Abstract
Aims
We studied the utility of multimarker risk stratification approach to predict cardiovascular outcomes in patients with stable coronary artery disease, undergoing elective percutaneous coronary intervention (PCI).
Methods
We prospectively evaluated 302 consecutive patients with stable coronary artery disease and normal CPK-MB and cardiac troponin T levels, and who underwent elective PCI at our institution. The following cardiac biomarkers were measured before and between 12 and 24 h post-procedure: CK-MB, cardiac troponin T, hs-CRP, and NT-ProBNP. Patients were followed up for a minimum of 6 months.
Results
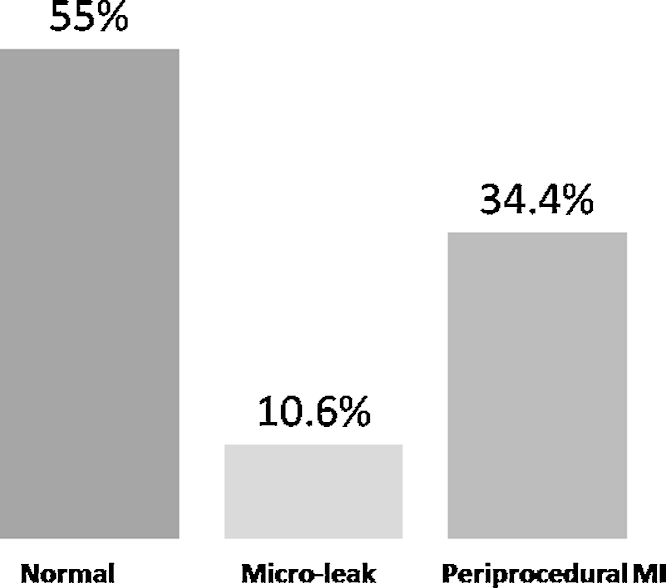
Post-PCI, CPK-MB levels were elevated but below myocardial infarction (MI) range in 70 patients (23%), and in the MI range in 6 patients (2%). Troponin T levels were detectable but below the 99th percentile (microleak) in 32 patients (10.6%) and elevated above the 99th percentile (periprocedural MI) in 104 patients (34.4%). At 9 months’ follow-up, 1% died, 2% had stable angina, 10.3% had non-fatal MI, and 87.7% remained asymptomatic. There was no significant difference in clinical events among groups stratified by elevation of one biomarker or multiple biomarkers.
Conclusion
Single or multiple biomarker strategy in patients with normal baseline biomarkers failed to predict major cardiac events after PCI over medium-term follow-up.
Keywords: Biomarkers, Percutaneous coronary intervention, Periprocedural myocardial infarction, Major adverse cardiovascular event
1. Introduction
Myocardial damage after percutaneous coronary intervention (PCI) can result from procedural complications such as distal embolization, side-branch occlusion, coronary dissection, or disruption of collateral flow. The incidence of myocardial damage after PCI, based on significant elevation of cardiac biomarkers, is 1–30%.1 Some of these episodes of periprocedural myocardial damage occur silently after uneventful PCI procedures. Although there is a consensus that troponin is probably the most relevant biomarker, the prognostic impact of troponin elevation after PCI is still debated.2, 3, 4 The universal definition of myocardial infarction (MI) arbitrarily includes ‘PCI-related MI’ as patients with normal baseline troponin levels and a rise of troponin three times the 99th percentile of the upper reference limit (URL).3 Cardiac troponins T (cTnT) and I (cTnI) are highly sensitive and specific markers of myocardial cell injury and necrosis. The prognostic value of troponins is now well established for patients presenting with acute coronary syndromes (ACS).4, 5, 6 Elevation of troponin following routine PCI has also been found to be predictive of both short- and long-term major adverse cardiovascular events (MACE).7, 8 However, there are conflicting reports on the value of cTn in the setting of PCI in stable and unstable coronary disease.9 Further, while the increasing sensitivity of cTn assays lowers the number of missed ACS diagnoses, it presents a diagnostic challenge because the gains in diagnostic sensitivity have inevitably come with a decrease in specificity.10
There is growing evidence that combining a biomarker of hemodynamic stress, such as B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP), and of inflammation, such as high-sensitivity C-reactive protein (hs-CRP), with a biomarker of necrosis (cardiac troponin) enhances risk assessment in patients with ACS.11, 12, 13, 14 Specifically, elevated levels of CRP and BNP at presentation identify patients who are at higher mortality risk, irrespective of whether or not there is detectable elevation of troponin.15, 16
The present study evaluated the clinical impact of a multimarker risk stratification approach on cardiovascular outcomes in patients with stable coronary artery disease undergoing elective PCI. This study also evaluated the impact of micro-cTn leak on long-term outcomes following elective PCI.
