literature. We first proceeded with gently retracting the gallbladder and liver cephalad exposing the portal triad. With good exposure, the ascending colon and cecum were seen to taper through the hernia, medial to the portal triad (Fig. 3). The ascending colon was grasped and then carefully reduced along with cecum and terminal ileum out of the hernia underneath the portal triad and back in to the abdominal cavity. The foramen of Winslow was then closed with silk sutures by suturing the peritoneum adjacent to the portal triad down to the retroperitoneum just lateral to the inferior vena cava (IVC) (Fig. 4). Attention was then turned toward the large bowel and it was noted that the patient had an extremely redundant ascending colon and cecum with an abnormal medial location of the appendix heading toward the foramen of Winslow with mesenteric fixation. It was felt necessary to do an appendectomy to release the cecum so that it could be placed back in the right lower quadrant. The cecum was very floppy and redundant and to prevent any future recurrences, a cecopexy was performed by securing the cecum to the anterolateral abdominal wall. Small bowel was then ran laparoscopically and showed no evidence of ischemia or any twisting of the mesentery. The entire procedure was performed laparoscopically with three ports and patient recovered well from the surgery. He had a short uneventful postoperative course and was discharged home the next day after he tolerated a regular diet.
Fig. 3.
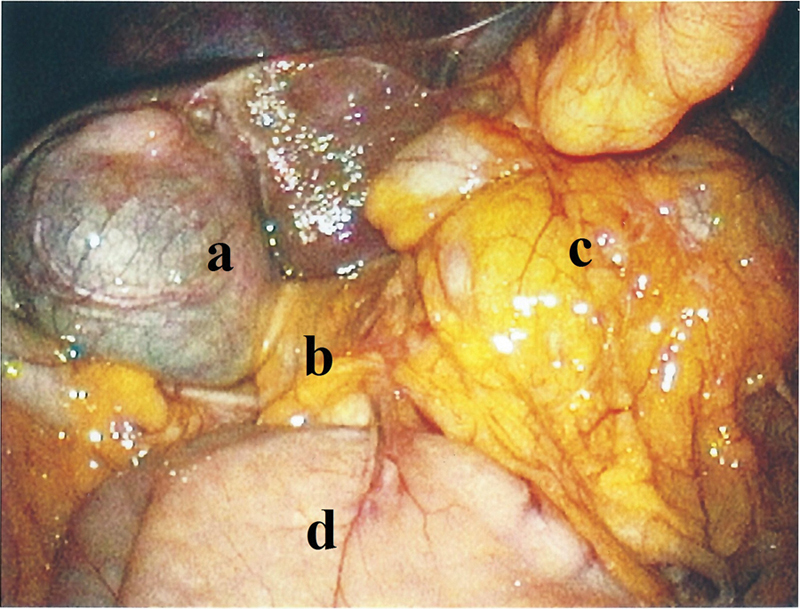
Laparoscopic view depicting: (a) gallbladder, (b) Foramen of Winslow, (c) Cecum going into hernia and (d) stomach.
Fig. 4.
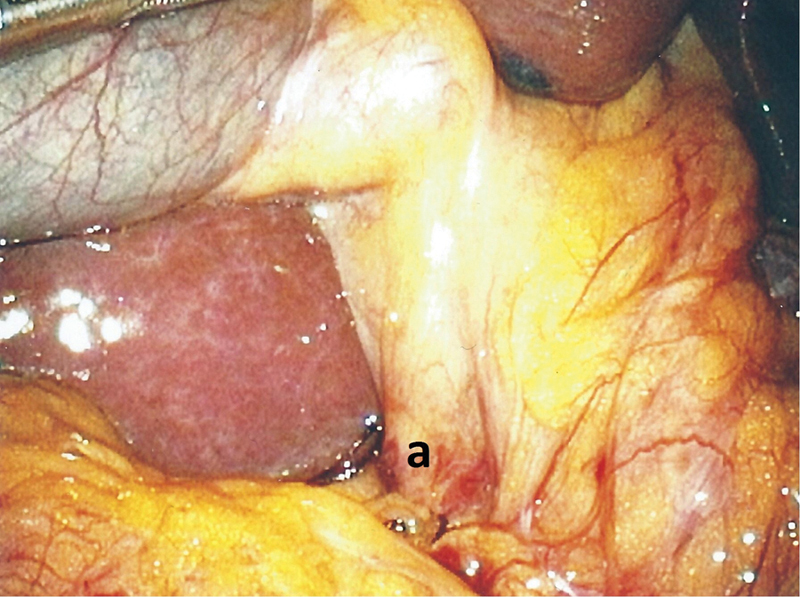
Laparoscopic view depicting: (a) Foramen of Winslow sutured closed.
