Abstract
Background:
An ideal approach for valgus knees must provide adequate exposure with minimal complications due to approach per se. Median parapatellar approach is most commonly used approach in TKA including valgus knees. A medial subvastus approach is seldom used for valgus knees and has definite advantages of maintaining extensor mechanism integrity and minimal effect on patellar tracking. The present study was conducted to evaluate outcomes of total knee arthroplasty (TKA) and efficacy of subvastus approach in valgus knees in terms of early functional recovery, limb alignment and complications.
Materials and Methods:
We retrospectively reviewed 112 knees with valgus deformity between January 2006 and December 2011. All patients were assessed postoperatively for pain using Visual Analog Scale (VAS) and quadriceps recovery in form of time to active straight leg raising (SLR) and staircase competency and clinical outcomes using American Knee Society (AKS) score and radiographic evaluation with average followup of 40 months (range 24–84 months).
Results:
The mean VAS on postoperative day (POD) 1 and POD2 at rest was 2.73 and 2.39, respectively and after mobilization was 3.28 and 3.08, respectively (P < 0.001). The quadriceps recovery was very early and 92 (86.7%) patients were able to do active SLR by POD1 with mean time of 21.98 h while reciprocal gait and staircase competency was possible at 43.05 h. The AKS and function score showed significant improvement from preoperative mean score of 39 and 36 to 91 and 79 (P < 0.001), respectively, and the mean range of motion increased from 102° preoperatively to 119° at recent followup (P < 0.001). The mean tibiofemoral valgus was corrected from preoperative 16° (range 10°–35°) to 5° (range 3°–9°) valgus (P < 0.001).
Conclusions:
Mini-subvastus quadriceps approach provides adequate exposure and excellent early recovery for TKA in valgus knees, without increase in incidence of complications.
Keywords: Functional outcomes, subvastus approach, total knee arthroplasty, valgus deformity
MeSh terms: Arthroplasty, replacement, knee, osteoarrthritis, quadriceps muscle
INTRODUCTION
Angular deformities around the knee joint necessitate special consideration to restore normal alignment during total knee arthroplasty (TKA). Valgus knees are defined as those with >10° of mechanical tibiofemoral angle on standing hip to ankle anteroposterior (AP) radiographs. Typically, a valgus deformity may be due to bony deformities such as hypoplastic lateral condyle, tibial bone loss, or due to soft tissue contracture involving iliotibial band (IT band), biceps femoris, lateral collateral ligament (LCL) or posterolateral capsule,1,2,3,4 or may be due to both bony and soft tissue involvement. Moreover, it may also result from an overcorrected proximal tibial valgus osteotomy. Consequently, attenuation of medial soft tissue structures may be a late secondary event.1
An ideal approach for valgus knees must provide adequate exposure with minimal complications due to approach per se. Median parapatellar approach is most commonly used approach in TKA including valgus knees. Several studies 5,6,7,8,9,10 had demonstrated the use of lateral capsular approach and modified lateral capsular approach with repositioning of vastus lateralis or tibial tubercle osteotomy (TTO). In addition, a lateral Subvastus 11,12 approach has been described, but it may require snip of vastus lateralis obliquus 11 or TTO 12 to shift the patella medially. However, these conventional approaches may result in short and long term deficit in quadriceps muscle function post-TKA 13,14,15 or complications related to TTO. Subsequently, this may reflect lower patient satisfaction due to reduced mobility and significant pain in postoperative period.13
With the recent emphasis on minimally invasive muscle sparing approach in orthopedic surgery including TKA, the subvastus approach has been commonly described for varus knees. Furthermore, this approach has definite advantages of maintaining extensor mechanism integrity, minimal effect on patellar tracking and preservation of patellar blood supply.16,17,18,19,20 Ultimately, these lead to faster recovery periods, shorter hospital stay, minimal postoperative physiotherapy, improved patellar tracking and less postoperative pain,13,17,20,21,22 thereby resulting in better functional outcomes. However, this approach is seldom used for TKA in valgus knees.
Therefore, the present study aimed to evaluate the outcomes of TKA and efficacy of minimally invasive subvastus (mini-subvastus) approach in valgus knees in terms of: (1) Early functional recovery (2) Postoperative limb alignment and (3) Incidence of complications. We hypothesized that mini-subvastus approach can be well utilized for TKA in valgus knees and it results in early functional recovery with minimal complications.
MATERIALS AND METHODS
112 knees in 108 patients with valgus deformity operated for elective primary TKAs by subvastus approach between January 2006 and December 2011 (out of 3000 consecutive primary TKA's patients) were included in this retrospective study. Institutional ethics committee approval was taken. There were 91 females and 17 males. Of these, 2 patients were lost to followup. Thus, a total of 110 knees were available for followup. We included all patients with valgus deformity posted for unilateral TKA. Exclusion criteria were patients with previous arthrotomy of knee, neurological problems and those requiring revision TKA. A written informed consent was taken from all patients.
