Abstract
Background
The aim of this study was to evaluate pediatric oncology providers’ attitudes toward fertility preservation (FP), their use of educational materials, their approach to FP discussion, and their FP knowledge specifically pertaining to adolescent males.
Methods
A 40-item online survey was distributed to physicians, advanced practice nurses (APN), and nurses within pediatric oncology.
Results
About 78.7% of physicians, 81.4% of APN, and 51.9% of nurses reported high levels of comfort in discussing FP options with adolescent males (P<0.05). Fifty-one percent of physicians and 54.2% of APN reported using educational materials, compared with 38.9% of nurses (P<0.05). Regarding knowledge of FP technologies, 48.7% of physicians, 52.5% of APN, and 81.1% of nurses reported being unfamiliar with intracytoplasmic sperm injection (P<0.05). An overwhelming majority (92.9%) of respondents reported having no formal training in discussing FP. Finally, 84.8% of respondents believed formal training on this issue would be useful to them.
Conclusions
This study illustrates an unmet need in the education of pediatric oncology providers, as knowledge gaps and discomfort are common themes reported by health care professionals within the context of adolescent male FP care. In addition, this study reveals a high level of receptiveness to FP training by these same providers.
Keywords: adolescent, cancer, fertility, fertility preservation, health care providers, pediatrics
Infertility is a primary concern of adult survivors of childhood cancer.1 Initially in 2006, and subsequently in 2013, the American Society of Clinical Oncology (ASCO) recommended that providers inform patients that cancer treatments can compromise fertility.2,3 Similarly, the National Comprehensive Cancer Network guidelines published in 2012 and updated in 2014, stated that fertility preservation (FP) should be an essential part of the oncology management of adolescent and young adults who are at risk of infertility due to cancer treatment.4,5 In 2014, the Association of Pediatric Hematology/Oncology Nurses (APHON) published a review of the evidence on various FP modalities and made recommendations on utilization of these methods. 6 All these above-mentioned recommendations/guidelines highlight the importance of FP discussions before cancer treatment and call for the referral of oncology patients to fertility specialists at the earliest possible time. Still, it is apparent that FP counseling and care have not reached a large proportion of the adolescent population who may benefit from these services.7 Survivors of pediatric cancer have reported never hearing about FP or even the risk of infertility following potentially sterilizing treatment.8 Moreover, there continues to be a paucity of educational material available to adolescent patients regarding the potential threat of cancer treatments to their fertility.9
There are a variety of FP approaches that can be used in the adolescent and adult oncology population that are age, disease, and treatment targeted. For adolescent males who have already entered puberty, the best-established method of preserving fertility is through cryopreservation of ejaculated sperm. Cryopreserved sperm can be used later in life for intrauterine insemination or in vitro fertilization with or without intracytoplasmic sperm injection (ICSI). Fortunately for most males, the process of providing sperm for cryopreservation is effective, inexpensive, and non-invasive, as most adolescent males are able to provide ejaculated semen. For prepubertal males, the options are limited to experimental techniques. Prepubertal testicular tissue banking under an IRB-approved protocol is currently available at several institutions.10
Numerous studies have shown that oncology providers inconsistently refer adolescent males and females for FP consultations before the onset of cancer treatment. In 1 study, 80% of physicians agreed that the threats to fertility are a major concern for them when dealing with adolescent male oncology patients, but only 2/3 of these providers routinely referred patients to a fertility specialist before cancer treatment.11 Known barriers to FP in adolescent patients include financial constraints, fear of delaying treatment, and a patient’s poor prognosis.12 In addition to these constraints, the lack of pediatric oncology provider comfort in discussing FP strategies, and limited access to educational materials and FP services can hamper delivery of care.12–14
The aim of this study was to evaluate pediatric oncology providers’ attitudes toward FP, their use of educational materials, their approach to FP discussion, and their FP knowledge specifically pertaining to adolescent males. We hypothesized that these providers often lack the requisite comfort, knowledge, and access to educational resources needed for effective counseling of adolescent male cancer patients.
MATERIALS AND METHODS
Survey Instrument
We created a survey template by first identifying 4 main content domains: FP practice behaviors, use of educational materials, approach to FP discussion, and FP knowledge. Keywords in the literature search included “cancer FP,” “adolescent sperm cryopreservation,” “FP discussion,” and “FP patient education.” Survey items were organized within the framework of these 4 domains, and reviewed by content experts, including a urologist, a pediatric oncologist, an advanced practice nurse (APN) in pediatric oncology, and a health services researcher with expertise in patient education and the topic area. The final survey contained 27 items relevant to the 4 content domains. Content domains included patient population demographics, FP knowledge, FP practice behaviors, and provider demographics. There were an additional 13 items pertaining to the providers’ demographic information. The survey was approved by the institutional review board at our institution before circulation.
