Abstract
Background
Single motherhood is associated with poorer health, but whether this association varies between countries is not known. We examine associations between single motherhood and poor later-life health in the US, England and 13 European countries.
Methods
Data came from 25,125 women aged 50+ who participated in the US Health and Retirement Study, the English Longitudinal Study of Ageing, and Survey of Health, Ageing and Retirement in Europe. We tested whether single motherhood at ages 16–49 was associated with increased risk of limitations with activities of daily living (ADL), instrumental ADL (IADL) and fair/poor self-rated health in later life.
Results
33% of American mothers had experienced single motherhood before age 50, versus 22% in England, 38% in Scandinavia, 22% in Western Europe and 10% in Southern Europe. Single mothers had higher risk of poorer health and disability in later life than married mothers, but associations varied between countries. For example, risk ratios for ADL limitations were 1.51 (95% CI 1.29, 1.98) in England, 1.50 (1.10, 2.05) in Scandinavia and 1.27 (1.17, 1.40) in the US, versus 1.09 (0.80, 1.47) in Western Europe, 1.13 (0.80, 1.60) in Southern Europe, and 0.93 (0.66, 1.31) in Eastern Europe. Women who were single mothers before age 20, for 8+ years, or resulting from divorce or non-marital childbearing, were at particular risk.
Conclusion
Single motherhood during early- or mid-adulthood is associated with poorer health in later life. Risks were greatest in England, the US, and Scandinavia. Both selection and causation mechanisms might explain between-country variation.
Keywords: single motherhood, aging, social determinants of health, cross-national comparisons
Introduction
Single motherhood—the experience of parenting without a marital partner—is associated with increased risk of health problems, including poor self-rated health (SRH), adverse cardiovascular risk, poor mental health, and increased mortality.[1–11] Prior studies have focused primarily on contemporaneous associations between single motherhood and health, but few studies have examined the “long arm of single motherhood” or how single motherhood during early and mid-adulthood relates to health and functioning at older ages. Recent birth cohorts are increasingly likely to have experienced a spell of single parenting,[12] but little research links single parenting to health in later life.
Except for several comparative studies of two or three countries,[4, 6, 9] no studies have systematically examined whether associations between single motherhood and health vary across countries; this question is important for several reasons. Single motherhood is associated with poverty in most societies, but more so in the US than in Europe.[13, 14] This may lead to different mechanisms of selection into lone motherhood between countries. Particularly in Southern European countries, strong social and family networks may offset some negative effects of single motherhood. Single mothers’ risk of poverty, for example, may be offset by family support. Family policies aiming to encourage women to combine motherhood with labor force participation in the UK and European may have positive effects, but they may also have unintended consequences. For example, feminist welfare state theories suggest that family policies may in fact reinforce women’s roles as unpaid caregivers or encourage part time paid work.[15–17]
We hypothesize that women experiencing an episode of single motherhood before age 50 have worse health at older ages than married mothers, and that single motherhood is most damaging in countries with relatively weak social safety nets, such as the US and England. Building on a life course model of health, we assess cumulative effects of single parenting as a risk factor for poorer functioning and health at older ages. We test these hypotheses using harmonized data from population-based studies of older adults in the US, England, and 13 continental European countries.
Methods
Data
We used three harmonized longitudinal surveys on health and aging: the US Health and Retirement Study (HRS), English Longitudinal Study of Aging (ELSA), and Survey of Health, Aging, and Retirement in Europe (SHARE) which represents 21 continental European countries (13 of which collected life history data essential for these analyses). These surveys are described in detail elsewhere.[18–21] Briefly, each study conducts biennial assessments of nationally representative samples of non-institutionalized adults age 50+. HRS was implemented in 1992, ELSA in 2002, and SHARE in 2004. Survey comparability is discussed elsewhere.[22] We categorized the 13 European SHARE countries into four geographic regions: Scandinavia (Denmark, Sweden), Western Europe (Austria, France, Germany, Switzerland, Belgium, Netherlands), Southern Europe (Italy, Spain, Greece), and Eastern Europe (Poland, Czech Republic). This categorization is based on geographic and cultural proximity and types of welfare regimes.
HRS data from 2004 and 2006 are included. ELSA data are from 2004 and 2006; ELSA life history interviews regarding childbearing and marriage were conducted in 2006, so we include only ELSA respondents who completed 2006 interviews. SHARE includes respondents participating in the 2008 wave (SHARELIFE), which collected life histories on childbearing and marriage. SHARE participants were interviewed at least once in 2004 or 2006. Response rates for the 2004 and 2006 HRS ranged from 75.3% to 91.4%.[23] In ELSA, response rates were 81% in 2004 and 69% for completing both main and life history interviews in 2006.[19] Overall SHARE rates were 52.5% in 2004, 46% in 2006, and 61% in 2008, with country variation.[20] Each survey provides individual-level sample weights, used in descriptive and regression analyses, accounting for both sample design and non-response; weighted samples are nationally representative of target populations in each country by survey year. We excluded women with no children by age 50. The final analytic sample was 25,125 women aged 50+, with 42,830 observations total (17,866 from HRS, 6,294 from ELSA, and 18,670 from SHARE). This study was approved by relevant human subjects committees.
Outcomes
We examine three outcomes: limitations in activities of daily living (ADLs), limitations in instrumental ADLs (IADLs), and fair/poor self-rated health (SRH).[24, 25] ADL questions asked about bathing, dressing, eating, getting in/out of bed, and walking across room. Participants were asked if they had any difficulty because of physical, mental, emotional, or memory problems. Response options were binary (yes/no) in ELSA and SHARE. In HRS there were two additional options: “don’t do” or “can’t do.” Individuals are classified as having any ADL limitation if they reported “yes” or “can’t do”. IADL questions asked about any difficulty with: making meals, shopping, making phone calls, medications, and managing money. Those reporting “yes” or “can’t do” for any activity are classified as having an IADL limitation. SRH is assessed by asking “Would you say your health is …” with a Likert scale response (excellent/very good/good/fair/poor). We dichotomize SRH into fair/poor versus other.