2. Methods
We prospectively evaluated patients with stable coronary artery disease undergoing elective PCI at G.B. Pant Hospital, New Delhi, India from June 2010 to May 2011. To ensure that any post-procedural increase in cardiac markers was exclusively PCI-related, we only included patients with stable coronary disease or previously stabilized unstable coronary disease with normal cardiac markers before PCI. Inclusion criteria were (1) patients with troponin/creatine kinase MB (CK-MB) values that were assessed pre-PCI and 12–24 h post-PCI, and where pre-procedure values were within the normal range, and (2) patients with stable coronary artery disease. Exclusion criteria were (1) patients with cardiac biomarker elevation (Tn or CK-MB) immediately before PCI, (2) patients with ACS, and (3) patients with significant renal, hepatic, or any other systemic dysfunction.
Institutional ethical guidelines were followed. All patients were included after informed consent. All patients were evaluated after a detailed history, physical examination, and appropriate investigations. Demographic and clinical characteristics of patients were documented. Blood samples were collected at baseline and at 8–12 h and 18–24 h after the procedure, and were analyzed in a core biochemistry laboratory.
All patients were pre-treated with oral aspirin and clopidogrel 2–6 h prior to the procedure in accordance with the established protocol. All PCI procedures were performed using femoral access. Oral aspirin and clopidogrel were recommended post-PCI for at least 1 year. All patients undergoing PCI were given 70 IU/kg unfractionated heparin before PCI, while the use of glycoprotein IIb/IIIa inhibitor and coronary stent type (bare-metal or drug-eluting stent) was at the operator's discretion.
Patients with >70% stenosis of only 1 epicardial coronary artery vessel were classified as single-vessel disease and those with >70% stenosis of >1 epicardial coronary artery were classified as multivessel disease. Coronary artery lesions were classified qualitatively according to modified American College of Cardiology/American Heart Association (ACC/AHA) classification into type A, B, or C; types A and B1 lesions were categorized as simple, while types B2 and C were categorized as complex lesions. For each procedure, the duration and pressure of balloon inflation, number, and type of stents were recorded. Any complications occurring during or within the first 24 h of PCI were also recorded.
Angiographic success was defined as residual coronary artery stenosis <50% after balloon angioplasty or <20% after stent implantation, with normal TIMI 3 coronary flow. To rule out Q-wave MI during the procedure, a 12-lead electrocardiogram (ECG) was performed before and at 24 h post-procedure. Additional ECGs were obtained in patients with post-procedural chest pain.
Pre-PCI blood samples were taken to analyze baseline myocardial damage marker values. Four cardiac markers, namely CK-MB, cTnT, hs-CRP, and NT-proBNP, were measured before and between 12 and 24 h post-procedure. cTnT was determined using the electro-chemiluminescence analyzer. cTnT elevation was taken as >3 times laboratory's upper limit for normal (normal, <0.1 ng/ml, following the universal definition of AMI). The lower detectable ranges for serum NT-proBNP and cTnT were 5 pg/ml and 0.01 ng/ml, respectively. CK-MB elevation was taken as 3 times our laboratory's upper limit for normal (normal, <25 U/L). Lower detectable range for CK-MB was 3 U/L.