Operative procedure
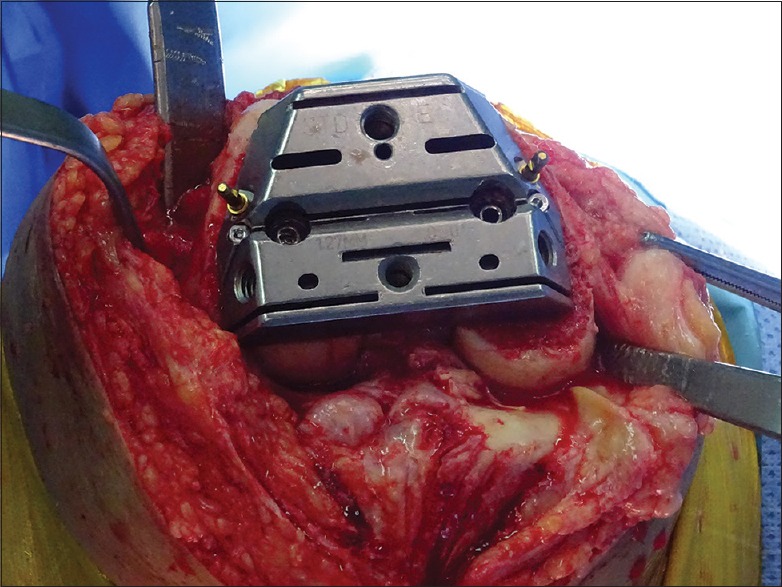
All surgeries were performed by senior author (NAS) using mini-subvastus approach without using pneumatic tourniquet. Tranexamic acid,23 15 mg/kg, was given 30 minutes prior to surgery and 2 doses 10 mg/kg were given 3 and 6 h postsurgery. A skin incision about 4 inches in length [Figure 1] was made slightly medial to the midline of the knee extending from the superior pole of patella to the tibial tubercle in 90° of flexion. Dissection was carried out until the extensor apparatus was exposed. Intraoperatively, saline adrenaline (1:300,000) was infiltrated into skin and subcutaneous tissue to reduce bleeding. Medial flap was raised to identify inferior margin of vastus medialis (VM). VM was bluntly dissected off the intermuscular septum. An L-shaped capsulotomy [Figure 2] made with horizontal limb of the L along the inferior margin of VM until the superior pole of patella and vertical limb of L was extended from here until tibial tubercle. The patella was displaced laterally to expose the suprapatellar synovium that was divided medially keeping the suprapatellar pouch intact [Figure 3].
Figure 1.
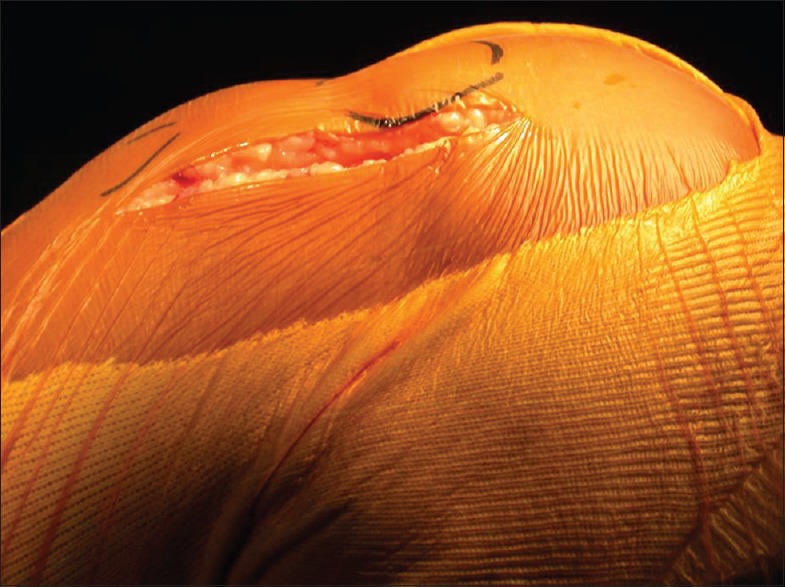
Peroperative photograph showing mini incision used for subvastus total knee arthroplasty
Figure 2.
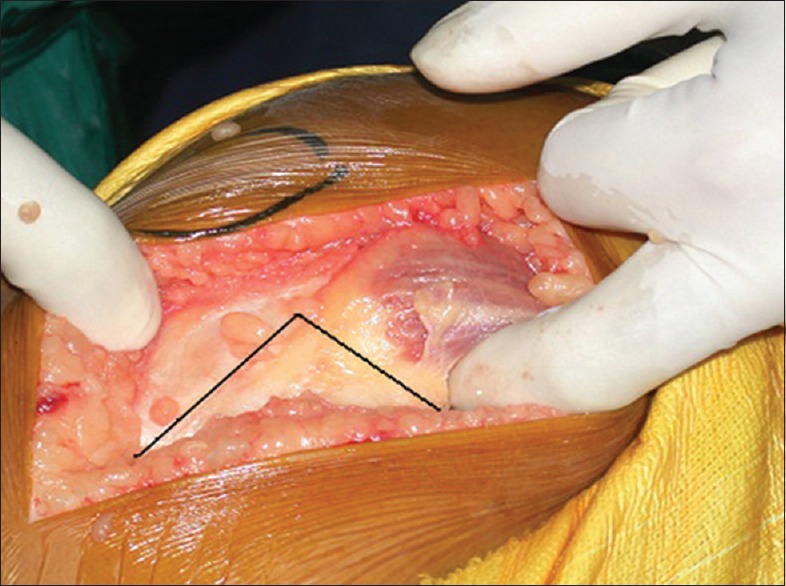
Intraoperative photograph showing L-shaped arthrotomy used for subvastus technique
Figure 3.
