Abstract
Introduction
Orthognathic surgery involves making several osteotomies that lead to varying degrees of post-operative swelling. The use of KT may be beneficial for postoperative treatment after head and neck surgery, accelerating drainage of tissue reaction or haemorrhages. The goal of this study was to find out if the application of KT prevents or improves swelling, pain and trismus after orthognathic surgery, improving patients’ postoperative quality of life.
Materials and Methods
In this double-blinded, randomized, control trial, 24 patients in whom bimaxillary orthognathic surgery was indicated, were included. Before surgery each patient alternatively was randomly included in the study group (treated with K-Taping® and corticosteroid) or in the control group (treated with corticosteroid). In the present study a MakerBot® Digitizer 3D™ was used to assess accurate volume measurements. All swelling measurements were expressed as total 3-D area of the landmarks (cm2 ) in T0 pre-operative, T1 fourth day after surgery.
Results
The differences T0–T1 are highly significant (p < 0.01) between group 1 or study group (treated with K-taping®) and group 2 (control group).
Discussion
The use of KT appears promising, because it is simple to carry out, less traumatic, economical, can be performed everywhere in the world, free from side effects on the body. Even when swelling persists, KT gives patients the impression of a minor swelling detracting them from their pain and morbidity. Further studies have to be performed to find out if KT can reduce or replace the need for additional medications such as the use of steroids.
Keywords: Orthognathic surgery, Kinesiotape, Edema, Digitizer 3-D
Introduction
Orthognathic surgery involves making several osteotomies in order to reposition the jaw in the right position. Any osteotomy, which involves the reflection of a full thickness mucoperiosteal flap, leads to varying degrees of post-operative swelling. An extensive swelling can compromise the surgical outcome as well as patient recovery and the airway [1].
Several methods to control the immediate inflammatory response associated with head and neck surgery have been described and used, including the use of drugs such as analgesics [1–3], corticosteroids [3], antibiotics [4], and proteolytic enzymes [5], laser application [6], or physical therapeutic methods like cryotherapy [7] or manual lymph drainage (MLD) [8]. No single modality of management significantly prevents and/or significantly reduces the occurrence of swelling, pain and trismus without potential undesirable side effects. Therefore further techniques for a better pain, swelling and trismus control should be developed for patients who undergo orthognathic surgery.
After its introduction in the 1970s, kinesiologic tape (KT) has increasingly become popular in the treatment of sport injuries and a variety of other conditions. There are several claims to the effects of KT including supporting injured muscles and joints, relieving pain, and increasing blood and lymph flow in the injured area.
However, there is still little evidence to support these claims and much more research is necessary [9]. The use of KT in the management of lymphoedema is gaining popularity. The tape is similar in weight to the epidermis, and lifting the skin, KT improves the blood and lymph flow, removing congestions of lymphatic fluid or hematomas [10]. By providing space, fluids are encouraged to move from areas of higher pressure towards the area of lower pressure, guided by the tape to the desired direction of drainage [11, 12]. Using this technique may be beneficial for postoperative treatment after head and neck surgery, accelerating drainage of tissue reaction or hematomas.
Several methods have been developed to measure facial soft tissue thickness in cadavers and in live patients [2]. Traditionally, facial soft tissue measurements have been studied using the needle depth probing method [13]. Several imaging-based methods for measuring living facial soft-tissue thickness have been reported [14, 15].
In the present study a MakerBot® Digitizer 3D™ was used to assess accurate volume measurements.
The goal of this study was to find out if the application of KT prevents or improves swelling, pain and trismus after orthognathic surgery, improving patients’ postoperative quality of life.
Materials and Methods
Patients
In this double-blinded, randomized, control trial, 24 patients (study group: 12 patients, control group: 12 patients) in whom bimaxillary orthognathic surgery was indicated, were included.
Before surgery each patient alternatively was randomly included in the study group (treated with K-Taping® and corticosteroid) or in the control group (treated with corticosteroid).
This study was in accordance by the ethical standards and all participants signed an informed consent agreement.
Inclusion criteria were as follows: patients selected had no preexisting medical conditions or medications that would influence their ability to undergo surgery or alter their wound healing after surgery.
All cases were diagnosed as skeletal Class III including mandibular prognathism and/or maxillary retrognathism on the basis of a lateral cephalogram analysis and the patients underwent orthognathic surgery.