Plasma and serum samples were collected into aliquots and stored. cTnT and NT-proBNP levels were determined in serum samples taken at admission, 12, and 24 h, using the one-step enzyme immunoassay based on electro-chemoluminescence immunoassay by Roche Elecsys, modular Cobas 2010 e 411 (Mannheim, Germany) using commercially available kits. CK-MB measurements were done by the principle of immunoinhibition by commercially available kits by RANDOX Laboratories Ltd., Antrim, United Kingdom on AU 400 autoanalyser by Beckman Coulter, CA, USA. Serum CRP was quantified by commercially available enzyme linked immune sorbent assay (ELISA) using commercially available kit by DCB, Canada (CAN-CRP-4360). Results were compared with standard curves and the lower detection limit was 0.01 μg/ml.
Patients were divided into 3 groups based on post-PCI serum cTnT levels: group 1 where cTnT was non-detectable; group 2 with microleak of cTnT (detectable but below the 99th percentile), and group 3 with elevated cTnT above the 99th percentile suggesting myocardial necrosis. Patients were followed up for at least 6 months by outpatient clinic attendance, telephonic contact, and review of the medical notes. Pre-defined endpoints were cardiovascular death, recurrent ACS, non-elective revascularization, and/or admission for acute heart failure. When events occurred during follow-up, we reviewed clinical records to obtain additional information. MACE was defined as a composite of death from any cause, MI, and the need for repeat revascularization (new PCI or coronary revascularization surgery).
Data analysis was performed using IBM SPSS Statistics 20.0 (IBM Corp., Armonk, NY). The frequency of abnormal results were determined for each marker and compared by the Fisher's exact test. Continuous variables were expressed as mean ± SD and were compared by the ANOVA test. Results with a p value <0.05 were considered statistically significant.
3. Results
Of the 512 consecutive patients screened for the study from June 2010 to May 2011, 302 patients were found eligible for this study. Table 1 shows the baseline demographic characteristics of the study patients. Table 2 shows the angiographic and procedural details of the patients.
Table 1.
Demographics and baseline patient characteristics.
| Parameter | Value (n = 302) |
|---|---|
| Age (mean ± SD) (years) | 53.8 ± 10.4 |
| Male | 293 (97%) |
| Hypertension (%) | 97 (32%) |
| Smoking (%) | 63 (21%) |
| Diabetes mellitus (%) | 66 (22%) |
| Recent MI (%) | 100 (33%) |
| Unstable angina (%) | 74 (25%) |
| Chronic stable angina (%) | 117 (39%) |
| Left ventricular ejection fraction (mean ± SD) (%) | 50 ± 10.3 |
| Previous PCI (%) | 24 (8%) |
| Prior CABG (%) | 3 (1%) |
| Prior MI (%) | 35 (12%) |
MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft surgery.
Table 2.
Angiographic and procedural characteristics.
| Characteristic | Value (n = 302) |
|---|---|
| Target vessel (%) | |
| Left anterior descending artery | 67.5 |
| Right coronary artery | 46.5 |
| Left circumflex artery | 40 |
| Lesion complexity (%) | |
| A | 54.9 |
| B | 33.8 |
| C | 11.8 |
| Multivessel PCI (%) | 22 |
| Stent length (mean ± SD) (mm) | 29.4 ± 14.3 |
| Mean stent diameter (mm) | 3.1 |
| Mean number of stents/patient | 1.2 |
| Drug eluting stent use | 283 (94%) |
| Longest inflation duration (s) | 33.4 ± 9 |
| Mean total no. of inflations | 11.6 |
PCI, percutaneous coronary intervention.
All patients had normal CPK-MB and cTnT levels pre-PCI as per protocol. Mean pre-PCI CPK-MB, cTnT, NT-proBNP, and CRP levels were 18.4 U/L, 0.01 ng/ml, 175.1 pg/ml, and 2.3 μg/ml, respectively. Mean post-PCI levels of these biomarkers were 30.1 U/L, 0.41 ng/ml, 311.3 pg/ml, and 2.8 μg/ml, respectively. Six (2%) patients had post-PCI CPK-MB levels in the MI range (>100 U/L). Elevated post-PCI CPK-MB levels but below MI range (35–100 U/L) were observed in 70 patients (23%). There was no significant difference in age, clinical presentation, vessel involvement, lesion type, or number of vessels stented between both groups. At follow-up, there was no significant difference in clinical events between both groups.