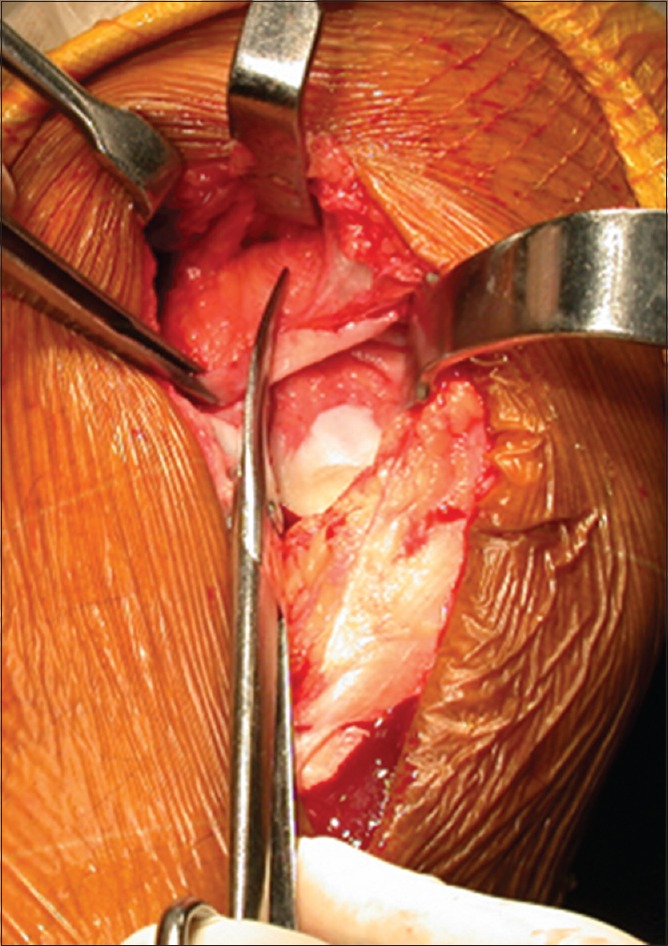
Intraoperative photograph showing division of suprapatellar synovium
At this stage, the femoral trochlea was visible. If present, prominent osteophytes in supratrochlear region were removed. The dissection on medial side was kept to a minimum and no ligament release was performed medially. The knee was exposed retracting the patella laterally. The distal femoral cut was made first using downsized intramedullary jig with the appropriate valgus angle, generally 3°. An extramedullary check was made preoperatively to confirm that this was indeed the correct valgus angle before making the femoral cut. The femoral pulse was felt and a marker (a stick on electrocardiography lead with metal) was placed over this. On this, a small vertical marker (an empty inverted water for injection sterile plastic ampoule) was strapped on in such a way that it would be easy to feel through the drapes. Before cutting the distal femur, the extramedullary femoral guide was used to ascertain that the rod was pointing to this marker applied preoperatively. An extramedullary jig was utilized to cut proximal tibia at adequate depth and angle. The tibial cut was made perpendicular to its mechanical axis using an extramedullary jig (i.e., neutral varus-valgus). The depth of the cut was 8–10 mm from the intact medial condyle (in valgus knee). The angle that is the slope of the cut was 0–3°. A spacer block was utilized to check extension space. If necessary, lateral release was performed to establish a symmetrical extension space as follows [Figure 4a and b]: With the knee in extension and distracted with lamina spreader, the posterolateral capsule was released from the tibia. Typically, this was done all along the tibial margin from 6° to 9° clock position. If further, posterolateral release was required, it was done with knee flexed at 90°. Care was taken not to detach the popliteus tendon as it is important to maintain stability in flexion. If still further release was required, IT band was released from Gerdy's tubercle. The LCL release although well described in literature, was not required in our cases.8,24,25 The anterior and posterior femoral cuts were made using the AP cutting jig. In all cases, we used the transepicondylar axis as a reference for jig placement [Figure 5]. The patella was everted only after femoral and tibial cuts had been made. Jig was utilized to size and resect the patella if patellar resurfacing was to be carried out. Trial components were inserted and careful check was made regarding range of motion (ROM), stability and patellar tracking. All knees used were fixed bearing metal backed components (cruciate retaining [CR] or posterioir stabilized [PS]; [Nexgen; LPS; Zimmer Inc., Warsaw, IN, USA]). All implants were fixed with cement. An apical stitch at the angle of the L was first taken to ensure that the capsule was neither advanced nor recessed. The rest of closure was routine. The knee was infiltrated with 20 cc of mixture containing 0.25% bupivacaine, cefuroxime and normal saline. At the end of the procedure, a bulky dressing was applied for the first 24 h.
Figure 4.
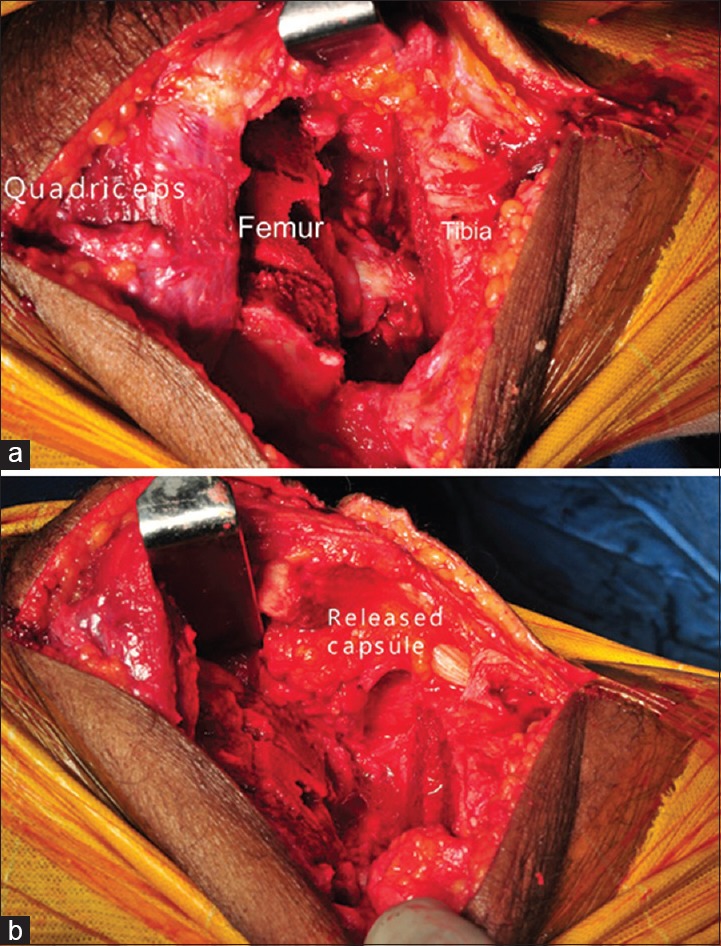
Intraoperative photograph showing (a) Asymmetrical extension gap with tight lateral structures. (b) Released lateral capsule
Figure 5.