A survey announcement was emailed to individual members registered to a database of US-based pediatric oncology providers, including physicians, APNs, and nurses. We chose these primary disciplines in an effort to reach the greatest number of individuals who work directly with adolescent oncology patients at the time of a cancer diagnosis. The email contained a brief explanation of the survey and a link to the survey site (http://www.survey-monkey.com). A follow-up email reminding recipients to complete the survey was sent 3 weeks later; the online survey was closed 5 weeks after the initial notification. We were blinded to the identities of individual respondents for the extent of the study.
Analysis
All data were coded by a single member of the research team, and analyzed by a staff statistician using SPSS.
RESULTS
Response Rate
In total, 3257 individuals were contacted through email and invited to complete the survey. A total of 326 individuals responded to the survey, yielding a response rate of 10%. Approximately 48% of respondents were physicians, 18% were APN, 17% were nurses, and the remaining 17% did not specify a highest level of training. The majority reported working primarily in an academic medical center (60.4%), whereas the remainder reported working in either community medical centers or in private practice (Table 1).
TABLE 1.
Demographics
| Demographics | No. Respondents | Respondents (%) |
|---|---|---|
| Total (N) | 326 | |
| Profession | ||
| Physician | 157 | 48.2 |
| Nurse practitioner | 59 | 18.1 |
| Nurse | 54 | 16.6 |
| Unknown | 56 | 17.2 |
| Practice setting | ||
| Academic medical center | 197 | 60.4 |
| Community medical center | 51 | 15.6 |
| Private practice | 16 | 4.9 |
| Other | 6 | 1.8 |
| Unknown | 56 | 17.2 |
Approach to FP Discussion
Of those surveyed, 93.6% of physicians report discussing the impact of cancer treatment on the future fertility of their adolescent male patients “usually” or “always” (76% to 100% of the time). Of APNs and nurses, 74.6% and 48.2%, respectively, reported discussing threats to fertility with this same frequency. In response to the survey item “How comfortable are you discussing FP with your adolescent male patients”: physicians and APNs reported high levels of comfort with FP discussions (somewhat or entirely comfortable), 78.7% and 81.4%, respectively. In comparison, only 51.9% of nurses reported being somewhat or entirely comfortable with FP discussions (Table 2). The difference between physician and nurse groups in both of these comparisons were found to be statistically significant (P<0.05).
TABLE 2.
Provider Responses to Survey Item: “How Comfortable are You Discussing Fertility Preservation With Your Adolescent Male Patients”
| Entirely Uncomfortable (%) | Somewhat Uncomfortable (%) | Neutral (%) | Somewhat Comfortable (%) | Entirely Comfortable (%) | |
|---|---|---|---|---|---|
| Physician (N=155) | 4.5 | 7.7 | 9.2 | 29.7 | 49.0 |
| Nurse practitioner (N=59) | 6.8 | 3.4 | 8.5 | 37.3 | 44.1 |
| Nurse (N=54) | 5.6 | 24.1 | 18.5 | 27.8 | 24.1 |
Educational Materials
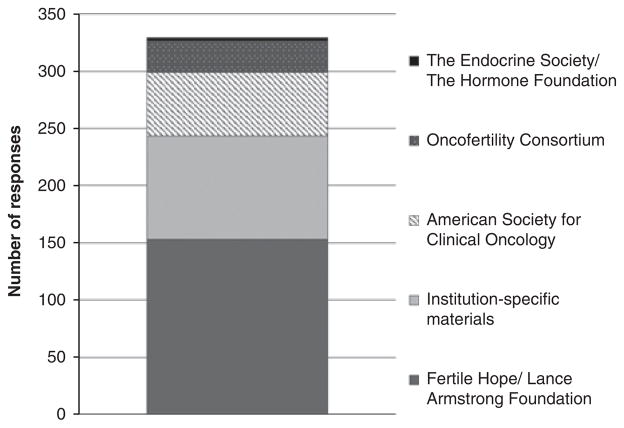
In assessing provider utilization of existing educational materials about FP in adolescent male patients, 51% of physicians and 54.2% of APNs reported using educational materials “usually” or “always,” compared with 38.9% of nurses (P<0.05, Table 3). Providers were subsequently queried about the specific educational materials they used in practice: the majority of providers endorsed using printed materials, with the next greatest proportion reported using Internet site referrals. These resources were most commonly published by Fertile Hope, ASCO, the Oncofertility Consortium, or were specific to a provider’s home institution (Fig. 1).
