Abstract
Background
Quadriceps strength deficits are observed clinically following anterior cruciate injury and reconstruction and are often not overcome despite rehabilitation. Given that quadriceps strength may be important for achieving symmetrical joint biomechanics and promoting long-term joint health, determining the magnitude of strength deficits that lead to altered mechanics is critical.
Purpose
To determine if the magnitude of quadriceps strength asymmetry alters knee and hip biomechanical symmetry, as well as functional performance and self-reported function.
Study Design
Cross-Sectional study.
Methods
Seventy-three patients were tested at the time they were cleared for return to activity following ACL reconstruction. Quadriceps strength and activation, scores on the International Knee Documentation Committee form, the hop for distance test, and sagittal plane lower extremity biomechanics were recorded while patients completed a single-legged hop.
Results
Patients with high and moderate quadriceps strength symmetry had larger central activation ratios as well as greater limb symmetry indices on the hop for distance compared to patients with low quadriceps strength symmetry (P<0.05). Similarly, knee flexion angle and external moment symmetry was higher in the patients with high and moderate quadriceps symmetry compared to those with low symmetry (P<0.05). Quadriceps strength was found to be associated with sagittal plane knee angle and moment symmetry (P<0.05).
Conclusion
Patients with low quadriceps strength displayed greater movement asymmetries at the knee in the sagittal plane. Quadriceps strength was related to movement asymmetries and functional performance. Rehabilitation following ACL reconstruction needs to focus on maximizing quadriceps strength, which likely will lead to more symmetrical knee biomechanics.
Key Terms: muscle, isometrics, biomechanics, knee, return to activity
INTRODUCTION
Quadriceps strength deficits are commonplace following anterior cruciate ligament (ACL) injury and reconstruction.37 Despite best efforts during post-operative rehabilitation to overcome this muscle weakness, strength deficits often persist after formal treatment ceases37 and thus remain a concern at the time patients are cleared to return to sport/activity.
Symmetrical quadriceps strength, defined as equivalent strength between the injured and non-injured sides, should be a rehabilitation goal as greater limb asymmetry following ACL reconstruction (ACLr) is predictive of patients who do not pass return to sport criteria11 and is related to poor self-reported function, functional performance41, and altered lower extremity mechanics during gait.11 Possibly of even bigger concern is that persistent quadriceps muscle weakness following ACLr is related to the life-long consequence of early onset post-traumatic osteoarthritis.36, 48 Given the deleterious effects of quadriceps weakness, it seems crucial to maximize quadriceps strength to preserve knee joint health and functional ability.
A myriad of guidelines have been utilized to define what clinical criterion value should be deemed “adequate” quadriceps symmetry following ACLr, with many suggesting between limb differences should not be more than 10%1, 19 while others have defined deficits upwards of 20% to be acceptable.8, 23, 43 Before clinical recommendations can be made as to an appropriate threshold for quadriceps strength symmetry a better understanding of how the magnitude of quadriceps strength asymmetry influences factors such as biomechanics and performance (e.g. factors related to poor outcomes following ACLr) are needed. Clear clinical guidelines will assist sports medicine professionals in making evidence-based decisions regarding return to sport/activity following ACLr.
Therefore, the primary purpose of this study was to determine if quadriceps strength asymmetry influences knee joint biomechanics and functional performance, as well as self-reported function. It was our hypothesis that those with the highest quadriceps indices would have more symmetrical sagittal plane hip and knee biomechanics as compared to those with moderate and low quadriceps strength symmetry. Further, we hypothesized that the patients with the highest quadriceps indices would have the greatest self-reported function and functional performance than the weaker subjects at return to activity.
METHODS
Participants
Sixty-six patients participated in the study as part of an ongoing investigation examining quadriceps function after ACL reconstruction (Table 1). Patients were eligible for enrollment in the parent study if they: 1) were between 14–30 years of age, 2) were planning to undergo rehabilitation at our sports medicine clinic, 3) had an acute ACL injury (defined as reporting to a physician within 48 hours from injury), 4) had no previous knee surgeries, 5) suffered a previous ACL injury, 6) weren’t currently or planning to become pregnant, and/or 7) had a known heart condition. Patients were not enrolled consecutively. Patients were retrospectively included in the current investigation if they had quadriceps strength and biomechanical variables collected at the time they were cleared to return to activity (6 patients currently available in our study database did not have biomechanical data collected). Patients were excluded from this study if they: had an ACL reconstruction utilizing a graft type other than patellar tendon. The University’s institutional review board approved the study protocol and all participants provided written informed consent prior to testing.
Table 1.