Intraoperative photograph showing Jig placement parallel to the transepicondylar axis
Postoperative management and rehabilitation
A continuous femoral nerve block technique was used for 12 h postoperatively for pain control and early recovery. Postoperatively, mobilization was early and aggressive. Static quadriceps exercises and straight leg raising (SLR) exercise were started from day 0 and ROM exercises beginning from day one. Below knee thromboembolic disease stockings for both lower limbs were utilized. Chemical prophylaxis for deep vein thrombosis was in form of tablet aspirin 75 mg once a day for 3 weeks. Patients were encouraged to get out of bed and walk as tolerated from day 1.
Evaluation of preoperative status and functional outcomes
All clinical information was collected from database system maintained from predesigned data sheets by an independent investigator (one of authors). The clinical information included demographic data, preoperative and postoperative clinical status [Figure 6a and b] including degree of valgus deformity, the correctability, ROM, patients categories based on Krackow et al.26 classification of valgus knees and postoperative outcomes (at 2 weeks, 6 weeks, 3 months, 6 months, 12 months and yearly thereafter). Postoperative pain was assessed using Visual Analog Scale (VAS) on postoperative day (POD) 1 and POD2. Early quadriceps recovery was measured in form of time to active SLR and staircase competency. Preoperative clinical statuses and postoperative outcomes were evaluated using American Knee Society (AKS) knee and functional score.22 Postoperatively, a standing whole-limb AP radiograph was taken after surgery and yearly thereafter to measure mechanical tibiofemoral angle [Figure 7a and b]. Knee series including AP view, lateral view [Figure 7c and d] and an additional merchant view radiograph were also taken and evaluated.
Figure 6.

Clinical photograph showing (a) severe valgus deformity before total knee arthroplasty and (b) after total knee arthroplasty
Figure 7.
(a) Preoperative scanogram of a patient showing valgus deformity. (b) Postoperative scanogram after total knee arthroplasty showing correction of deformity (c) Postoperative radiograph with cruciate retaining prosthesis, anteroposterior view. (d) Postoperative radiograph with cruciate retaining prosthesis, lateral view
Two of the authors (NPJ, NAS) made all radiographic measurements using full length weight bearing AP radiographs. We measured mechanical tibiofemoral angle of knee, which was defined as the angle formed by the intersection between mechanical axes of the femur (line from the femoral head center to the femoral intercondylar notch center) and the tibia [line from the centre of ankle (talus) center to the center of knee (tibial spine tips)]. To determine the intra and inter-observer reliabilities of radiographic assessments, two investigators performed all radiographic assessments in 20 randomly selected radiographs twice with an interval of 1-week. The intra- and inter-observer reliabilities of assessments of all radiographic measurements were evaluated using intraclass correlation coefficients (ICCs). The ICCs of the intra- and inter-observer reliabilities of all measurements were >0.90. Because the measurements were judged reliable, measurements taken by a single investigator (NPJ) were used in the analyses.
Statistical analysis
Statistical analyses were performed using SPSS® for Windows® (version 20.0, IBM, Chicago, IL, USA). The difference was considered significant with P < 0.05 at a probability level of 95% for all comparisons. Statistical significance was determined using Student's t-test for continuous variables and the Chi-square, or the Fisher's exact test for categorical variables.
RESULTS
Mini-subvastus approach provided satisfactory exposure in all 110 cases of valgus knees. The mean duration of followup was 40 months (range 24–84 months). In no case, this approach was abandoned and the approach proved effective irrespective of the degree of valgus deformity [Table 1]. According to Krackow et al.,26 category for valgus knee, 76 knees were Type 1, 32 knees were Type 2 and 2 knees belonged to Type 3 category. The average surgical time was 80 min (range 60–122 min). The average blood loss was 600 ml (range 450–800 ml). A release of posterolateral capsule was done in 86 cases. An additional release of IT band was required in 62 cases. Release of the LCL or popliteus was not performed in any case. In all these cases, exposure of the lateral structures was satisfactory. A CR knees were used in 89 patients and PS knees in 20 patients and constrained condylar knee in one patient with severe combined valgus and recurvatum deformity and patellar resurfacing was done in 36 cases.
Table 1.