The study group consisted of two men (average age 18–37 years) and ten women (average age 19–31 years). Control group consisted of three men (average age 18–30 years) and nine women (average age 20–27 years).
Selection of Landmarks
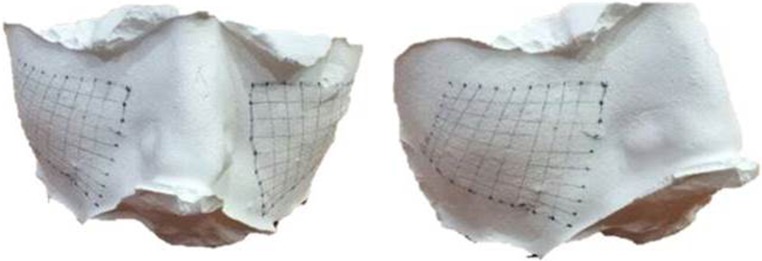
Bilaterally in each patient the area between four lines was selected (1) the line passing through the tragus of the ear and the ipsilateral labial commissure; (2) the line passing through 1 cm below the eyelid with the open eye and the tragus ipsilateral; (3) the line perpendicular to the Frankfurt plane and passing through the tail of the eyebrow; (4) the line passing through the medial canthus and the ipsilateral labial commissure (Fig. 1).
Fig. 1.
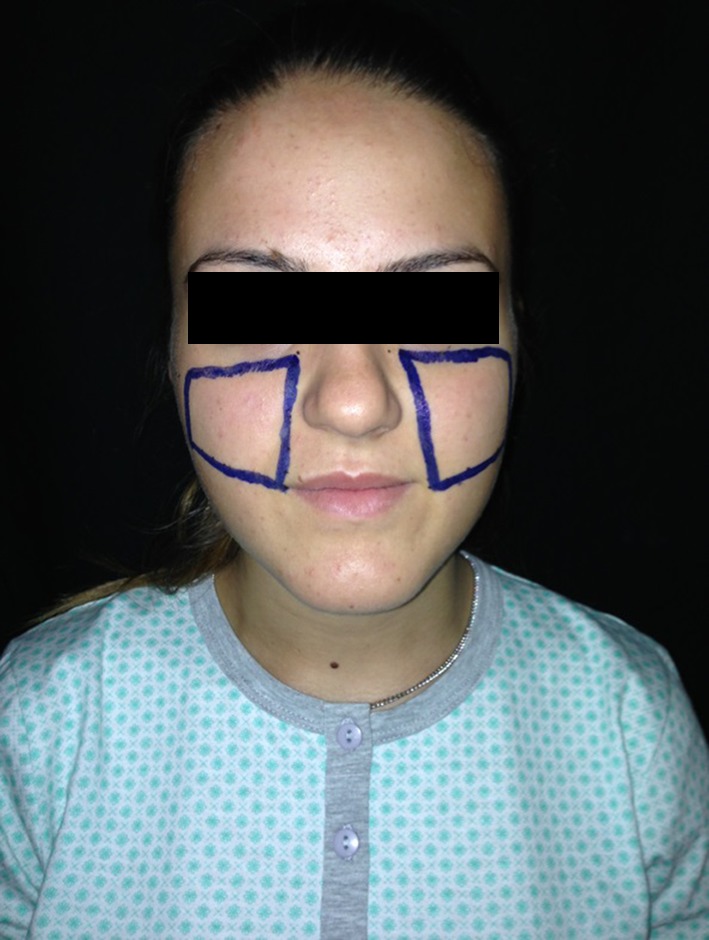
Area landmarks, frontal view
Taping
All taping procedures were performed by the same investigator—a certified K-Taping therapist. Skin was cleaned and freed of moisture and oils prior to application; if necessary the area was shaved. All tape applications were performed using skin coloured K-Active Tape Classic, 50 mm × 5 m (K-Active Europe GmbH, Wiesthal, Germany). Tape length was individually measured for every patient starting at the clavicle to the point of highest swelling. The tape was cut into three equal stripes (approximal 1.5 cm wide). Tape endings were rounded down. The tape was carefully removed from paper backing, trying to touch the adhesive as little as possible. The base was placed slightly above the lymph node area to which the drainage was being directed (supraclavicular nodes). The patient was moved into a stretch position.