Participant Demographics (mean±SD)
| High-Quadriceps (n=12) | Moderate-Quadriceps (n=12) | Low-Quadriceps (n=42) | |
|---|---|---|---|
| Sex | Female=4 | Female=4 | Female=17 |
| Age (yrs) | 19.3±6.3 | 21.58±7.49 | 21.09±5.05 |
| Height (m) | 1.73±0.08 | 1.74±0.10 | 1.75±0.12 |
| Mass (kg) | 73.0±14.88 | 71.19±11.64 | 76.78±14.17 |
| Time to Return to Activity (days) | 212.25±36.43 | 218.25±35.51 | 231.33±37.83 |
| Injured limb | Left=7 | Left=8 | Left=23 |
| Meniscectomy | 4 | 2 | 4 |
| Meniscal Repair | 1 | 4 | 12 |
| Collateral Ligament | 0 | 1 | 0 |
| Bone Bruise | 7 | 8 | 28 |
| Articular Cartilage | 0 | 1 | 2 |
| Mechanism of Injury | Contact=1 | Contact=5 | Contact=5 |
| Return to Competitive Sport | Yes=7 | Yes=12 | Yes=27 |
No significant differences in age, height, mass or time to return to activity across groups (P > 0.05).
Post-operative Rehabilitation and Return to Activity
All participants completed a standard postoperative rehabilitation regimen at a single clinic consisting of 2–3 visits per week beginning in the first post-operative week. The rehabilitation protocol emphasized full knee extension range of motion immediately and knee flexion as tolerated, progression of functional exercises, and quadriceps strengthening.
Testing for this study began once the orthopedic surgeon cleared participants for return to activity (Table 1). In addition to full range of motion and no effusion, return criteria at our clinic require patients to complete a three-week agility program and pass a leg press test. To successfully complete the leg press test, patients need to finish at least 15 repetitions of the exercise requiring the knee to be moved from neutral to 90 degrees of flexion with their affected limb at 100% of body weight. If either the leg press test was not passed or the agility program was not completed clearance for return to activity was postponed until criteria were satisfied.
Quadriceps Strength Measurements
Isokinetic quadriceps muscle strength was assessed bilaterally. Briefly, participants were secured in a dynamometer (Biodex System 3, Biodex Medical Systems, Shirley, NY, USA) with the knee and hip of the test limb flexed to 90°. Participants completed three maximum voluntary concentric knee extension contractions at 60°/sec with two minutes rest between each trial. Verbal encouragement and real-time visual feedback of the torque output were also provided. This procedure was completed for both legs with testing order being counterbalanced so as to minimize the potential of a learning effect. The trial with the largest peak torque in each limb was extracted and used to calculate the quadriceps index ([ACLr leg/uninjured leg] × 100). The quadriceps index (QI) was then utilized to place patients into groups. Participants with a QI ≥90 were placed in the HIGH group, those with was a QI < 90 but ≥80 were placed in the MOD Group and those with a QI < less than 80 were placed in the LOW Group. Strength asymmetries of 10% or less are commonly deemed acceptable for return to activity following ACLr30 and have been used as a cutoff value in similar studies27, 41 and thus a cutoff value of 90% was selected for our HIGH group. Strength asymmetries 20% or larger are considered abnormal and thus served as the cutoff for the LOW group.27, 40 As for the MOD group, we contend it is important to examine patients falling between the high and low criterion values as it has been suggested that strength indices above 80% can be considered adequate.23, 43 Understanding how the MOD patients compare to those considered to have high and low strength seems important as no universal criterion is followed when returning patients activity.
Quadriceps Activation
Quadriceps activation was measured utilizing the burst superimposition technique and quantified with the central activation ratio (CAR).44 Burst superimposition procedures require subjects to complete maximal voluntary isometric knee extension contractions (MVICs) and they completed these contractions until no improvement in torque was noted22. Subjects always completed a minimum of three MVICs. Once it was apparent that participants were no longer increasing torque between trials, an additional trial was initiated and participants were asked to maintain this contraction for approximately five seconds. A custom written program (LabVIEW version 8.5, National Instruments, Austin, TX, USA) was set to deliver a supramaximal stimulus (Grass S88 Dual Output Square Pulse Stimulator/SIU8T Stimulus Isolation Unit, Grass Technologies, West Warrick, RI, USA) to the quadriceps via two self-adhesive electrodes (Dura-Stick II [7×13 cm] Chattanooga Group, Hixson, TN, USA) that were placed over the vastus lateralis and the vastus medialis. The stimulus was delivered once the MVIC was reached and subsequently dropped by one Newton meter.44 Automated stimulus delivery was utilized because it has been shown to improve stimulus timing and thus reduce measurement error.21 The CAR was then calculated (CAR = (MVIC/MVIC+Superimposed burst)*100) and a value of 100 was used to represent complete quadriceps activation.20 The trial with the largest CAR (i.e. least amount of activation failure) was used for statistical analysis.