Demographic characteristics of patients undergoing total knee arthroplasty
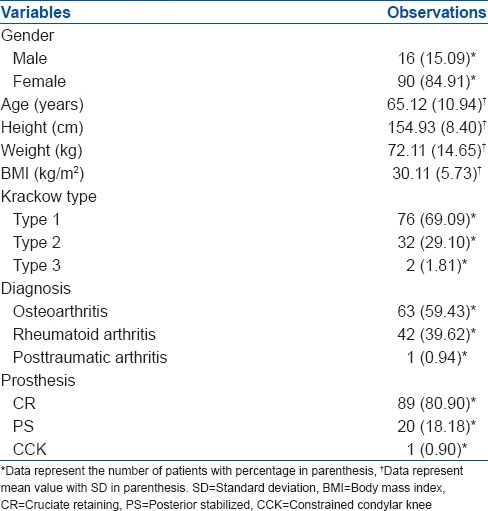
The mean (standard deviation [SD]) VAS on POD1 and POD2 at rest was 2.73 (0.67) and 2.39 (1.11), respectively and after mobilization was 3.28 (0.68) and 3.08 (1.20), respectively (P < 0.001). The quadriceps recovery was good, and 92 (86.7%) patients were able to do active SLR by POD1 with mean (SD) time of 21.98 (4.09) h. The mean (SD) time for reciprocal gait and staircase competency was 43.05 (6.59) h. The mean (SD) length of hospital stay was 3.3 (0.44) days.
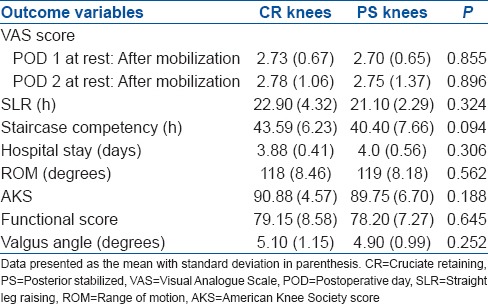
The AKS and function score showed significant improvement from preoperative mean of 39 (11.58) and 36 (11.27) to 91 (5.04) and 79 (8.30), respectively at latest followup (P < 0.001). The mean ROM increased from 102° (10) preoperatively to 119° (9) at recent followup (P < 0.001). Furthermore, overall mechanical alignment on radiological assessment was satisfactory. The mean tibiofemoral valgus angle was corrected from preoperative 16° (range 10–35°) to 5° (range 3–9°) of valgus (P < 0.001). There were three outliers with two patient having 9° valgus each and one with 8° valgus. Moreover, the component positioning and cementation appeared satisfactory on radiographs with no radiolucency's and signs of loosening in any patient. Furthermore, the outcome of TKA using either CR or PS knee showed similar results without any significant difference [Table 2].
Table 2.
Comparison of outcomes among CR and PS implant groups
Two patients underwent revision surgery, one for patellar component malposition; one had liner exchange for hyperextension. Also, one patient had foot drop postoperatively probably due to peroneal nerve injury that recovered gradually and completely within 6 weeks.
DISCUSSION
The most important finding of the present study is that medial-subvastus approach provides satisfactory and adequate exposure for TKA in valgus knees. TKA in valgus knees is considered to be more challenging 1,22 as it is relatively uncommon in practice. Moreover, it has a different pathoanatomy: Femur is internally rotated and tibia externally rotated, lateral femoral condyle is deficient in contrast to varus knee where tibia is usually involved, lateral and posterior contractures are present, and ligament balancing is difficult.2,3,4,27 Thus, the present study was undertaken to demonstrate the efficacy of mini-subvastus approach in valgus knees.
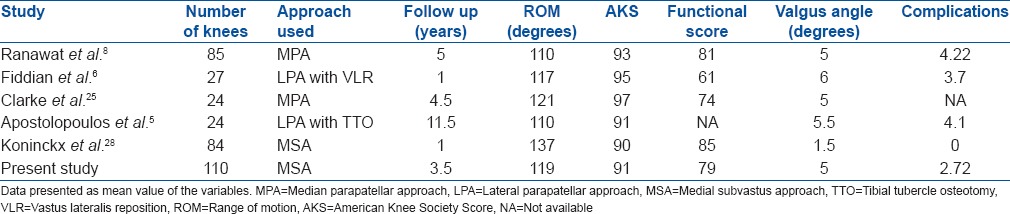
Our findings support the hypothesis that mini subvastus approach can be utilized for TKA in valgus knees and that it results in good functional outcome. The present study showed early postoperative recovery in patients post TKA with lower mean VAS score,28 early mobilization with active SLR and staircase competency. The findings of the present study of lower mean VAS score is considerably better than the similar VAS score assessed by Huang et al.22 using median parapatellar approach. Moreover, several studies 19,20,29,30 in past have evidently endorsed the benefits of muscle sparing subvastus approach in faster recovery and less postoperative pain. Also, recently published study 28 on effect of far medial-subvastus technique in fixed valgus Type 2 Krackow knees showed similar results. The functional outcome at the latest followup assessed by mean AKS score showed significant improvement. Moreover, the mechanical alignment was good with mean valgus angle of 5°. Similarly, comparable findings were reported in several studies [Table 3] using different approaches for TKA in valgus knees.
Table 3.