Of the 302 patients, post-PCI cTnT level was normal (<0.01 ng/ml) in 166 patients (55%), detectable but below the 99th percentile (0.01–0.03 ng/ml – microleak) in 32 patients (10.6%), and elevated cTnT above the 99th percentile (>0.03 ng/ml, MI) in 104 patients (34.4%) (Fig. 1). Clinical and procedural characteristics of the 3 groups are summarized in Table 3. B-type lesion was significantly more common in the MI group (41% vs. 16% in microleak and 29% in normal group; p = 0.007). Patients in MI group received more balloon inflations (mean 12.4 vs. 10.4 in normal group; p = 0.023). There was no difference in disease burden or other clinical comorbidities among the three groups. Patients were followed for a median of 9 months (range 7–16 months). During follow-up, 3 patients (1.0%) died, 2% had stable angina, 10.3% had non-fatal MI, and 87.7% remained asymptomatic. There was no statistically significant difference in the in the incidence of angina or MI across the 3 sub-groups.
Fig. 1.
Categories of post-PCI troponin level elevations. PCI, percutaneous coronary intervention; MI, myocardial infarction.
Table 3.
Clinical characteristics and outcomes on follow-up stratified by troponins categories.
| Parameter | Normal | Microleak | Periprocedural MI | p value |
|---|---|---|---|---|
| Age (years) | 52.9 | 52.6 | 54.6 | 0.20 |
| Recent MI (%) | 34.6 | 32.3 | 33.1 | 0.96 |
| Number of diseased vessels | 1.6 | 1.7 | 1.6 | 0.40 |
| Lesion type (A/B/C) | 62/29/13 | 74/16/16 | 57/41/9 | 0.17/0.007/0.44 |
| Number of stents | 1.1 | 1.3 | 1.3 | 0.052 |
| Total number of inflations | 10.3 | 12.4 | 12.4 | 0.02 |
| Longest inflation (mean) (s) | 34 | 28.1 | 34 | 0.003 |
| Follow-up | ||||
| Angina (%) | 2.8 | 0 | 3.8 | 0.62 |
| MI (%) | 8.4 | 3.2 | 9.4 | 0.51 |
| Asymptomatic | 87.9 | 93.5 | 86.9 | 0.43 |
MI, myocardial infarction.
Next, we stratified patients into groups based on number of biomarkers elevated after PCI. Table 4 shows clinical and procedural characteristics of patients across various groups. There was no statistically significant difference in the incidence of angina or MI at 9 months follow-up between these groups.
Table 4.
Clinical characteristics and outcomes on follow-up stratified by categories of number of elevated biomarkers.
| Parameter | No biomarker | Single biomarker | Two biomarkers | Three biomarkers | Four biomarkers | p value |
|---|---|---|---|---|---|---|
| Age (years) | 48.3 | 52.1 | 55.1 | 54.6 | 52.5 | 0.12 |
| Recent MI (%) | 45 | 34 | 31 | 33 | 35 | 0.51 |
| Number of diseased vessels | 1.5 | 1.6 | 1.6 | 1.6 | 1.5 | 0.40 |
| Lesion type (A/B/C) | 72/18/9 | 62/28/15 | 62/33/8 | 55/40/13 | 64/35/3 | 0.96 |
| Number of stents | 1.3 | 1.2 | 1.2 | 1.3 | 1.3 | 0.77 |
| Total number of inflations | 11.9 | 11.0 | 11.1 | 12.6 | 11.4 | 0.40 |
| Longest inflation (s) | 36.8 | 34.1 | 32.9 | 32.4 | 35.4 | 0.35 |
| Follow-up | ||||||
| Angina (%) | 0 | 4.7 | 3.2 | 2 | 3.5 | 0.69 |
| MI (%) | 9 | 9.4 | 4.3 | 11.9 | 7.1 | 0.60 |
| Asymptomatic | 91 | 85.9 | 92.6 | 84.2 | 89.3 | 0.87 |
MI, myocardial infarction.