Single-Legged Landing Task
Three-dimensional biomechanical data were collected for the knee and hip during a single-legged landing task using a motion capture system (Vicon, Oxford Metrics, London, England) sampling at 240 Hz and synchronized with analog data sampling at 1200 Hz. The task required patients to perform a single-leg forward hop onto a force platform (OR 6–7; Advanced Medical Technology, Inc, Watertown, MA) with the ACL reconstructed limb. The distance to hop was determined by each participant’s leg length, defined as the tip of the greater trochanter to the tip of the lateral malleolus.49 Trials were collected until at least three successful trials were captured. A trial was considered successful when participants landed on the force platform and were able to balance on their take-off limb without touching the floor with the contralateral limb. Data were collected for both limbs, with the limb subjects were required to land on being counterbalanced.
Kinematic and Kinetic Data Processing
Lower limb joint rotations were defined based on three-dimensional coordinates of 32 retro-reflective markers (right and left limb; anterior and posterior superior iliac spines, iliac crest, greater trochanter, distal thigh, medial and lateral femoral epicondyles, tibial tuberosity, distal shank, lateral shank, medial and lateral malleoli, calcaneus, dorsal navicular, head of first and fifth metatarsal). A static trial of each participant aligned with the laboratory coordinate system was recorded allowing a kinematic model comprised of seven skeletal segments (bilateral foot, shank and thigh segments and the pelvis) and 24 degrees of freedom to be created (Visual3D v. 4, C-Motion; Rockville, MD).34 Marker trajectories recorded during each trial were subsequently processed within the respective subject’s Visual3D model to solve for the generalized coordinates of each frame. Rotations were calculated utilizing the Cardan rotation sequence 7 and were expressed relative to each subject’s neutral static position.31 Ground reaction force data was sampled and synchronized with the kinematic data and both were filtered using a fourth-order, zero-lag, low-pass Butterworth filter at 12 Hz cut-off frequency.35 Filtered kinematic and ground reaction force data were then submitted to a standard inverse dynamics approach within Visual3D.51 Segmental inertial properties were defined based on the previous work of Dempster.9 The intersegmental moments at the knee and hip joints were expressed as flexion-extension with respect to the Cardan axes of the local joint coordinate system.31, 33 Joint moments were normalized to subject body height and mass and expressed as external moments.
Biomechanical data were time normalized to 100% of the stance phase for graphical purposes, with initial contact equating to the time when the vertical ground reaction force first exceeded and fell below 10 N 4, 31 and the end of the landing equating to 250 msec post-initial contact.10 Ensemble averages were calculated across stance for all rotations and moments32, as this is when ACL injury is thought to occur.14 In order to assess symmetry of kinematics and kinetics between limbs, the peak angles and moments for the ACL reconstructed limb were normalized to the contralateral non-injured limb utilizing the limb symmetry index ((injured limb angle or moment/uninjured limb angle or moment) *100), with a value 100 reflecting perfect symmetry. Given that healthy individuals have been shown to display nearly identical between limb mechanics47, asymmetrical mechanics in our ACLr patients should reflect a difference that was a result of the injury/reconstruction and/or inadequate rehabilitation.
One-Legged Hop for Distance
We used a one-legged hop for distance as a clinical assessment of functional performance. To complete this task, subjects stood on their test leg and hopped forward as far as possible landing only on the same leg. The distance was quantified with a tape measure that was fixed to the ground and recorded to the nearest tenth of a centimeter. Patients were allowed to practice the hop until they felt comfortable and/or until no improvement was seen in the hop distance and then was asked to complete 3 successful trials. A limb symmetry index (distance of involved limb/distance of uninvolved limb * 100) was calculated and used in statistical analysis.3 Participants completed this task for both the affected and healthy limbs and testing order was counterbalanced. Intra-rater reliability of this test has been shown to be high in patients who have undergone ACL reconstruction.2, 15, 16
International Knee Documentation Committee (IKDC) Form
Self-reported knee function was quantified using the IKDC subjective knee evaluation form. The form is scored on a scale of 0 to 100, with 100 representing highest knee function. The IKDC score has been shown to be a reliable and valid measure of function in persons following ACL injury.18
Statistical Analysis
One-way analyses of variances ANOVAs were ran to determine if the groups (HIGH, MOD, LOW) were different on demographic parameters such as age, height, mass and time to return to activity. Multivariate analysis of covariance was utilized to examine group differences for all dependent variables (QI, CAR, IKDC, and limb symmetry indices for the hop for distance, sagittal plane knee and hip angles and moments). Covariates included in the analysis were gender, meniscal status (e.g. whether or not meniscal repair or meniscectomy were performed), age, mass, and time to return to activity. Where appropriate, post hoc Bonferroni multiple comparison procedures were used. To examine the factors that would predict biomechanical symmetry for the knee and hip, hierarchical linear regressions were used to evaluate the influence of age, mass, gender, time to return to sport, meniscal status, and QI (independent variables) on knee flexion angles and moment symmetry indices (dependent variables). QI was entered into the model last so that we could ascertain the influence that QI had on our dependent measures above the influences of age, mass, gender, time to return to sport, and meniscal status. The alpha level was set a priori at P≤0.05. SPSS version 22 was used to perform all analyses.
RESULTS
Patient Demographics
No significant differences were identified between groups in terms of age (P = 0.66), height (P =0.95), mass (P=0.95), and/or time of return to activity (P = 0.09) (Table 1).