TABLE 3.
Provider Responses to Survey Item: “I Provide My Pubertal (Approximately 13–18 y Old) Male Patients and Their Families With Educational Material About Fertility Preservation”
| N (%)
|
||||||
|---|---|---|---|---|---|---|
| Never (0% of the Time) | Rarely (1%–25% of the Time) | Sometimes (26%–50% of the Time) | Often (51%–75% of the Time) | Usually (76%–99% of the Time) | Always (100% of the Time) | |
| Physician (N=155) | 6 (3.9) | 14 (9.0) | 28 (18.1) | 28 (18.1) | 41 (26.5) | 38 (24.5) |
| Nurse practitioner (N=59) | 3 (5.1) | 6 (10.2) | 6 (10.2) | 12 (20.3) | 22 (37.3) | 10 (16.9) |
| Nurse (N=54) | 9 (16.7) | 16 (29.6) | 6 (11.1) | 2 (3.7) | 11 (20.4) | 10 (18.5) |
FIGURE 1.
Sources of fertility preservation educational materials that providers distribute to adolescent male patients and their families (N = 330).
An additional survey component asked providers to comment on the limitations of existing educational materials, and how these resources can be improved. About 1/3 of participants responded to this question. Among them, 49% stated that adult content, adult language, and overall reading level was a shortcoming of existing educational material.
Provider Knowledge of FP Guidelines and Technologies
When asked about exposure to and familiarity with the 2006 ASCO recommendations on FP, 26% of physicians reported being “unfamiliar” with these recommendations, compared with 35.6% of APNs and 64.8% of nurses (Table 4). All professions reported low familiarity with ICSI, a standard technique in reproductive endocrinology that allows for the use of an individual sperm for in vitro fertilization. About 48.7% physicians reported being unfamiliar with this technique, compared with 52.5% of APNs and 81.1% of nurses (P<0.05, Table 4).
TABLE 4.
Provider Responses to Survey Items Assessing Fertility Preservation Knowledge
| N (%)
|
|||
|---|---|---|---|
| Very Familiar | Somewhat Familiar | Unfamiliar | |
| Are you familiar with the American Society of Clinical Oncology (ASCO) recommendations on fertility preservation? | |||
| Physician | 19 (12.3) | 95 (61.7) | 40 (26.0) |
| Nurse practitioner | 11 (18.6) | 27 (45.8) | 21 (35.6) |
| Nurse | 2 (3.7) | 17 (31.5) | 35 (64.8) |
| Are you familiar with the process of intracytoplasmic sperm injection (ICSI)? | |||
| Physician | 20 (13.0) | 59 (38.3) | 75 (48.7) |
| Nurse practitioner | 11 (18.6) | 17 (28.8) | 31 (52.5) |
| Nurse | 0 | 10 (18.6) | 43 (81.1) |
| Are you familiar with current fertility preservation research? | |||
| Physician | 19 (12.3) | 84 (54.2) | 52 (33.5) |
| Nurse practitioner | 6 (10.2) | 36 (61.0) | 17 (28.8) |
| Nurse | 1 (1.9) | 21 (38.9) | 32 (59.3) |
A subsequent survey item asked providers to report whether they received any formal training regarding FP in adolescent oncology patients. About 92.9% of providers received no formal training on this issue. However, 84.4% of all providers reported that formal training on FP would be useful to them (Table 5).
TABLE 5.
Provider Responses to Survey Item
| “Do You Have any Formal Training on Discussing Fertility Preservation?”
|
“Do You Think That Formal Training on the Issue of Fertility Preservation Would be Useful to You?”