4. Discussion
Large-scale studies, such as by Fuchs et al.17 (n = 1129), Cavallini et al.18 (n = 3494), and Kini et al.19 (n = 2873), showed that any increase in post-PCI cTnT has no prognostic implications during mid- or long-term follow-up, which is consistent with the findings of the present study. Nallamothu et al.20 (n = 1157, with 960 patients in the follow-up) showed that only very substantial cTnT elevation (>8 times the normal high levels) was associated with a reduction in long-term survival. Small-scale studies have shown similar results with no prognostic implications for post-PCI survival.21, 22, 23
All these studies have analyzed the prognostic value of myocardial damage determined only by measuring post-PCI cTnT. In this respect, they differ from our study because they included patients with very different degrees of myocardial damage in the same group. In our study, we combined markers of myocardial damage, and inflammatory and hemodynamic damage so as to facilitate the definition of 3 patient groups (no myocardial damage, minimal myocardial damage (microleak), and MI) on the basis of the results. Adding CK-MB values enabled us to distinguish between 2 groups of patients: those with minimal damage, whose prognosis does not differ from that of patients with no myocardial damage observed during the procedure, and those with myonecrosis (major myocardial damage), whose prospects for survival during follow-up are worse. Herrmann et al.24 showed that after elective PCI, elevated troponin T identified patients at risk of worse long-term results. Troponin T analysis was conducted quickly at the patient's bedside. With this test, post-PCI troponin T elevation was detected in 17.3% of patients, considerably fewer than in our patients with myocardial damage and in those reported elsewhere. In a group of 1949 patients, Prasad et al.25 showed that troponin T elevation, which occurred in 19.6% of patients, had clear prognostic implications for mortality and incidence of MI at 2-year follow-up. Moreover, troponin elevation was shown to be independently related to long-term mortality. In our study, the short-term (mean follow-up 8 months) results show non-significant correlation with prognostic relation of post-procedure troponin elevation both in the minimal myocardial damage (microleak) group as well in myonecrosis (MI) group.
Our study reported that 45% of patients experienced cTnT elevation post-PCI (10.6% in microleak and 34.4% in MI range). Milani et al.9 showed that post-PCI troponin microleak impacts cardiac prognosis similarly but much less than clear troponin elevation. Differences in the distribution could be contributed to the highly sensitive troponin assays used in our study with lower cut-off values (normal <0.01 ng/ml, microleak 0.01–0.03 ng/ml, and MI range >0.03 ng/ml), whereas in study by Milani et al., troponin I was used with a normal reference range of 0.59 ng/ml. This difference could have contributed to higher proportion of periprocedural MI and hence a weaker association with clinical outcomes. It has been difficult to understand why modest biomarker elevations after PCI are associated with an adverse prognosis. It is now clear that individuals at risk for mortality and/or recurrent AMI are not those who develop de novo elevations but those with elevations at baseline. It appears that biomarker elevations mark an adverse anatomic substrate. Consequently, these patients do worse. Initially, most studies were done utilizing insensitive assays or high cut-off values. Patients who develop substantial cTn elevations post-PCI are those with baseline elevations. Elevations from a normal baseline are less frequent and, with rare exception, usually modest. Commonly, minor elevations pre-PCI are accentuated post-PCI, and if high cut-off values or insensitive assays are used, it is only post-PCI when they are identified.