Summary of studies reporting outcomes of total knee arthroplasty in valgus knees
Medial parapatellar is universally accepted due to its familiarity to most surgeons and providing satisfactory exposure in valgus knees, even for lateral soft tissue release.19,20,31 However, several studies 6,32,33 have reported inferior outcomes with medial capsular approach. Particularly, it may be due to additional release of lateral soft tissue structures jeopardizing patellar blood supply.34 Multiple previous studies 5,6,7,8,9,10,11 had described lateral parapatellar and subvastus approaches for valgus knees. Moreover, one advantage of lateral approach is that it can directly address the disturbed pathoanatomy of valgus knee. Furthermore, lateral approach maintains intact medial soft tissue structures thereby rendering patellar vascularity 34 undisturbed. However, difficulties related to lateral capsulotomy is medial patellar eversion, its unfamiliarity to most surgeons and problems related to TTO.2,6,10 In spite of having obvious advantages over other conventional approaches, mini-subvastus approach is seldom used for TKA in valgus knees. In fact, it is considered to be relative contraindication in valgus knees.31 Moreover, the approach is considered difficult as it is not a familiar approach. Theoretically, it can be as good as or even better than median parapatellar approach, as illustrated by several studies.17,19,20,21,35 Nonetheless, it preserves the patellar vascularity even after lateral soft tissue release due to intact quadriceps mechanism. Furthermore, major criticism for subvastus technique includes difficulty in subluxation and eversion of patella, poor, and unpredictable exposure, more so of lateral structures and malalignment of components.29
In valgus knees, the patella tends to subluxate laterally due to tight lateral structures and attenuation of medial structures.36 Thus, it in fact makes the surgeon's job easier to dislocate the patella laterally if VM is released adequately from intermuscular septum.35 Moreover, synovial division further helps in lateral displacement of patella.35 Also, our surgical technique involves eversion of patella after tibial and femoral cuts were taken as quadriceps gets relaxed. Although, all the parts of the knee may not be seen simultaneously, symbiotic use of retractors and use of mobile skin window to accomplish the sequential steps with adequate exposure are the key factors in the mini-subvastus approach.35,37 In our series, we were able to gain exposure that even suffice for release of the lateral structures including posterolateral capsule and IT band. In addition, in this study, posterolateral capsule was released in 86 (78.18%) cases while IT band was released in 62 (56.36%) knees using piecrust technique. While none of the cases required extensive lateral release including LCL and popliteus, and medial advancement techniques. Likewise, several studies 8,24,25 had revealed the importance of isolated IT band release or titrated release of lateral structures by pie crusting method for gap balancing. Furthermore, the present study did not observe any component malalignment, which has also been case with similar other studies.18,38 However, a detailed analysis of component positioning would form the basis of another study. Appropriate exposure of lateral tibial plateau 35 and use of transepicondylar axis for referencing instead of posterior condylar referencing 1 for femur helps us to minimize the component malalignment in valgus knees.
In present study, CR implants were used in 89 (80.90%) knees. A recent study 39 demonstrated the efficacy of CR implants in valgus knees and that survival of implant is improved when lateral stabilizers like LCL and/or popliteus tendon are preserved. Moreover, we assessed the sagittal plane stability intraoperatively by adequacy of posterior cruciate ligament (PCL), and the decision to retain or substitute the PCL was made intraoperatively. Sacrifice of PCL was done in cases of laxity and deformity not correctable without the release of PCL. A previous study 40 used similar trends based on integrity of PCL. Posterior stabilized implants were used in 20 (18.18%) knees. Furthermore, the outcome of patients with both CR and PS implant types were similar with no significant differences [Table 2]. Only one patient needed constrained condylar knee with severe combined valgus and recurvatum deformity. Likewise, several studies in past had reported the use of constrained knees using various approaches.5,7,40 Patellar resurfacing was done in selected 36 knees, especially those with significant disease of femoral trochlear surface.
In our series, one knee had patellar component malpositioning, due to surgical error, which can be avoided by carefully identifying the boundaries of patella after resection. One patient had hyperextension of knee that was revised with liner exchange. One patient had foot drop postoperatively that recovered gradually. It may be due to peroneal nerve injury,41,42 direct traction on the nerve, traction on the surrounding tissues resulting in vascular compromise to the nerve, direct pressure on the nerve from the postoperative dressing, or a combination of these factors. The complication rates were comparable to other series using various conventional approaches [Table 3].
The limitations of the study are:First, this is a retrospective study with all its inherent biases and limitations. However, all the patients were managed by single surgeon senior author (NAS), using same protocol thereby decreasing the influence of the confounding factors. Second, the current study is a midterm followup study with average followup of 40 months. Long term followup to assess the outcome is required. Nevertheless, this issue can be undertaken with further followup of same study group. Third, this study does not involve any comparison with the other approaches used for valgus knees. But, the senior author exclusively uses subvastus approach for all cases of TKA including varus knees and revisions with satisfactory outcomes. Therefore, evaluation of TKA outcome with this sole technique is prudent. Fourth, the assessment of VAS scores was done on postoperative day 1 and 2. However, the results may have been affected by the use of femoral nerve block though it has been used for 12 h postoperatively only.
CONCLUSIONS
A mini-subvastus medial quadriceps approach provides adequate exposure for TKA in valgus knees including the lateral structures, without increase in incidence of complications. It provides excellent early recovery phase.13,17,20,21 Midterm followup showed good outcome in terms of mechanical alignment and the functional scores.