Predictors
The key predictor of interest is single motherhood experience between ages 15–49. A woman was considered a single mother in any year when she had children under age 18 and was not married. Each woman was asked to report all children’s birth or adoption dates. Women were asked about beginning and ending dates of each marriage. For each year between ages 15–49, we created indicators for whether she had at least one biological or adopted child under age 18 (based on child birth-year data) and for whether she was married (based on whether that year fell between beginning and ending years of any marriage reported). Information on non-marital partners was not consistently collected, so is not included in main analyses, but is used in sensitivity analyses. Child and marriage variables were used to generate a binary indicator for whether a woman ever experienced single motherhood before age 50. We developed categorical indicators for duration of single motherhood (1–3; 4–7; 8–13; 14+ years), corresponding to quartiles of single motherhood duration among those with any single motherhood history. We further characterized types of single motherhood (attributable to non-marital childbearing, widowhood, or divorce) and earliest age of single motherhood (before age 20, 20–29, 30–39, 40+).
Statistical analysis
For each outcome, we estimate adjusted relative risks (RRs) and 95% confidence intervals (CI) associated with single motherhood in each region using modified Poisson regression models, which assume Poisson distributions and use robust variances to correct for error term misspecification. Modified Poisson regression permits estimation of RRs with common binary outcomes [26] if log-binomial models fail to converge, as occurred here.[27–33] Because we had up to two observations per individual, we corrected standard errors by clustering at the individual level to account for correlations between repeated outcomes in the same woman. Sensitivity analyses used one observation per woman.
For primary analyses, key independent variables were interactions between the six country/region dummy variables (US, England, Scandinavia, Western Europe, Southern Europe, Eastern Europe) and an indicator of any single motherhood experience. We additionally adjusted for covariates: assessment year, age, age squared, educational attainment (secondary, primary or less, tertiary [reference]), number of children (one [reference], two, three or more), and current marital status (married [reference] or not). We allow effects of covariates to vary by country/region by including region-covariate interaction terms. We include country-level fixed effects. We conduct Wald tests to assess whether RRs associated with single motherhood were equivalent across different country/regions.[34] We use alpha criteria of 0.05 and 0.10 for statistical and marginal significance respectively.
Next, we examine whether adjustment for current relative income and wealth attenuates associations between single motherhood and outcomes, by region. For these models, we add interactions of six country/region dummies with per-capita household income and wealth quintiles. These metrics were generated by dividing income or wealth by square root of household size[35]. We used country- and time-specific income and wealth quintiles.
We investigate variation in observed associations by single motherhood duration, type, and age. Sample size limitations precluded interactions between those characteristics and the six regional indicators. Models adjust for core covariates as in primary analyses. Models for type and age of single motherhood were each adjusted for duration. Sampling weights were used and robust variances clustered within individuals were estimated. While our preference was for region specific analysis, small sample sizes by regions meant we had limited power to explore regional effects of duration and pathways into single motherhood. We therefore focus on pooled analyses.
Analyses were conducted in Stata Special Edition, version 11 (StataCorp, College Station, Texas).
Results
History of single motherhood among women age 50+
In the US, 32.8% of mothers aged 50+ had any single motherhood experience ages 15–49, compared to 22.0% in England, 38.2% in Scandinavia, and 10.2% in Southern Europe (Table 1). Divorce was the most common reason for single motherhood. In European countries and England, excluding unmarried women with partners from the single motherhood definition, lifetime prevalence of single motherhood decreased by less than four percentage points, except in Scandinavia where it decreased by 11 percentage points. In pooled analyses, we do not take partnership into account since it is not available for all countries. In sensitivity analyses by region, however, we explicitly test associations of partnership versus marriage with health.
Table 1.
Single motherhood experience among mothers aged 50+, by region
| US (n=17866) | England (n=6294) | Scandinavia (n=2972) | Western Europe (n=8576) | Southern Europe (n=5305) | Eastern Europe (n=1817) | |
|---|---|---|---|---|---|---|
|
|
||||||
| Ever single mother, No (%) | 5429 (32.8) | 1337 (22.0) | 1068 (38.2) | 1687 (22.8) | 472 (10.2) | 312 (20.4) |
| Single motherhood due to | ||||||
| Non-marital childbearing+ | 1710 (8.8) | 353 (6.2) | 527 (18.2) | 606 (8.7) | 129 (3.1) | 94 (5.8) |
| Widowhood | 829 (4.8) | 183 (3.0) | 74 (2.9) | 300 (4.5) | 193 (4.5) | 76 (6.0) |
| Divorce | 3494 (22.6) | 875 (14.3) | 559 (20.5) | 870 (11.3) | 157 (2.8) | 154 (9.7) |
| Single motherhood at age | ||||||
| <20 | 868 (4.2) | 88 (1.6) | 122 (4.3) | 154 (2.3) | 32 (0.9) | 26 (1.0) |
| 20–29 | 2046 (12.5) | 394 (6.8) | 467 (15.9) | 612 (8.7) | 121 (2.8) | 113 (8.3) |
| 30–39 | 1558 (10.2) | 517 (8.5) | 314 (11.6) | 553 (7.3) | 148 (2.9) | 103 (6.8) |
| 40–49 | 957 (5.8) | 338 (5.2) | 165 (6.4) | 368 (4.5) | 171 (3.7) | 70 (4.2) |
| Ever single mother without partner#, No (%) | NA | 1106 (18.3) | 714 (26.9) | 1420 (19.3) | 405 (8.8) | 275 (17.8) |
Notes:
Mothers include women who have ever had any biological or adopted children. A woman was defined as having been “ever single mother” if, in any year when she was age 15–49, she had a child under age 18 but was not married.
Number of observations and the percentages (in parentheses) are shown. Sampling weights were used for estimating percentages.
Mothers in the “non-marital childbearing” include the “never married” group as well as women who reported one or more marriages, but were unmarried at the time of the child’s birth.
HRS does not collect information on partnership history.