|
||||
|---|---|---|---|---|---|
| Yes (N [%]) | No (N [%]) | Yes (N [%]) | No (N [%]) | ||
| Physician (N=155) | 10 (6.5) | 145 (93.5) | Physician (N=150) | 122 (81.3) | 28 (18.7) |
| Nurse practitioner (N=58) | 5 (8.6) | 53 (91.4) | Nurse practitioner (N=59) | 49 (83.1) | 10 (16.9) |
| Nurse (N=54) | 4 (7.4) | 50 (92.6) | Nurse (N=53) | 50 (94.3) | 3 (5.7) |
| Total (N=267) | 19 (7.1) | 248 (92.9) | Total (N=262) | 221 (84.4) | 41 (15.6) |
DISCUSSION
In accord with the recommendations from the American Academy of Pediatrics,15 the results of our study indicate that physicians and APNs involved in the care of adolescent male oncology patients often discuss FP options with their adolescent patients. Likewise, surveys in the literature support a high rate of FP discussions among pediatric oncologists. A 2014 Dutch study by Overbeek et al16 reported that 97% of the 37 pediatric oncologists surveyed discussed fertility issues with patients before treatment. Similarly, in a 2014 European survey, Terenziani and colleagues demonstrated that 64 of 68 pediatric oncology programs offer pretreatment fertility counseling. In the majority of cases, physicians were responsible for providing this counseling and roughly 1/3 of sites reported utilizing a team approach to pretreatment fertility counseling. 17 These studies are consistent with our findings, with 93.6% of physicians reporting that they discuss the impact of cancer treatment on future fertility with their adolescent male patients.
Our study also found that pediatric oncology nurses participate in FP discussions much less frequently than pediatric oncology APNs and physicians. Clayton et al18 found that 80% to 90% of nurses agree they should discuss FP with oncology patients. In addition, prior studies show that both physicians and patients recognize that ongoing contact between patients and nurses early in the course of an individual’s oncology care represents an excellent opportunity for discussing FP.19,20 Unfortunately, in a survey of 2 separate cohorts of pediatric oncology nurses, Vadaparampil et al21 found that only 50% of nurses and APNs were routinely discussing threats to fertility with pediatric cancer patients. By comparison, our data indicate that 75% of APNs and 50% of nurses are routinely having FP discussions with adolescent male patients. The higher observed frequency of FP discussions among APNs may reflect a growing awareness of FP care in the field of pediatric oncology when compared with the afore-mentioned 2007 study. The nonparalleled increase in FP discussions by APN compared with nurses echoes our findings in which nurses report being less comfortable with FP discussion and less familiar with published FP recommendations and techniques than the physician and APN respondents. This disparity suggests that there might be a paucity of targeted educational programs and resources available to nurses in the field of pediatric oncology to enable them to effectively and comfortably counsel adolescents about FP. In addition, there may be a lack of awareness among nursing professionals regarding the APHON recommendations and existing educational materials.
According to the 2006 and 2013 ASCO recommendations, providers are encouraged to provide written materials concerning FP; however, pediatric oncology providers inconsistently use educational materials to facilitate FP discussions. Our data show that only 50% of all providers surveyed use educational materials in their discussions with adolescent male patients “usually” or “always.” The most common resources that survey participants endorsed using are provided by Fertile Hope (http://www.livestrong.org), ASCO (http://www.asco.org), and the Oncofertility Consortium (http://oncofertility.northwestern.edu). An additional survey component asked providers to comment on the limitations of existing educational materials, and how these resources can be improved. The comments expressed indicate that many providers believe existing educational materials are missing age-appropriate language and subject matter required to make them useful in discussions with adolescents, particularly younger adolescents. From these comments, we can deduce that there continues to be a paucity of materials and/or a lack of awareness of these materials that effectively facilitate FP discussions between providers, adolescent patients, and their families.
It is also well known that adolescents have a strong desire to actively participate in discussions related to FP in the context of cancer treatments.22 Educational materials that cater to different age groups and diagnoses can play a key role in involving adolescents in FP discussions. Murphy et al23 used a small focus group–based study to determine the preferences of survivors of pediatric cancer and their parents regarding design and content of educational materials on FP. Interviews with 7 survivors (ages 12 to 21) of pediatric cancer and their parents demonstrated mixed impressions of the FP-centered educational materials they reviewed. Many parents felt that the language was overly technical for a young audience, whereas many of the adolescents expressed they understood the content. Although this study was the first of its kind to examine patient responses to educational materials specifically for adolescent oncology patients, the results are limited by a small sample size. Quantitative analyses of FP utilization trends over time among adolescent patients will be useful in determining whether updated educational resources are truly effective in reducing existing barriers to FP care in this group.
Importantly, in our study, a significant proportion of all survey respondents reported low familiarity with FP recommendations, procedures, and research. While over 90% of physicians indicate commonly discussing FP with their patients before treatment, the vast majority (92%) of all providers have had no formal training on the topic of FP. Nurses demonstrated the least familiarity with ASCO recommendations, the process of ICSI, and current FP research. A large proportion of physicians and APNs surveyed were also unfamiliar with these elements of FP care in adolescents, as nearly 50% of all physicians and APNs reported being “unfamiliar” with ICSI.