REFERENCES
- 1.Wheeless CR. Wheeless’ Textbook of Orthopaedics. Duke university medical center and Trace internet publishing, LLC. 2013 Feb [Google Scholar]
- 2.Elkus M, Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS. Total knee arthroplasty for severe valgus deformity. Five to fourteen-year followup. J Bone Joint Surg Am. 2004;86-A:2671–6. doi: 10.2106/00004623-200412000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Favorito PJ, Mihalko WM, Krackow KA. Total knee arthroplasty in the valgus knee. J Am Acad Orthop Surg. 2002;10:16–24. doi: 10.5435/00124635-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Sasanuma H, Sekiya H, Takatoku K, Takada H, Sugimoto N. Evaluation of soft-tissue balance during total knee arthroplasty. J Orthop Surg (Hong Kong) 2010;18:26–30. doi: 10.1177/230949901001800106. [DOI] [PubMed] [Google Scholar]
- 5.Apostolopoulos AP, Nikolopoulos DD, Polyzois I, Nakos A, Liarokapis S, Stefanakis G, et al. Total knee arthroplasty in severe valgus deformity: Interest of combining a lateral approach with a tibial tubercle osteotomy. Orthop Traumatol Surg Res. 2010;96:777–84. doi: 10.1016/j.otsr.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Fiddian NJ, Blakeway C, Kumar A. Replacement arthroplasty of the valgus knee. A modified lateral capsular approach with repositioning of vastus lateralis. J Bone Joint Surg Br. 1998;80:859–61. doi: 10.1302/0301-620x.80b5.7626. [DOI] [PubMed] [Google Scholar]
- 7.Nikolopoulos DD, Polyzois I, Apostolopoulos AP, Rossas C, Moutsios-Rentzos A, Michos IV. Total knee arthroplasty in severe valgus knee deformity: Comparison of a standard medial parapatellar approach combined with tibial tubercle osteotomy. Knee Surg Sports Traumatol Arthrosc. 2011;19:1834–42. doi: 10.1007/s00167-011-1474-4. [DOI] [PubMed] [Google Scholar]
- 8.Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am. 2005;87(Suppl 1):271–84. doi: 10.2106/JBJS.E.00308. [DOI] [PubMed] [Google Scholar]
- 9.Satish BR, Ganesan JC, Chandran P, Basanagoudar PL, Balachandar D. Efficacy and mid term results of lateral parapatellar approach without tibial tubercle osteotomy for primary total knee arthroplasty in fixed valgus knees. J Arthroplasty. 2013;28:1751–6. doi: 10.1016/j.arth.2013.04.037. [DOI] [PubMed] [Google Scholar]
- 10.Sekiya H, Takatoku K, Takada H, Sugimoto N, Hoshino Y. Lateral approach is advantageous in total knee arthroplasty for valgus deformed knee. Eur J Orthop Surg Traumatol. 2014;24:111–5. doi: 10.1007/s00590-012-1137-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hay GC, Kampshoff J, Kuster MS. Lateral subvastus approach with osteotomy of the tibial tubercle for total knee replacement: A two-year prospective, randomised, blinded controlled trial. J Bone Joint Surg Br. 2010;92:862–6. doi: 10.1302/0301-620X.92B6.24027. [DOI] [PubMed] [Google Scholar]
- 12.Niki Y, Matsumoto H, Hakozaki A, Kanagawa H, Toyama Y, Suda Y. Clinical and radiographic outcomes of minimally invasive total knee arthroplasty through a lateral approach. Knee Surg Sports Traumatol Arthrosc. 2011;19:973–9. doi: 10.1007/s00167-010-1323-x. [DOI] [PubMed] [Google Scholar]
- 13.Bonutti PM, Zywiel MG, Ulrich SD, Stroh DA, Seyler TM, Mont MA. A comparison of subvastus and midvastus approaches in minimally invasive total knee arthroplasty. J Bone Joint Surg Am. 2010;92:575–82. doi: 10.2106/JBJS.I.00268. [DOI] [PubMed] [Google Scholar]
- 14.Mizner RL, Petterson SC, Stevens JE, Vandenborne K, Snyder-Mackler L. Early quadriceps strength loss after total knee arthroplasty. The contributions of muscle atrophy and failure of voluntary muscle activation. J Bone Joint Surg Am. 2005;87:1047–53. doi: 10.2106/JBJS.D.01992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silva M, Shepherd EF, Jackson WO, Pratt JA, McClung CD, Schmalzried TP. Knee strength after total knee arthroplasty. J Arthroplasty. 2003;18:605–11. doi: 10.1016/s0883-5403(03)00191-8. [DOI] [PubMed] [Google Scholar]
- 16.Bindelglass DF, Vince KG. Patellar tilt and subluxation following subvastus and parapatellar approach in total knee arthroplasty. Implication for surgical technique. J Arthroplasty. 1996;11:507–11. doi: 10.1016/s0883-5403(96)80101-x. [DOI] [PubMed] [Google Scholar]
- 17.Boerger TO, Aglietti P, Mondanelli N, Sensi L. Mini-subvastus versus medial parapatellar approach in total knee arthroplasty. Clin Orthop Relat Res. 2005;440:82–7. doi: 10.1097/01.blo.0000185755.09777.2d. [DOI] [PubMed] [Google Scholar]
- 18.Laskin RS. Minimally invasive total knee arthroplasty: The results justify its use. Clin Orthop Relat Res. 2005;440:54–9. doi: 10.1097/01.blo.0000186562.08685.a2. [DOI] [PubMed] [Google Scholar]
- 19.Matsueda M, Gustilo RB. Subvastus and medial parapatellar approaches in total knee arthroplasty. Clin Orthop Relat Res. 2000;371:161–8. doi: 10.1097/00003086-200002000-00020. [DOI] [PubMed] [Google Scholar]