Quadriceps Strength and Activation
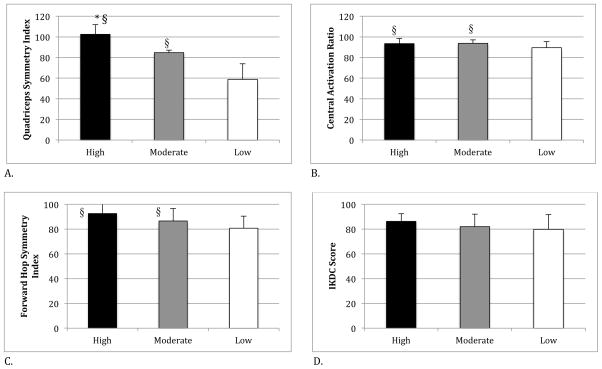
As expected, the quadriceps index (QI) differed among groups, with the HIGH group displaying the largest QI (102.48±9.31), the MOD group displaying the middle QI (84.71±2.44) and the LOW group displaying the smallest QI (58.80±15.02) (P=<0.0001) (Figure 1a). Further, there was a significant group difference identified for the CAR, with the LOW group displaying a smaller CAR (89.53±5.78) when compared with the HIGH (93.49±4.83) and MOD (93.77±3.31) groups (P=0.05) (Figure 1b).
FIGURE 1.
Quadriceps Index, Central Activation Ratio, Forward Hop Symmetry Index, and IKDC Score for High, Moderate, and Low Quadriceps Groups. * represents significantly different from moderate group. § represents significantly different from low group.
Hop for Distance and IKDC
No significant differences were noted between groups for the IKDC score (HIGH: 86.30±6.23; MOD: 82.07±10.03; LOW: 79.84±11.91) (P = 0.20) (Figure 1c). However, a statistically significant group difference was detected for the hop index with the LOW group displaying less symmetry between sides (80.75±9.65), compared with patients in the HIGH (92.62±9.00) or MOD (86.62±10.03) groups (P =.049) (Figure 1d).
Kinematics and Kinetics
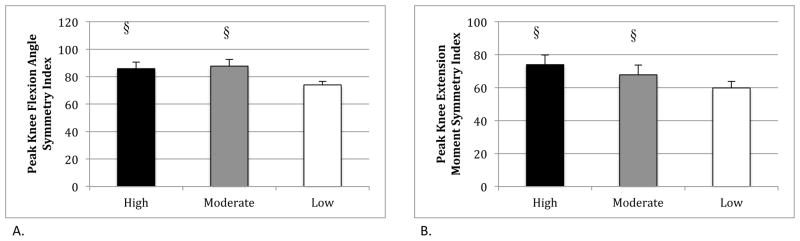
Statistically significant differences were noted for the peak knee flexion symmetry index (Figure 2a). The HIGH (LSI = 85.82±4.80) and MOD (LSI = 87.67±4.80) groups were not different in terms of knee flexion symmetry (P = 1.00), but were found to have statistically greater symmetry from those in the LOW group (LSI =73.95±2.56) (P< 0.05). Similar results were noted for the external knee flexion moment, wherein the HIGH (73.98±5.77) and MOD (67.79±5.82) groups had greater symmetry when compared to the LOW group (59.79±4.06) (P < 0.05), but no differences were noted between the HIGH and MOD (P =0.86).
FIGURE 2.
Symmetry indices for knee flexion angles and moments for high, moderate, and low quadriceps groups. * represents significantly different from moderate group. § represents significantly different from low group.
Regression Analyses
Meniscal status, mass, and time to return to activity were not found to be significant predictors of biomechanical symmetry for peak knee flexion angle (P > 0.05), while age (P = 0.013) and gender (P = 0.049) did influence values. After controlling for all these variables in the model however, the QI was a significant predictor for knee flexion angle symmetry (R2 change = 0.285). With regards to knee flexion moment symmetry, only age (P = 0.042) and QI (P = 0.008) were significant predictors (R2 change = .250 for QI). Lastly, only QI was a predictor of hop symmetry (R2 change = 0.251) (P < 0.002).