Countries in each regions are: Scandinavia (Denmark and Sweden), Western Europe (Austria, France, Germany, Switzerland, Belgium, Netherlands), Southern Europe (Italy, Spain and Greece), and Eastern Europe (Poland and Czech Republic).
Data sources: Health and Retirement Study (HRS) in year 2004 and 2006; English Longitudinal Study of Aging (ELSA) in year 2004 and 2006; Survey of Health, Ageing, and Retirement in Europe (SHARE) in year 2004 and 2006 and SHARELIFE in year 2008.
Sample characteristics by single motherhood status
In every region, women with past experiences of single motherhood were younger, had lower income and wealth, and were less likely to be married as older adults compared with consistently married mothers (Table 2). In the US and England, single mothers were more likely to have primary education or lower. Single motherhood was not associated with education in other regions.
Table 2.
Demographic and health characteristics by single motherhood experience, among mothers aged 50+, by region
| US (n=17866) | England (n=6294) | Scandinavia (n=2972) | Western Europe (n=8576) | Southern Europe (n=5305) | Eastern Europe (n=1817) | |
|---|---|---|---|---|---|---|
|
|
||||||
| Mean age (years) | ||||||
| Married mother | 67.1 | 66.5 | 67.7 | 65.3 | 66.1 | 64.5 |
| Ever single mother | 62.5 | 62.4 | 61.8 | 63.7 | 65.6 | 62.7 |
| No (%) Currently married | ||||||
| Married mother | 7569 (67.4) | 3226 (77.2) | 1445 (65.7) | 5086 (69.1) | 3732 (70.1) | 1080 (63.2) |
| Ever single mother | 2078 (39.3) | 305 (26.7) | 594 (45.5) | 636 (32.8) | 123 (25.0) | 107 (28.0) |
| Number of children = 2 | ||||||
| Married mother | 3978 (37.4) | 2350 (47.5) | 950 (49.0) | 2821 (41.3) | 2276 (42.1) | 733 (41.9) |
| Ever single mother | 1502 (31.3) | 496 (35.2) | 458 (41.5) | 624 (32.6) | 160 (27.5) | 120 (36.6) |
| Number of children>= 3 | ||||||
| Married mother | 6291 (50.4) | 1601 (32.9) | 676 (36.1) | 2744 (38.6) | 1794 (43.0) | 555 (45.8) |
| Ever single mother | 3069 (51.8) | 543 (43.5) | 364 (33.4) | 665 (40.7) | 174 (45.4) | 123 (42.9) |
| Secondary education | ||||||
| Married mother | 4741 (40.2) | 1789 (33.7) | 553 (28.1) | 2249 (39.0) | 763 (12.8) | 610 (41.8) |
| Ever single mother | 1958 (36.2) | 504 (33.6) | 347 (32.3) | 575 (42.4) | 86 (16.3) | 126 (45.4) |
| Primary education or less | ||||||
| Married mother | 2421 (17.4) | 2632 (57.9) | 774 (43.6) | 3277 (42.0) | 3686 (82.8) | 789 (52.3) |
| Ever single mother | 1522 (22.5) | 719 (59.6) | 364 (36.1) | 761 (37.8) | 346 (77.8) | 164 (51.4) |
| Bottom income quintile | ||||||
| Married mother | 2109 (15.7) | 742 (16.1) | 280 (18.4) | 1178 (17.2) | 889 (18.9) | 257 (19.3) |
| Ever single mother | 1820 (30.2) | 328 (26.9) | 149 (15.6) | 388 (23.8) | 116 (23.8) | 85 (27.2) |
| Top income quintile | ||||||
| Married mother | 2016 (21.3) | 1133 (22.0) | 469 (21.4) | 1504 (21.0) | 1011 (19.5) | 342 (22.2) |
| Ever single mother | 657 (14.9) | 232 (15.5) | 264 (22.8) | 292 (17.3) | 94 (20.0) | 46 (12.2) |
| Bottom wealth quintile | ||||||
| Married | 1787(13.7) | 611 (14.1) | 210 (12.8) | 946 (14.2) | 810 (17.6) | 226 (18.3) |
| Ever single mother | 1955 (33.8) | 454 (37.9) | 209 (22.1) | 469 (30.4) | 130 (31.9) | 65 (22.8) |
| Top wealth quintile | ||||||
| Married mother | 2543 (22.7) | 1187 (22.4) | 509 (25.0) | 1592 (23.5) | 980 (19.5) | 322 (21.9) |
| Ever single mother | 549 (11.7) | 172 (10.9) | 234 (20.6) | 250 (15.1) | 71 (16.1) | 55 (16.1) |
| No (%) Any ADL limitations | ||||||
| Married mother | 1863 (15.0) | 874 (18.4) | 142 (8.4) | 590 (9.7) | 495 (12.3) | 233 (21.2) |
| Ever single mother | 1089 (18.9) | 329 (26.3) | 90 (9.5) | 154 (10.5) | 64 (14.3) | 39 (17.8) |
| Any IADL limitations | ||||||
| Married mother | 1711 (13.8) | 539 (11.9) | 119 (7.5) | 445 (7.6) | 402 (9.9) | 178 (16.6) |
| Ever single mother | 929 (16.1) | 236 (20.0) | 50 (5.5) | 107 (6.7) | 50 (11.1) | 28 (11.6) |
| Fair/poor SRH | ||||||
| Married mother | 3098 (23.9) | 1272 (27.2) | 384 (21.2) | 1941 (33.1) | 2060 (49.5) | 769 (59.6) |
| Ever single mother | 2020 (34.4) | 524 (42.9) | 240 (23.0) | 580 (40.7) | 207 (52.3) | 166 (57.6) |
Notes:
Mothers include women who have ever had any biological or adopted children. A woman was defined as having been “ever single mother” if, in any year when she was age 15–49, she had a child under age 18 but was not married. “Married mothers” were continuously married in all years they had children under age 18, i.e. they were never single mothers.
“(I)ADLs”: (Instrumental) activities of daily living.