It is important that providers who are counseling patients about FP have some understanding of the process by which cryopreserved sperm can be used in the future to achieve a pregnancy. Encouragingly, a large proportion of the health care providers in our study expressed an interest in receiving formal training in FP. Creating formal training programs and educational modules is a logical next step in preparing pediatric oncology providers to effectively counsel adolescent male patients about FP options before undergoing cancer treatment.
There are a few limitations of this study that should be addressed. The first limitation is this survey was not a validated questionnaire. It is also important to note that the response rate to this survey was low; however, our results do mirror participation in similar published studies.24–27 Participation rate can be partially attributed to the nature of the survey. For one, response rates are highly dependent on having valid email addresses. Furthermore, we did not offer multiple repeat reminder emails nor did we offer compensation for participation, which have been shown in the past to significantly increase response rates to online surveys.28 Lastly, the broad-based nature of this mailing list likely includes a subset of people who do not actually engage in clinical work.
This survey may also suffer from participation bias, with respondents being more interested in FP than non-respondents. However, if this were the case, then our findings of low knowledge of FP and low usage of educational materials would represent underestimates of the problem. We did aim to seek a diverse, nationwide response, and thus the data are not subject to potential inherent biases related to geographic regions. In addition, despite the survey being anonymous, some degree of voluntary reporting bias likely occurred.
In conclusion, pediatric oncology providers are integral to the delivery of FP care, directing male patients to urologists for sperm cryopreservation before starting treatment. Our study suggests a need for formal training of pediatric oncology providers on the topic of FP to facilitate effective patient counseling and implementation of FP care. Nurses are often in an optimal position to have FP discussions with young patients and their families, but a high percentage of nurses have not been provided with the requisite tools and training to engage in these conversations. Furthermore, a high percentage of pediatric oncology providers, including physicians, APNs, and nurses, express willingness to participate in further FP training, indicating a future step toward diminishing existing barriers to FP care in the pediatric population.
Footnotes
The authors declare no conflict of interest.
References
- 1.Stevens MC, Mahler H, Parkes S. The health status of adult survivors of cancer in childhood. Eur J Cancer. 1998;34:694–698. doi: 10.1016/s0959-8049(98)00012-4. [DOI] [PubMed] [Google Scholar]
- 2.Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917–2931. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- 3.Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31:2500–2510. doi: 10.1200/JCO.2013.49.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levine J, Canada A, Stern CJ. Fertility preservation in adolescents and young adults with cancer. J Clin Oncol. 2010;28:4831–4841. doi: 10.1200/JCO.2009.22.8312. [DOI] [PubMed] [Google Scholar]
- 5.Coccia PF, Altman J, Bhatia S, et al. Adolescent and young adult oncology. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2012;10:1112–1150. doi: 10.6004/jnccn.2012.0117. [DOI] [PubMed] [Google Scholar]
- 6.Fernbach A, Lockart B, Armus CL, et al. Evidence-based recommendations for fertility preservation options for inclusion in treatment protocols for pediatric and adolescent patients diagnosed with cancer. J Pediatr Oncol Nurs. 2014;31:211–222. doi: 10.1177/1043454214532025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheth KR, Sharma V, Helfand BT, et al. Improved fertility preservation care for male patients with cancer after establishment of formalized oncofertility program. J Urol. 2012;187:979–986. doi: 10.1016/j.juro.2011.10.154. [DOI] [PubMed] [Google Scholar]
- 8.Schover LR. Patient attitudes toward fertility preservation. Pediatr Blood Cancer. 2009;53:281–284. doi: 10.1002/pbc.22001. [DOI] [PubMed] [Google Scholar]
- 9.Jeruss JS, Woodruff TK. Preservation of fertility in patients with cancer. N Engl J Med. 2009;360:902–911. doi: 10.1056/NEJMra0801454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trost LW, Brannigan RE. Oncofertility and the male cancer patient. Curr Treat Options Oncol. 2012;13:146–160. doi: 10.1007/s11864-012-0191-7. [DOI] [PubMed] [Google Scholar]