Tails were placed on to the skin with slight tension (20 %). Placement of the lymphatic stripes was directed at the appropriate lymphatic duct crossing the cervical, sub mental, mandibular, submandibular, preauricular and parotid nodes, crossing the zygomatic arch, reaching the infraorbital rim and frontozygomatic suture surrounding the lower eye (Fig. 2). After application the tape was lightly rubbed to activate the medical grade acrylic adhesive.
Fig. 2.

Kinesiotape application
The tape was left for at least 5 days. Edges were trimmed if tape lifted before removal.
Measurements
Area: After the selection of landmarks with a marking pen a silicone mask with VynilPolysiloxane Impression Material Putty (Express STD Putty, 3 M ESPE, Pioltello, Milan—Italy) was made for the area of interest. The silicone mask did not distort or displace tissues because initially the mask is soft and lies on the area of interest and in a few minutes became quite dense. The silicone masks, once hardened, are semi-rigid, but they are still inextensible: this has led to feasible measurement, due to the fact that the evaluation of the regions was carried out not taking into account the volume, which can vary due to the fact that mask is not completely stiff, but taking into account the area, which remains constant due to the inextensibility of the mask. In this way the landmarks made with the marking pen are impressed on the silicon mask. The next step was to create a plaster cast conforming to the mask previously formed, like creating a dental impression. In the same way the landmarks made with the marking pen are impressed on the mold (Fig. 3). The mold was processed by the program Digitizer 3-D™ (MakerBot®) of Aerospace Engineering (S.U.N. University of Naples) for the precise measurement of the three-dimensional area (Fig. 4). It was only a transposition technique of the landmarks from the mold to the software, made by remarking the landmarks by a mechanical arm with a pen. This method is easily reproduced by others.
Fig. 3.
The mold of the area
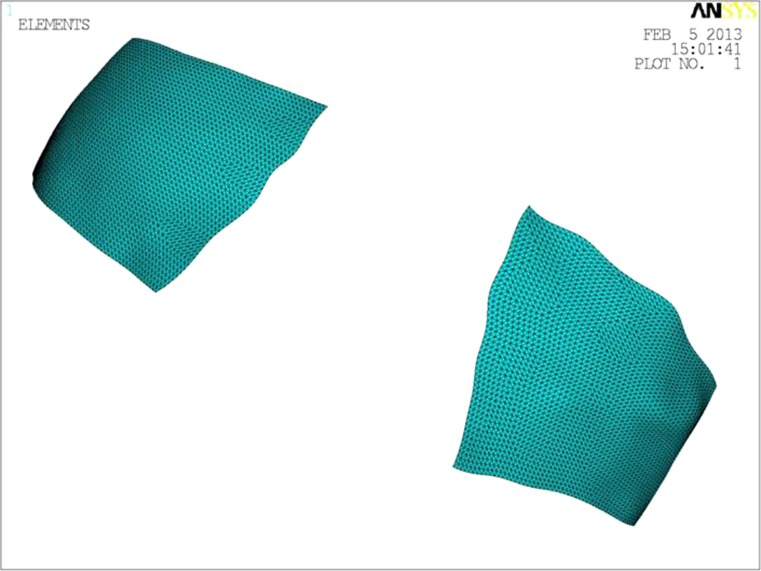
Fig. 4.
The mold processed by the program Digitizer 3-D™
Pain: Pain scores were assessed using a 10 level visual analogue scale (VAS) of 100 mm, representing all pain sensations from none to maximum; where zero indicates no pain, five moderate pain and ten worst pain possible. Patients were asked to place a mark along the line that corresponded to the amount of pain they were experiencing.
Trismus: Maximal mouth opening was recorded measuring the maximum inter-incisal distance using calipers.
All measurements were performed at two specific time points: T0 pre-operative, T1 4 days after surgery.
All measurements were recorded by a single operator (U.T.) and supervised by a single engineer (A.S.).
Surgical Technique
All patients underwent bimaxillary orthognathic surgery (Le Fort I osteotomy plus bilateral sagittal split osteotomy plus genioplasty). The duration of surgery and the cheek retraction time were recorded for all patients. As a part of the routine premedication protocol, 1 dose of dexamethasone 6 mg was injected in all patients 30 min before surgery. A dose of dexamethasone 4 mg was repeated after 3 and 6 h on the same day of surgery, dexamethasone 4 mg was repeated on the first day after surgery, dexamethasone 2 mg was repeated on the second day after surgery. No surgical drains were placed and ice packs were given to all patients.