SRH: Self-rated health.
Number of observations and the percentages (in parentheses) are shown. Sampling weights are used for estimating percentages.
Data sources: HRS in year 2004 and 2006; ELSA in year 2004 and 2006; SHARE in year 2004 and 2006 and SHARELIFE in year 2008.
Countries in each regions are: Scandinavia (Denmark and Sweden), Western Europe (Austria, France, Germany, Switzerland, Belgium, Netherlands), Southern Europe (Italy, Spain and Greece), and Eastern Europe (Poland and Czech Republic).
Are associations between single motherhood and functioning and health similar across countries?
Single motherhood was associated with higher risk of ADL/IADL limitations and fair/poor SRH in both the US and England; with ADL limitations and SRH in Scandinavia; but only with SRH in Western Europe (Table 3, Model I). For ADL limitations, RRs associated with single motherhood were highest in England (RR 1.51; 95%CI: 1.29, 1.77), followed by Scandinavia (1.50; 1.10, 2.05), and the US (1.27; 1.14, 1.40). RRs in Western Europe, Southern Europe and Eastern Europe were close to one and not significant. Wald tests provided marginally significant evidence (p=0.074) that coefficients for single motherhood differed by region.
Table 3.
Single motherhood and adjusted relative risks of disability and SRH among mothers aged 50+, by region
| Model specification I
|
Model specification II
|
|||||
|---|---|---|---|---|---|---|
| Any ADLs limitations | Any IADLs limitations | Fair/Poor SRH | Any ADLs limitations | Any IADLs limitations | Fair/Poor SRH | |
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
|
|
|||||
| Ever single mother in | ||||||
| US | 1.27*** | 1.27*** | 1.32*** | 1.09 | 1.09 | 1.16*** |
| [1.14,1.40] | [1.14,1.42] | [1.22,1.42] | [0.99,1.21] | [0.98,1.21] | [1.09,1.25] | |
| England | 1.51*** | 1.66*** | 1.61*** | 1.40*** | 1.41*** | 1.47*** |
| [1.29,1.77] | [1.36,2.02] | [1.43,1.81] | [1.19,1.65] | [1.15,1.71] | [1.31,1.66] | |
| Scandinavia | 1.50* | 0.98 | 1.20* | 1.40* | 0.87 | 1.12 |
| [1.10,2.05] | [0.63,1.53] | [1.01,1.44] | [1.03,1.90] | [0.57,1.33] | [0.93,1.34] | |
| Western Europe | 1.09 | 0.96 | 1.23*** | 0.99 | 0.87 | 1.17* |
| [0.80,1.47] | [0.66,1.39] | [1.09,1.39] | [0.73,1.35] | [0.60,1.26] | [1.04,1.32] | |
| Southern Europe | 1.13 | 1.07 | 1.06 | 0.97 | 0.94 | 1.04 |
| [0.80,1.60] | [0.73,1.55] | [0.92,1.22] | [0.69,1.38] | [0.65,1.37] | [0.91,1.20] | |
| Eastern Europe | 0.93 | 0.87 | 1.01 | 0.90 | 0.84 | 1.01 |
| [0.66,1.31] | [0.59,1.28] | [0.89,1.15] | [0.64,1.27] | [0.58,1.22] | [0.89,1.15] | |
| P-value for Wald test of equivalence of relative risks associated with single motherhood | ||||||
| All six regions | 0.074 | 0.011 | 0.000 | 0.037 | 0.046 | 0.000 |
| England vs. US | 0.068 | 0.021 | 0.004 | 0.011 | 0.027 | 0.001 |
| England vs. Scandinavia | 0.971 | 0.036 | 0.008 | 0.991 | 0.046 | 0.012 |
| England vs. Western Europe | 0.061 | 0.011 | 0.002 | 0.051 | 0.025 | 0.008 |
| England vs. Southern Europe | 0.139 | 0.042 | 0.000 | 0.064 | 0.063 | 0.000 |
| England vs. Eastern Europe | 0.012 | 0.003 | 0.000 | 0.024 | 0.016 | 0.000 |
P<0.001,
P<0.01,
P<0.05
Notes: Each column of Column (1) to (6) presents adjusted relative risks (point estimates and 95% confidence intervals) of single motherhood by region, obtained from modified Poisson regressions, with robust variance clustered at individual level. Data are weighted by sampling weights. Other control variables in “Model specification I” include the interactions of six country/region dummies with age, age squared, secondary education, primary education or less, number of children, and current marital status, as well as country and time fixed effects. Extra control variables are in “Model specification II”: per-capita household income quintiles and per-capita household wealth quintiles. Wald test p-values correspond to the null hypothesis that the relative risks associated with single motherhood are the same in the regions specified.
Data sources: HRS in year 2004 and 2006; ELSA in year 2004 and 2006; SHARE in year 2004 and 2006 and SHARELIFE in year 2008.
Countries in each regions are: Scandinavia (Denmark and Sweden), Western Europe (Austria, France, Germany, Switzerland, Belgium, Netherlands), Southern Europe (Italy, Spain and Greece), and Eastern Europe (Poland and Czech Republic).
Single motherhood experience was associated with IADL limitations in England (1.66; 1.36, 2.02) and the US (1.27; 1.14, 1.42) only. Wald tests showed RRs in England was significantly higher than RRs anywhere else. Single motherhood was associated with higher risk of poor SRH in all regions except Southern and Eastern Europe; associations were largest in England (1.61; 1.43, 1.81).
Do differences in income and wealth explain associations between single motherhood and health?
Adjusting for income and wealth quintiles, RRs for any ADL and IADL limitations were attenuated by more than 66% from Model I and were no longer statistically significant in the US (Table 3, Model II). The RR for SRH in US single mothers was substantially attenuated (from 1.32 to 1.16) but remained statistically significant after adjustment. In England, adjustment for income and wealth modestly attenuated associations between single motherhood and outcomes; all RRs remained statistically significant. In Scandinavia, adjustment for income and wealth modestly attenuated RRs for ADLs (1.50 to 1.40) and SRH (1.20 to 1.12).