- 20.Tashiro Y, Miura H, Matsuda S, Okazaki K, Iwamoto Y. Minimally invasive versus standard approach in total knee arthroplasty. Clin Orthop Relat Res. 2007;463:144–50. [PubMed] [Google Scholar]
- 21.King J, Stamper DL, Schaad DC, Leopold SS. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty. Assessment of the learning curve and the postoperative recuperative period. J Bone Joint Surg Am. 2007;89:1497–503. doi: 10.2106/JBJS.F.00867. [DOI] [PubMed] [Google Scholar]
- 22.Huang HT, Su JY, Chang JK, Chen CH, Wang GJ. The early clinical outcome of minimally invasive quadriceps-sparing total knee arthroplasty: Report of a 2-year followup. J Arthroplasty. 2007;22:1007–12. doi: 10.1016/j.arth.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 23.Benoni G, Fredin H. Fibrinolytic inhibition with tranexamic acid reduces blood loss and blood transfusion after knee arthroplasty: A prospective, randomised, double-blind study of 86 patients. J Bone Joint Surg Br. 1996;78:434–40. [PubMed] [Google Scholar]
- 24.Aglietti P, Lup D, Cuomo P, Baldini A, De Luca L. Total knee arthroplasty using a pie-crusting technique for valgus deformity. Clin Orthop Relat Res. 2007;464:73–7. doi: 10.1097/BLO.0b013e3181591c48. [DOI] [PubMed] [Google Scholar]
- 25.Clarke HD, Fuchs R, Scuderi GR, Scott WN, Insall JN. Clinical results in valgus total knee arthroplasty with the “pie crust” technique of lateral soft tissue releases. J Arthroplasty. 2005;20:1010–4. doi: 10.1016/j.arth.2005.03.036. [DOI] [PubMed] [Google Scholar]
- 26.Krackow KA, Jones MM, Teeny SM, Hungerford DS. Primary total knee arthroplasty in patients with fixed valgus deformity. Clin Orthop Relat Res. 1991;273:9–18. [PubMed] [Google Scholar]
- 27.Whiteside LA. Correction of ligament and bone defects in total arthroplasty of the severely valgus knee. Clin Orthop Relat Res. 1993;288:234–45. [PubMed] [Google Scholar]
- 28.Koninckx A, Schwab PE, Deltour A, Thienpont E. The minimally invasive far medial subvastus approach for total knee arthroplasty in valgus knees. Knee Surg Sports Traumatol Arthrosc. 2014;22:1765–70. doi: 10.1007/s00167-013-2701-y. [DOI] [PubMed] [Google Scholar]
- 29.Dalury DF, Dennis DA. Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res. 2005;440:77–81. doi: 10.1097/01.blo.0000185757.17401.7b. [DOI] [PubMed] [Google Scholar]
- 30.Fauré BT, Benjamin JB, Lindsey B, Volz RG, Schutte D. Comparison of the subvastus and paramedian surgical approaches in bilateral knee arthroplasty. J Arthroplasty. 1993;8:511–6. [PubMed] [Google Scholar]
- 31.Scuderi RG, Tria JA. Insall and Scott's Textbook of Knee Surgery. 4th ed. Churchill Livingstone; 2006. Jan, [Google Scholar]
- 32.Karachalios T, Sarangi PP, Newman JH. Severe varus and valgus deformities treated by total knee arthroplasty. J Bone Joint Surg Br. 1994;76:938–42. [PubMed] [Google Scholar]
- 33.Stern SH, Moeckel BH, Insall JN. Total knee arthroplasty in valgus knees. Clin Orthop Relat Res. 1991;273:5–8. [PubMed] [Google Scholar]
- 34.Wetzner SM, Bezreh JS, Scott RD, Bierbaum BE, Newberg AH. Bone scanning in the assessment of patellar viability following knee replacement. Clin Orthop Relat Res. 1985;199:215–9. [PubMed] [Google Scholar]
- 35.Shah N, Nilesh G, Patel N. Mini-subvastus approach for total knee arthroplasty in obese patients. Indian J Orthop. 2010;44:292–9. doi: 10.4103/0019-5413.65157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lotke PA, Lonner JH. Master Techniques in Orthopaedic Surgery: Knee Arthroplasty. Philadelphia: Lippincott Williams and Wilkins; 2008. [Google Scholar]
- 37.Bonutti PM, Mont MA, Kester MA. Minimally invasive total knee arthroplasty: A 10-feature evolutionary approach. Orthop Clin North Am. 2004;35:217–26. doi: 10.1016/j.ocl.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 38.Haas SB, Cook S, Beksac B. Minimally invasive total knee replacement through a mini midvastus approach: A comparative study. Clin Orthop Relat Res. 2004;428:68–73. doi: 10.1097/01.blo.0000147649.82883.ca. [DOI] [PubMed] [Google Scholar]
- 39.McAuley JP, Collier MB, Hamilton WG, Tabaraee E, Engh GA. Posterior cruciate-retaining total knee arthroplasty for valgus osteoarthritis. Clin Orthop Relat Res. 2008;466:2644–9. doi: 10.1007/s11999-008-0436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rajgopal A, Dahiya V, Vasdev A, Kochhar H, Tyagi V. Long term results of total knee arthroplasty for valgus knees: Soft-tissue release technique and implant selection. J Orthop Surg (Hong Kong) 2011;19:60–3. doi: 10.1177/230949901101900114. [DOI] [PubMed] [Google Scholar]
- 41.Rose HA, Hood RW, Otis JC, Ranawat CS, Insall JN. Peroneal-nerve palsy following total knee arthroplasty. A review of The Hospital for Special Surgery experience. J Bone Joint Surg Am. 1982;64:347–51. [PubMed] [Google Scholar]
- 42.Schinsky MF, Macaulay W, Parks ML, Kiernan H, Nercessian OA. Nerve injury after primary total knee arthroplasty. J Arthroplasty. 2001;16:1048–54. doi: 10.1054/arth.2001.26591. [DOI] [PubMed] [Google Scholar]