Results
The data were analyzed and compared using the T Student test (Table 1).
Table 1.
Area measurements
| Group 1 (cm2)—study group | Group 2 (cm2)—control group | |||
|---|---|---|---|---|
| Right area | Left area | Right area | Left area | |
| Pt 1 pre | 20.22 | 22.43 | 23.60 | 23.46 |
| 4 day-post | 22.46 | 25.18 | 29.01 | 29.12 |
| Pt 2 pre | 18.00 | 18.50 | 17.80 | 16.93 |
| 4 day-post | 19.08 | 19.62 | 22.67 | 22.51 |
| Pt 3 pre | 23.09 | 22.50 | 16.30 | 17.12 |
| 4 day-post | 26.44 | 27.01 | 21.76 | 21.89 |
| Pt 4 pre | 21.90 | 19.82 | 19.41 | 19.28 |
| 4 day-post | 24.07 | 23.86 | 23.65 | 23.61 |
| Pt 5 pre | 20.76 | 21.55 | 24.12 | 23.89 |
| 4 day-post | 23.08 | 24.12 | 29.33 | 29.18 |
| Pt 6 pre | 25.02 | 24.81 | 21.78 | 22.14 |
| 4 day-post | 26.98 | 26.88 | 26.88 | 27.01 |
| Pt 7 pre | 17.89 | 18.33 | 16.15 | 16.77 |
| 4 day-post | 22.32 | 23.16 | 18.82 | 18.84 |
| Pt 8 pre | 16.67 | 16.52 | 16.72 | 17.04 |
| 4 day-post | 21.73 | 21.13 | 21.87 | 22.13 |
| Pt 9 pre | 19.58 | 19.36 | 21.82 | 21.53 |
| 4 day-post | 22.41 | 22.77 | 26.08 | 26.06 |
| Pt 10 pre | 21.76 | 20.53 | 23.71 | 24.02 |
| 4 day-post | 22.98 | 22.51 | 28.43 | 28.58 |
| Pt 11 pre | 21.30 | 20.78 | 16.44 | 16.12 |
| 4 day-post | 23.80 | 23.41 | 20.84 | 20.86 |
| Pt 12 pre | 20.82 | 19.89 | 18.30 | 17.91 |
| 4 day-post | 23.09 | 23.01 | 23.56 | 23.06 |
Area: All swelling measurements were expressed as total 3-D area of the landmarks (cm2) in T0 pre-operative, T1 fourth day after surgery. For each patient we compared, by adding left and right area, the increase of swelling between T1–T0. The differences had a Gaussian distribution. The differences T0–T1 are highly significant (p < 0.01) between group 1 or study group (treated with K-taping®) and group 2 (control group) (Table 2).
Table 2.
Statistical analysis
| Mean value | SD | p value | |||
|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 1 | Group 2 | ||
| Area T1–T0 | 5.7550 | 9.4475 | 2.2659 | 1.6701 |
p < 0.01 99 % |
In group 1 (study group) the mean value of the difference between the total/bilateral area 4 days after surgery (T1) and before surgery (T0) was 5.7550 cm2; in group 2 (control group) the mean value of the difference between the total/bilateral area 4 days after surgery (T1) and before surgery (T0) was 9.4475 cm2.
Pain: Comparing the study group and the control group results for pain scores assessed using a 10 level visual analogue scale (VAS) were not significant.
Trismus: Mouth opening values did not differ significantly in both groups.
Discussion
Postoperative swelling, pain and trismus are common events after orthognathic surgery affecting the social and working life of the patients [16].
There are many studies on the control of postoperative edema in maxillofacial surgery. In third molar surgery, the use of laser is a relatively new method for reducing postoperative discomfort, especially swelling [17]. It is believed that laser irradiation induces an increase in number and diameter of lymph vessels, with a simultaneous decrease of blood vessel permeability.
However, its use in maxilla-facial surgery has not been investigated yet. Ice therapy is a simple, cheap, repeatable modality. Its therapeutic effects are due to changes in blood flow, consequent vasoconstriction and reduced metabolism, therefore reducing bacterial growth. However, data concerning the effect of cryotherapy on swelling are controversial [7].