DISCUSSION
The goal of the current work was to examine whether quadriceps strength asymmetry influenced functional performance and knee and hip biomechanics at the time patients were cleared to return to activity following ACLr. The data partially supported our initial hypotheses in that patients with LOW quadriceps symmetry performed worse on hop testing and landed with less peak knee flexion angle symmetry and external knee flexion moment symmetry than patients with HIGH and MOD quadriceps symmetry. In contrast, no differences in knee flexion angle or extension moment limb symmetry were detected between the HIGH and MOD quadriceps strength groups. The asymmetrical knee flexion angles and moments demonstrated by the LOW group during the single-legged landing are consistent with the literature. Xergia et al52 noted that men 6 to 9 months post ACL reconstruction with a bone patellar tendon bone autograft demonstrated lower knee flexion angles in the injured limb compared to the non-injured limb during hopping. While the relationship between quadriceps strength and biomechanics was not established in this study52, the isokinetic quadriceps indices calculated from their data revealed values less than 80%, supporting the premise that residual quadriceps weakness in the ACLr limb likely contributed to the reduced knee flexion angles that were observed. Lewek et al27 reported that patients with weak quadriceps, defined as a QI less than 80%, walked and jogged with lower flexion angles and moments than those with high isometric quadriceps strength (i.e. QI > 90%) following ACLr with a semitendinosus/gracilis autograft or allograft. Likewise, Di Stasi11 and colleagues noted that ACL patients reconstructed with a semitendinosus/gracilis autograft or allograft not passing return to play criteria, which included having an isometric quadriceps index below 90%, had less symmetrical knee flexion angles and moments than patients passing return criteria. We contend the asymmetry noted in our work and that of others suggest that at return to play patients often do not have adequate eccentric quadriceps strength and/or control to resume normal knee mechanics during functional activity. The reduced knee flexion in the reconstructed limb or a stiffening strategy in an attempt to control body weight upon landing may also be problematic as these alterations in movement are thought to contribute to the early onset post-traumatic osteoarthritis associated with ACL injury. Chaudhari et al6 proposed that altered knee motion following ACL injury or reconstruction could load cartilage in unfamiliar ways and perpetuate cartilage degradation. Following this proposed framework it is indeed possible that the altered mechanics noted in our study population could have serious consequences for the long-term health of the affected knee joint. Therefore, it seems critical that rehabilitation post-ACLr aims to achieve quadriceps symmetry thereby leading to more symmetrical movement patterns in the sagittal plane.
While the LOW group displayed less knee flexion angle and moment symmetry than the HIGH and MOD groups, there was no difference in symmetry when comparing the HIGH to the MOD groups. While quadriceps symmetry of 90% is recommended as a clinical criterion for return to activity following ACLr,30 the empirical evidence supporting that 90% is necessary to achieve acceptable symmetry in joint mechanics and functional performance is sparse. Current trends in ACL rehabilitation promote using objective return to activity guidelines, rather than the subjective criteria of time post-surgery, which has been classically used as a marker for patient clearance. As such, it is critical that the objective data put forth are backed with strong experiential support as to why the criterion were chosen. While biomechanical symmetry is not the only factor rehabilitation professionals are aiming to achieve, it could be critical for long-term joint health6 and prevention of re-injury38 and thus should be considered. In the current study, it appears that an 80–89% QI was equivalent to a 90–100% QI in terms of elucidating biomechanical symmetry. While neither group had complete symmetry, they were not statistically or clinically different from each other suggesting that at least in terms of sagittal plane knee symmetry a QI of 80% may lead to similar biomechanical outcomes. The design of our study however, is not adequate to delineate a specific criterion value and thus future research should focus on establishing evidence-based criteria. Furthermore, the N for the High and Mod groups is rather small and thus the lack of significant difference between these groups could be due to inadequate statistical power. It is also important to discuss that factors other than quadriceps strength, such as fear of re-injury, joint range of motion, core muscle and other lower extremity strength, are likely important in achieving movement symmetry following ACLr and these factors should be established and considered when developing return to activity guidelines. This contention is supported by our study in that quadriceps strength only accounted for a small part of the variance in knee flexion angle and moment symmetry (R2 change =25% for both variables).
Hop distance symmetry was worse in patients in the LOW group compared to those in the MOD and HIGH groups. In a similar study, Schmitt et al41 noted patients with lower quadriceps strength, having a QI < 85%, had greater asymmetry in hop distance for the single and triple hop tests when compared to patients with higher quadriceps strength, QI > 90%, at the time they returned to sport. Further, similar to our results, they note the QI was significantly associated with hop performance, albeit that both studies revealed modest R2 values (0.14 for Schmit and .25 for the current study). Other studies39, 50 have revealed correlations ranging from 0.3 to 0.7 for quadriceps strength and hop symmetry, but due to methodological differences direct comparisons between our work and theirs is difficult. There is no doubt that additional factors also contribute to hop symmetry such as fear of re-injury, effusion, knee pain, and lower extremity range of motion, among others and require consideration in future studies.
The HIGH and MOD groups had higher scores on the IKDC when compared to the LOW group, although this did not reach statistical significance (P = 0.20). Similar results were seen by Schmitt et al41 with a trend towards differences between groups with higher and lower quadriceps strength. We believe failure to reach statistical significance is due to a lack of statistical power rather than there being no true differences between groups. Many studies5, 12, 24, 28, 42, 50 have revealed that quadriceps strength influences self-reported knee function though the strength of the relationship has varied.