Duration, type, and age of single motherhood
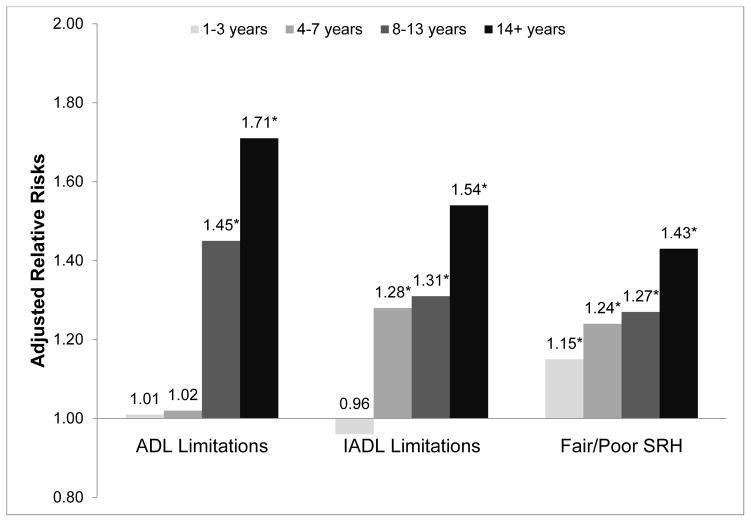
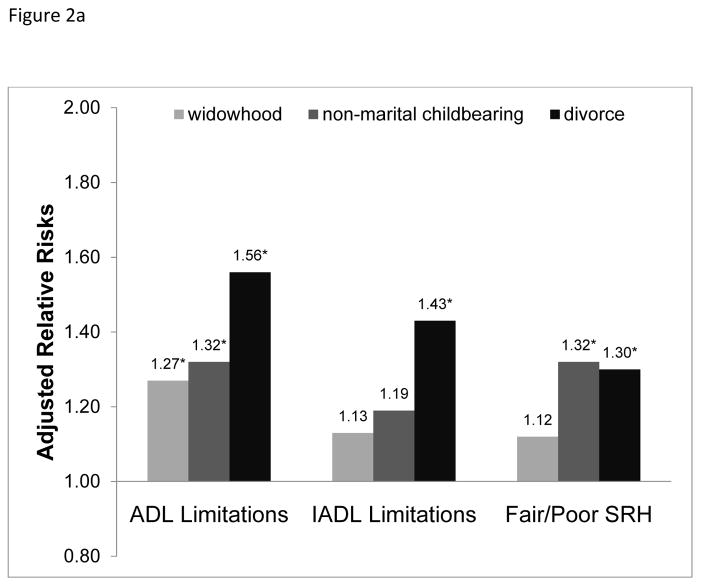
In pooled analyses for all countries, we found a ‘dose-response’ relationship between single motherhood duration and health (figure 1). For ADL limitations, being a single mother for 1–3 years was associated with a RR of 1.01 (0.87, 1.18); while being a single mother for 14+ years was associated with a RR of 1.71 (1.49, 1.97). Divorced single mothers had higher RRs than widowed single mothers (figure 2a).
Figure 1.
Single motherhood and adjusted relative risks of disability and SRH among mothers aged 50+, by quartiles of single motherhood duration
Notes:
“*” indicates p value < 0.05.
Data from ELSA, SHARE, and HRS are pooled in this analysis. Adjusted relative risks were obtained from modified Poisson regressions, with robust variance clustered at individual level. Key independent variables include binary indicators on quartiles of single motherhood duration: 1–3 years, 4–7 years, 8–13 years, 14+ years. The comparison group is mothers who never had single motherhood experience before age 50. Additional covariates include age, age squared, education, number of children, current marital status, time of interview, and country-fixed effects. Data are weighted by sampling weights.
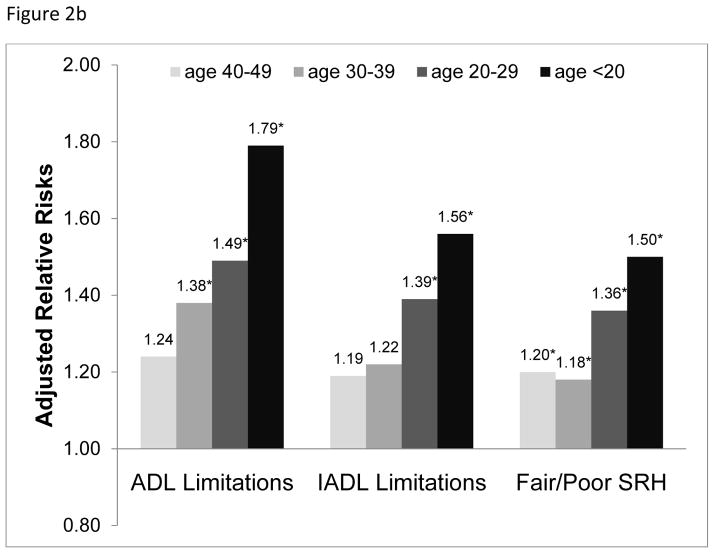
Figure 2.
Single motherhood and adjusted Relative risks of disability and SRH among mothers aged 50+, by causes or ages of single motherhood, conditional on single motherhood duration
Notes:
“*” indicates p value < 0.05.
Adjusted relative risks (RRs) of single motherhood by causes and ages of the single motherhood experience were estimated by running two sets of Poisson regressions: one has causes and quartiles of single motherhood duration as key independent variables, while the other has ages and quartiles of single motherhood duration as key independent variables. RRs reported in Figure 2-a and 2-b reflect the RRs of single mothers assuming a single motherhood duration of 8–13 years. The comparison group is mothers who never had single motherhood experience before age 50. Additional covariates include age, age squared, education, number of children, current marital status, time of interview, and country-fixed effects.
Women who were single mothers at younger ages also had higher RRs for later-life poor health and disability than women who experienced single motherhood at older ages (figure 2b).