Unfortunately, comparison of published drug studies is difficult because of the variability in parameters and methods used for each study.
The use of steroids is common in oral and maxillofacial surgery [18]. However, except for the use of steroids after third molar extraction [19, 20], little has been published about potential benefits after orthognathic surgery.
The use of non-steroid anti-inflammatory drugs (NSAID) has been investigated with regard to reducing pain and inflammation.
In the current literature, it is apparent that the combination of another drug with an NSAID is often more effective in controlling postoperative pain and swelling in head and neck surgery than a NSAID alone [21].
With any medication helping to reduce postoperative side effects, adverse effects and serious complications may follow.
Emerging cases of drug allergies and drug-associated side effects are focussing more attention on alternative methods.
In an initial study, Szolonoky et al. investigated the efficacy of manual lymph drainage (MLD) after third molar extraction. Using reproducible facial measurement and a VAS pain scale, they demonstrated that MLD promoted an improvement of lymph circulation and worked in an adjunctive role for a significant reduction of postoperative swelling and pain [8].
Although KT has been increasingly used in the rehabilitation protocols and prevention of sport injuries, there is no clear evidence regarding potential mechanisms underlying the beneficial effects of KT. While promising anecdotal reports and case studies exist, there is a need for evidence-based studies with good methodological quality showing beneficial clinical effects [9]. KT has a potential influence on the reduction of swelling and haemorrhage.
Studies performed on the treatment of neoplastic or cancer related lymphoedema, have no evidence-based significance [10, 22].
Literature shows that the application of KT after orthognathic surgery has a significant influence on tissue reaction and swelling with an average cost for unilateral taping below one Euro per patient. The primary endpoint, increase of swelling, was significantly lower for the KT group than the no-KT group. Maximum swelling usually occurs 2nd to 3rd day after operation. However, using KT means peak swelling was reached after 0.5 days with significant lower values compared to the no-KT group. Furthermore, reduction of swelling was faster in the KT group compared to the no-KT group, decreasing the swelling by more than 60 % during the first 2 days after surgery [23]. This might be due to KT stretch capabilities, thickness and adhesion allowing approximating the quality of the skin. The material used for KT is an elastic cotton tape with a non-allergenic heat sensitive adhesive layer. KT has been designed to allow 30–40 % longitudinal stretch. By extending and rotating the muscles, the skin of the area to be treated is stretched. KT is then applied to the skin with a slight stretch. When the body parts return to their starting points the tape subsequently recoils back to its original length following the application. This creates a pulling force to the skin forming convolutions below the taped area. It is believed that these convolutions increase the interstitial space between the skin and underlying connective tissue, thus promoting the flow of blood and lymphatic fluid. In the head neck region, as performed in this study, changes in the length of tissue and the tape are extreme around a flexed, extended or rotated joint. Major convolutions could be recognized. As proposed by Shim et al. [24] in a pilot animal study these emerging wrinkles are not only indenting, but also elevating the skin. These investigators propose a positive effect on the formation of lymph by opening micro valves in the initial lymphatic vessels, therefore generating appropriate dynamic pressure variation and sufficient periodic compression and decompression of superficial and deep initial lymphatics.
According to some investigators KT facilitates the decrease of pain by pressure reduction on nociceptors [11, 12]. In this study no reduction of pain for the KT group compared to the no-KT group was demonstrated. Other studies performed are in agreement with these findings [25, 26]. The results of this study show patients scored moderate pain or less in both groups (VAS < 5) for all measurement times. This might be due to the standardized analgesic drug therapy protocol which both study groups received postoperatively and during their hospital admission. In order to make an evidenced statement, further investigation needs to be performed, eliminating the standardized analgesic and providing rescue drugs.
Using KT, patients mouth opening is similar to the no-KT group. These results are as seen in our subjective findings. Patients in the KT group had higher satisfaction after operation compared to the no-KT group. This might be because the swelling resolves faster, taking the tension from the skin. In addition, KT effect detracts from pain and perception.
Movement stresses KT, it only partially adjusts its length to that of the skin, and thus deforms the skin. This constant stimulus stimulates the skin and diverts patients’ recognition, but our study design was not designed to exclude possible placebo effects caused by the KT.