Patients in the LOW group displayed lower CAR values, suggestive of increased quadriceps muscle inhibition, when compared to the MOD or HIGH groups. The larger magnitude of inhibition in the LOW group may have contributed to the lower overall strength values in this group. Muscle inhibition prevents complete voluntary activation of the quadriceps. As such, if higher levels of inhibition were noted prior to reconstruction or soon after reconstruction among our LOW group this may have prevented patients from activating their musculature to the same degree as patients in the MOD or HIGH groups thereby impeding rehabilitation. Hurley et al17 showed an inverse relationship between muscle inhibition and quadriceps strength and also revealed that larger magnitudes of inhibition have the ability to negatively influence strength gains through rehabilitation after traumatic knee injuries. We did not quantify the CAR prior to or soon after reconstruction so we are unable to determine if patients in the LOW group did indeed have greater amounts of inhibition than the HIGH or MOD groups and thus cannot be certain this was the case in our subject population.
In our sample, only ~20% of patients (13 of 66) were able to achieve 90% quadriceps strength symmetry between limbs. Ninety percent symmetry in quadriceps (and hamstring) strength was recently identified by a consensus as a measure important for achieving successful outcome following ACLr.30 As such, our patients may be primarily viewed as unsuccessful when this criterion is considered. Our patients undergo standardized rehabilitation25 similar to what would be seen in most outpatient rehabilitation clinics, with 2–3 visits per week and where quadriceps strengthening is emphasized. Despite this, symmetrical muscle strength is still not achieved and is rather poor with an average QI in our sample (across all 3 groups) 71.25 ± 21.8. This reinforces that standard rehabilitation and clearance around the time of 6–7 months is not adequate to generate a successful outcome post ACLr. Rehabilitation programs including high-intensity neuromuscular electrical stimulation and perturbation training along with aggressive quadriceps strengthening have been proven successful in restoring limb symmetries and should strongly be considered for inclusion in post-operative rehabilitation.29, 45, 46 Further, eccentric exercise has been shown to improve quadriceps strength compared to standard of care or electrical stimulation.13, 26 Six weeks of eccentric exercise in addition to standard of care has been able to more effectively restore quadriceps strength at time of return to activity.26 Therefore, alternative methods to achieve maximal quadriceps strength, such as those mentioned above need to become the standard rather than the exception when it comes to ACL rehabilitation.
CONCLUSION
Isokinetic quadriceps strength deficits following ACL reconstruction negatively influence sagittal plane knee movement symmetry and functional performance. Specifically, patients with QIs < 80% had smaller knee flexion angles and moments in the involved compared to the uninvolved sides. Furthermore, quadriceps strength was shown to be associated with hop performance and sagittal plane knee symmetry accounting for a significant portion of the variance. Rehabilitation programs following ACL reconstruction need to focus on restoring symmetrical quadriceps strength prior to clearing patients to return to activity.
What is known about this subject
Quadriceps strength is diminished following ACL injury and reconstruction. Joint biomechanics and functional performance are also negatively affected by ACL trauma.
What this study adds to existing knowledge
This study utilized common cited clinical criterion values for acceptable quadriceps strength symmetry (i.e. 80% and 90%) to determine if movement symmetries are restored in patients with greater quadriceps strength. It was found that individuals that return to activity with greater quadriceps strength indices post-ACL reconstruction were capable of performing a dynamic movement task with greater limb symmetry than those with lower quadriceps strength indices. This data is important, as it is a first step in identifying the magnitude of quadriceps strength that affects limb asymmetry post-ACL reconstruction, and provides clinicians with information related with the magnitude of quadriceps strength symmetry at return to activity that leads to more symmetrical knee mechanics.
Acknowledgments
The authors would like to thank Nicole Stortini and Meagan Strickland for their assistance with data collection and processing. Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under Award Number K08 AR05315201A2 to Dr. Palmieri-Smith. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Adams D, Logerstedt DS, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42(7):601–614. doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andersson C, Odensten M, Gillquist J. Knee function after surgical or nonsurgical treatment of acute rupture of the anterior cruciate ligament: a randomized study with a long-term follow-up period. Clin Orthop Relat Res. 1991;(264):255–263. [PubMed] [Google Scholar]
- 3.Barber SD, Noyes FR, Mangine RE, McCloskey JW, Hartman W. Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clin Orthop Relat Res. 1990;(255):204–214. [PubMed] [Google Scholar]