Discussion
Foramen of Winslow was first described by Jacobus Benignus Winslow (1669–1760).1 This Foramen can be the cause of a rare internal abdominal hernia that usually presents as bowel obstruction.1 Internal hernias can be classified according to location into paraduodenal (50–55%), pericecal (10–15%), foramen of Winslow (8%), transmesenteric and transmesocolic (8%), pelvic and paravesical (6%), sigmoid (6%), and transomental (1–4%).3 Foramen of Winslow hernia is reported to occur at 0.2 to 0.9% of necropsy studies.3 Foramen of Winslow is a normal anatomical peritoneal orifice that usually remains closed from the intraabdominal pressure and usually does not allow viscera to go through it. It allows virtual communication between the greater peritoneal cavity and lesser sac.2
The foramen of Winslow is bounded above by the peritoneum on the caudate process of the liver, below by the peritoneum covering the first part of the duodenum, behind by the peritoneum covering the IVC, and in front by the free edge of the lesser omentum, containing the portal vein, the hepatic artery, and the common bile duct. It normally admits one finger and allows entry into the lesser peritoneal sac.4 In one of the published reports by Roberts, 45 cases involved herniation of the small bowel, 16 of the right side of the colon and cecum, and five of the transverse colon.5
Many factors have been implicated in the cause of this hernia such as abnormally large foramen, the presence of an abnormally long hypermobile small-bowel mesentery,6 a redundant ascending colon with cecum allowing marked mobility of the colon, failure of right colon to retroperitonealize7 and even an enlarged right hepatic lobe that could be directing the intestinal loops into the foramen.2
The clinical presentation can include a spectrum of symptoms ranging from upper abdominal pain mostly in the epigastric area to signs and symptoms of acute bowel obstruction such as nausea and vomiting.1 2 Symptoms are mild where the hernia reduces easily resulting in intermittent symptoms and diagnosis can be delayed. This delay in diagnosis can result in the development of gangrenous bowel requiring resection.8 Clinical examination is usually nonspecific and seldom helps in diagnosing this condition. Physical exam cannot palpate the herniated mass and peritonitis is rarely present. Laboratory findings are not that helpful either.8
Early diagnosis is imperative as delay in recognition of this hernia can result in significant morbidity and mortality.4 5 Radiographic imaging is the mainstay to diagnose this hernia preoperatively. CT scan is the imaging modality of choice with some specific radiological signs such as a thin-walled retro-gastric collection, absence of ascending colon in the right abdominal region, mesentery or bowel posterior to the portal triad, and presence of mesentery between the IVC and portal vein. Anterior and lateral displacement of the stomach may be present too. Plain radiographs characteristically demonstrate gas filled loops of large bowel within the epigastrium or left upper quadrant with anterior and lateral displacement of the stomach.2 9 10
Surgery involves urgent laparotomy and/or laparoscopic reduction of hernia via the foramen of Winslow. The herniation may be reduced by simply pushing the herniated colon back through the foramen squeezing the air back into the distal colon. Previous techniques have reported enlarging the foramen by performing a Kocher maneuver, thus lifting the duodenum with its hepatoduodenal ligament away from the IVC.4 If this proves difficult, the gastrohepatic or gastrocolic ligaments can be opened or a large Kocher maneuver can be performed to help.8
Treatment may also involve bowel resection, if the bowel herniating is ischemic.1 In our patient, we were able to pull the colonic segment out laparoscopically from the hernia and there was no evidence of ischemia. Literature is scarce regarding recurrences with most literature reporting no recurrence.1 4 However, methods used to prevent recurrence have been occlusion of foramen by suture and/or cecopexy where in the cecum is tacked to the anterior abdominal wall in the right iliac fossa.4 Literature is also divided regarding the need to close the foramen with sutures with recent literature recommending closing the foramen of Winslow defect if it can be done safely.9
Conclusion
Foramen of Winslow hernia can be diagnosed with a great deal of confidence preoperatively with the help of CT. Untreated mortality rate is high and definitive treatment is surgery. Exploratory laparotomy used to be the most common way of performing these surgeries but with advent of laparoscopy, these internal hernias can be repaired laparoscopically successfully with decreased length of stay.
References
- 1.Higgins P M, Eadie D GA. Herniation through the Foramen of Winslow. Ann Surg. 1965;161(4):592–596. doi: 10.1097/00000658-196504000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martin L C, Merkle E M, Thompson W M. Review of internal hernias: radiographic and clinical findings. AJR Am J Roentgenol. 2006;186(3):703–717. doi: 10.2214/AJR.05.0644. [DOI] [PubMed] [Google Scholar]
- 3.Takeyama N, Gokan T, Ohgiya Y. et al. CT of internal hernias. Radiographics. 2005;25(4):997–1015. doi: 10.1148/rg.254045035. [DOI] [PubMed] [Google Scholar]
- 4.Blevis L S, Van Patter H T. Hernia through the foramen of Winslow. Can Med Assoc J. 1963;88(2):89–92. [PMC free article] [PubMed] [Google Scholar]
- 5.Lane-Roberts PA Hernia through the foramen of Winslow. Guy's Hosp Rep. 1953;102:253–264. [PubMed] [Google Scholar]
- 6.Cook J L. Bowel herniation through the foramen of winslow. Am Surg. 1970;36(4):241–247. [PubMed] [Google Scholar]
- 7.Wojtasek D A, Codner M A, Nowak E J. CT diagnosis of cecal herniation through the foramen of Winslow. Gastrointest Radiol. 1991;16(1):77–79. doi: 10.1007/BF01887310. [DOI] [PubMed] [Google Scholar]
- 8.Jacquemin G, Boeur J P, Laloux P. Caecum and ascending colon herniated in the lesser sac through the Winslow's hiatus. A case report. Acta Chir Belg. 2008;108(1):127–129. [PubMed] [Google Scholar]
- 9.Osvaldt A B, Mossmann D F, Bersch V P, Rohde L. Intestinal obstruction caused by a foramen of Winslow hernia. Am J Surg. 2008;196(2):242–244. doi: 10.1016/j.amjsurg.2007.05.058. [DOI] [PubMed] [Google Scholar]
- 10.Selçuk D, Kantarci F, Oğüt G, Korman U. Radiological evaluation of internal abdominal hernias. Turk J Gastroenterol. 2005;16(2):57–64. [PubMed] [Google Scholar]