Although friction resulting from the elasticity of the tape could cause skin irritation and some adhesives might provoke allergies to some patients, we had no incidence of adverse reactions in our study, but these reactions should be considered for different types of tape. To the best of our knowledge, there are no reported cases of severe allergic reaction to KT application.
The assessment of facial volume reduction is one of the biggest obstacles for an objective and reliable demonstration of a used method. Numerous methods have been tried, most of which are imprecise, complex, expensive or difficult to standardize [13–15].
In the present study we used Digitizer 3-D™ under standardized conditions for the measurement of the area representative of the entire swelling. It is a simple, safe and accurate method. It is not widely available but we choose it for this study because this method is very accurate and we needed the precise measurement of the area.
Conclusion
The use of KT appears promising, because it is simple to carry out, less traumatic, economical, can be performed everywhere in the world, rare side effects (only allergy to adhesive). Even when swelling persists, KT gives patients the impression of a minor swelling detracting them from their pain and morbidity. Further studies have to be performed to find out if KT can reduce or replace the need for additional medications such as the use of steroids.
Acknowledgments
There was no financial support for this study by any company.
Conflict of interest
We declare that we have no conflicts of interest.
References
- 1.Kim K, Brar P, Jakubowski J, Kaltman S, Lopez E. The use of corticosteroids and nonsteroidal antiinflammatory medication for the management of pain and inflammation after third molar surgery: a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:630–640. doi: 10.1016/j.tripleo.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Aznar-Arasa L, Harutunian K, Figueiredo R, Valmaseda-Castellon E, Gay-Escoda C. Effect of preoperative ibuprofen on pain and swelling after lower third molar removal: a randomized controlled trial. Int J Oral Maxillofac Surg. 2012;41:1005–1009. doi: 10.1016/j.ijom.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 3.Thoren H, Snall J, Kormi E, Numminen L, Fah R, Iizuka T, et al. Does perioperative glucocorticosteroid treatment correlate with disturbance in surgical wound healing after treatment of facial fractures? A retrospective study. J Oral Maxillofac Surg. 2009;67:1884–1888. doi: 10.1016/j.joms.2009.04.089. [DOI] [PubMed] [Google Scholar]
- 4.Knepil GJ, Loukota RA. Outcomes of prophylactic antibiotics following surgery for zygomatic bone fractures. J Craniomaxillofac Surg. 2010;38:131–133. doi: 10.1016/j.jcms.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 5.Al-Khateeb TH, Nusair Y. Effect of the proteolytic enzyme serrapeptase on swelling, pain and trismus after surgical extraction of mandibular third molars. Int J Oral Maxillofac Surg. 2008;37:264–268. doi: 10.1016/j.ijom.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 6.Markovic A, Todorovic L. Effectiveness of dexamethasone and low-power laser in minimizing oedema after third molar surgery: a clinical trial. Int J Oral Maxillofac Surg. 2007;36:226–229. doi: 10.1016/j.ijom.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Rana M, Gellrich NC, von See C, Weiskopf C, Gerressen M, Ghassemi A, et al. 3D evaluation of postoperative swelling in treatment of bilateral mandibular fractures using 2 different cooling therapy methods: a randomized observer blind prospective study. J Craniomaxillofac Surg. 2013;41(1):17–23. doi: 10.1016/j.jcms.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Szolnoky G, Szendi-Horvath K, Seres L, Boda K, Kemeny L. Manual lymph drainage efficiently reduces postoperative facial swelling and discomfort after removal of impacted third molars. Lymphology. 2007;40:138–142. [PubMed] [Google Scholar]