If we factor in the pre-PCI elevation values, the prognostic importance of post-PCI cTn and/or CK-MB values is totally obviated.19 However, the baseline value is substantially prognostic. It is for this reason that recent guidelines indicate that, in the absence of a normal baseline cTn, one cannot diagnose post-PCI injury because it is impossible to discern whether the elevation is related to the initial injury or the PCI. Consequently, post-PCI injury occurs, and it can be diagnosed by elevations in cTn if the baseline is normal, but elevations have little if any prognostic significance for cardiac events. If the baseline is elevated, one should not attempt to make the diagnosis of post-PCI injury.26
We observed a significant rise in overall mean NT-proBNP levels at 12–24 h post-PCI. Following PCI, 45% of patients had NT-proBNP >100 pg/ml; nearly 20% of patients had post-PCI NT-proBNP levels >100 pg/ml despite pre-PCI NT-proBNP levels <100 pg/ml. Though the prognostic role of natriuretic peptides following elective PCI and stenting has been documented, only single pre-procedural levels were evaluated in these studies.27, 28 Whether coronary stenting, which results in shorter procedural ischemic times as compared to plain balloon angioplasty, is also associated with rise in natriuretic peptides following PCI has not been well characterized, with studies reporting conflicting results. Though Tateishi et al.29 also reported a rise in BNP at 24 h following plain balloon angioplasty, our results contrast with previous studies of temporal changes in BNP levels following coronary stenting. Cantor et al., in a study of 55 patients undergoing elective PCI, showed that though BNP levels did not change significantly at 6 h post-PCI, there was an insignificant trend toward higher values at 18–24 h post-PCI.30 Yildirir et al. demonstrated that in patients undergoing coronary stenting, PCI did not cause any significant alteration in plasma BNP levels measured either at 1 or 24 h. Those with complex coronary lesions were more likely to have higher baseline BNP, a difference that persisted after stenting.31 These differences may be partly explained by the fact that patients with ACS were excluded in both of these studies, while our patient population was a relatively heterogeneous group, with nearly 65% of patients having a recent ACS. However, despite this, we observed that even patients with chronic stable angina demonstrated a significant rise in BNP following PCI.
Observational studies have suggested that periprocedural CRP levels might be a risk indicator for clinical outcomes after drug-eluting stent implantation. Elevated CRP levels were independently associated with increased risk of stent thrombosis and major clinical events. In the study by Park et al., there was no association between CRP levels and the need for repeat revascularization in patients treated with DES.32 These results were consistent with previous studies reporting the lack of an association between CRP and repeat revascularization after bare metal stent treatment.
We hypothesized that the addition of a combination of biomarkers from different pathophysiological pathways – a multimarker approach – could add substantial prognostic information with respect to the risk of MACE post-PCI as similar to clinical spectrum of spontaneous MI and ACS. Accordingly, we investigated whether the incorporation of troponin I, N-terminal pro-brain natriuretic peptide, and hs-CRP in a model with established risk factors improved the prediction of MACE post-PCI. Sabatine et al.16 have shown that it is possible to use a simple multimarker approach combining each of these markers (BNP, hs-CRP, cardiac troponins), assigning 1 point for each elevated marker, to improve risk stratification in patients with ACS. With this simple strategy, a 6- to 13-fold gradient of mortality risk may be established between those without elevation of any marker and those in whom all 3 markers are elevated.
5. Conclusion
In conclusion, our findings suggest that simultaneous assessment of troponin, CRP, and BNP in risk stratification of patients undergoing elective PCI does not provide incremental prognostic information. Usage of a simple multimarker strategy, in which patients are categorized based on the number of elevated biomarkers, failed to show better risk stratification of patients over a broad range of short- and long-term major cardiac events. Minor elevation in troponin levels post-PCI represents myocardial damage and, without meeting the criteria for necrosis, remains a clinically irrelevant event, not predicting a subsequent increase in MI or death.
Conflicts of interest
The authors have none to declare.