- 4.Borotikar BS, Newcomer R, Koppes R, McLean SG. Combined effects of fatigue and decision making on female lower limb landing postures: central and peripheral contributions to ACL injury risk. Clinical Biomechanics. 2008;23(1):81–92. doi: 10.1016/j.clinbiomech.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 5.Bryant AL, Kelly J, Hohmann E. Neuromuscular adaptations and correlates of knee functionality following ACL reconstruction. J Orthop Res. 2008;26(1):126–135. doi: 10.1002/jor.20472. [DOI] [PubMed] [Google Scholar]
- 6.Chaudhari AM, Briant PL, Bevill SL, Koo S, Andriacchi TP. Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc. 2008;40(2):215–222. doi: 10.1249/mss.0b013e31815cbb0e. [DOI] [PubMed] [Google Scholar]
- 7.Cole GK, Nigg BM, Ronsky JL, Yeadon MR. Application of the joint coordinate system to three-dimensional joint attitude and movement representation: a standardization proposal. J Biomech Eng. 1993;115(4A):344–349. doi: 10.1115/1.2895496. [DOI] [PubMed] [Google Scholar]
- 8.Daniel DM, Malcolm L, Stone ML, Perth H, Morgan J, Riehl B. Quantification of knee instability and function. Contemp Orthop. 1982;5:83–91. [Google Scholar]
- 9.Dempster WT, Gabel WC, Felts WJL. The anthropometry of the manual work space for the seated subject. American journal of physical anthropology. 1959;17(4):289–317. doi: 10.1002/ajpa.1330170405. [DOI] [PubMed] [Google Scholar]
- 10.Deneweth JM, Bey MJ, McLean SG, Lock TR, Kolowich PA, Tashman S. Tibiofemoral joint kinematics of the anterior cruciate ligament-reconstructed knee during a single-legged hop landing. The American journal of sports medicine. 2010;38(9):1820–1828. doi: 10.1177/0363546510365531. [DOI] [PubMed] [Google Scholar]
- 11.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310–1318. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eitzen I, Risberg MA, Holm I. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009 doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 13.Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, Lastayo PC. Safety, feasibility, and efficacy of negative work exercise via eccentric muscle activity following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2007;37(1):10–18. doi: 10.2519/jospt.2007.2362. [DOI] [PubMed] [Google Scholar]
- 14.Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries. The American journal of sports medicine. 2006;34(9):1512. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 15.Harner CD, Marks PH, Fu FH, Irrgang JJ, Silby MB, Mengato R. Anterior cruciate ligament reconstruction: endoscopic versus two-incision technique. Arthroscopy. 1994;10(5):502–512. doi: 10.1016/s0749-8063(05)80004-0. [DOI] [PubMed] [Google Scholar]
- 16.Howell SM, Deutsch ML. Comparison of endoscopic and two-incision techniques for reconstructing a torn anterior cruciate ligament using hamstring tendons. Arthroscopy. 1999;15(6):594–606. doi: 10.1053/ar.1999.v15.015059. [DOI] [PubMed] [Google Scholar]
- 17.Hurley MV, Jones DW, Newham DJ. Arthrogenic quadriceps inhibition and rehabilitation of patients with extensive traumatic knee injuries. Clin Sci (Colch) 1994;86(3):305–310. doi: 10.1042/cs0860305. [DOI] [PubMed] [Google Scholar]
- 18.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 19.Keays SL, Bullock-Saxton J, Newcombe P, Keays AC. The relationship between knee strength and fucntional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21:231–237. doi: 10.1016/S0736-0266(02)00160-2. [DOI] [PubMed] [Google Scholar]
- 20.Kent-Braun JA, Le Blanc R. Quantitation of central activation failure during maximal voluntary contractions in humans. Muscle Nerve. 1996;19(7):861–869. doi: 10.1002/(SICI)1097-4598(199607)19:7<861::AID-MUS8>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 21.Krishnan C, Allen EJ, Williams GN. Torque-based triggering improves stimulus timing precision in activation tests. Muscle & nerve. 2009;40(1):130–133. doi: 10.1002/mus.21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krishnan C, Williams GN. Factors explaining chronic knee extensor strength deficits after ACL reconstruction. Journal of Orthopaedic Research. 2011;29(5):633–640. doi: 10.1002/jor.21316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JH, Bae DK, Song SJ, Cho SM, Yoon KH. Comparison of clinical results and second-look arthroscopy findings after arthroscopic anterior cruciate ligament reconstruction using 3 different types of grafts. Arthroscopy. 2010;26(1):41–49. doi: 10.1016/j.arthro.2009.06.026. [DOI] [PubMed] [Google Scholar]
- 24.Lentz TA, Tillman SM, Indelicato PA, Moser MW, George SZ, Chmielewski TL. Factors associated with function after anterior cruciate ligament reconstruction. Sports Health. 2009;1(1):47–53. doi: 10.1177/1941738108326700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lepley LK, Wojtys EM, Palmieri-Smith RM. Does concomitant meniscectomy or meniscal repair affect the recovery of quadriceps function post-ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2014 doi: 10.1007/s00167-014-3093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lepley LK, Wojtys EM, Palmieri-Smith RM. Combination of eccentric exercise and neuromuscular electrical stimulationto improve quadriceps function post-ACL reconstruction. Knee. doi: 10.1016/j.knee.2014.11.013. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewek MD, Rudolph KS, Axe MJ, Snyder-Mackler L. The effect of insufficeint quadriceps strength after anterior cruciate ligament reconstruction. Clin Biomech. 2002;17:56–63. doi: 10.1016/s0268-0033(01)00097-3. [DOI] [PubMed] [Google Scholar]