Sensitivity analyses: Partnership status, childhood experiences, health and sociodemographics
A potential concern is the relatively larger proportion of unmarried women with a partner in some European countries. European women who had a partner during spells of single motherhood had better health on average than other single mothers, but worse health than married mothers. However, effect estimates were imprecise and confidence intervals (eTable 1). Sensitivity analyses indicate that risks between lone motherhood and outcomes are very similar regardless of whether we define lone motherhood by marital status alone, or include non-marital partnership in the definition. This is true for Scandinavia and other regions. For Scandinavian countries in SHARE, ADL risks associated with single motherhood were 1.56 (CI 1.11–2.18) when based on marital status alone, compared to 1.50 (CI 1.10,2.05) when defined by both marital status and non-marital partnership. Risk ratios for IADL were 0.99 (CI 0.62–1.58) for lone mothers (including partners) compared to 0.98 (CI 0.63,1.53) for lone mothers without partners; and risk ratios for poor self-rated health were 1.15(CI 0.95,1.40) for unmarried mothers compared to 1.20 (CI 1.01,1.44) for unmarried mothers without partners. Numbers are smaller in these analyses and CIs wider than in pooled analyses, yet our “bottom line” is that partnership status does not substantively change our findings. HRS did not assess partnership.
Given concern about selection into single motherhood, we assess whether social or health circumstances in childhood influence risk of becoming a single mother. Among European women, single mothers averaged worse childhood health and SES (eTable 2). Adjusting for these factors did not substantially change associations between single motherhood and health outcomes in England or Western Europe, but attenuated associations with ADLs in Scandinavia (eTable 3). Results suggest that some—although not all—of cross-national variations may reflect differences in mechanisms leading to selection into single motherhood.
Women with single-motherhood histories had greater cardiovascular risks than others (eTable 4). Adjustment for potential mediators, including smoking (eTable 5), obesity (eTable 5) and hypertension, plus diabetes, stroke or heart disease (eTable 6), attenuated but did not eliminate associations between single motherhood and poor health. Additional sensitivity analyses are shown in eTable 7–eTable 12.
Discussion
Lifetime experiences of single motherhood were associated with increased risks of physical limitations and poor health at older ages among mothers in England, Scandinavian countries and the US. Single motherhood was less consistently associated with health in Continental Western, Eastern or Southern European countries. Longer duration of single motherhood was associated with poorer outcomes.
Potential explanations for association between single motherhood and later-life health
Controlling for income and wealth attenuated effects in the US, but less so in other regions. Associations may reflect both selection and causation in cycles of disadvantage: poverty increasing risk of single motherhood reflecting in part earlier health disadvantages. Being a lone mother may hamper women’s abilities to gain education, accrue careers, and accumulate income also leading to poorer health. While our study is longitudinal in design, we often draw on retrospective recall of events occurring in early adulthood. Longitudinal data, prospectively following women from early to late adulthood would better enable us to disentangle pathways and mechanisms.
Single motherhood was strongly associated with adverse health in Sweden and Denmark. Two previous studies have shown that current single mothers in both Sweden and Britain had higher prevalence of poor SRH and chronic illnesses relative to coupled mothers, and magnitudes of relative differences were similar for these countries.[4, 9] In our study, although adjusting for later-life socioeconomic conditions somewhat attenuated RRs for Scandinavia (7%), associations between single motherhood and ADL limitations remained statistically significant. Strikingly, associations between single motherhood and ADLs and SRH in the US and Scandinavia were similar. We do present multiplicative effect estimates (RRs), so this result should be interpreted in light of overall better health in Scandinavia. Nevertheless, mechanisms besides poor social protection policies, such as a lack of social or family support, may have contributed to this finding. Future studies should incorporate employment experiences since it is likely that employment contributes to long run health and may relate to single motherhood. Detailed work histories necessary for these analyses are not available in a comparable way across all countries included here, prohibiting a full analysis. We acknowledge that employment patterns may be an explanation for observations.
Across all regions, single mothers were more likely to be smokers but not more likely to be obese; controlling for these risks did not eliminate associations. Controlling for cardiovascular conditions moderately reduced relative risks in the US/England, but not in other European countries, suggesting that such conditions may partially explain links between single motherhood and later functional impairment.
The role of social support in shaping observed associations
Social support and cohesive networks may partially explain associations between single motherhood and health. Social support is itself an important predictor of adult health and functioning.[36–39] Although we did not have detailed data in mid-life, social support might play an important role in alleviating strains of single motherhood. For example, in Southern Europe, a region emphasizing family solidarity, single motherhood is not associated with increased health risks. In the US, where Hispanics tend to have more family support than non-Hispanic whites,[40] Hispanic single mothers did not have increased risks.
Our results identify several vulnerable populations. Women with prolonged spells of single motherhood; those whose single motherhood resulted from divorce; women who became single mothers at young ages; and single mothers with two or more children were at particular risk.
Strengths and limitations
Major strengths are harmonized data across many countries and in-depth retrospective data on marriage and childbearing. The greatest limitation is reliance on self-reported health outcomes. Although SRH is a general health measure, it has been repeatedly shown to predict objective outcomes such as mortality.[41] ADLs and IADLs are commonly assessed by self-report.
HRS did not collect retrospective data on non-marital or same-sex partnership, so we were not able to test whether these partnerships offered similar protections as marriage. In sensitivity analyses, we found that incorporating non-married partners into analyses for Scandinavian and other European countries did not change associations substantially. Finally, we did not have retrospective information on SES, social support, or networks during single motherhood, so we cannot explicitly examine roles of these conditions during childbearing years in shaping observed effects.