- 11.Kohler TS, Kondapalli LA, Shah A, et al. Results from the survey for preservation of adolescent reproduction (SPARE) study: gender disparity in delivery of fertility preservation message to adolescents with cancer. J Assist Reprod Genet. 2011;28:269–277. doi: 10.1007/s10815-010-9504-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vadaparampil S, Quinn G, King L, et al. Barriers to fertility preservation among pediatric oncologists. Patient Educ Couns. 2008;72:402–410. doi: 10.1016/j.pec.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 13.Ginsberg JP, Ogle SK, Tuchman LK, et al. Sperm banking for adolescent and young adult cancer patients: sperm quality, patient, and parent perspectives. Pediatr Blood Cancer. 2008;50:594–598. doi: 10.1002/pbc.21257. [DOI] [PubMed] [Google Scholar]
- 14.Burns KC, Boudreau C, Panepinto JA. Attitudes regarding fertility preservation in female adolescent cancer patients. J Pediatr Hematol Oncol. 2006;28:350–354. doi: 10.1097/00043426-200606000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Fallat ME, Hutter J. Preservation of fertility in pediatric and adolescent patients with cancer. Pediatrics. 2008;121:e1461–e1469. doi: 10.1542/peds.2008-0593. [DOI] [PubMed] [Google Scholar]
- 16.Overbeek A, van den Berg M, Louwe L, et al. Practice, attitude and knowledge of Dutch paediatric oncologists regarding female fertility. Neth J Med. 2014;72:264–270. [PubMed] [Google Scholar]
- 17.Terenziani M, Spinelli M, Jankovic M, et al. Practices of pediatric oncology and hematology providers regarding fertility issues: a European survey. Pediatr Blood Cancer. 2014;61:2054–2058. doi: 10.1002/pbc.25163. [DOI] [PubMed] [Google Scholar]
- 18.Clayton H, Quinn GP, Lee JH, et al. Trends in clinical practice and nurses’ attitudes about fertility preservation for pediatric patients with cancer. Oncol Nurs Forum. 2008;35:249–255. doi: 10.1188/08.ONF.249-255. [DOI] [PubMed] [Google Scholar]
- 19.Quinn GP, Vadaparampil ST, Gwede CK, et al. Discussion of fertility preservation with newly diagnosed patients: oncologists’ views. J Cancer Surviv. 2007;1:146–155. doi: 10.1007/s11764-007-0019-9. [DOI] [PubMed] [Google Scholar]
- 20.Leonard M, Hammelef K, Smith GD. Fertility considerations, counseling, and semen cryopreservation for males prior to the initiation of cancer therapy. Clin J Oncol Nurs. 2004;8:127, 131, 145. doi: 10.1188/04.CJON.127-131. [DOI] [PubMed] [Google Scholar]
- 21.Vadaparampil ST, Clayton H, Quinn GP, et al. Pediatric oncology nurses’ attitudes related to discussing fertility preservation with pediatric cancer patients and their families. J Pediatr Oncol Nurs. 2007;24:255–263. doi: 10.1177/1043454207303878. [DOI] [PubMed] [Google Scholar]
- 22.Quinn GP, Block RG, Clayman ML, et al. If you did not document it, it did not happen: rates of documentation of discussion of infertility risk in adolescent and young adult oncology patients’ medical records. J Oncol Pract. 2015;11:137–144. doi: 10.1200/JOP.2014.000786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murphy D, Sawczyn KK, Quinn GP. Using a patient-centered approach to develop a fertility preservation brochure for pediatric oncology patients: a pilot study. J Pediatr Adolesc Gynecol. 2012;25:114–121. doi: 10.1016/j.jpag.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 24.King JW, Davies MC, Roche N, et al. Fertility preservation in women undergoing treatment for breast cancer in the UK: a questionnaire study. Oncologist. 2012;17:910–916. doi: 10.1634/theoncologist.2012-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Forman EJ, Anders CK, Behera MA. A nationwide survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. Fertil Steril. 2010;94:1652–1656. doi: 10.1016/j.fertnstert.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 26.Adams E, Hill E, Watson E. Fertility preservation in cancer survivors: a national survey of oncologists’ current knowledge, practice and attitudes. Br J Cancer. 2013;108:1602–1615. doi: 10.1038/bjc.2013.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quinn GP, Vadaparampil ST, Lee JH, et al. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009;27:5952–5957. doi: 10.1200/JCO.2009.23.0250. [DOI] [PubMed] [Google Scholar]
- 28.Braithwaite D, Emery J, De Lusignan S, et al. Using the Internet to conduct surveys of health professionals: a valid alternative? Fam Pract. 2003;20:545–551. doi: 10.1093/fampra/cmg509. [DOI] [PubMed] [Google Scholar]