- 28.Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Pre-operative quadriceps strength predicts IKDC2000 scores 6 months after anterior cruciate ligament reconstruction. Knee. 2013;20(3):208–212. doi: 10.1016/j.knee.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):859–868. doi: 10.1007/s00167-012-1929-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lynch AD, Logerstedt DS, Grindem H, et al. Consensus criteria for defining ‘successful outcome’ after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2013 doi: 10.1136/bjsports-2013-092299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McLean SG, Felin RE, Suedekum N, Calabrese G, Passerallo A, Joy S. Impact of fatigue on gender-based high-risk landing strategies. Med Sci Sports Exerc. 2007;39(3):502–514. doi: 10.1249/mss.0b013e3180d47f0. [DOI] [PubMed] [Google Scholar]
- 32.McLean SG, Huang X, Su A, Van Den Bogert AJ. Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. Clin Biomech (Bristol, Avon) 2004;19(8):828–838. doi: 10.1016/j.clinbiomech.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 33.McLean SG, Huang X, Van Den Bogert AJ. Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury. Clin Biomech (Bristol, Avon) 2005;20:863–870. doi: 10.1016/j.clinbiomech.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 34.McLean SG, Lipfert SW, Van Den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Medicine & Science in Sports & Exercise. 2004;36(6):1008. doi: 10.1249/01.mss.0000128180.51443.83. [DOI] [PubMed] [Google Scholar]
- 35.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in ”high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:39. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palmieri-Smith RM, Thomas AC. A Neuromuscular mechanism of posttraumatic osteoarthritis associated with ACL injury. Exerc Sport Sci Rev. 2009;37(3):147–153. doi: 10.1097/JES.0b013e3181aa6669. [DOI] [PubMed] [Google Scholar]
- 37.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27(3):405–424. vii–ix. doi: 10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 38.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Risberg MA, Holm I, Ekeland A. Reliability of functional knee tests in normal athletes. Scand J Med Sci Sports. 1995;5(1):24–28. doi: 10.1111/j.1600-0838.1995.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 40.Sapega AA. Muscle performance evaluation in orthopaedic practice. J Bone Joint Surg Am. 1990;72(10):1562–1574. [PubMed] [Google Scholar]
- 41.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Seto JL, Orofino AS, Morrissey MC, Medeiros JM, Mason WJ. Assessment of quadriceps/hamstring strength, knee ligament stability, functional and sports activity levels five years after anterior cruciate ligament reconstruction. Am J Sports Med. 1988;16:170–180. doi: 10.1177/036354658801600215. [DOI] [PubMed] [Google Scholar]
- 43.Shelbourne KD, Foulk DA. Timing of surgery in acute anterior cruciate ligament tears on the return of quadriceps muscle strength after reconstruction using an autogenous patellar tendon graft. Am J Sports Med. 1995;23(6):686–689. doi: 10.1177/036354659502300609. [DOI] [PubMed] [Google Scholar]
- 44.Snyder-Mackler L, De Luca PF, Williams PR, Eastlack ME, Bartolozzi AR., 3rd Reflex inhibition of the quadriceps femoris muscle after injury or reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1994;76(4):555–560. doi: 10.2106/00004623-199404000-00010. [DOI] [PubMed] [Google Scholar]
- 45.Snyder-Mackler L, Delitto A, Bailey SL, Stralka S. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1995;77(8):1167–1173. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Snyder-Mackler L, Delitto A, Stralka S, Balley SL. Use of electrical stimulation to enhance recovery of quadriceps femoris muscle force production in patients following anterior cruciate ligament reconstruction. Phys Ther. 1994;74(10):901–907. doi: 10.1093/ptj/74.10.901. [DOI] [PubMed] [Google Scholar]
- 47.Teichtahl AJ, Wluka AE, Morris ME, Davis SR, Cicuttini FM. The associations between the dominant and nondominant peak external knee adductor moments during gait in healthy subjects: evidence for symmetry. Archives of physical medicine and rehabilitation. 2009;90(2):320–324. doi: 10.1016/j.apmr.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 48.Tourville TW, Jarrell KM, Naud S, Slauterbeck JR, Johnson RJ, Beynnon BD. Relationship between isokinetic strength and tibiofemoral joint space width changes after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(2):302–311. doi: 10.1177/0363546513510672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Webster KE, Gonzalez AR, Feller JA. Dynamic joint loading following hamstring and patellar tendon anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12(1):15–21. doi: 10.1007/s00167-003-0400-9. [DOI] [PubMed] [Google Scholar]
- 50.Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20(2):60–73. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]
- 51.Willson JD, Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clinical Biomechanics. 2008;23(2):203–211. doi: 10.1016/j.clinbiomech.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 52.Xergia SA, Pappas E, Zampeli F, Georgiou S, Georgoulis AD. Asymmetries in functional hop tests, lower extremity kinematics, and isokinetic strength persist 6 to 9 months following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2013;43(3):154–162. doi: 10.2519/jospt.2013.3967. [DOI] [PubMed] [Google Scholar]