References
- 1.Cuculi C., Lim C.C., Banning A.P. Periprocedural myocardial injury during elective percutaneous coronary intervention: is it important and how can it be prevented? Heart. 2010;96:736–740. doi: 10.1136/hrt.2009.186189. [DOI] [PubMed] [Google Scholar]
- 2.Miller W.L., Garratt K.N., Burritt M.F. Baseline troponin level: key to understanding the importance of post-PCI troponin elevations. Eur Heart J. 2006;27:1061–1069. doi: 10.1093/eurheartj/ehi760. [DOI] [PubMed] [Google Scholar]
- 3.Thygesen K., Alpert J.S., White H.D., (Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction) Universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 4.Ohman E.M., Armstrong P.W., Christenson R.H. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. N Engl J Med. 1996;335:1333–1341. doi: 10.1056/NEJM199610313351801. [DOI] [PubMed] [Google Scholar]
- 5.Antman E.M., Tanasijevic M.J., Thompson B. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med. 1996;335:1342–1349. doi: 10.1056/NEJM199610313351802. [DOI] [PubMed] [Google Scholar]
- 6.Nageh T., Sherwood R.A., Harris B.M. Prognostic role of cardiac troponin I after percutaneous coronary intervention in stable coronary disease. Heart. 2005;91:1181–1185. doi: 10.1136/hrt.2004.042911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nienhuis M.B., Ottervanger J.P., Bilo H.J. Prognostic value of troponin after elective percutaneous coronary intervention: a meta-analysis. Catheter Cardiovasc Interv. 2008;71:318–324. doi: 10.1002/ccd.21345. [DOI] [PubMed] [Google Scholar]
- 8.Milani R.V., Fitzgerald R., Milani J.N. The impact of micro troponin leak on long-term outcomes following elective percutaneous coronary intervention. Catheter Cardiovasc Interv. 2009;74:819–822. doi: 10.1002/ccd.22160. [DOI] [PubMed] [Google Scholar]
- 9.Cantor W.J., Newby K., Chistenson R.H. Prognostic significance of elevated troponin I after percutaneous coronary intervention. J Am Coll Cardiol. 2002;39:1738–1744. doi: 10.1016/s0735-1097(02)01877-6. [DOI] [PubMed] [Google Scholar]
- 10.Mahajan V.S., Jarolim P. How to interpret elevated cardiac troponin levels. Circulation. 2011;124:2350–2354. doi: 10.1161/CIRCULATIONAHA.111.023697. [DOI] [PubMed] [Google Scholar]
- 11.de Lemos J.A., Morrow D.A., Bentley J.H. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med. 2001;345:1014–1021. doi: 10.1056/NEJMoa011053. [DOI] [PubMed] [Google Scholar]
- 12.Morrow D.A., de Lemos J.A., Sabatine M.S. Evaluation of B-type natriuretic peptide for risk assessment in unstable angina/non-ST elevation MI: BNP and prognosis in TACTICS-TIMI 18. J Am Coll Cardiol. 2003;41:1264–1272. doi: 10.1016/s0735-1097(03)00168-2. [DOI] [PubMed] [Google Scholar]
- 13.Omland T., de Lemos J.A., Morrow D.A. Prognostic value of N-terminal pro-atrial and pro-brain natriuretic peptide in patients with acute coronary syndromes. Am J Cardiol. 2002;89:463–465. doi: 10.1016/s0002-9149(01)02271-8. [DOI] [PubMed] [Google Scholar]
- 14.Morrow D.A., Rifai N., Antman E.M. C-reactive protein is a potent predictor of mortality independently of and in combination with troponin T in acute coronary syndromes: a TIMI 11A substudy. Thrombolysis in Myocardial Infarction. J Am Coll Cardiol. 1998;31:1460–1465. doi: 10.1016/s0735-1097(98)00136-3. [DOI] [PubMed] [Google Scholar]
- 15.Lindahl B., Toss H., Siegbahn A. Markers of myocardial damage and inflammation in relation to long-term mortality in unstable coronary artery disease. FRISC Study Group. Fragmin during Instability in Coronary Artery Disease. N Engl J Med. 2000;343:1139–1147. doi: 10.1056/NEJM200010193431602. [DOI] [PubMed] [Google Scholar]
- 16.Sabatine M.S., Morrow D.A., de Lemos J.A. Multimarker approach to risk stratification in non-ST elevation acute coronary syndromes: simultaneous assessment of troponin I, C-reactive protein, and B-type natriuretic peptide. Circulation. 2002;105:1760–1763. doi: 10.1161/01.cir.0000015464.18023.0a. [DOI] [PubMed] [Google Scholar]