The risks observed in Scandinavian countries are provocative and we speculate about some reasons for increased risks. However, previous research focusing on health inequalities have also found that Scandinavia (Denmark, Finland, Norway, perhaps with the exception of Sweden) have larger inequalities in mortality by educational attainment than other European countries and particularly in Southern European, where inequalities tend to be smaller despite less generous welfare state traditions. Thus, while surprising, our study is not contradictory to previous evidence that countries with generous welfare states may have smaller income inequality, but not necessarily smaller health Inequality [42]. A second issue relates to the risk of poverty among single mothers. In general, given higher levels of income support policies and overall lower levels of poverty in Scandinavia compared to other countries, it seems unlikely that poverty would be more strongly associated with lone motherhood in Scandinavian countries compared to other countries. A third explanation refers to the role of employment. Indeed, employment rates in Sweden and Denmark were relatively high compared to rates in other countries. It is difficult to predict whether this would result in larger or smaller risks associated with single motherhood. For example, higher employment rates among lone mothers may reduce poverty rates for Scandinavian women leading to smaller health risks associated with lone motherhood. On the other hand, higher levels of stress in combining work and family roles may have increased work-family strain, potentially leading to worse health. In addition, issues raised with regard to feminist theories about the welfare state may be important. [16, 17] For example, Sweden had more generous maternity benefits than other countries during the time that many women were single mothers in this study. It is possible that these policies reinforced the gendered division of roles and the strain associated with continued unpaid caregiving coupled with labor force participation. Although speculative, higher rates of work-family conflict may have contributed to their higher risk of poor health in later life. Finally, studies of social isolation suggest that risks of social isolation may be greater in Sweden- similar to US rates. Family dynamics and informal support in Southern Europe may play a protective role.
Conclusions and future directions
Findings add to the growing recognition that single motherhood may have long-term health effects on mothers.[6, 10, 43] As lone motherhood is on the rise in many countries, policies addressing health disadvantages of lone mothers may be essential to improving women’s health and reducing disparities. Social support and family dynamics may further protect single mothers. In environments where social interactions are valued at a cultural level, we find reduced risks. Anti-poverty programs may additionally moderate impacts of single parenting. Access to family planning resources and policies that help single mothers remain in the labor force balancing work and family demands, as well as informal work-family practices, may yield important benefits for single mothers and their families.
Supplementary Material
What is already known on this subject?
Single motherhood has been shown to predict multiple health conditions, both concurrently with single motherhood and later in life. While a few studies have compared two or three countries, no study has explicitly conducted a cross-national comparison of the magnitude of the association between single motherhood and later-life health.
What does this study add?
Lifetime history of single motherhood was associated with increased risk of later-life disability and poor health in the US, the UK, and Scandinavia, but not in continental Western, Eastern, or Southern Europe. As prevalence of single motherhood is on the rise across the developed world, social policies that protect women in vulnerable family situations may help improve population health and reduce health disparities as women age.
Acknowledgments
Funding: This study was supported by the National Institute on Aging 1 R01 AG040248-02. Funders had no role in conception, design, analysis, or interpretation of findings.
Footnotes
License for publication: The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in JECH editions and any other BMJPGL products to exploit all subsidiary rights, as set out in our licence (http://group.bmj.com/products/journals/instructions-for-authors/licence-forms/)
Competing interests: None to declare
Contributorship statement: YZ conducted the statistical analyses. All authors (LFB, YZ, MMG, MA, ABS, ELS) conceived the idea of the paper; read, commented and contributed to the writing of the paper; and approved the final version
References
- 1.Benzeval M. The self-reported health status of lone parents. Soc Sci Med. 1998;46:1337–53. doi: 10.1016/s0277-9536(97)10083-1. [DOI] [PubMed] [Google Scholar]
- 2.Berkman PL. Spouseless motherhood, psychological stress, and physical morbidity. J Health Soc Behav. 1969;10:323–34. [PubMed] [Google Scholar]
- 3.Burstrom B, Diderichsen F, Shouls S, et al. Lone mothers in Sweden: trends in health and socioeconomic circumstances, 1979–1995. J Epidemiol Community Health. 1999;53:750–6. doi: 10.1136/jech.53.12.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burstrom B, Whitehead M, Clayton S, et al. Health inequalities between lone and couple mothers and policy under different welfare regimes - the example of Italy, Sweden and Britain. Soc Sci Med. 2010;70:912–20. doi: 10.1016/j.socscimed.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Fritzell S, Burstrom B. Economic strain and self-rated health among lone and couple mothers in Sweden during the 1990s compared to the 1980s. Health Policy. 2006;79:253–64. doi: 10.1016/j.healthpol.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Grundy EMD, Tomassini C. Marital history, health and mortality among older men and women in England and Wales. Bmc Public Health. 2010;10 doi: 10.1186/1471-2458-10-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ringback Weitoft G, Haglund B, Rosen M. Mortality among lone mothers in Sweden: a population study. Lancet. 2000;355:1215–9. doi: 10.1016/s0140-6736(00)02087-0. [DOI] [PubMed] [Google Scholar]
- 8.Weitoft GR, Haglund B, Hjern A, et al. Mortality, severe morbidity and injury among long-term lone mothers in Sweden. Int J Epidemiol. 2002;31:573–80. doi: 10.1093/ije/31.3.573. [DOI] [PubMed] [Google Scholar]
- 9.Whitehead M, Burstrom B, Diderichsen F. Social policies and the pathways to inequalities in health: a comparative analysis of lone mothers in Britain and Sweden. Soc Sci Med. 2000;50:255–70. doi: 10.1016/s0277-9536(99)00280-4. [DOI] [PubMed] [Google Scholar]