- 9.Williams S, Whatman C, Hume PA, Sheerin K. Kinesio taping in treatment and prevention of sports injuries: a meta-analysis of the evidence for its effectiveness. Sports Med. 2012;42:153–164. doi: 10.2165/11594960-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 10.Chou YH, Li SH, Liao SF, Tang HW (2012) Case report: manual lymphatic drainage and kinesio taping in the secondary malignant breast cancer-related lymphedema in an arm with arteriovenous (A-V) fistula for hemodialysis. Am J Hosp Palliat Care, PMID: 22879520 [DOI] [PubMed]
- 11.Kase K, Hashimoto T, Tomoki O (1996) Development of kinesio taping perfect manual. Kinesio Taping Association
- 12.Kase K, Wallis J, Kase T. Clinical therapeutic applications of the kinesio taping method. 2. Tokyo: Ken Ikai Co., Ltd; 2003. [Google Scholar]
- 13.Bjorn H, Lundqvist C, Hjelmstrom P. A photogrammetric method of measuring the volume of facial swellings. J Dent Res. 1954;33:295–308. doi: 10.1177/00220345540330030201. [DOI] [PubMed] [Google Scholar]
- 14.Milles M, Desjardins PJ, Pawel HE. The facial plethysmograph: a new instrument to measure facial swelling volumetrically. J Oral Maxillofac Surg. 1985;43:346–352. doi: 10.1016/0278-2391(85)90255-1. [DOI] [PubMed] [Google Scholar]
- 15.Van Gool AV, Ten Bosch JJ, Boering G. A photographic method of assessing swelling following third molar removal. Int J Oral Surg. 1975;4:121–129. doi: 10.1016/S0300-9785(75)80004-4. [DOI] [PubMed] [Google Scholar]
- 16.Calderoni DR, Guidi Mde C, Kharmandayan P, Nunes PH. Seven-year institutional experience in the surgical treatment of orbito-zygomatic fractures. J Craniomaxillofac Surg. 2011;39:593–599. doi: 10.1016/j.jcms.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 17.Osunde OD, Adebola RA, Omeje UK. Management of inflammatory complications in third molar surgery: a review of the literature. Afr Health Sci. 2011;11:530–537. [PMC free article] [PubMed] [Google Scholar]
- 18.Assimes TL, Lessard ML. The use of perioperative corticosteroids in craniomaxillofacial surgery. Plast Reconstr Surg. 1999;103:313–321. doi: 10.1097/00006534-199901000-00050. [DOI] [PubMed] [Google Scholar]
- 19.Buyukkurt MC, Gungormus M, Kaya O. The effect of a single dose prednisolone with and without diclofenac on pain, trismus, and swelling after removal of mandibular third molars. J Oral Maxillofac Surg. 2006;64:1761–1766. doi: 10.1016/j.joms.2005.11.107. [DOI] [PubMed] [Google Scholar]
- 20.Grossi GB, Maiorana C, Garramone RA, Borgonovo A, Beretta M, Farronato D, et al. Effect of submucosal injection of dexamethasone on postoperative discomfort after third molar surgery: a prospective study. J Oral Maxillofac Surg. 2007;65:2218–2226. doi: 10.1016/j.joms.2006.11.036. [DOI] [PubMed] [Google Scholar]
- 21.Gassner R, Tuli T, Hachl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31:51–61. doi: 10.1016/S1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 22.Tsai HJ, Hung HC, Yang JL, Huang CS, Tsauo JY. Could kinesio tape replace the bandage in decongestive lymphatic therapy for breast-cancer-related lymphedema? A pilot study. Support Care Cancer. 2009;17:1353–1360. doi: 10.1007/s00520-009-0592-8. [DOI] [PubMed] [Google Scholar]
- 23.Ristow O, et al. Influence of kinesiologic tape on postoperative swelling, pain and trismus after zygomatico-orbital fractures. J Craniomaxillofacial Surg. 2013;42(5):469–476. doi: 10.1016/j.jcms.2013.05.043. [DOI] [PubMed] [Google Scholar]
- 24.Shim JY, Lee HR, Lee DC. The use of elastic adhesive tape to promote lymphatic flow in the rabbit hind leg. Yonsei Med. 1993;44:1045–1052. doi: 10.3349/ymj.2003.44.6.1045. [DOI] [PubMed] [Google Scholar]
- 25.Gonzalez-Iglesias J, Fernandez-de-Las-Penas C, Cleland JA, Huijbregts P, Del Rosario Gutierrez-Vega M. Short-term effects of cervical kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: a randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:515–521. doi: 10.2519/jospt.2009.3072. [DOI] [PubMed] [Google Scholar]
- 26.Thelen MD, Dauber JA, Stoneman PD. The clinical efficacy of kinesio tape for shoulder pain: a randomized, double-blinded, clinical trial. J Orthop Sports Phys Ther. 2008;38:389–395. doi: 10.2519/jospt.2008.2791. [DOI] [PubMed] [Google Scholar]