- 17.Fuchs S., Kornowski R., Mehran R. Prognostic value of cardiac troponin I levels following catheter-based coronary interventions. Am J Cardiol. 2000;85:1077–1082. doi: 10.1016/s0002-9149(00)00699-8. [DOI] [PubMed] [Google Scholar]
- 18.Cavallini C., Savonitto S., Violini R. Impact of the evaluation of biochemical markers of myocardial damage on long-term mortality after percutaneous coronary intervention: results of the CK-MB and PCI study. Eur Heart J. 2005;26:1506–1512. doi: 10.1093/eurheartj/ehi173. [DOI] [PubMed] [Google Scholar]
- 19.Kini A., Lee P., Marmur J.D. Correlation of postpercutaneous coronary intervention creatine kinase-MB and troponin I elevation in predicting mid-term mortality. Am J Cardiol. 2004;93:18–23. doi: 10.1016/j.amjcard.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 20.Nallamothu B.K., Chetcuti S., Mukherjee D. Prognostic implication of troponin I elevation after percutaneous coronary intervention. Am J Cardiol. 2003;91:1272–1274. doi: 10.1016/s0002-9149(03)00283-2. [DOI] [PubMed] [Google Scholar]
- 21.Bertinchant J.P., Polge A., Ledermann B. Relation of minor cardiac troponin I elevation to late cardiac events after uncomplicated elective successful percutaneous transluminal coronary angioplasty for angina pectoris. Am J Cardiol. 1999;84:51–57. doi: 10.1016/s0002-9149(99)00191-5. [DOI] [PubMed] [Google Scholar]
- 22.Garbarz E., Iung B., Lefevre G. Frequency and prognostic value of cardiac troponin I elevation after coronary stenting. Am J Cardiol. 1999;84:515–518. doi: 10.1016/s0002-9149(99)00369-0. [DOI] [PubMed] [Google Scholar]
- 23.Wu A.H., Boden W.E., McKay R.G. Long-term follow-up of patients with increased cardiac troponin concentrations following percutaneous coronary intervention. Am J Cardiol. 2002;89:1300–1302. doi: 10.1016/s0002-9149(02)02331-7. [DOI] [PubMed] [Google Scholar]
- 24.Herrmann J., von Birgelen C., Haude M. Prognostic implication of cardiac troponin T increase following stent implantation. Heart. 2002;87:549–553. doi: 10.1136/heart.87.6.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prasad A., Singh M., Lerman A. Isolated elevation in troponin T after percutaneous coronary intervention is associated with higher long-term mortality. J Am Coll Cardiol. 2006;48:1765–1770. doi: 10.1016/j.jacc.2006.04.102. [DOI] [PubMed] [Google Scholar]
- 26.Jaffe A.S. The 10 commandments of troponin: with special reference to high sensitivity assays. Heart. 2011;97:940–946. doi: 10.1136/hrt.2009.185751. [DOI] [PubMed] [Google Scholar]
- 27.de Winter R.J., Stroobants A., Koch K.T. Plasma N-terminal pro-B-type natriuretic peptide for prediction of death or nonfatal myocardial infarction following percutaneous coronary intervention. Am J Cardiol. 2004;94:1481–1485. doi: 10.1016/j.amjcard.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 28.Saleh N., Braunschweig F., Jensen J. Usefulness of preprocedural serum N-terminal pro-brain natriuretic peptide levels to predict long-term outcome after percutaneous coronary intervention in patients with normal troponin T levels. Am J Cardiol. 2006;97:830–834. doi: 10.1016/j.amjcard.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 29.Tateishi J., Masutani M., Ohyanagi M. Transient increase in plasma brain (B-type) natriuretic peptide after percutaneous transluminal coronary angioplasty. Clin Cardiol. 2000;23:776–780. doi: 10.1002/clc.4960231016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cantor W.J., Kim H.H., Jolly S. B-type natriuretic peptide and serum unbound free fatty acid levels after contemporary percutaneous coronary intervention. J Invasive Cardiol. 2008;20:186–188. [PubMed] [Google Scholar]
- 31.Yildirir A. Effects of lesion complexity on baseline and post procedural B-type natriuretic peptide levels in patients undergoing percutaneous coronary interventions. Tex Heart Inst J. 2007;34:282–289. [PMC free article] [PubMed] [Google Scholar]
- 32.Park D.W., Yun S.C., Lee J.Y. C-reactive protein and the risk of stent thrombosis and cardiovascular events after drug-eluting stent implantation. Circulation. 2009;120:1987–1995. doi: 10.1161/CIRCULATIONAHA.109.876763. [DOI] [PubMed] [Google Scholar]