- 10.Williams K, Sassler S, Frech A, et al. Nonmarital Childbearing, Union History, and Women’s Health at Midlife. Am Sociol Rev. 2011;76:465–86. doi: 10.1177/0003122411409705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young LE, Cunningham SL, Buist DSM. Lone mothers are at higher risk for cardiovascular disease compared with partnered mothers. Data from the National Health and Nutrition Examination Survey III (NHANES III) Health Care for Women International. 2005;26:604–21. doi: 10.1080/07399330591004845. [DOI] [PubMed] [Google Scholar]
- 12.Montez J, Sabbath E, Glymour M, et al. Trends in Work-Family Context among U.S. Women by Education Level, 1976 to 2011. Population Research and Policy Review. doi: 10.1007/s11113-013-9315-4. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gornick J, Meyers M. More Alike than Different: Revisiting the Long- Term Prospects for Developing “ European- Style” Work/Family Policies in the United States. Journal of Comparative Policy Analysis: Research and Practice. 2004;6:251–73. [Google Scholar]
- 14.Gornick JC, Meyers M. Families that work: policies for reconciling parenthood and employment. New York: Russell Sage Foundation; 2003. [Google Scholar]
- 15.Ruspini E. Living on the poverty line: lone mothers in Belgium, Germany, Great Britain, Italy and Sweden. MZES Working Papers. 1998 [Google Scholar]
- 16.Orloff A. Gender in the Welfare State. Annual Review of Sociology. 1996;22:51–78. [Google Scholar]
- 17.Lewis J. Gender and Welfare Regimes: Further Thoughts. Social Politics. 1997:160–77. [Google Scholar]
- 18.Börsch-Supan A, Jürges H. The Survey of Health, Ageing and Retirement in Europe – Methodology. Mannheim: MEA; 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scholes S, Medina J, Cheshire H, et al. Technical report (wave 3): living in the 21st century: older people in England: the 2006 English Longitudinal Study of Ageing. National Centre for Social Research; 2009. [Google Scholar]
- 20.Schröder M. Retrospective Data Collection in the Survey of Health, Ageing and Retirement in Europe. SHARELIFE Methodology. Mannheim: MEA; 2011. [Google Scholar]
- 21.Servais M. Overview of HRS Public Data Files for Cross-sectional and Longitudinal Analysis. 2010. [Google Scholar]
- 22.Meijer E, Zamarro G, Fernandes M. Comparison between SHARE, ELSA and HRS. In: Börsch-Supan A, Brugiavini A, Jürges H, et al., editors. Health, Ageing and Retirement in Europe (2004–2007) – Starting the longitudinal dimension. Mannheim: MEA; 2008. pp. 99–107. [Google Scholar]
- 23.Health and Retirement Study. Sample sizes and response rates. University of Michigan; 2011. [Google Scholar]
- 24.Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 25.Guralnik JM, LaCroix AZ, Abbott RD, et al. Maintaining Mobility in Late Life. I. Demographic Characteristics and Chronic Conditions. American Journal of Epidemiology. 1993;137:845–57. doi: 10.1093/oxfordjournals.aje.a116746. [DOI] [PubMed] [Google Scholar]
- 26.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA: the journal of the American Medical Association. 1998;280:1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 27.Brown TT, Cole SR, Li X, et al. Antiretroviral therapy and the prevalence and incidence of diabetes mellitus in the multicenter AIDS cohort study. Arch Intern Med. 2005;165:1179–84. doi: 10.1001/archinte.165.10.1179. [DOI] [PubMed] [Google Scholar]
- 28.LaCoursiere DY, Bloebaum L, Duncan JD, et al. Population-based trends and correlates of maternal overweight and obesity, Utah 1991–2001. Am J Obstet Gynecol. 2005;192:832–9. doi: 10.1016/j.ajog.2004.11.034. [DOI] [PubMed] [Google Scholar]
- 29.Pollack AZ, Buck Louis GM, Sundaram R, et al. Caffeine consumption and miscarriage: a prospective cohort study. Fertil Steril. 2010;93:304–6. doi: 10.1016/j.fertnstert.2009.07.992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Szklo-Coxe M, Young T, Peppard PE, et al. Prospective associations of insomnia markers and symptoms with depression. American Journal of Epidemiology. 2010;171:709–20. doi: 10.1093/aje/kwp454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zou GY. A modified Poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 32.Yelland LN, Salter AB, Ryan P. Performance of the Modified Poisson Regression Approach for Estimating Relative Risks From Clustered Prospective Data. American Journal of Epidemiology. 2011;174:984–92. doi: 10.1093/aje/kwr183. [DOI] [PubMed] [Google Scholar]
- 33.Spiegelman D, Hertzmark E. Easy SAS Calculations for Risk or Prevalence Ratios and Differences. American Journal of Epidemiology. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 34.Judge GG. The Theory and practice of econometrics. New York: Wiley; 1985. [Google Scholar]
- 35.The Organisation for Economic Co-operation and Development (OECD) Growing Unequal ? Income Distribution and Poverty in OECD Countries. Paris: 2008. [Google Scholar]
- 36.Berkman LF, Melchior M, Chastang JF, et al. Social integration and mortality: a prospective study of French employees of Electricity of France-Gas of France: the GAZEL Cohort. Am J Epidemiol. 2004;159:167–74. doi: 10.1093/aje/kwh020. [DOI] [PubMed] [Google Scholar]
- 37.Berkman L, Glass TA. Social integration, social networks, social support, and health. In: Berkman L, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. [Google Scholar]
- 38.Capistrant BD, Moon JR, Berkman LF, et al. Current and long-term spousal caregiving and onset of cardiovascular disease. Journal of Epidemiology and Community Health. 2011 doi: 10.1136/jech-2011-200040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kumar S, Calvo R, Avendano M, et al. Social support, volunteering and health around the world: Cross-national evidence from 139 countries. Social science & medicine. 2012;74:696–706. doi: 10.1016/j.socscimed.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 40.Almeida J, Molnar BE, Kawachi I, et al. Ethnicity and nativity status as determinants of perceived social support: Testing the concept of familism. Social Science & Medicine. 2009;68:1852–8. doi: 10.1016/j.socscimed.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 41.Idler EL, Benyamini Y. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 42.Mackenbach JP. The persistence of health inequalities in modern welfare states: The explanation of a paradox. Social Science & Medicine. 2012;75:761–9. doi: 10.1016/j.socscimed.2012.02.031. [DOI] [PubMed] [Google Scholar]
- 43.Williams K, Sassler S, Nicholson LM. For better or for worse? The consequences of marriage and cohabitation for single mothers. Soc Forces. 2008;86:1481–511. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.